Abstract
INTRODUCTION
Paraduodenal hernia (paramesocolic hernia), a rare congenital anomaly due to a midgut malrotation during fetal development, is recognized as the most frequent internal hernias. Two variants have been described: left and right, the latter less common than the first one.
PRESENTATION OF CASE
We report a right paraduodenal hernia case in a 86 years old female patient who developed an acute bowel obstruction syndrome. Final diagnosis was achieved by imaging techniques as abdomen X-ray and CT and confirmed only after surgical operation.
DISCUSSION
Surgical approach was via median laparotomy, consisting in hernia reduction, replacement and stitching of the bowel in its anatomical orientation, and fixing of the posterior wall defect. At 15 months follow-up from surgical procedure the patient is asymptomatic.
CONCLUSION
Paraduodenal hernia is a rare pathology but its involvement in bowel obstruction syndrome should be always taken into account during diagnostic process.
Keywords: Paraduodenal hernia, Small bowel obstruction, Abdominal surgery, Retroperitoneum defects
1. Introduction
Internal hernia development came from defects or recessum presence in which a viscera could became entrapped being incarcerated or strangulated. Wall defects origin could derive from fetal development abnormalities, traumas, infectious diseases or iatrogenic trauma after previous surgery.1 Paraduodenal hernia (PDH) refers to a small bowel herniation through a peritoneal sac in the IVth duodenal part or in duodenal caudal segment. First description about internal hernias developed in retroperitoneal abdomen areas, near duodenal–jejunal junction, was reported by Treitz in 1857.2 First classification in right and left PDH was done in 1889 by Jonnesco.3 Defect presence is due to rotation and fixation abnormalities of the primitive midgut during fetal development, with accessory peritoneal recessum and fossae as results (Fig. 1). Nearly 10 types of these formations are been known and classified, with the most common reported in the Treitz inferior fossae (60%), inferior and superior paraduodenal fossae (30%), superior paraduodenal fossae (5%), paraduodenal Landzert fossae (2%), duodenal–jejunal fossae (Treitz's hernia, 2%), and Waldeyer fossae (1%).4,5 In right PDH the presence of Waldeyer fossae represents the major development cause, through this entity the erniation lies and is fixed against by the following ascending mesocolon fusion to retroperitoneum, shaping a hernia sac which reside right to the median line. Structures involved are the ascending mesocolon and a transverse colon segment which build the anterior part of the hernia sac, and the SMA with ileocolic artery which lie along the free sac edge.3,6,7 Common clinical presentation of PDH is an acute small bowel obstruction (SBO). Internal hernia incidence in this syndrome is about 1–4.1% and in these PDH is reported to be between 30% and 50%.6,8,9 The exact incidence, however, is difficult to assess due to asymptomatic patients. Post-mortem findings report incidence to be between 0.2 and 2%.10 About 75% of the PDH develops in the left side of abdomen near Landzert fossae, 25% in right side near Waldeyer fossae below duodenum and superior mesenteric artery (SMA).5,11 While left PDH development does not seems to correlate with patient gender, right development is more common in men with a 3:1 rate of incidence.5
Fig. 1.
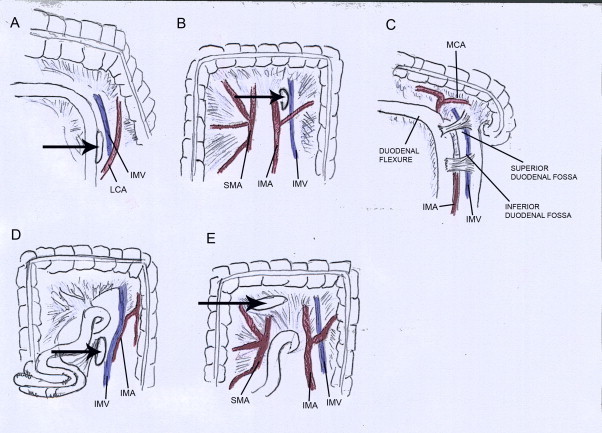
Coronal drawing of abdominal recessum and fossae (arrows and lines). (A and B) Landzert's fossae. IMA, inferior mesenteric artery; IMV, inferior mesenteric vein; LCA, left colic artery; SMV, superior mesenteric vein. (C) Superior + inferior duodenal hernias. MCA, middle colic artery. (D) Waldeyer's fossae. (E) Transmesocolic fossae.
2. Clinical case
In Surgery Emergency Department of “San Camillo” Hospital in Rome, a old female patient was transferred following a suspected diagnosis of SBO. Patient (86 years old, 96 kg weight) complained about strong abdominal pain presence, nausea, vomititing episodes starting the day before and stool absence since 2 days. Patient inspection showed mild condition, absence of fever, localized pain and tenderness localized in lower abdominal quadrants, with mild distension and increased enterocolic timpanism. Peristalsis was normal and Blumberg sign was slightly positive. Blood routine exams showed normal GB, HGB, HCT values with elevated WBC, ESR and C-reactive proteins. Plain abdominal X-ray showed small fluid levels within bowel walls and subsequent abdominal CT demonstrated signs of small bowel sovradistension in meso-ipogastrium, fluid levels presence and thickening in mesentery walls (Fig. 2). Patient underwent median laparotomy, after peritoneum dissection right ansae delocalization was evident. First operation step was to locate, isolate and reduce the hernia sac with a gently dissection along the lateral avascular plane by finger and with ultracision dissector (Fig. 3). About 30 cm of small bowel were injured from ischemic damage and did not benefit from revascularization within time limits (Fig. 4), hence a resection followed by a hand termino-terminal anastomosis was performed (Fig. 5). Anatomical ansae relocalization was finally obtained by a gently rotation and fixation of ascending and descending colon to the posterior retroperitoneal wall by non-absorbable suture. Suture was also used in defect closure to prevent successive hernias risks. A perianastomotic drainage tube was placed during surgery. Patient was discharged the Xth day post-operative.
Fig. 2.
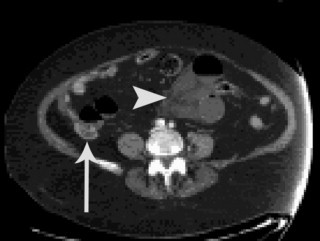
CT scan with small bowel ansa sovradistension, fluid levels presence among bowel segments (arrows) and thickening in mesentery walls (arrows head).
Fig. 3.
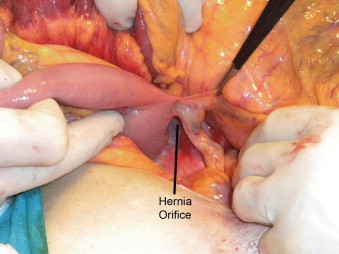
Intraoperative findings: hernia orifice along Treitz's ligament.
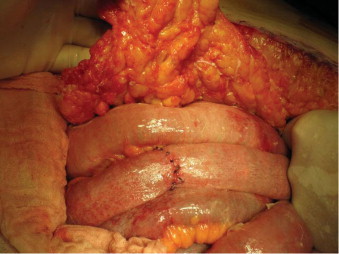
Fig. 4.
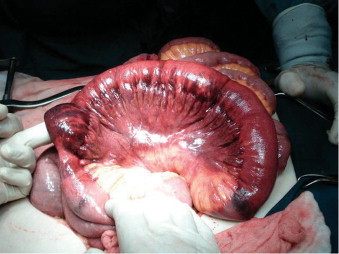
Ischemic suffering of small bowel ansa.
Fig. 5.
Termino-terminal anastomosis after intestinal resection.
3. Discussion
Paramesocolic hernias define rare anatomic anomalities which could lead to a SBO syndrome. Usually both internal and external hernias behave the same way, except for the lack of swelling in the internal ones. Hernias derive from any defect, inborn or acquired, in which a sac contains any abdominal organ. Usually hernias are mildly symptomatic or asymptomatic at all, with symptoms rising over time due to the sac growth and extension. Hernia symptoms could appear at any age, however are rare in the first two decades and the median diagnosis age is between 4th and 6th decades. Symptoms could be aspecific: from patient generic discomfort with undefined or localized postprandial abdominal pain and weight loss, to a sub-acute small bowel obstruction with nausea and slight abdominal distension and finally with heavy abdominal pain, vomiting, large abdominal distension and timpanism in an acute bowel obstruction episode. Pain appearance comes from onset of complications, like inflammation, strangulation or obstruction. Because small bowel content is mostly liquid, obstruction less likely develops in these hernias, delaying symptoms to advanced stages, like ischemia and necrosis. In advanced stages, bowel wall contracture can be considered as a peritoneal complication and a sign of perforation. As explained above, in external hernias symptomatology is easy reliable to the swelling, in internal ones this correlation is not constant, due to the lack of swelling evidence. SBO development, as a common final stage, is often preceded by several symptoms frequently founded in GI tract diseases such as irritable bowel syndrome, gastritis, gastroesophageal reflux disease, iatal hernia, and biliary disease.10 Therefore most of the patients remain asymptomatic over years, or the misguided interpretation of these symptoms leads to inappropriate treatment, until obstructive or ischemic complications appear. Surgery represents the treatment of choice in SBO, while a great attention should be assert to patient history and actual conditions. Paraduodenal hernia presence could emerge during emergency operations as well elective abdominal surgery for other diseases: hernias incidental findings during abdominal surgery are now considered enough for an immediate fixation due to the high risks (50%) of future SBO syndrome.10,12 Completely removal of sac is inadvisable, as described in literature, because of high risks of damage to the SMA and its branches and a potentially massive blood loss. Laparotomy is the most used incision when diagnosis has to be assessed among several causes. Laparoscopic repair has been utilized in various reports from 1998, this technique demonstrates its efficacy and reliability in defect repair, under expert operator hands, in both emergency and elective procedures.12–15 Patients should be still carefully evaluated to avoid wide dilated ansae and pneumoperitoneum related risks. Prostesis placement in defects repair is not common, typical defects width ranges are well closed by a single suture which is, by some authors,15 used to create a new ligament in bowel relocation. Mesh implants are reserved in large defects presence or recurrence hernias.14
4. Conclusion
We reported our experience in diagnosing and treating a right paraduodenal hernia, though PDH is actually a rare pathology, its involvement in obstructive syndrome development should be always suspected until it became ruled out. Preparation and execution of surgery require specific anatomical knowledge because of both preoperative doubts and low global incidence of the disease. CT scan is the most specific imaging technique to acquire a diagnosis preoperatively. Surgical approach represents the appropriate treatment, and it is mandatory in perforation–necrosis evidence; besides differences in the course of SMA and its branches represent a major threat to surgeons. Both open techniques and laparoscopy are used, with the latter one being preferred mostly with a pre-operative diagnosis and a determined plan.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
None.
Ethical approval
Written consent obtained.
Author contributions
Manfredelli Simone, Zitelli Andrea and Pontone Stefano are the manuscript authors. Manfredelli Simone, Mancini Renato and Angelici Alberto performed surgery and study design. Leonetti Giovanni, Forte Angelo and Marcantonio Maria performed data collections, data analysis and supervised the work.
References
- 1.Stern L.E., Warner B.W. Congenital internal abdominal hernias: incidence and management. In: Fitzgibbons R.J., Greenburg A.G., editors. Nyhus and condon's hernia. 5th ed. Lippincott Williams and Wilkins; Philadelphia: 2002. [Google Scholar]
- 2.Treitz W. Credner; Prague: 1857. Hernia retroperitonealis. Ein Beitrag zur Geschichte innerer Hernien. [Google Scholar]
- 3.Jonnesco T. Legrosnier et Babe; Paris: 1889. Anatomie topographique du duodenum et hernies duodenales. [Google Scholar]
- 4.Murray H.O. Left paraduodenal hernia. Canadian Medical Association Journal. 1955;72(4):263–267. [PMC free article] [PubMed] [Google Scholar]
- 5.Desjardins A.U. Left paraduodenal hernia. Annals of Surgery. 1918;67(2):195–201. doi: 10.1097/00000658-191802000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghahremani G.G. Internal abdominal hernias. Surgical Clinics of North America. 1984;64(2):393–406. doi: 10.1016/s0039-6109(16)43293-7. [DOI] [PubMed] [Google Scholar]
- 7.Bartlett M.K., Wang C., Williams W.H. The surgical management of paraduodenal hernia. Annals of Surgery. 1968;168(2):249–254. doi: 10.1097/00000658-196808000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moran J.M., Salas J., Sanjuán S., Amaya J.L., Rincón P., Serrano A., Tallo E.M. Paramesocolic hernias: consequences of delayed diagnosis. Report of three new cases. Journal of Pediatric Surgery. 2004;39(1):112–116. doi: 10.1016/j.jpedsurg.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 9.Khan M.A., Lo A.Y., Vande Maele D.M. Paraduodenal hernia. American Surgeon. 1998;64(12):1218–1222. [PubMed] [Google Scholar]
- 10.Zissin R., Hertz M., Gayer G., Paran H., Osadchy A. Congenital internal hernia as a cause of small bowel obstruction: CT findings in 11 adult patients. British Journal of Radiology. 2005;78(933):796–802. doi: 10.1259/bjr/87050272. [DOI] [PubMed] [Google Scholar]
- 11.Cogswell H.D., Thomas C.A. Right paraduodenal hernia. Annals of Surgery. 1941;114(6):1035–1041. doi: 10.1097/00000658-194112000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uematsu T., Kitamura H., Iwase M., Yamashita K., Ogura H., Nakamuka T. Laparoscopic repair of a paraduodenal hernia. Surgical Endoscopy. 1998;12(1):50–52. doi: 10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]
- 13.Antedomenico E., Singh N.N., Zagorski S.M., Dwyer K., Chung M.H. Laparoscopic repair of a right paraduodenal hernia. Surgical Endoscopy. 2004;18(1):165–166. doi: 10.1007/s00464-003-4516-2. [DOI] [PubMed] [Google Scholar]
- 14.Palanivelu C., Rangarajan M., Jategaonkar P.A., Anand N.V., Senthilkumar K. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12(6):649–653. doi: 10.1007/s10029-008-0376-y. [DOI] [PubMed] [Google Scholar]
- 15.Khalaileh A., Schlager A., Bala M., Abu-Gazala S., Elazary R., Rivkind A.I. Left laparoscopic paraduodenal hernia repair. Surgical Endoscopy. 2010;24(6):1486–1489. doi: 10.1007/s00464-009-0794-7. [DOI] [PubMed] [Google Scholar]


