Abstract
Cystic adenomyosis is a rare form of adenomyosis mostly seen in middle aged women.We report two cases of cystic adenomyosis in juvenile patients, which simulate uterine malformation and presented as a diagnostic dilemma. The first patient initially was diagnosed as uterus bicornis with a hematometra in obstructed rudimentary horn while the second patient was diagnosed as broad ligament fibroid. Surgical exploration by laparoscopic approach confirmed the diagnosis and excision of the cystic mass relieved the symptoms of the patients.
KEY WORDS: Adult cystic adenomyoma, juvenile cystic adenomyoma, mullerian duct anomalies, uterine bicornis
INTRODUCTION
Adenomyomas are uncommon tumors of the uterus, composed of smooth muscle fibers and endometrial glands. Etiology is still unknown and myometrium is invaded by the endometrium. It mainly affects perimenopausal women[1,2] and usually appears as a diffuse disease, but may also occur as a focal lesion.[3] The juvenile form is seen in 13 to 20 years age group patients and its true incidence is unknown. Till now, only less than ten cases have been reported in the literature. Its location is frequently intramural and few millimeters in diameter.[4] Cystic degeneration is often seen in a leiomyoma, but is reported rarely in adenomyoma. In differential diagnosis of juvenile cystic adenomyosis, exclusion of mullerian duct anomalies such as rudimentary horn with uterine unicornis is very important and conventional hysterosalpingography or MRI are highly sensitive in confirmation of the diagnosis. In this paper, two rare cases of juvenile cystic adenomyosis are presented, in which diagnostic dilemma was there till the laparoscopy was performed; because even magnetic resonance imaging (MRI) proved unsatisfactory in confirmation of the diagnosis and in the other case laparoscopy in inexperienced hands provide the diagnosis of broad ligament fibroid.
CASE REPORTS
Case 1
A 19-year-old unmarried girl presented to us with the complaint of severe dysmenorrhea and menorrhagia for last three months; refractory to any medication. The pain was colicky in nature associated with menstruation and so severe in intensity that incapacitates her routine activities. The pain was not associated with gastrointestinal or urinary symptoms. At consultation in other hospital, she was treated with Oral contraceptive pills (OCP's) and Non steroidal anti-inflammatory drugs (NSAID's); but not relieved. On transabdominal ultrasonography, she was diagnosed as the case of uterine bicornis with a hematometra in obstructed rudimentary horn [Figure 1]. Even MRI findings were suggestive of uterine bicornis with right horn hematometra [Figure 2]. With these findings, patient was referred to our laparoscopy center and laparoscopy was performed on her. A primary umbilical 12 mm port and three 5 mm ancillary ports were created. On inserting the laparoscope; uterus was found to be enlarged asymmetrically, marked globular on left anterior wall, below the cornual end, near attachment of round ligament. No other uterine horn could be seen. Bilateral fallopian tubes and ovaries were normal in appearance. On hysteroscopy, uterine cavity was normal sized and bilateral ostia were seen normally. Diluted vasopressin was injected into the swelling [Figure 3]. A transverse incision was given on anterior uterine surface over the swelling with the harmonic scalpel. When the incision reached the cystic cavity, thick chocolate material was drained [Figure 4] and endometriotic cyst lining was removed with the harmonic scalpel [Figure 5]. There was no direct communication between the uterine cavity and cyst. Uterine cavity was not entered. The defect was closed meticulously with vicryl 1-0 in three layers [Figure 6].
Figure 1.
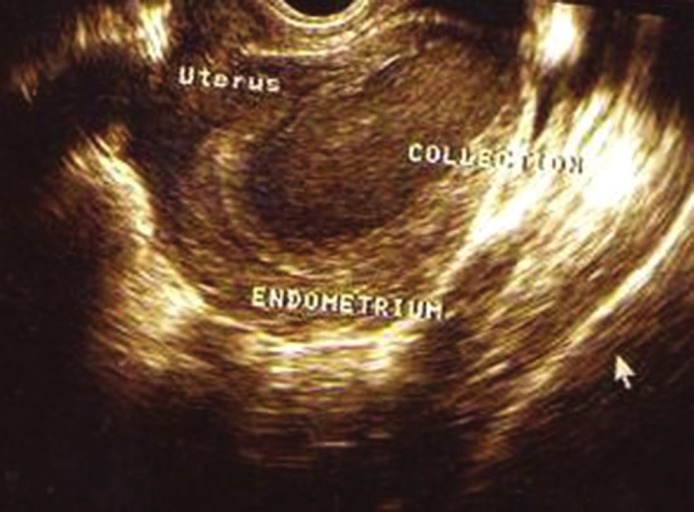
Case 1: USG showing endometrial collection
Figure 2.

MRI showing uterus bicornis with right horn hematometra
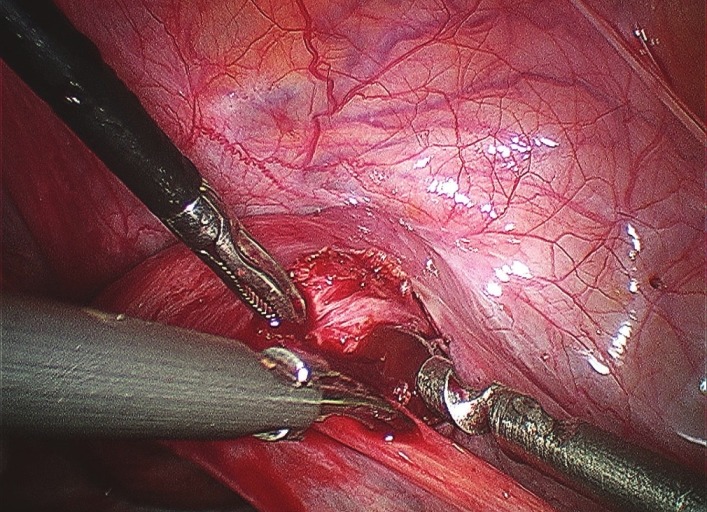
Figure 3.
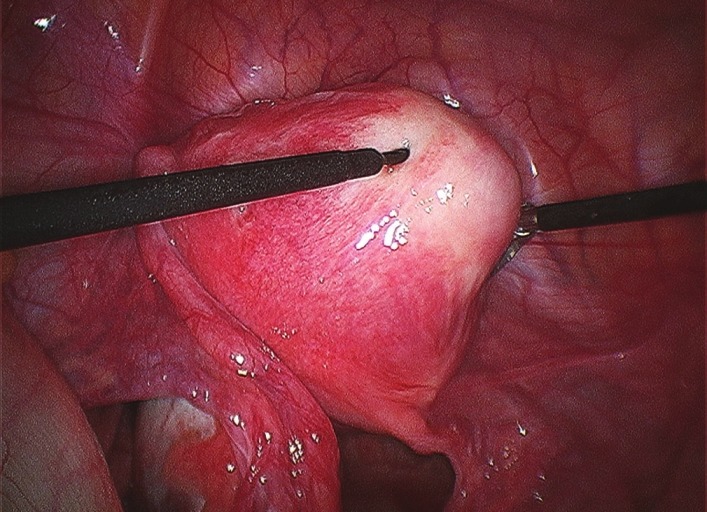
Pitressin injected over cystic adenomyoma
Figure 4.
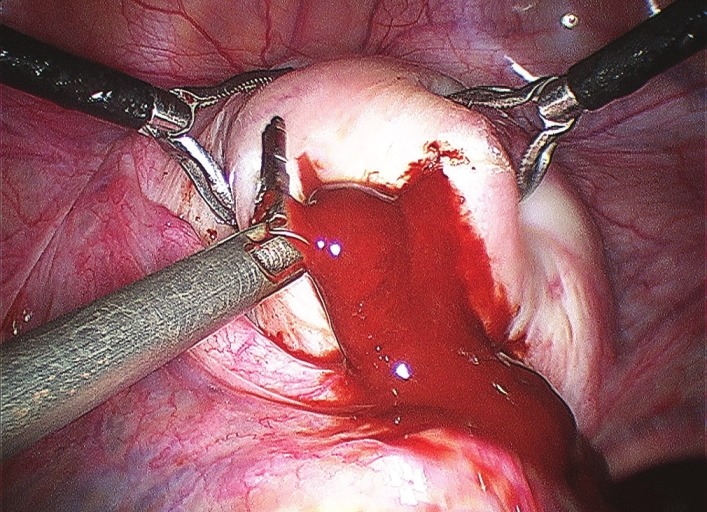
Chocolate material drained from cystic adenomyoma
Figure 5.
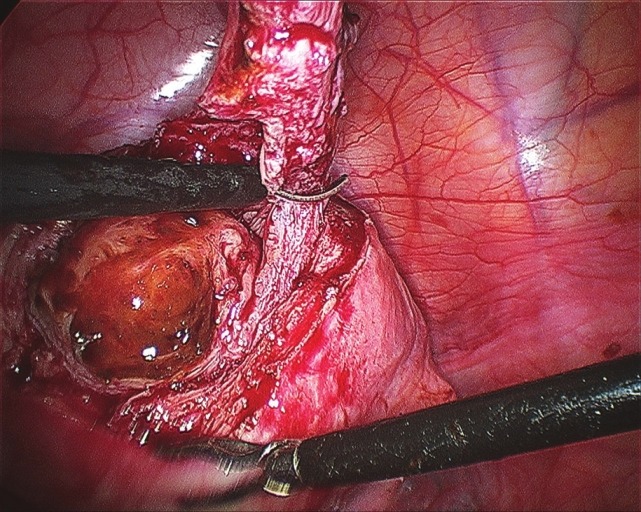
Cyst wall enucleated
Figure 6.
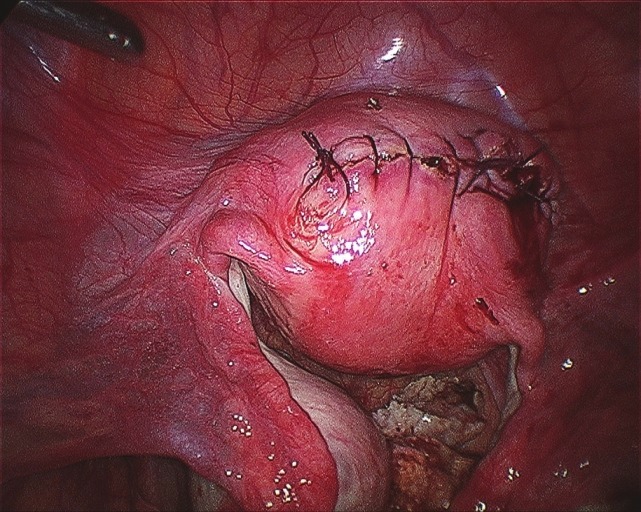
Defect closed meticulously in three layers
There were no intraoperative or postoperative complications. The patient was discharged next day after surgery. Postoperatively, GnRH agonist treatment was extended for 2 months. When the menstrual cycle returned, the patient did not experience dysmenorrhea.
Case 2
A 22-year-old female P1+1 presented with the complaint of severe dysmenorrhea, menorrhagia and secondary infertility for two years. At consultation in other hospital, diagnostic laparoscopy was performed and she was diagnosed as having broad ligament fibroid and referred to our laparoscopy center. Transvaginal ultrasonography was suggestive of cystic mass in uterus with mixed echogenicity. On performing the laparoscopy, endometriotic implants were found on bilateral ovaries and uterosacral ligaments which were fulgurated with the bipolar cautery. Uterine veins were tortuous and forming the plexus in the broad ligament. A cystic swelling was noted on the anterior surface on right side of uterus below the round ligament. Diluted vasopressin (Pitressin, 5 units in 100 ml of normal saline) was injected into the cystic swelling. A transverse incision was given on the anterior surface of swelling with the harmonic scalpel. When the incision reached the cystic cavity, thick chocolate material was drained [Figure 7] and the defect was closed with vicryl 2-0, meticulously [Figure 8]. Good approximation was achieved. There were no intraoperative or postoperative complications. The patient was discharged next day after surgery.
Figure 7.
Case 2: Incision over cystic swelling- chocolate material drained
Figure 8.
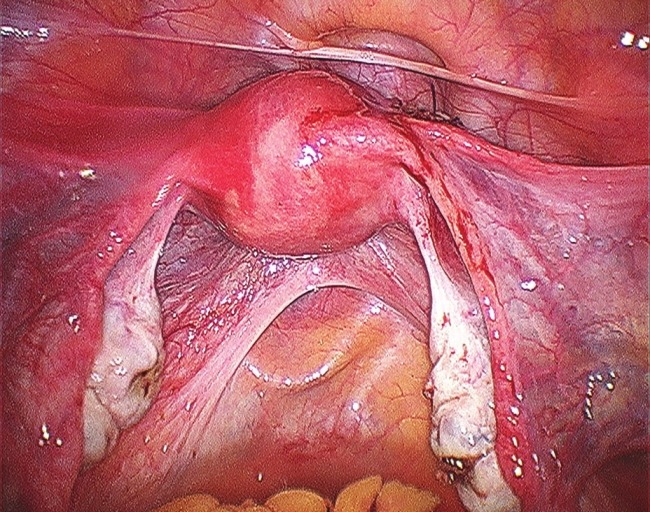
Defect closed meticulously in three layers
DISCUSSION
Cyst within the myometrium is a rare finding, and cystic adenomyoma is one such disorder.[5] Based on the patient's age at symptom development, these lesions are classified into juvenile cystic adenomyoma and adult cystic adenomyoma. Adult cystic adenomyoma shows clinical features similar to those of common adenomyosis, which is usually found in multiparous women over age 30,[6] and is considered a rare variant of adenomyosis characterized by the presence of a hemorrhagic cyst resulting from menstrual bleeding in the ectopic endometrial gland.[3] However, juvenile cystic adenomyoma has different clinical characteristics than those in adult cystic adenomyoma.[7,8]
The pathognomonic clinical feature of juvenile cystic adenomyoma is its early onset of severe dysmenorrhea that usually starts with menarche. This symptom could be attributed to intracystic bleeding and stretching of the cystic cavity.[7] Medical treatment with GnRH agonist only provide temporary relief, symptoms resumed with the return of menstruation. Therefore, surgical intervention was required in these juvenile cases with sever dysmenorrhea, refractory to any treatment.
When diagnosing juvenile cystic adenomyoma, exclusion of known mόllerian duct anomalies such as non-communicating rudimentary horn with uterine unicornis is most important. For this purpose, conventional Hystero-salpingography (HSG) is useful. In cases with a non-communicating rudimentary horn, the fallopian tube on the affected side is not visualized on HSG, while in cases of cystic adenomyoma, the bilateral tubes appear normal. But use of the conventional HSG in unmarried patients is limited; so laparoscopic surgery should be chosen as minimally invasive procedure for these young women, if available.
Further, early occurrence of the symptoms soon after menarche suggests that juvenile cystic adenomyoma is a congenital malformation caused by a defect in the developmental process of mόllerian ducts. The most common location of this lesion is the anterior wall of the uterus at the level of insertion of the round ligament.[9] Accessory uterine mass could be caused by duplication and persistence of ductal mόllerian tissue in a critical area at the attachment level of the round ligament, possibly related to a gubernaculum dysfunction. This is the location we have found in our both patients, on anterior surface of the uterus near cornual end; just at the level of insertion of round ligament. The actual incidence of juvenile cystic adenomyoma is unknown at present. There is a possibility that these juvenile lesions were previously diagnosed as uterine anomalies, especially non-communicating rudimentary horn with uterine unicornis. However, with advances in diagnostic procedures and increasingly widespread knowledge of juvenile cystic adenomyoma, this disease is expected to be recognized more frequently and properly treated.
CONCLUSION
Noncommunicating accessory uterine cavities and isolated cystic adenomyomas correspond to the same pathology: cavitated accessory uterine mass associated with an otherwise normal uterus. They present problems of differential diagnosis with true cavitated adenomyomas and cavitated rudimentary uterine horns. Conventional HSG and MRI are helpful in providing a clue toward the correct diagnosis but laparoscopy in the hands of experienced surgeon is the only confirmatory option for such rare disorders.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Azziz R. Adenomyosis: Current perspectives. Obstet Gynecol Clin North Am. 1989;16:221–35. [PubMed] [Google Scholar]
- 2.Troiano RN, Flynn SD, McCarthy S. Cystic adenomyosis of the uterus: MRI. J Magn Reson Imaging. 1998;8:1198–202. doi: 10.1002/jmri.1880080603. [DOI] [PubMed] [Google Scholar]
- 3.Tamai K, Koyama T, Umeoka S, Saga T, Fujii S, Togashi K. Spectrum of MR features in adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20:583–602. doi: 10.1016/j.bpobgyn.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Slezak P, Tillinger KG. The incidence and clinical importance of hysterographic evidence of cavities in the uterine wall. Radiology. 1976;118:581–6. doi: 10.1148/118.3.581. [DOI] [PubMed] [Google Scholar]
- 5.Buerger PT, Petzing HE. Congenital cysts of the corpus uteri. Am J Obstet Gynecol. 1954;67:143–51. doi: 10.1016/0002-9378(54)90205-7. [DOI] [PubMed] [Google Scholar]
- 6.Kataoka ML, Togashi K, Konishi I, Hatabu H, Morikawa K, Kojima N, et al. MRI of adenomyotic cyst of the uterus. J Comput Assist Tomogr. 1998;22:555–9. doi: 10.1097/00004728-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Tamura M, Fukaya T, Takaya R, Ip CW, Yajima A. Juvenile adenomyotic cyst of the corpus uteri with dysmenorrhea. Tohoku J Exp Med. 1996;178:339–44. doi: 10.1620/tjem.178.339. [DOI] [PubMed] [Google Scholar]
- 8.Nabeshima H, Murakami S, Terada Y, Noda T, Yaegashi N, Okamura K. Total laparoscopic surgery of cystic adenomyoma under hydroultrasonographic monitoring. J Am Assoc Gynecol Laparosc. 2003;10:195–9. doi: 10.1016/s1074-3804(05)60298-8. [DOI] [PubMed] [Google Scholar]
- 9.Acien P, Acien M, Fernandez F, Jose Mayol M, Aranda I. The cavitated accessory uterine mass: A müllerian anomaly in women with an otherwise normal uterus. Obstet Gynecol. 2010;116:1101–9. doi: 10.1097/AOG.0b013e3181f7e735. [DOI] [PubMed] [Google Scholar]


