Abstract
INTRODUCTION
The Median Arcuate Ligament Syndrome is a rare condition characterized by postprandial abdominal pain, bowel function disorder and weight loss. We report the first case to our knowledge of Crohn's disease and Median Arcuate Ligament Syndrome.
PRESENTATION OF CASE
The patient was a 33 year-old female with a previous diagnosis of Crohn's disease. Acute postprandial abdominal pain affected the patient every day; she was, therefore, referred to US-Doppler and magnetic resonance angiography of the abdominal vessels and received a diagnosis of Median Arcuate Ligament Syndrome. Consequently, the patient was surgically treated, releasing the vascular compression. After the operation, she reported a complete relief from postprandial pain which was one of her major concerns. Subocclusive symptoms occurred after six months due to the inflammatory reactivation of the terminal ileitis.
DISCUSSION
The diagnosis of Median Arcuate Ligament Syndrome is mainly based on the exclusion of other intestinal disorders but it should be always confirmed using noninvasive tests such as US-Doppler, angio-CT or magnetic resonance angiography.
CONCLUSION
This case demonstrates that the Median Arcuate Ligament Syndrome could be the major cause of symptoms, even in presence of other abdominal disorders.
Abbreviations: MALS, Median Arcuate Ligament Syndrome; MAL, Median Arcuate Ligament; CD, Crohn's disease; CT, computerized tomography; MRA, magnetic resonance angiography; US, ultra-sonography; WBC, white blood cells; ESR, erythrocyte sedimentation rate
Keywords: Median Arcuate Ligament Syndrome, Dunbar's Syndrome, Crohn's disease
1. Introduction
Clinical radiological studies based on the relation between abdominal symptoms and celiac trunk compression by right diaphragmatic crux, led to the inclusion of a new condition in the field of vascular pathology – the Celiac Trunk Compression Syndrome.1 This disorder mainly affects young ectomorphic females between the age of 20 and 50 (F:M ratio of 4:1).2 The symptoms are typically three: postprandial abdominal pain, bowel function disorder and weight loss. This triad resembles the symptoms of intestinal angina caused by atherosclerotic lesions of the major splanchnic vessels; postprandial pain, however, is less severe.1,3,4 The grade of stenosis, the systolic and diastolic flow velocities in the celiac trunk can be evaluated by means of noninvasive tests such as US-Doppler, angio-CT or magnetic resonance angiography (MRA).5–8 What follows is our first case of Median Arcuate Ligament Syndrome (MALS) in a patient with Crohn's disease (CD).
2. Presentation of case
A 33 year-old female patient arrived with a history of abdominal pain associated with alternating bowel function and nausea she experienced since the age of 20. In the previous 3 years she lost 5 kg and experienced a degeneration of abdominal pain, especially after meals, weakness, fatigue, nausea and diarrhea. The patient was admitted to the Gastroenterology Department. Laboratory evaluation revealed higher WBC (13.7 mg/dl) and inflammatory markers (ESR 33 mm/h, CR-Protein 48 mg/L). A pancolonoscopy with retrograde ileoscopy showed hyperemic mucosa with vascular pattern alteration at the ileal site. The histopathological examination of biopsies showed inflammatory changes, typical of CD. Thickening of the terminal ileal loop and its mesentery was seen on CT scan. The patient started a treatment of mesalazine 1600 mg × 2/die. A period of remission was followed by a relapse, as treatment had to be suspended because of a pregnancy. The patient, however, continued suffering from postprandial pain; a US-Doppler of the abdominal vessels was performed (Fig. 1) which showed stenosis of the celiac trunk with an increase in flow velocity. The MRA confirmed the stenosis of celiac trunk with extrinsic compression (Fig. 2). Although CD was confirmed by the histopathological examination, the clinical history of postprandial pain along with the radiological evidence of celiac artery stenosis facilitated a diagnosis of both MALS and Crohn's disease. With this joint clinical scenario, the situation was thoroughly discussed with the patient and the decision to perform surgical release of the MAL was agreed. Laparotomy was performed; inspection of the ileum showed no CD features. Consequently, we made an exploration and skeletonization of the celiac trunk, common hepatic and left gastric artery (Fig. 3A). Digital palpation of celiac artery branches elicited very weak pulse. An intraoperative Doppler of the celiac trunk confirmed the stenosis and the increased flow velocity. A fibrotic area compressing the celiac trunk at the origin of the left gastric artery was identified and cut (Fig. 3B). Subsequently, the arcuate ligament was cut along its entire length (about 2 cm) and sent for a histopathological test. The normalization of the celiac blood flow was confirmed by intraoperative US-Doppler; the pulse was restored in the common hepatic, gastroduodenal and left gastric arteries. The histopathological examination of the specimen revealed a fibrotic tissue with hypertrophic peripheral nerve structures. The patient had a short hospital stay and was discharged after three days reporting a complete relief of symptoms, especially of postprandial pain, and relative good health. Six months after the operation, she returned for a complaint of abdominal pain and subocclusion. Colonoscopy with retrograde ileoscopy showed a mild terminal ileum inflammation; fecal calprotectin was 97 mg/kg. To date, the patient is on medical treatment for CD with a good response.
Fig. 1.

US-Doppler showing the increase in flow velocity (A) and stenosis of the celiac trunk (B).
Fig. 2.
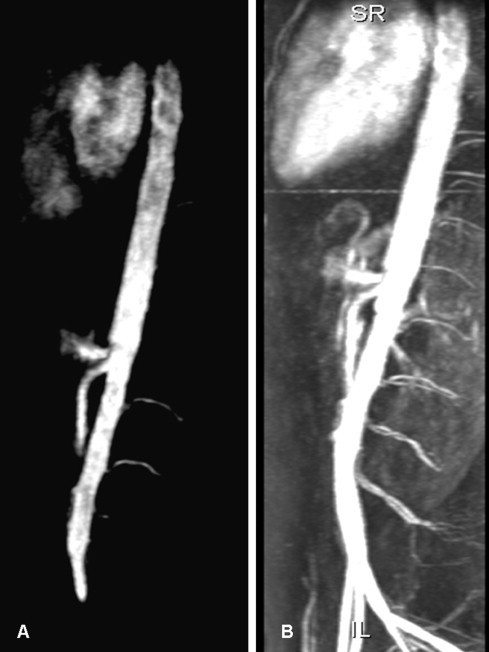
MRA images of the aorta and celiac trunk showing stenosis at the origin of the celiac trunk.
Fig. 3.

Intraoperative image of the median arcuate ligament fibers compressing the celiac trunk (A). An image after cutting the median arcuate ligament (B).
3. Discussion
The MALS is a rare vascular disorder with an incidence of about 2 cases per 100,000 patients, with diffused and non-specific abdominal pain. In literature, it was found that the incidence of MALS in asymptomatic patients ranges between 7.3 and 27%.2,8–10 Such high incidence in asymptomatic patients could raise the issue whether surgical release of the compression would relieve the symptoms of non-specific abdominal pain, which could be related to other causes. It is known that many patients have minimal asymptomatic celiac trunk compression; hence, it is of major importance to discriminate those having a pathological compression.5 The first anatomic description of MALS dates back to 1917, given by Lipshutz,11 but only in 1965 the radiologist J.D. Dunbar reported the first case series focusing on diagnosis and treatment.1 This syndrome is due to the celiac trunk compression by the median arcuate ligament in association with ganglionic periaortic tissue.9 Although 47 years have elapsed, the pathogenesis of MALS is still uncertain. Some authors support the theory based on a higher origin of the celiac trunk from aorta, others maintain the exuberant growth of neurofibrous tissue originating from the celiac plexus causing compression.12 The symptoms are the typical postprandial pain associated with nausea, vomiting, and unintentional weight loss.13 The pathophysiology of MALS is still unknown. The first hypothesis is based on mesenteric ischemia even if the superior and inferior mesenteric arteries are normal. It could be due to postprandial “theft” of blood, which causes pain. The second, instead, is the consequence of direct or indirect overstimulation of the celiac plexus, caused by chronic inflammation, resulting in splanchnic vasoconstriction with ischemia.5,13 Despite several tests, the diagnosis is based on the exclusion of other abdominal diseases. Lateral aortic angiography is the gold standard but there are other less invasive techniques such as US-Doppler, CT or MRA. In every case it is important to correlate abdominal symptoms with radiological data.8,13 The treatment consists in the section of the MAL, and may be carried out by an open or laparoscopic approach. Most of the cases in literature were treated with the open technique.5,8,9,13 The longest case series was published in 1985, by Reilly, with 51 patients, showing good long-term results.9 Some authors proposed also an endovascular treatment, but it did not give good results due to the persisting extrinsic compression. Conversely, this may be a useful treatment in case of persistent symptoms following the surgical section of the MAL, due to vessel wall alterations caused by the chronic external compression.5,13 CD, one of the two major forms of inflammatory bowel diseases, has an etiology and pathogenesis that includes complex interactions of genetic, immunological and environmental factors, with an important role being played by luminal microbial agents.14 It has different clinical pattern and, in every case, the common symptoms are mainly abdominal pain associated with diarrhea and fever. Extraintestinal symptoms such as erythema nodosum, iritis and uveitis, peripheral artritis could also appear.15 As reported in literature, the diagnosis of MALS is mainly based on the fusion of symptoms and radiological images excluding other abdominal diseases. Although in our patient CD would have justified most of the symptoms, postprandial pain was so typical that it lead us to think of other pathologies and, consequently, to performing vascular investigations. After surgery, the patient had a complete remission of abdominal symptoms, especially postprandial pain. It would also be important to evaluate if the chronic ischemia, resulting from the compression of the celiac trunk, could be a long-term co-factor in the development of a multiple-site chronic inflammatory disease compatible with CD.
4. Conclusion
This case demonstrates that the Median Arcuate Ligament Syndrome could be the major cause of symptoms, even in existence of other abdominal disorders. For this reason in patients with upper gastrointestinal disorders, especially postprandial pain, that persist after medical therapy, it could be useful to perform vascular investigation evaluating the possibility of celiac trunk compression.
Conflict of interest
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors’ contribution
All authors contributed equally to this work: Alessandro Sturiale, Giovanni Alemanno and Francesco Bellucci collected the data, Alessandro Sturiale and Giovanni Alemanno analyzed data, Alessandro Sturiale, Giovanni Alemanno, Francesco Giudici and Rami Addasi wrote the manuscript, Francesco Tonelli supervised all the manuscript and obtained an informed consent from the patient.
Acknowledgement
Prof. Maria Rosaria Buri, Professional Translator/AIIC Conference Interpreter, University of Salento for the English language editing.
References
- 1.Dunbar J.D., Molnar W., Beman F.F., Marable S.A. Compression of the celiac trunk and abdominal angina. American Journal of Roentgenology, Radium Therapy and Nuclear Medicine. 1965;95(3):731–744. doi: 10.2214/ajr.95.3.731. [DOI] [PubMed] [Google Scholar]
- 2.Trinidad-Hernandez M., Keith P., Habib I., White J.V. Reversible gastroparesis: functional documentation of celiac axis compression syndrome and postoperative improvement. American Surgeon. 2006;72(4):339–344. [PubMed] [Google Scholar]
- 3.Bobbio A., Zanella E., Chiampo L. Stenosis caused by compression of the celiac trunk. Minerva Chirurgica. 1967;22(18):1024–1034. [PubMed] [Google Scholar]
- 4.Curl J.H., Thopson N.W., Stanley J.C. Median arcuate ligament compression of the celiac and superior mesenteric arteries. Annals of Surgery. 1971;173(2):314–320. doi: 10.1097/00000658-197102000-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duncan A.A. Median arcuate ligament syndrome. Current Treatment Options in Cardiovascular Medicine. 2008;10(2):112–116. doi: 10.1007/s11936-008-0012-2. [DOI] [PubMed] [Google Scholar]
- 6.Horton K.M., Talamini M.A., Fishman E.K. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics. 2005;25(5):1177–1182. doi: 10.1148/rg.255055001. [DOI] [PubMed] [Google Scholar]
- 7.Kopecky K.K., Stine S.B., Dalsing M.C., Gottlieb K. Median arcuate ligament syndrome with multivessel involvement: diagnosis with spiral CT angiography. Abdominal Imaging. 1997;22(3):318–320. doi: 10.1007/s002619900199. [DOI] [PubMed] [Google Scholar]
- 8.Vaziri K., Hungness E.S., Pearson E.G., Soper N.J. Laparoscopic treatment of celiac artery compression syndrome: case series and review of current treatment modalities. Journal of Gastrointestinal Surgery. 2009;13(2):293–298. doi: 10.1007/s11605-008-0702-9. [DOI] [PubMed] [Google Scholar]
- 9.Grotemeyer D., Duran M., Iskandar F., Blondin D., Nguyen K., Sandmann W. Median arcuate ligament syndrome: vascular surgical therapy and follow-up of 18 patients. Langenbeck's Archives of Surgery. 2009;394(6):1085–1092. doi: 10.1007/s00423-009-0509-5. [DOI] [PubMed] [Google Scholar]
- 10.Park C.M., Chung J.W., Kim H.B., Shin S.J., Park J.H. Celiac axis stenosis: incidence and etiologies in asymptomatic individuals. Korean Journal of Radiology. 2001;2(1):8–13. doi: 10.3348/kjr.2001.2.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipshutz B. A composite study of the coeliac axis artery. Annals of Surgery. 1917;65(2):159–169. doi: 10.1097/00000658-191702000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petrella S., Prates J.C. Celiak trunk compression syndrome. A review. International Journal of Morphology. 2006;24(3):429–436. [Google Scholar]
- 13.Duffy A.J., Panait L., Eisenberg D., Bell R.L., Roberts K.E., Sumpio B. Management of median arcuate ligament syndrome: a new paradigm. Annals of Vascular Surgery. 2009;23(6):778–784. doi: 10.1016/j.avsg.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Sartor R. Elsevier; Edinburgh: 2003. Microbial influences in inflammatory bowel disease: role in pathogenesis and clinical implications. [Google Scholar]
- 15.Greenstein A.J., Janowitz H.D., Sachar D.B. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine. 1976;55(5):401–412. doi: 10.1097/00005792-197609000-00004. [DOI] [PubMed] [Google Scholar]


