Abstract
Background:
Anemia has been a very important nutritional disorder in the world. India has reported high prevalence of anemia in pregnancy. Most of the articles have reported an adverse pregnancy outcome related to anemia. Of late, reports are emerging suggesting anemia could be indeed beneficial. Apart from that, there was no consistency in the timing of hemoglobin considered for analysis. Hence, we designed an observational study to look into these aspects.
Methods:
1000 mothers admitted for delivery were recruited and their hemoglobin was measured. Hemoglobin in previous trimesters was noted from their antenatal record. We followed up these mothers till delivery and looked into the gestation and birth weight of the babies. Descriptive statistics was used for baseline characteristics. Comparison of means was done using Student's t-test. Qualitative variables were compared using Fisher's exact test.
Results:
More than 50% of the mothers were anemic at some point of time during their pregnancy and 39% of the mothers were anemic throughout. Mean birth weight of babies born to anemic mothers was marginally lower compared to that of babies born to nonanemic mothers. This difference was statistically significant. There was 6.5% increase in the incidence of low birth weight babies and 11.5% increase in preterm deliveries in mothers who were anemic in their third trimester.
Conclusions:
The incidence of low birth weight babies was significantly more in mothers who were anemic in their third trimester. Preterm deliveries occurred more frequently in mothers who were anemic in their second and third trimesters. Higher hemoglobin did not show any effect on either birth weight or gestation in our study.
Keywords: Anemia, birth weight, gestation age, maternal hemoglobin, trimester
INTRODUCTION
Anemia has been a very important nutritional disorder in the world. India has a big chunk of population suffering from anemia. India has reported high prevalence of anemia in pregnancy. In one of the studies conducted on a large population, it was estimated that 87% of the Indian pregnant women are anemic.[1] This figure is the highest among the neighboring South East Asian countries.[1] Interestingly, anemia in pregnant women has multiple effects on pregnancy and fetal growth. It is a well established fact that there is a physiological drop in hemoglobin (Hb) in the mid-trimester. This physiological drop is attributed to increase in plasma volume, and hence decrease in blood viscosity. This aids in better circulation in the placenta. The nadir of this drop is variable, and hence there was a need for criteria for defining anemia in pregnancy. WHO has defined Hb of less than 110 g/l as anemia in pregnancy.[2] Hitherto, anemia in pregnant women has been regarded as detrimental to the fetal growth and pregnancy outcome. Low birth weight and preterm delivery have been persistently linked to anemia in pregnancy.[1–4] The role of anemia in pregnancy and iron on the growing fetus has been studied in the last few decades. The outcome of these studies is either inconclusive or at the most supportive of the popular notions held so far regarding pregnancy outcome and anemia.[2–6] Hence, most of the countries have adopted the policy of supplementing pregnant women with iron and folic acid with a view that increasing the Hb levels has some beneficial effect.[1] In the modern era of research methodology, researchers have attempted to revisit this fundamental notion of increasing the Hb in pregnancy by iron supplementation in order to have better pregnancy outcome. Several randomized control trials (RCTs) and meta-analyses have shown that routine iron supplementation is not of much use.[7,8] Few of the studies have also shown that increase in the Hb beyond a certain level could in fact have a negative outcome.[9–19] This has led both clinicians and researchers to look for the optimal level of Hb that would yield the best outcome. Though there are defined criteria for anemia in pregnancy, it is still not clear which trimester Hb should be taken as the standard for assessment. Studies done so far have not looked into this aspect in detail. The fetal growth occurs in various phases, and most of the micronutrient related issues occur in the third trimester. Hence, studying the impact of anemia in various trimesters on fetal outcome would be more meaningful.
We aimed at comparing the gestation and birth weight of the babies who were born to mothers with and without anemia at different trimesters.
METHODS
Study design
This was an observational study. No specific intervention for the sake of study was done. Mothers were recruited when they arrived for delivery. Required information was obtained from interview and antenatal record. Once they delivered the baby, the remaining data were collected.
Study setting
The study was conducted at Department of Pediatrics and Obstetrics and Gynecology, JSS Medical College Hospital, Mysooru, Karnataka, India. This is a tertiary center with annual delivery rate of approximately 2500 and is a 20-bedded neonatal unit.
Sample size
This was designed as a prospective observational study. Alpha was taken as 0.5 and beta to be 0.2. The power of the study was taken as 80%. Using the standard deviations from similar previous studies, sample size was calculated using the nomogram with the above inputs. This returned a value of 400. The design effect was considered to be 2as done in anemia surveys. The sample size needed was 800. Assuming dropouts and technical issues during the course of the study, extra 20% was added. This returned a value of 960. Thus, a minimum of 960 subjects were planned to be included in this study.
Inclusion criteria
All pregnant women who came for delivery in our institute were included.
Exclusion criteria
Pregnant women with one of the following at booking were excluded:
Diabetes mellitus.
Hypertension (including pregnancy-induced hypertension).
Toxoplasmosis, Rubella, Cytomegalovirus, Herpes infection.
Diagnosed renal or cardiac illness.
Smoker or alcoholic.
Hemoglobinopathies (e.g. thalassemia).
Multiple gestation.
Sampling
This study was done over a period of 2 years. After obtaining consent, pregnant mothers were included provisionally into the study. They were initially interviewed and their antenatal record was checked. If they met any one of the exclusion criteria, they were excluded. This exercise was continued till the required sample size was achieved. Recruitment for the study was later stopped. A total of 1000 mothers were included for the study.
Intervention
Measurement of Hb was done by cyanmethemoglobin method (Analyzer–Coulter). Measurement was done in all the three trimesters when they arrived for antenatal checkup. Rest of the management was as per the standards practiced in antenatal care. Birth weight was recorded in kilograms using a digital scale. Gestation assessment was done using first trimester dating scan. This was complemented by obstetric assessment and postnatal assessment using modified Ballard scoring.
Statistical analysis
Statistical analysis was done on Microsoft Excel and Prism's Graph Pad software. Categorical variables were analyzed using Fischer's exact test. Odds ratio was additionally calculated. Comparison of means was done using Student's t-test.
Ethical committee approval
The medical college ethical committee had approved this study.
Consent
The details of the study were explained to the pregnant mothers. Informed consent was taken from them before recruitment.
RESULTS
Analysis of quantitative variables
Anemia
More than half of our mothers were anemic to start with. Higher percentage of anemia was seen in the second trimester and was lowest in the third trimester. More than one-third of the mothers remained anemic throughout all the trimesters. Less than 30% of the mothers were non-anemic throughout. There were only 18 mothers who could be categorized as having severe anemia (Hb <70g/l). Twelve of them were in the first trimester, five in the second trimester, and only one was in the third trimester. Hb of the mothers who were anemic in the first trimester showed an improving trend over the next two trimesters. Results are as shown in the Table 1.
Table 1.
Showing number of anemic mothers and their mean hemoglobin in 3 trimesters
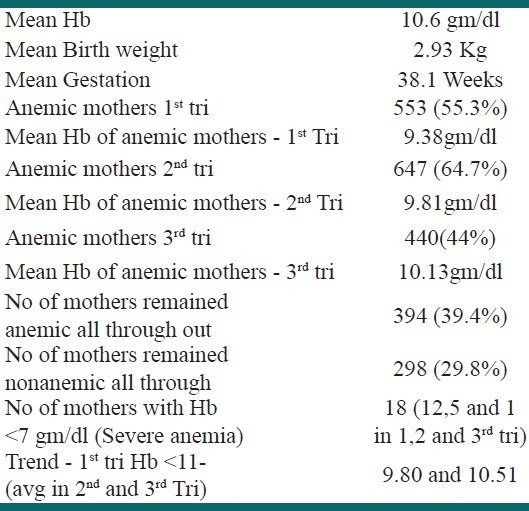
Mean Hb in the no anemia group remained high in all the three trimesters compared to the anemia group. However, it is interesting to note that the mid-trimester drop was seen only in mothers who were not anemic. In the anemic mothers, there was a general trend of increment in Hb in all the trimesters [Figure 1]. The difference in the mean Hb values in the two groups reduced as the pregnancy progressed. However, the difference always remained till the end of pregnancy.
Figure 1.
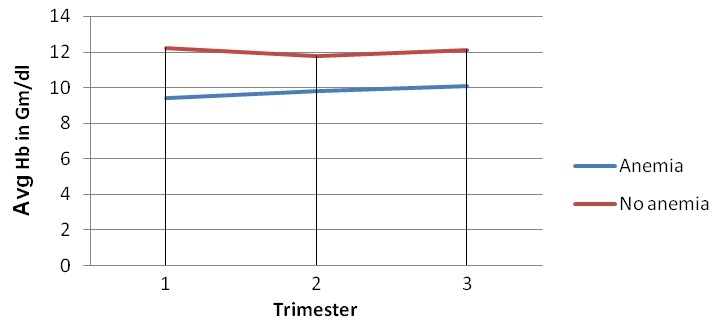
The trend in hemoglobin over the three trimesters (Avg Hb=average hemoglobin in mg/dl)
Birth weight
Mean birth weight and gestation of the babies in both the groups of anemic and nonanemic mothers were in clinical normal range irrespective of the trimester [Table 2]. There was marginal but “statistically significant” difference between both the groups in all the parameters studied. Babies born to the anemic mothers remained lighter compared to their counterparts. The difference got accentuated if babies of all trimester anemia mothers were compared with the babies of all trimester nonanemic mothers.
Table 2.
Mean birth weight and gestation in Anemic and non anemic groups at various trimesters
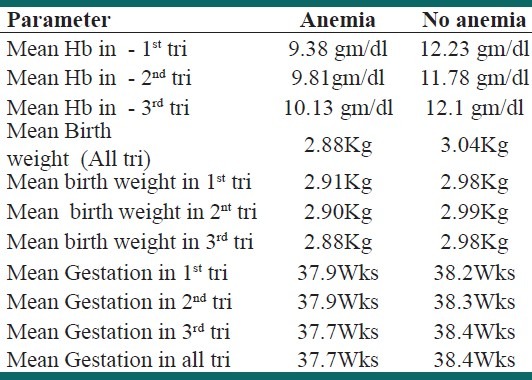
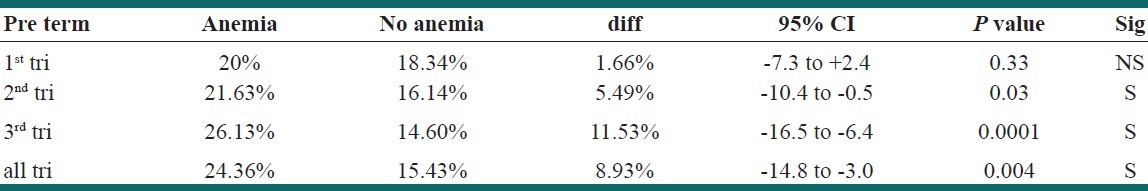
Gestation
The mean gestation of the babies born to anemic mothers was lesser compared to babies born to nonanemic mothers. Figure 2 shows the dramatic deviation in the direction of the curves. This difference was striking in the third trimester. The difference remained even when all trimester anemia group was compared with all trimester no anemia group [Figure 3].
Figure 2.
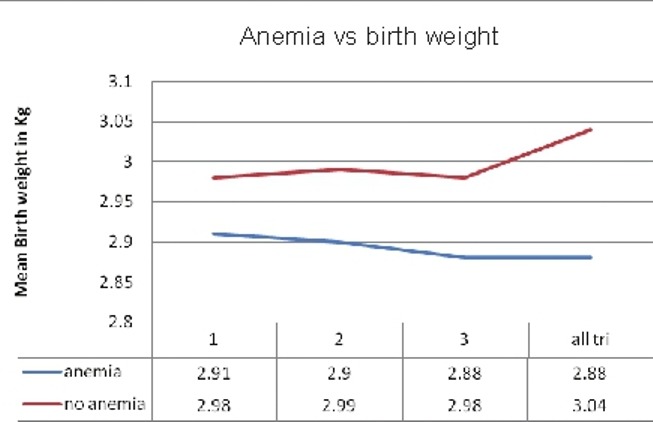
The average birth weight trends in two groups at different trimesters (kg=kilograms, all tri=all trimesters)
Figure 3.
The average gestation trends in two groups at different trimesters (all tri=all trimesters)
Analysis of qualitative variables
Low birth weight (birth weight less than 2499 g)
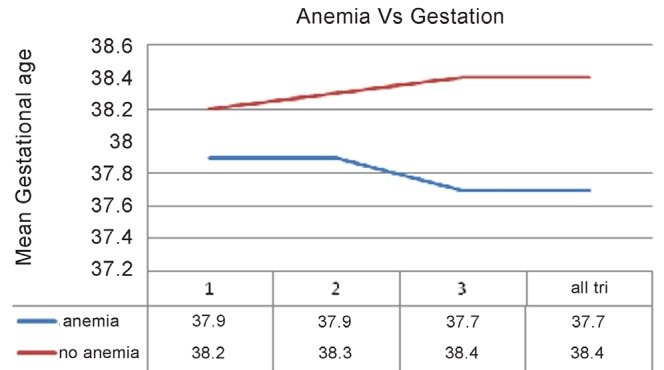
The proportion of children who were of low birth weight was marginally higher in mothers who had anemia. The difference was not significant except for anemia in the third trimester. The difference was 6.5% in the present study and 95% confidence interval (CI) was between 10.4% and 2.5%, favoring no anemia group. In rest of the trimesters, the difference was small (<5% overall). The CI had a wide range and crosses zero [Table 3].
Table 3.
The difference in LBW babies between anemic and non anemic groups
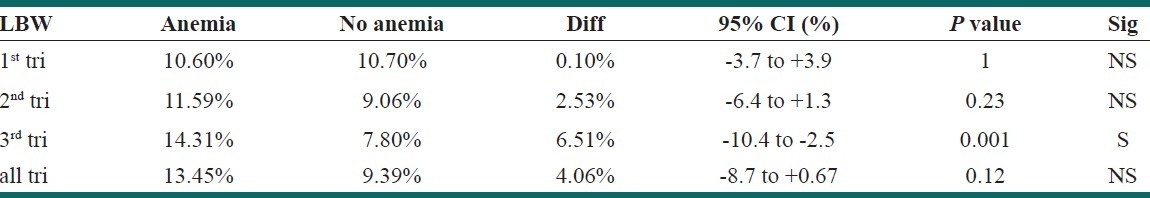
Prematurity (gestation of 36 weeks and 6 days or less)
There was significantly increased incidence of preterm deliveries in anemic mothers compared to nonanemic mothers, except in the first trimester. The difference was more than 5% overall, with maximum difference in the third trimester. Except for the first trimester, the 95% CI remained below zero, favoring no anemia group [Table 4].
Table 4.
The difference in Preterm deliveries between anemic and non anemic groups
In our study, we had only small number of mothers who could be classified as having severe anemia. Hence, we did not attempt to analyze them as a separate group.
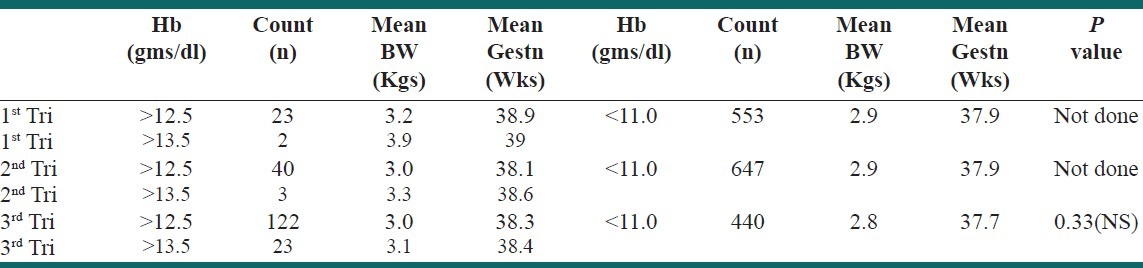
High Hb levels and outcome
We noted that the outcome in terms of mean birth weight and mean gestation was not adversely influenced by high Hb (for both>125 and 135 g/l). The number of mothers in these groups was small, and hence was not comparable with the number in anemia group. We attempted to compare the third trimester high Hb group as there was more number of mothers in this group. Mean birth weight and gestational age was marginally high, but not significant [Table 5].
Table 5.
Showing comparison between mean birth weight and gestational age in high hemoglobin and anemic mothers
DISCUSSION
Prevalence of anemia in pregnancy is quite high.[1,2] Our figures showed more than half of the mothers were anemic to start with. Similar figures are quoted in other studies as well.[1,20] The trend in Hb level is quite interesting. The mid-trimester drop seen in nonanemic mothers was not seen in anemic mothers. This indicates that mid-trimester drop in Hb is a very essential physiological arrangement. However, in anemic mothers, as the mean Hb in the mid-trimester was below that in nonanemic mothers, no drop phenomenon was seen. This suggests that there may be a narrow range of what the Hb should be in order to have good outcome. Looking at the graph [Figure 1], we believe that the range is between 10.5 and 12 g/dl. Comparison of mean birth weight and gestation in the two groups shows that both the parameters were lower in the anemic group than in the nonanemic group. Table 2 reveals marginal but “statistically significant” difference between both the groups in all the trimesters. The difference in mean weight was a maximum of 160 g and that of gestation was approximately 5 days. Given the fact that average birth weight and gestation are well in the safe normal clinical range in both the groups, this small difference of 160 g and 5 days between the two groups remains only as a point of statistical interest. Clinical implication of such a difference is hardly important. Swain et al. have reported an inverse relation between the second trimester Hb and birth weight.[16] The analysis of qualitative variables in our data has revealed noteworthy clinically relevant results. The incidence of low birth weight babies in the two groups remained similar with minimal difference and there was no statistical significance in the first two trimesters. The difference was significant only if the mothers were anemic in the third trimester. Many studies have reported significant association between low birth weight and maternal anemia.[3,5,21–23] A retrospective study has shown no association between the first trimester anemia and low birth weight.[24] Most of these studies have considered the Hb levels in the third trimester or at delivery for comparison.[3,5,21–23] This could well suggest that third trimester Hb is an important factor in determining birth weight. It is well known that rapid growth of fetus occurs in the third trimester. Iron and other micronutrient accretion rates are the highest in the same trimester as well. This physiology explains the association of third trimester Hb and low birth weight. In contrast to the above, association of preterm delivery with maternal anemia is quite striking. Except for the first trimester, anemia in other trimesters has shown significantly increased incidence of preterm delivery. This association appears strongest in the third trimester. There are many studies showing similar association.[3,5,22,25] Kumar et al. and Monika et al. have found such an association only when mothers are severely anemic, i.e. Hb <7.0 g/dl.[26,27] Another retrospective study has found no association between first trimester anemia and preterm delivery, similar to our study.[24] Contrast to our results, a study from China[28] has reported association of preterm delivery with anemia in all the trimesters, but with a reverse trend. The authors had observed a strong association of first trimester anemia and the least association of third trimester anemia. Few other studies have also reported a similar trend.[16,29] Currently, this still remains as a dogma. Though this association is convincing, this study could not provide any information about the possible mechanism. Maternal Hb versus uterine dynamics or other feto-placental complex relations are subjects of further intensive research which could explain such an association.
High Hb/hematocrit and low birth weight have been documented by some authors.[30] The sample number in our study was not sufficient enough to make meaningful conclusions. Third trimester high Hb does not seem to lead to more number of low birth weight babies. Usha et al. in their study of about 100 cases have a similar opinion.[3] In another study from Nepal, wherein the outcome of 1400 pregnancies was studied retrospectively, no association was found between high hematocrit and either low birth weight or preterm deliveries.[6] It seems keeping the Hb levels at optimal levels throughout the pregnancy would yield best neonatal outcome regarding prematurity and low birth weight. This leads to the question of reconsideration of iron supplementation policy to mothers. Looking at the above results, we feel a policy of earlier supplementation of iron in the second and third trimesters needs to be considered.
CONCLUSIONS
Anemia in pregnancy has a recognizable association with fetal outcome. Increased incidence of low birth weight babies is seen if the mother is anemic in her third trimester only. Increased incidence of preterm deliveries is seen if the mother is anemic in her second and third trimesters. Supplementing iron earlier and maintaining optimal Hb (10–12 g/dl) throughout gestation has better overall outcome regarding premature deliveries and low birth weight babies.
ACKNOWLEDGEMENTS
We thank Dr. Narayanappa D., Prof and Head of Pediatrics, and Dr. Parvathamma, Prof and Head, Department of Obstetrics and Gynecology, JSS Hospital, for their guidance and cooperation for this study.
We have not received any financial aid from anybody for this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Kalaivani K. Prevalence and consequences of anemia in pregnancy. Indian J Med Res. 2009;130:627–33. [PubMed] [Google Scholar]
- 2.Jaleel R, Khan A. Severe anemia and adverse pregnancy outcome. J Surg Pak (International) 2008;13:147–50. [Google Scholar]
- 3.Rusia U, Madan N, Agarwal N, Sikka M, Sood SK. Effect of maternal iron deficiency anemia on foetal outcome. Indian J pathol Microbiol. 1995;38:273–9. [PubMed] [Google Scholar]
- 4.Haggaz AD, Radi EA, Adam I. Anemia and low birth weight in western Sudan. Trans R Soc Trop Med Hyg. 2010;104:234–6. doi: 10.1016/j.trstmh.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Levy A, Fraser D, Katz M, Sheiner E. Maternal anemia during pregnancy is an independent risk factor for low birthweight and preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2005;122:182–6. doi: 10.1016/j.ejogrb.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Bondevik GT, Lie RT, Ulstein M, Kvale G. Maternal hematological status and risk of low birth weight and preterm delivery in Nepal. Acta Obstet Gynecol Scand. 2001;80:402–8. [PubMed] [Google Scholar]
- 7.Pena-Rosas JP, Viteri FE. Effects of routine oral iron supplementation with or without folic acid for women during pregnancy. Cochrane Database Syst Rev. 2006;(3):CD004736. doi: 10.1002/14651858.CD004736.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Hemminki E, Merilainen J. Long-term follow-up of mothers and their infants in a randomized trial on iron prophylaxis during pregnancy. Am J Obstet Gynecol. 1995;173:205–9. doi: 10.1016/0002-9378(95)90191-4. [DOI] [PubMed] [Google Scholar]
- 9.Koller O, Sagen N, Ulstein M, Vaula D. Fetal growth retardation associated with inadequate haemodilution in otherwise uncomplicated pregnancy. Acta Obstet Gynecol Scand. 1979;58:9–13. doi: 10.3109/00016347909154904. [DOI] [PubMed] [Google Scholar]
- 10.Koller O, Sandvei R, Sagen N. High hemoglobin levels during pregnancy and fetal risk. Int J Gynaecol Obstet. 1980;18:53–6. doi: 10.1002/j.1879-3479.1980.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 11.Ortner A, Zech H, Humpeler E, Mairbaeurl H. May high oxygen affinity of maternal hemoglobin cause fetal growth retardation? Arch Gynecol. 1983;234:79–85. doi: 10.1007/BF00207679. [DOI] [PubMed] [Google Scholar]
- 12.Huisman A, Aarnoudse JG. Increased 2nd trimester hemoglobin concentration in pregnancies later complicated by hypertension and growth retardation. Early evidence of a reduced plasma volume. Acta Obstet Gynecol Scand. 1986;65:605–8. doi: 10.3109/00016348609158396. [DOI] [PubMed] [Google Scholar]
- 13.Murphy JF, O’Riordan J, Newcombe RG, Coles EC, Pearson JF. Relation of haemoglobin levels in first and second trimesters to outcome of pregnancy. Lancet. 1986;1:992–5. doi: 10.1016/s0140-6736(86)91269-9. [DOI] [PubMed] [Google Scholar]
- 14.Sagen N, Nilsen ST, Kim HC, Bergsjo P, Koller O. Maternal hemoglobin concentration is closely related to birth weight in normal pregnancies. Acta Obstet Gynecol Scand. 1984;63:245–8. doi: 10.3109/00016348409155506. [DOI] [PubMed] [Google Scholar]
- 15.Gaspar MJ, Ortega RM, Moreiras O. Relationship between iron status in pregnant women and their newborn babies. Investigation in a Spanish population. Acta Obstet Gynecol Scand. 1993;72:534–7. doi: 10.3109/00016349309058158. [DOI] [PubMed] [Google Scholar]
- 16.Rasmussen S, Oian P. First- and second-trimester hemoglobin levels. Relation to birth weight and gestational age. Acta Obstet Gynecol Scand. 1993;72:246–51. doi: 10.3109/00016349309068032. [DOI] [PubMed] [Google Scholar]
- 17.Steer PJ. Maternal Hemoglobin concentration and birth weight. Am J Clin Nutr. 2000;71(5 Suppl):1285–7. doi: 10.1093/ajcn/71.5.1285s. [DOI] [PubMed] [Google Scholar]
- 18.Forest JC, Masse J, Moutquin JM. Maternal hematocrit and albumin as predictors of intrauterine growth retardation and preterm delivery. Clin Biochem. 1996;29:563–6. doi: 10.1016/s0009-9120(96)00101-4. [DOI] [PubMed] [Google Scholar]
- 19.Lu ZM, Goldenberg RL, Cliver SP, Cutter G, Blankson M. The relationship between maternal hematocrit and pregnancy outcome. Obstet Gynecol. 1991;77:190–4. doi: 10.1097/00006250-199102000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ Comparative Risk Assessment Collaborating Group. Selected risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 21.Elhassan EM, Abbaker AO, Haggaz AD, Abubaker MS, Adam I. Anaemia and low birth weight in Medani, Hospital Sudan. BMC Res Notes. 2010;3:181. doi: 10.1186/1756-0500-3-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lone FW, Quershi RN, Emanuel F. Maternal anemia and its impact on Perinatal outcome. Trop Med Int Health. 2004;9:486–90. doi: 10.1111/j.1365-3156.2004.01222.x. [DOI] [PubMed] [Google Scholar]
- 23.Shobeiri F, Begum K, Nazari M. A prospective study of maternal hemoglobin status of Indian women during pregnancy and pregnancy outcome. Nutr Res. 2006;26:209–13. [Google Scholar]
- 24.Phaloprakam C, Tangjitgamol S. Impact of high maternal hemoglobin at first antenatal visit on pregnancy outcomes: A Cohort study. J Perinat Med. 2008;36:115–9. doi: 10.1515/JPM.2008.018. [DOI] [PubMed] [Google Scholar]
- 25.Karasahin E, Ceyhan ST, Goktolga U, Baser I. Maternal Anemia and perinatal outcome. Perinatal Journal (Perinatoloji Dergisi) 2007;15:127–30. [Google Scholar]
- 26.Kumar A, Chaudhary K, Prasad S. Maternal Indicators and obstetric outcome in the north Indian population: A hospital based study. J Postgrad Med. 2010;56:192–5. doi: 10.4103/0022-3859.68647. [DOI] [PubMed] [Google Scholar]
- 27.Malhotraa M, Sharmaa JB, Batraa S, Sharma S, Murthy NS, Aroraa R. Maternal and perinatal outcome in varying degrees of anemia. Int J Gynaecol Obstet. 2002;79:93–100. doi: 10.1016/s0020-7292(02)00225-4. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Q, Ananth CV, Li Z, Smulian JC. Maternal anemia and preterm birth: A prospective cohort study. Int J Epidemiol. 2009;38:1380–9. doi: 10.1093/ije/dyp243. [DOI] [PubMed] [Google Scholar]
- 29.Scanlon KS, Yip R, Schieve LA, Cogswell ME. High and low hemoglobin levels during pregnancy: Differential risks for preterm birth and small for gestational age. Obstet Gynecol. 2000;96(5 Pt 1):741–8. doi: 10.1016/s0029-7844(00)00982-0. [DOI] [PubMed] [Google Scholar]
- 30.Blankson ML, Goldenberg RL, Cutter G, Cliver SP. The relationship between maternal hematocrit and pregnancy outcome: Black-white differences. J Natl Med Assoc. 1993;85:130–4. [PMC free article] [PubMed] [Google Scholar]


