Abstract
Background:
Sleep disturbances are common among uremic patients; however, limited data are available on predictors of sleep quality in this population. We assessed sleep quality in patients on hemodialysis (HD) and peritoneal dialysis (PD) and investigated predictors related to sleep quality.
Methods:
Patients on maintenance HD and PD were consecutively included from two medical centers in Isfahan city (Iran). They completed the Pittsburgh sleep quality index (PSQI) and hospital anxiety and depression scale. Laboratory tests were done for iron state, kidney function, and electrolytes. Univariate and multivariate analyses were performed to find predictors of sleep quality.
Results:
About 90 patients were evaluated (53 males, age = 54.2 ± 15.2 years, disease duration = 5.3 ± 4.5 years). Poor sleep quality was frequent in 86.6% of the cases in each group of HD and PD patients. Patients on HD had poorer sleep quality in terms of total PSQI scores and two dimensions of sleep latency and sleep efficiency (P < 0.05). Anxiety (β = 0.232, P = 0.027), depression (β = 0.317, P = 0.004), and being on HD (β = 2.095, P = 0.009) were independent predictors of overall poor sleep quality.
Conclusions:
Poor sleep quality is highly frequent in patients on maintenance dialysis and mood disorders and being on HD are predictive factors. Further studies are required for better understanding of risk factors associated with poor sleep quality and thus possible treatments in these patients.
Keywords: End-stage renal disease, hemodialysis, peritoneal dialysis, risk factors, sleep disorders
INTRODUCTION
Various types of sleep disturbances are common among patients with end-stage renal disease (ESRD), ranging from 50% to 80% by subjective manner and in up to 50% of the cases as objectively documented with polysomnography.[1,2] Frequent sleep disorders in patients on hemodialysis (HD) and peritoneal dialysis (PD) include sleep apnea syndrome, restless legs syndrome, and periodic limb movement disorder.[2,3] The etiology of sleep disorders in patients on dialysis is not completely discovered; however, it is known to be multi-factorial. Various conditions, including dialysis, medications, metabolic abnormalities, malnutrition, fatigue, muscle cramps, peripheral neuropathy, and emotional problems, all common in ESRD patients, can have effects on development of sleep disturbances in these patients.[1,2,4,5]
The presence of sleep disorder is associated with lower quality of life and higher mortality in patients on dialysis.[5–7] Thus, it is important to investigate the risk factors associated with sleep disorders and improve the quality of sleep in ESRD patients in order to increase patients’ quality of life and probably reduce associated mortality. Although separate studies have investigated the type and frequency of sleep disturbances in HD and PD patients, only few reports are available on the effects of dialysis type on sleep quality.[8–10] Furthermore, the results of previous studies on other risk factors have been controversial. Hence, we assessed sleep quality in patients on HD and PD and evaluated possible risk factors related to sleeping disturbances.
METHODS
Patients and settings
This cross-sectional study was conducted between January and December 2011 on adult patients with ESRD who were on maintenance HD or PD for at least 3 consecutive months in two academic medical centers in Isfahan city (Iran). Patients with a history of hospitalization within 4 weeks before the study were not enrolled. Consecutive sampling was done and with regard to the first type of error (α) = 0.05, study power = 80%, and minimum expected difference of 10% in the frequency of poor sleep quality between the HD and PD patients based on previous studies,[9] sample size was calculated as 45 cases in each group of the HD and PD patients. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences and an informed consent was obtained from all patients.
Assessments
Based on patients’ documents and during an interview with a trained resident of internal medicine, a questionnaire, including demographic, disease, and dialysis characteristics, sleep quality, and psychological factor (anxiety and depression) was completed with the following parts:
Pittsburgh sleep quality index
The Pittsburgh sleep quality index (PSQI) is an 18-item self-rated questionnaire for the evaluation of the overall sleep quality within the preceding month. PSQI evaluates seven components of sleep quality, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of medication for sleep, and daytime dysfunction due to poor sleep. Each component score is calculated and coded from 0 to 3, where 0 indicates “no difficulty,” and 3, “severe difficulty.” The global score ranges from 0 to 21, where scores of ≤5 indicate good sleep quality and scores of >5 indicates poor sleep quality.[11]
The hospital anxiety and depression scale
The hospital anxiety and depression scale (HADS) is a brief and widely used measure of psychological distress in outpatient setting. The HADS contains 14 items and consists of two sub scales of anxiety and depression. Each item is rated on a 4-point scale, giving a maximum score of 21 for each of the anxiety and depression sub scales. Scores of 11 or more on either sub scale are considered to be a significant “case” of psychological morbidity, while scores of 8-10 represents a “borderline” and 0-7 a “normal” case.[12,13] For the above-mentioned questionnaires, a linguistically validated and reliable Persian version was used in this study.[14,15]
Laboratory assessments
Patients were tested for complete blood counts, iron state with serum iron, ferritin, total iron binding capacity (TIBC), and transferrin (and saturation), albumin, electrolytes, including calcium and phosphorus, creatinine, blood urea nitrogen (BUN), and C-reactive protein (CRP). Fasting blood samples were taken in the morning in almost all patients when they came to the hospitals for dialysis session or for visits, and then were sent to one clinical laboratory for analyses. In those who came for dialysis session, blood samples were taken before the dialysis.
Data analyses
Data were analyzed using the SPSS software for windows (version 16.0, Chicago IL., USA). Comparisons between categorical variables were done using the Fisher's exact or Chi-square tests. Student's t-test and Mann–Whitney tests were used for comparison of parametric and non-parametric data, respectively. Multivariate regression analyses were also performed to find factors associated with sleep quality. Statistical significance was defined at the 95% level (P < 0.05). Because not all comparisons have a predefined 1-tailed hypothesis, we reported 2-tailed P values for all analyses.
RESULTS
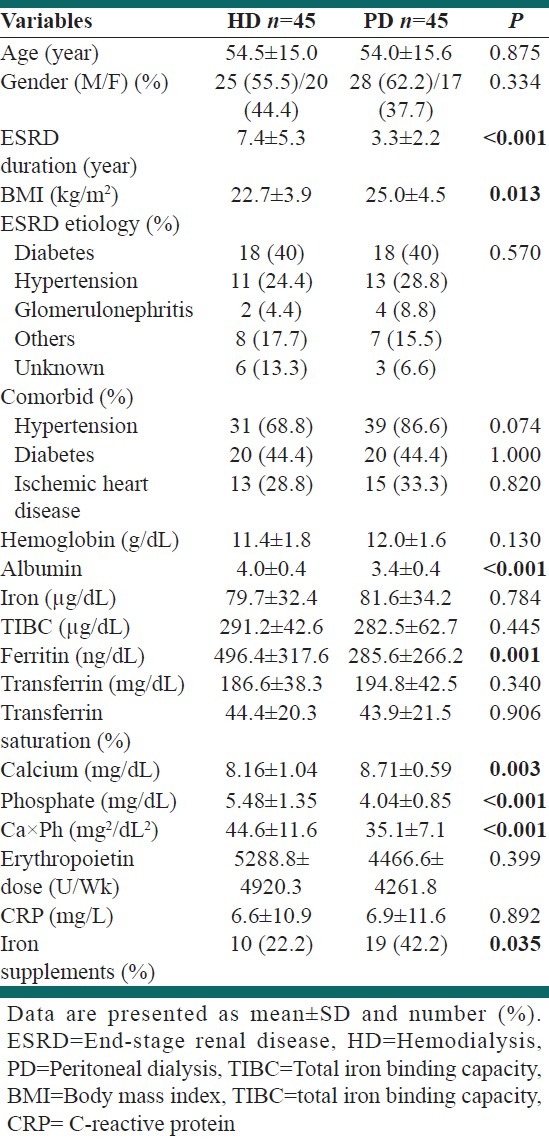
During the study period, 45 patients on HD and 45 patients on PD were evaluated including 53 males and 37 females with the mean age of 54.2 ± 15.2 years and disease duration of 5.3 ± 4.5 years. Demographic data, disease characteristics, and laboratory tests’ results of the patients are presented in Table 1. Compared with patients on PD, those who were on HD had longer disease duration (P < 0.001), lower body mass index (BMI) (P = 0.013), lower calcium (P = 0.003) and higher phosphate and calcium × phosphate product (P < 0.001), lower BUN (P = 0.044) and creatinine (P < 0.001), and higher albumin (P < 0.001) and ferritin levels (P = 0.001). Furthermore, patients on PD were under iron supplementation more frequently than HD patients (P = 0.035). Other variables were the same between the HD and PD patients.
Table 1.
Demographic, clinical, and laboratory characteristics of patients on hemodialysis and peritoneal dialysis
Psychological state and sleep quality
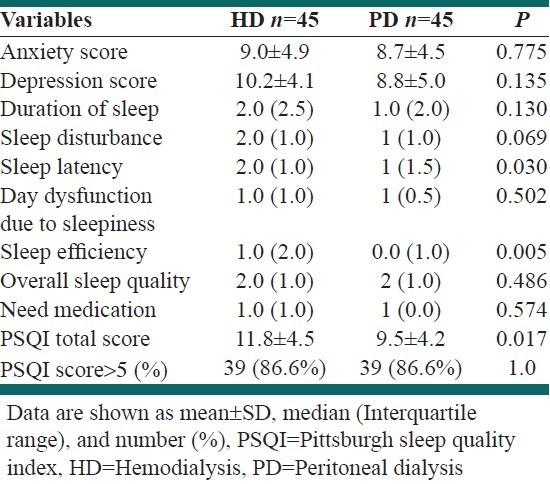
Comparisons of psychological state and sleep quality between the two groups of HD and PD patients are presented in Table 2. The two groups were not significantly different regarding anxiety or depression scores (P > 0.05). Poor sleep quality was frequent in 86.6% of the cases in each group. However, patients on HD had poorer sleep quality in terms of total PSQI scores and two dimensions of sleep latency and sleep efficiency (P < 0.05).
Table 2.
Comparison of psychological state and sleep quality components between the hemodialysis and peritoneal dialysis patients
Predictors of sleep quality
In univariate analyses, there was a significant association between anxiety/depression scores and PSQI total score (r = 0.463 and 0.478, respectively, P < 0.001). Age, gender, ESRD duration, comorbid diseases, or BMI were not significantly associated with PSQI total score, but there was a non-significant relationship between physical activity and total PSQI score (r = –0.198, P = 0.063). Physical activity was also significantly associated with sleep quality in terms of “day dysfunction due to sleepiness” (r = –0.429, P < 0.001). Scores of this component of sleep quality was also associated with CRP levels (r = 0.249, P = 0.019). Other laboratories tests results were not associated with PSQI total score or its components.
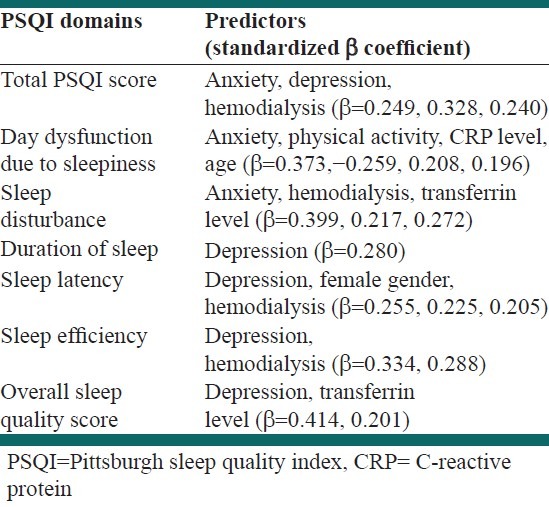
In multivariate analysis, with a stepwise model, anxiety (β = 0.232, P = 0.027), depression (β = 0.317, P = 0.004), and being on HD (β = 2.095, P = 0.009) were independent factors associated with overall poor sleep quality (total PSQI score). Predictors of sleep quality with regards to different PSQI domains are presented in Table 3. Mood disorders were independently associated with poor sleep quality in most of the PSQI domains.
Table 3.
Predictors of overall poor sleep quality and each Pittsburgh sleep quality index components based on stepwise logistic regression analysis
DISCUSSION
Sleep disturbances are common among ESRD patients and are associated with decreased quality of life and higher mortality rates.[5–7] Having knowledge about the risk factors of sleep disorders is helpful in designing preventive and therapeutic strategies for these patients. We evaluated the association of dialysis type (HD vs. PD) and other possible risk factors with sleep quality in patients on dialysis. The prevalence of poor sleep quality in our patients was similar to other reports from our society (87.8%).[16] Using the same sleep measure (PSQI), the frequency of poor sleep quality is reported from 57% to 88.5% in other societies.[9,17–19] This variation between different populations highlights the role of internal as well as external factors affecting the quality of sleep. Although previous studies evaluated different possible risk factors in patients on dialysis, only few of them included both HD and PD patients. Turkmen et al., found similar sleep quality scores between the HD and PD patients.[8] Another study in the same population (Turkey) also found a non-significant difference between the HD and PD patients in the frequency of poor sleep quality (88.5% vs. 78.0%).[9] The study by Holley et al., also did not found difference between HD and PD patients in the frequency or severity of sleep disturbances.[10] In our study, the overall frequency of poor sleep quality was similar between the HD and PD patients, but the total PSQI score was higher in the HD patients. This difference was confirmed by the multivariate analysis, controlling for different factors, which showed independent association of being on HD with poorer sleep quality. On the other hand, patients on PD had higher BMI, more frequent hypertension, and lower albumin and ferritin levels, and these factors are supposed to be associated with poor sleep quality based on some reports.[9,17,18,20,21] Regarding dialysis shift, Hsu et al., found a beneficial effect of evening HD, compared with morning and afternoon HD, on sleep quality and reduction of daytime symptoms,[22] while another study did not find an association in this regard.[23] Our sample was not large enough for such comparison as we only have one patient not receiving evening HD. Unfortunately, we did not have access to data on dialysis adequacy for all patients and precise analysis of such an association remains for future studies. Furthermore, in future studies other factors related to HD compared with PD must be considered as possible mechanisms by which patients on HD have poorer quality of sleep compared with patients on PD.
With regards to possible risk factors of poor sleep quality other than type of dialysis, similar to several other studies,[24–26] we found that mood disorders (anxiety and depression) are important factors independently associated with sleep quality. Mood disorders are highly prevalent in patients on dialysis, describing high prevalence of sleep disturbance in these patients.[27] Although mood disorders have direct effects on sleep disorders,[28] this association in ESRD patients may also be mediated by increased (neuro) inflammatory burden due to mood disorders resulting in other comorbidities such as cardiovascular and pulmonary disorders.[29] An association between age and sleep quality in ESRD patients is also reported by some studies.[18,25,30] In our study, however, age was independently associated with only one of the sleep quality domains, “day dysfunction due to sleepiness.” Although age is found to be independently associated with sleep quality, this association may be, at least in part, mediated by the presence of comorbid diseases, less physical activity, and nutritional status in older patients.[18,31–33] We also found female gender an independent predictor of sleep latency. Female gender was associated with poor sleep quality in one other study,[26] but the other one found an association between male gender and sleep quality.[34] While male gender is found to be associated with sleep apnea syndrome,[35,36] female gender is an independent risk factor for restless legs syndrome,[37,38] and both of these syndrome are common among dialysis patients and are associated with poor sleep quality.[19,38,39] Thus, the association between gender and sleep quality may be mediated by the presence of other sleep disorders.
With regards to laboratory tests’ results, we did not find an association between calcium/phosphate and sleep quality, while in one study, poor sleep quality was associated with higher serum phosphate levels,[34] and other studies found that higher amount of calcium × phosphate product is associated with sleep quality.[18] This association may be justified by higher frequency of comorbidities in patients with elevated calcium × phosphate product, though further investigations are required in this regard.[18] Similar to several other reports we found an independent association between CRP levels and sleep quality.[40–42] This association corroborated to the role of inflammation in the pathogenesis of sleep disturbances. On the other hand, the inflammatory state in dialysis patients might be due to sleep related breathing disorders.[43] Indeed, it might be a bidirectional relationship between sleep disturbance and inflammatory state in ESRD patients, which can also justify the association of sleep disorders with an increased mortality rate of dialysis patients.
Anemia is another possible mechanism that has long been considered as a risk factor for sleep disturbance in dialysis patients. An association between hemoglobin levels,[26] iron deficiency,[16] and transferrin saturation[17] has been indicated by previous reports. In our study, higher transferrin level (that may indicate an iron deficient state) was a predictor of poor overall sleep quality and sleep disturbance. However, other indicators of iron state were not associated with sleep quality in our study and a precise conclusion is not possible from our data in this regard. Anyway, the full evaluation of iron status in ESRD patients with sleep disorder and appropriate therapy when results indicate an iron deficiency state seems to be warranted.
While several studies showed high prevalence of sleep disorders among patients on dialysis, few reports are available on treatment strategies, which could be attributed to the unclear pathophysiology of sleep disorders in these patients. Also, the presence of frequent comorbidities and drug interactions limit the use of sleep medications in ESRD patients. However, considering the current known risk factors, some trials have been done with two main approaches; therapeutic interventions and dialysis modifications. In one study, a course of cognitive-behavioral therapy resulted in improvement of sleep quality and psychological state.[44] Another study with intradialytic aerobic exercise found the same results.[45] In these studies, sleep quality improvement has been associated with decrease in inflammation and oxidative stress markers, highlighting the role of inflammation and oxidative stress in sleep disturbances in patients on dialysis.[45,46] The beneficial effects of cognitive-behavioral therapy and (intradialytic aerobic) exercise have also been reported by other studies.[47,48] Thus, regarding high prevalence of mood disorders in ESRD patients on dialysis and its effects on sleep quality, psycho-behavioral therapies could be good candidates for the treatment of mood/sleep disorders in ESRD patients. Regarding dialysis-related factors, skin temperature changes following dialysis have possible effects on nocturnal sleep, and using cool dialysate during HD showed improved sleep during the night following treatment in one trial.[49] The underlying mechanism in this trial might be decreasing sympathetic activation and maintaining normal nocturnal skin temperature.[49] Several studies also reported beneficial effects of nocturnal dialysis, which provides superior dialysis based upon dose, duration, and frequency.[50–53] Correction of melatonin rhythm[51,54] and better fluid and uremic clearance are mentioned as possible mechanisms in this regard.[52] Anyway, much more studies are required for the treatment of sleep disorders in ESRD patients.
CONCLUSIONS
The results of the present study showed that poor sleep quality is highly frequent in uremic patients on maintenance dialysis, and mood disorders and being on HD are major risk factors for poor sleep quality in these patients. Furthermore, we found that age, female gender, lower physical activity, inflammation, and an iron deficient state are independent predictors of quality of sleep in some of its dimensions. Further studies are required for better understanding of risk factors associated with poor sleep quality and thus possible treatments in these patients. With current knowledge, psycho-behavioral therapies could be good candidates for the treatment of mood/sleep disorders in ESRD patients on maintenance dialysis.
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences. Authors are thankful to Prof. Richard Allen from the Johns Hopkins University and Dr. Mohammad Saadatnia from the Isfahan University of Medical Sciences for helping us in designing the study. We appreciate Mojtaba Akbari for helping in data analyses, staffs of dialysis units in Alzahra and Noor hospitals for helping us in data gathering, and Dr. Baradaran Clinical Laboratory for doing the laboratory tests.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Koch BC, Nagtegaal JE, Kerkhof GA, ter Wee PM. Circadian sleep-wake rhythm disturbances in end-stage renal disease. Nat Rev Nephrol. 2009;5:407–16. doi: 10.1038/nrneph.2009.88. [DOI] [PubMed] [Google Scholar]
- 2.Perl J, Unruh ML, Chan CT. Sleep disorders in end-stage renal disease: ‘Markers of inadequate dialysis’? Kidney Int. 2006;70:1687–93. doi: 10.1038/sj.ki.5001791. [DOI] [PubMed] [Google Scholar]
- 3.Tang SC, Lai KN. Sleep disturbances and sleep apnea in patients on chronic peritoneal dialysis. J Nephrol. 2009;22:318–25. [PubMed] [Google Scholar]
- 4.Bilgic A, Akgul A, Sezer S, Arat Z, Ozdemir FN, Haberal M. Nutritional status and depression, sleep disorder, and quality of life in hemodialysis patients. J Ren Nutr. 2007;17:381–8. doi: 10.1053/j.jrn.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Gusbeth-Tatomir P, Boisteanu D, Seica A, Buga C, Covic A. Sleep disorders: A systematic review of an emerging major clinical issue in renal patients. Int Urol Nephrol. 2007;39:1217–26. doi: 10.1007/s11255-007-9262-2. [DOI] [PubMed] [Google Scholar]
- 6.La Manna G, Pizza F, Persici E, Baraldi O, Comai G, Cappuccilli ML, et al. Restless legs syndrome enhances cardiovascular risk and mortality in patients with end-stage kidney disease undergoing long-term haemodialysis treatment. Nephrol Dial Transplant. 2011;26:1976–83. doi: 10.1093/ndt/gfq681. [DOI] [PubMed] [Google Scholar]
- 7.Masuda T, Murata M, Honma S, Iwazu Y, Sasaki N, Ogura M, et al. Sleep-disordered breathing predicts cardiovascular events and mortality in hemodialysis patients. Nephrol Dial Transplant. 2011;26:2289–95. doi: 10.1093/ndt/gfq756. [DOI] [PubMed] [Google Scholar]
- 8.Turkmen K, Yazici R, Solak Y, Guney I, Altintepe L, Yeksan M, et al. Health-related qualıty of lıfe, sleep qualıty, and depressıon in peritoneal dialysis and hemodıalysıs patıents. Hemodial Int. 2012;16:198–206. doi: 10.1111/j.1542-4758.2011.00648.x. [DOI] [PubMed] [Google Scholar]
- 9.Eryavuz N, Yuksel S, Acarturk G, Uslan I, Demir S, Demir M, et al. Comparison of sleep quality between hemodialysis and peritoneal dialysis patients. Int Urol Nephrol. 2008;40:785–91. doi: 10.1007/s11255-008-9359-2. [DOI] [PubMed] [Google Scholar]
- 10.Holley JL, Nespor S, Rault R. A comparison of reported sleep disorders in patients on chronic hemodialysis and continuous peritoneal dialysis. Am J Kidney Dis. 1992;19:156–61. doi: 10.1016/s0272-6386(12)70125-7. [DOI] [PubMed] [Google Scholar]
- 11.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 12.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P) Sleep Breath. 2012;16:79–82. doi: 10.1007/s11325-010-0478-5. [DOI] [PubMed] [Google Scholar]
- 15.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dashti-Khavidaki S, Chamani N, Khalili H, Hajhossein Talasaz A, Ahmadi F, Lessan-Pezeshki M, et al. Comparing effects of clonazepam and zolpidem on sleep quality of patients on maintenance hemodialysis. Iran J Kidney Dis. 2011;5:404–9. [PubMed] [Google Scholar]
- 17.Araujo SM, Bruin VM, Daher EF, Medeiros CA, Almeida GH, Bruin PF. Quality of sleep and day-time sleepiness in chronic hemodialysis: A study of 400 patients. Scand J Urol Nephrol. 2011;45:359–64. doi: 10.3109/00365599.2011.584694. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Guo Q, Ye X, Lin J, Yi C, Mao H, et al. Prevalence and risk factors of sleep disturbance in continuous ambulatory peritoneal dialysis patients in Guangzhou, southern China. Int Urol Nephrol. 2012;44:929–36. doi: 10.1007/s11255-011-0060-5. [DOI] [PubMed] [Google Scholar]
- 19.Chen WC, Lim PS, Wu WC, Chiu HC, Chen CH, Kuo HY, et al. Sleep behavior disorders in a large cohort of chinese (Taiwanese) patients maintained by long-term hemodialysis. Am J Kidney Dis. 2006;48:277–84. doi: 10.1053/j.ajkd.2006.04.079. [DOI] [PubMed] [Google Scholar]
- 20.Bilgic A, Akman B, Sezer S, Arat Z, Ozelsancak R, Ozdemir N. Daytime sleepiness and quality of life in peritoneal dialysis patients. Ther Apher Dial. 2011;15:565–71. doi: 10.1111/j.1744-9987.2011.00987.x. [DOI] [PubMed] [Google Scholar]
- 21.Wei CY, Chung TC, Wu SC, Chung CF, Wu WP. The subjective sleep quality and heart rate variability in hemodialysis patients. Ren Fail. 2011;33:109–17. doi: 10.3109/0886022X.2010.541578. [DOI] [PubMed] [Google Scholar]
- 22.Hsu CY, Lee CT, Lee YJ, Huang TL, Yu CY, Lee LC, et al. Better sleep quality and less daytime symptoms in patients on evening hemodialysis: A questionnaire-based study. Artif Organs. 2008;32:711–6. doi: 10.1111/j.1525-1594.2008.00593.x. [DOI] [PubMed] [Google Scholar]
- 23.Bastos JP, Sousa RB, Nepomuceno LA, Gutierrez-Adrianzen OA, Bruin PF, Araújo ML, et al. Sleep disturbances in patients on maintenance hemodialysis: Role of dialysis shift. Rev Assoc Med Bras. 2007;53:492–6. doi: 10.1590/s0104-42302007000600014. [DOI] [PubMed] [Google Scholar]
- 24.Araujo SM, de Bruin VM, Daher Ede F, Almeida GH, Medeiros CA, de Bruin PF. Risk factors for depressive symptoms in a large population on chronic hemodialysis. Int Urol Nephrol. 2012;44:1229–35. doi: 10.1007/s11255-011-0032-9. [DOI] [PubMed] [Google Scholar]
- 25.Guney I, Atalay H, Solak Y, Altintepe L, Toy H, Tonbul HZ, et al. Predictors of sleep quality in hemodialysis patients. Int J Artif Organs. 2010;33:154–60. doi: 10.1177/039139881003300304. [DOI] [PubMed] [Google Scholar]
- 26.Pai MF, Hsu SP, Yang SY, Ho TI, Lai CF, Peng YS. Sleep disturbance in chronic hemodialysis patients: The impact of depression and anemia. Ren Fail. 2007;29:673–7. doi: 10.1080/08860220701459642. [DOI] [PubMed] [Google Scholar]
- 27.Feroze U, Martin D, Reina-Patton A, Kalantar-Zadeh K, Kopple JD. Mental health, depression, and anxiety in patients on maintenance dialysis. Iran J Kidney Dis. 2010;4:173–80. [PubMed] [Google Scholar]
- 28.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: A focus on insomnia. Sleep Med Rev. 2010;14:227–38. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 29.Maes M, Kubera M, Obuchowiczwa E, Goehler L, Brzeszcz J. Depression's multiple comorbidities explained by (neuro) inflammatory and oxidative and nitrosative stress pathways. Neuro Endocrinol Lett. 2011;32:7–24. [PubMed] [Google Scholar]
- 30.Güney I, Biyik M, Yeksan M, Biyik Z, Atalay H, Solak Y, et al. Sleep quality and depression in peritoneal dialysis patients. Ren Fail. 2008;30:1017–22. doi: 10.1080/08860220802406419. [DOI] [PubMed] [Google Scholar]
- 31.Burrowes JD, Russell GB, Unruh M, Rocco MV. Is nutritional status associated with self-reported sleep quality in the HEMO study cohort? J Ren Nutr. 2012;22:461–71. doi: 10.1053/j.jrn.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Sabbagh R, Iqbal S, Vasilevsky M, Barré P. Correlation between physical functioning and sleep disturbances in hemodialysis patients. Hemodial Int. 2008;12:S20–4. doi: 10.1111/j.1542-4758.2008.00319.x. [DOI] [PubMed] [Google Scholar]
- 33.Han SY, Yoon JW, Jo SK, Shin JH, Shin C, Lee JB, et al. Insomnia in diabetic hemodialysis patients. Prevalence and risk factors by a multicenter study. Nephron. 2002;92:127–32. doi: 10.1159/000064460. [DOI] [PubMed] [Google Scholar]
- 34.Unruh ML, Hartunian MG, Chapman MM, Jaber BL. Sleep quality and clinical correlates in patients on maintenance dialysis. Clin Nephrol. 2003;59:280–8. doi: 10.5414/cnp59280. [DOI] [PubMed] [Google Scholar]
- 35.Argekar P, Griffin V, Litaker D, Rahman M. Sleep apnea in hemodialysis patients: Risk factors and effect on survival. Hemodial Int. 2007;11:435–41. doi: 10.1111/j.1542-4758.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- 36.Kuhlmann U, Becker HF, Birkhahn M, Peter JH, von Wichert P, Schütterle S, et al. Sleep-apnea in patients with end-stage renal disease and objective results. Clin Nephrol. 2000;53:460–6. [PubMed] [Google Scholar]
- 37.Siddiqui S, Kavanagh D, Traynor J, Mak M, Deighan C, Geddes C. Risk factors for restless legs syndrome in dialysis patients. Nephron Clin Pract. 2005;101:c155–60. doi: 10.1159/000087073. [DOI] [PubMed] [Google Scholar]
- 38.Araujo SM, de Bruin VM, Nepomuceno LA, Maximo ML, Daher Ede F, Correia Ferrer DP, et al. Restless legs syndrome in end-stage renal disease: Clinical characteristics and associated comorbidities. Sleep Med. 2010;11:785–90. doi: 10.1016/j.sleep.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 39.Jurado-Gamez B, Martin-Malo A, Alvarez-Lara MA, Muñoz L, Cosano A, Aljama P. Sleep disorders are underdiagnosed in patients on maintenance hemodialysis. Nephron Clin Pract. 2007;105:c35–42. doi: 10.1159/000096982. [DOI] [PubMed] [Google Scholar]
- 40.Lee JH, Kim SJ, Jung HH. Nocturnal sleep related with metabolic markers in end-stage renal disease patients receiving hemodialysis. Psychiatry Investig. 2009;6:34–8. doi: 10.4306/pi.2009.6.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bornivelli C, Alivanis P, Giannikouris I, Arvanitis A, Choustoulakis I, Georgopoulou K, et al. Relation between insomnia mood disorders and clinical and biochemical parameters in patients undergoing chronic hemodialysis. J Nephrol. 2008;21:S78–83. [PubMed] [Google Scholar]
- 42.Chiu YL, Chuang YF, Fang KC, Liu SK, Chen HY, Yang JY, et al. Higher systemic inflammation is associated with poorer sleep quality in stable haemodialysis patients. Nephrol Dial Transplant. 2009;24:247–51. doi: 10.1093/ndt/gfn439. [DOI] [PubMed] [Google Scholar]
- 43.Koehnlein T, Schmidt A, Moesenthin M, Dierkes J, Neumann KH, Welte T. Increased cardiac troponin T and C-reactive protein levels in end-stage renal disease are associated with obstructive sleep apnea. Clin Nephrol. 2009;71:50–8. doi: 10.5414/cnp71050. [DOI] [PubMed] [Google Scholar]
- 44.Chen HY, Cheng IC, Pan YJ, Chiu YL, Hsu SP, Pai MF, et al. Cognitive-behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patients. Kidney Int. 2011;80:415–22. doi: 10.1038/ki.2011.151. [DOI] [PubMed] [Google Scholar]
- 45.Afshar R, Emany A, Saremi A, Shavandi N, Sanavi S. Effects of intradialytic aerobic training on sleep quality in hemodialysis patients. Iran J Kidney Dis. 2011;5:119–23. [PubMed] [Google Scholar]
- 46.Duarte PS, Miyazaki MC, Blay SL, Sesso R. Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int. 2009;76:414–21. doi: 10.1038/ki.2009.156. [DOI] [PubMed] [Google Scholar]
- 47.Giannaki CD, Sakkas GK, Hadjigeorgiou GM, Karatzaferi C, Patramani G, Lavdas E, et al. Non-pharmacological management of periodic limb movements during hemodialysis session in patients with uremic restless legs syndrome. ASAIO J. 2010;56:538–42. doi: 10.1097/MAT.0b013e3181f1cc04. [DOI] [PubMed] [Google Scholar]
- 48.Heidarzadeh M, Zamanzadeh V, Maghvan AP, Oshvandi K. The effect of physical exercise on physical and psychological problems. Iran J Nurs Midwifery Res. 2010;15:20–6. [PMC free article] [PubMed] [Google Scholar]
- 49.Parker KP, Bailey JL, Rye DB, Bliwise DL, Van Someren EJ. Insomnia on dialysis nights: The beneficial effects of cool dialysate. J Nephrol. 2008;21:S71–7. [PubMed] [Google Scholar]
- 50.Beecroft JM, Duffin J, Pierratos A, Chan CT, McFarlane P, Hanly PJ. Decreased chemosensitivity and improvement of sleep apnea by nocturnal hemodialysis. Sleep Med. 2009;10:47–54. doi: 10.1016/j.sleep.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 51.Koch BC, Hagen EC, Nagtegaal JE, Boringa JB, Kerkhof GA, Ter Wee PM. Effects of nocturnal hemodialysis on melatonin rhythm and sleep-wake behavior: An uncontrolled trial. Am J Kidney Dis. 2009;53:658–64. doi: 10.1053/j.ajkd.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 52.Tang SC, Lam B, Lai AS, Pang CB, Tso WK, Khong PL, et al. Improvement in sleep apnea during nocturnal peritoneal dialysis is associated with reduced airway congestion and better uremic clearance. Clin J Am Soc Nephrol. 2009;4:410–8. doi: 10.2215/CJN.03520708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hanly PJ, Pierratos A. Improvement of sleep apnea in patients with chronic renal failure who undergo nocturnal hemodialysis. N Engl J Med. 2001;344:102–7. doi: 10.1056/NEJM200101113440204. [DOI] [PubMed] [Google Scholar]
- 54.Koch BC, Nagtegaal JE, Hagen EC, Wee PM, Kerkhof GA. Different melatonin rhythms and sleep-wake rhythms in patients on peritoneal dialysis, daytime hemodialysis and nocturnal hemodialysis. Sleep Med. 2010;11:242–6. doi: 10.1016/j.sleep.2009.04.006. [DOI] [PubMed] [Google Scholar]


