Abstract
CONTEXT:
Recurrent miscarriages, the loss of three or more consecutive intrauterine pregnancies before 20 weeks of gestation with the same partner, affect 1%–1.5% of the pregnant population. The inadequate secretion of progesterone in early pregnancy has been proposed as a cause of recurrent miscarriages.
AIMS:
The aim was to investigate the efficacy of progesterone supplementation in patients with unexplained recurrent miscarriages.
SETTINGS AND DESIGN:
This was a 9-year cohort study of women with otherwise unexplained recurrent miscarriages who attended a recurrent miscarriage clinic in a tertiary care university hospital.
SUBJECTS AND METHODS:
Women with at least three unexplained recurrent miscarriages were included in the study. They were divided into three groups according to their initial and 48-h repeat progesterone levels. For women with inadequate endogenous progesterone secretion, natural progesterone vaginal pessaries 400 mg 12-hourly were offered until 12 weeks gestation.
STATISTICAL ANALYSIS:
Proportions and 95% confidence intervals calculated for categorical variables and the chi-square test were used to show statistical significance. Medians and ranges were calculated for noncontinuous variables.
RESULTS:
Pregnancy cycles (n = 203) were analyzed to examine the miscarriage rate following progesterone supplementation. Overall live birth and miscarriage rates were 63% and 36%, respectively. When analyzed by the number of previous miscarriages there was a reduction in the miscarriage rate following progesterone supplementation in women with 4 previous miscarriages when compared with historical data.
CONCLUSIONS:
Progesterone supplementation may have beneficial effects in women with otherwise unexplained recurrent miscarriages.
KEY WORDS: Live birth rate, miscarriage rate, progesterone vaginal pessaries, recurrent miscarriage
INTRODUCTION
Recurrent miscarriages, the loss of three or more consecutive intrauterine pregnancies before 20 weeks of gestation with the same partner, affect 1%–1.5% of the pregnant population.[1,2] The pathophysiology of recurrent miscarriages is incompletely understood and despite investigation, no cause is found in more than 50% of cases.[1,3] Management is distressing for patients and frustrating for the physician. With a limited understanding of the etiology, no specific treatment regimens can be offered, though several therapies with varying degrees of success have been proposed to prevent this condition.[4–6]
Progesterone maintains the early pregnancy and is mainly secreted by the corpus luteum during pregnancy.[7,8] Insufficient progesterone secretion and delayed endometrial development at the time of implantation or during early pregnancy may occur naturally or due to luteal phase defect and has been implicated as a cause of sporadic and recurrent miscarriages.[9–11]
If progesterone supplementation reduces the risk of repeat miscarriage, the scientific basis for its use may be related in part to its role in the regulation of inflammatory mediators in pregnancy.[12] Progesterone deficiency leads to increased levels of pro-inflammatory interleukin 8 (IL-8), cyclo-oxygenase-2, and monocyte chemoattractant protein-1 which destabilize the endometrium.[13] Successful pregnancy is associated with the downregulation of pro-inflammatory T helper cell type 1 (Th-1) cytokines and upregulation of anti-inflammatory T helper cell type 2 (Th-2) cytokines. A 34-kDa protein, progesterone-induced blocking factor (PIBF) prevents inflammatory reactions by blocking Th-1 cytokines and natural killer cells degranulation and increasing asymmetric nontoxic blocking antibodies.[14,15]
The paucity of good quality clinical studies drives skepticism among clinicians about the role of progesterone to treat recurrent miscarriages, though a meta-analysis of the available (poor quality) trials is quite favorable.[16] A large randomized controlled trial is underway in the UK to address this but results are not expected for at least 2 years (ISRCTN 92644181; full protocol is available at www.hta.ac.uk/project/1764.asp). Meanwhile, we present data from our experience of progesterone supplementation in women with otherwise unexplained recurrent miscarriages who had suboptimal progesterone secretion in early pregnancy.
SUBJECTS AND METHODS
This was a retrospective cohort study of women with recurrent miscarriages who attended our clinic over 9 years and who in the index pregnancy were noted to have subnormal early pregnancy progesterone secretion. Ethical approval was not required because there was no direct contact with the study population.
For all these women, prior to the index pregnancy, the following investigations were undertaken: follicle stimulating hormone (FSH), luteinizing hormone (LH), thrombophilia screen, autoimmune antibodies, thyroid function tests, vaginal ultrasound scan, and, if indicated, hysterosalpingography or hysteroscopy to rule out uterine anomalies. All women and their partners had karyotype examination. Women with three or more unexplained miscarriages were included; women with a recognized cause of recurrent miscarriages or a structural uterine abnormality distorting the cavity were excluded.
Early pregnancy surveillance was offered to all women with recurrent miscarriages in the form of initial and repeat (48 h later) serum progesterone. Women were advised to contact the clinic on the day of or the next day after the urinary pregnancy test was positive for progesterone measurement. A transvaginal ultrasound scan was performed at 6-week gestation and again 2–3 weeks later when patients with ongoing intrauterine pregnancies were referred to an antenatal clinic.
The outcome for women was analyzed according to progesterone levels. Group I included women whose initial serum progesterone level was <40 nmol/L (≤12.6 ng/mL, 1 nmol/L = 0.318 ng/ml). Group II included women whose initial progesterone level was ≥40 nmol/L but rose by less than 15% after 48 h. Group III included women with an initial progesterone level of ≥40 nmol/L and rose by more than 15% after 48 h. Progesterone supplementation was offered to all women in Groups I and II. Cyclogest® (Actavis, Barnstaple, UK) natural progesterone vaginal pessaries, 400 mg 12-hourly until the 12th week of pregnancy were offered. Group III with normal progesterone levels was not included in the analysis.
The threshold for the diagnosis of progesterone insufficiency is based partly on published data[17] showing levels of progesterone less than 40 nmol/L being associated with miscarriage, and on our own (unpublished) data (in ultimately successful pregnancies and a history of recurrent miscarriage, 95% of progesterone concentrations at all gestations from 5-12 weeks exceeded to 40 nmol/L).
A progesterone level of <20 nmol/L has a high positive predictive value for failing pregnancies.[18] However, viable pregnancies have been reported with initial progesterone levels of <15.9 nmol/L (5 ng/mL).[19] Defining a discriminatory value using a single serum progesterone result is not helpful and at least two measurements are required. We chose the value of a 15% rise after 48 h based on our laboratory's data suggesting that a rise of 15% in the analyzed sample is required to be confident about the fact that a true rise in the progesterone level has actually occurred.
The assessment of initial and 48 h repeat serum progesterone levels was designed to evaluate suboptimal progesterone secretion by the corpus luteum of early pregnancy, which may be due to unexplained causes or luteal phase defect. Progesterone supplementation was started only in early pregnancy once suboptimal progesterone secretion was confirmed. Serum progesterone levels were not checked after progesterone supplementation because 400 mg twice daily natural progesterone vaginal pessaries have previously been shown to be adequate to maintain the serum progesterone levels to support the early pregnancy.[20]
The end-point of the study was clinical pregnancy rate (by 10 weeks or more), calculating the number of women with ongoing pregnancy and miscarriage rate by calculating the proportions and 95% confidence intervals. When appropriate, the chi-square test was used to test significance of proportions. Medians and ranges were calculated for noncontinuous variables.
RESULTS
A total of 213 pregnancy cycles were analyzed; according to the initial and 48-h repeat serum progesterone levels, there were 31 (15%), 175 (82%), and 7 (3%) patients in the three groups, respectively. Overall, the median age of the women was 36 years (range 20–45) and the median number of miscarriages was 4 (range 3–9). There were 3 (1.4%) ectopic pregnancies and 1 (0.5%) still birth during the study period. Women in Group III (n = 7) and women with ectopic pregnancies (n = 3) were not included in the final analysis. This left 203 pregnancy cycles to be analyzed to examine the efficacy of progesterone supplementation.
The live birth rate and repeat miscarriage rate after progesterone supplementation was 63% (95% CI 56%–70%) and 36% (95% CI 30%–43%), respectively. There was no difference (χ2 test, P = 0.387) in the repeat miscarriage rate in women with or without a previous live birth (33% vs. 39%, respectively).
Table 1 shows the risk of subsequent miscarriage rate after progesterone supplementation according to the number of previous miscarriages. According to the number of previous miscarriages, there was no difference between the ages of women in three different groups. The mean age of women was 35 (±5.4), 36 (±5.4), and 36 (±5.4) years, and the average number of miscarriages was 3, 4, and 5.6 in patients with previous 3, 4, and 5, or more than 5 miscarriages, respectively.
Table 1.
Risk of repeat miscarriage after progesterone supplementation
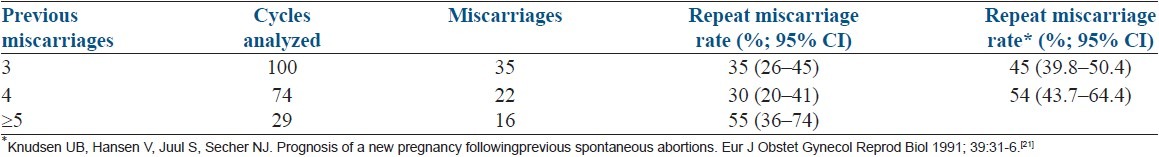
In the absence of a control group, we compared our data with similar historical data which showed subsequent miscarriage rates of 45% (95% CI 40–50) and 54% (95% CI 44–64) in women with previous three and four miscarriages, respectively.[21] In comparison with these data, our results demonstrated a reduction in the subsequent miscarriage rate in women with previous three miscarriages (35% vs. 45%) but the confidence limits overlapped (hence not likely to be statistically significant), while for women with previous four miscarriages, there was a further reduction in miscarriage rates (30% vs. 54%) with no confidence limit overlap (suggesting statistical significance).
DISCUSSION
The study of treatments for recurrent miscarriages is fraught due to the desperation of the patients and the wide range of unaccredited treatments. This study has particular flaws, but reports on experience of practice in one unit with homogenous treatment policies managed by one individual (DJC). The RCTs published in the Cochrane database on recurrent miscarriage illustrate this difficulty;[22] papers were published many years ago or had peculiar methodology (e.g., late recruitment – less than 10% receiving any intervention before 7 weeks gestation).[23] The data we used as our comparative control are relatively unique in that they represent an unselected population cohort (approximately, 300,500 pregnancies) in the Danish population.[21]
The protective effect of previous live birth on the occurrence of repeat miscarriage in the future is not very clear and studies have shown different results.[24,25] We have not observed a protective effect of previous live birth on future pregnancy loss.
Progesterone has been used in different routes and doses to prevent miscarriage in early to mid-pregnancy. Although some early reports of progesterone use showed an improved outcome,[26] however, later studies showed conflicting results of beneficial effects of progesterone.[11,27] El-Zibdeh showed that oral dydrogesterone reduced recurrent miscarriage but the methodology in the paper is flawed due to the randomization and no proper concealment.[23]
Progesterone is an important pregnancy hormone and despite its longstanding use to treat recurrent miscarriages, insufficient data exist to support its widespread use. Most (90%) UK physicians remain unconvinced of any beneficial effects without a placebo-controlled randomized trial.[16] Two randomized controlled trials of progesterone supplementation for recurrent miscarriage are awaited (20 mg oral dydrogesterone versus placebo for recurrent miscarriage; clinical trial number: NCT00193674; Cyclogest vaginal pessaries versus placebo, PROMISE study ISRCTN 92644181). These studies may provide clearer evidence for the role of progesterone in recurrent miscarriage management.
CONCLUSION
Considering that progesterone has important immunomodulatory functions by decreasing proinflammatory and increasing anti-inflammatory cytokines in early pregnancy, progesterone's role in maintaining early pregnancy is crucial. This study provides support that progesterone supplementation reduces the subsequent miscarriage rate in patients with unexplained recurrent miscarriages in comparison with historical data. Although this study is limited by having no control group, the results contribute to the existing body of the literature on this subject which claims that progesterone supplementation may improve the pregnancy outcome in selected groups of unexplained recurrent miscarriages.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Stirrat GM. Recurrent miscarriage. Lancet. 1990;336:673–5. doi: 10.1016/0140-6736(90)92159-f. [DOI] [PubMed] [Google Scholar]
- 2.Washington DC: American College of Obstetricians and Gynaecologists; 1995. American College of Obstetricians and Gynaecologists (ACOG), early pregnancy loss ACOG technical bulletin No. 212. [Google Scholar]
- 3.Quenby SM, Farquharson RG. Predicting recurring miscarriage: What is important? Obstet Gynecol. 1993;82:132–8. [PubMed] [Google Scholar]
- 4.Tempfer CB, Kurz C, Bentz EK, Unfried G, Walch K, Czizek U, et al. A combination treatment of prednisone, aspirin, folate and progesterone in women with idiopathic recurrent miscarriage: A matched-pair study. Fertil Steril. 2006;86:145–8. doi: 10.1016/j.fertnstert.2005.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2003;(1):CD000112. doi: 10.1002/14651858.CD000112. [DOI] [PubMed] [Google Scholar]
- 6.Rai R, Backos M, Baxter N, Chilcott I, Regan L. Recurrent Miscarriage-an aspirin a day? Hum Reprod. 2000;15:2220–3. doi: 10.1093/humrep/15.10.2220. [DOI] [PubMed] [Google Scholar]
- 7.Arredondo F, Noble LS. Endocrinology of recurrent pregnancy loss. Semin Reprod Med. 2006;24:33–9. doi: 10.1055/s-2006-931799. [DOI] [PubMed] [Google Scholar]
- 8.Di Renzo GC, Mattei A, Gojnic M, Gerli S. Progesterone and pregnancy. Curr Opin Obstet Gynecol. 2005;17:589–600. doi: 10.1097/01.gco.0000191899.84567.4d. [DOI] [PubMed] [Google Scholar]
- 9.Insler V. Corpus luteum defects. Curr Opin Obstet Gynecol. 1992;4:203–11. [PubMed] [Google Scholar]
- 10.Daya S. Issues in the etiology of recurrent spontaneous abortion. Curr Opin Obstet Gynecol. 1994;6:153–9. [PubMed] [Google Scholar]
- 11.Daya S. Efficacy of progesterone support for pregnancy in women with recurrent miscarriage. A meta-analysis of controlled trials. Br J Obstet Gynaecol. 1989;96:275–80. doi: 10.1111/j.1471-0528.1989.tb02386.x. [DOI] [PubMed] [Google Scholar]
- 12.Daya S, Ward S, Burrows E. Progesterone profiles in luteal phase defect cycles and outcome of progesterone treatment in patients with recurrent spontaneous abortion. Am J Obstet Gynecol. 1988;158:225–32. doi: 10.1016/0002-9378(88)90127-5. [DOI] [PubMed] [Google Scholar]
- 13.Critchley HO, Jones RL, Lea RG, Drudy TA, Kelly RW, Williams AR, et al. Role of inflammatory mediators in human endometrium during progesterone withdrawal and early pregnancy. J Clin Endocrinol Metab. 1999;84:240–8. doi: 10.1210/jcem.84.1.5380. [DOI] [PubMed] [Google Scholar]
- 14.Raghupathy R. Pregnancy: Success and failure within the Th1/Th2/Th3 paradigm. Semin Immunol. 2001;13:219–27. doi: 10.1006/smim.2001.0316. [DOI] [PubMed] [Google Scholar]
- 15.Raghupathy R, Al-Mutawa E, Al-Azemi M, Makhseed M, Azizieh F, Szekeres- Bartho J. Progesterone-induced blocking factor (PIBF) modulates cytokine production by lymphocytes from women with recurrent miscarriage or preterm delivery. J Reprod Immunol. 2009;80:91–9. doi: 10.1016/j.jri.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Coomarasamy A, Truchanowicz EG, Rai R. Does first trimester progesterone prophylaxis increase the live birth rate in women with unexplained recurrent miscarriages? BMJ. 2011;342:d1914. doi: 10.1136/bmj.d1914. [DOI] [PubMed] [Google Scholar]
- 17.Banerjee S, Aslam N, Zosmer N, Woelfer B, Jurkovic D. The expectant management of women with early pregnancy of unknown location. Ultrasound Obstet Gynecol. 1999;14:231–6. doi: 10.1046/j.1469-0705.1999.14040231.x. [DOI] [PubMed] [Google Scholar]
- 18.Banerjee S, Aslam N, Woelfer B, Lawrence A, Elson J, Jurkovic D. Expectant management of early pregnancies of unknown location: A prospective evaluation of methods to predict spontaneous resolution of pregnancy. BJOG. 2001;108:158–63. doi: 10.1111/j.1471-0528.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 19.Green-Top guideline no. 25. The management of early pregnancy loss. London: RCOG Press; 2006. Royal College of Obstetricians and Gynaecologists (RCOG) [Google Scholar]
- 20.Joels JA, Watt EM, Wardle PG. Pilot study of continuous combined HRT using vaginal Crinone on alternate days or twice weekly. J Brit Men Soc. 1998;4(Suppl 1):19. [Google Scholar]
- 21.Knudsen UB, Hansen V, Juul S, Secher NJ. Prognosis of a new pregnancy following previous spontaneous abortions. Eur J Obstet Gynecol Reprod Biol. 1991;39:31–6. doi: 10.1016/0028-2243(91)90138-b. [DOI] [PubMed] [Google Scholar]
- 22.Haas DM, Ramsey PS. Progestogen for preventing miscarriage. Cochrane Database Syst Rev. 2008;(2):CD003511. doi: 10.1002/14651858.CD003511.pub2. [DOI] [PubMed] [Google Scholar]
- 23.El-Zibdeh MY. Dydrogesterone in the reduction of recurrent spontaneous abortion. J Steroid Biochem Mol Biol. 2005;97:431–4. doi: 10.1016/j.jsbmb.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Roman EA, Alberman E, Pharoah PO. Pregnancy order and reproductive loss. Br Med J. 1980;280:715. doi: 10.1136/bmj.280.6215.715-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clifford K, Rai R, Regan L. Future pregnancy outcome in unexplained recurrent first trimester miscarriage. Hum Reprod. 1997;12:387–9. doi: 10.1093/humrep/12.2.387. [DOI] [PubMed] [Google Scholar]
- 26.Tho SP, Reindollar RH, McDonough PG. Recurrent abortion. Obstet Gynecol Annu. 1983;12:259–81. [PubMed] [Google Scholar]
- 27.Goldstein P, Berrier J, Rosen S, Sacks HS, Chalmers TC. A meta-analysis of randomized control trials of progestational agents in pregnancy. Br J Obstet Gynaecol. 1989;96:265–74. doi: 10.1111/j.1471-0528.1989.tb02385.x. [DOI] [PubMed] [Google Scholar]


