Abstract
Background:
Vitiligo is an acquired, idiopathic disorder characterized by circumscribed depigmented macules and patches. The exact etiology and pathogenesis of vitiligo is not clear. Many theories have been presented regarding this subject among them aautoimmune theory is the most important one. The association of vitiligo with other autoimmune disorders has been reported, but the relationship between vitiligo and celiac disease is controversial. The aim of this study was to study the frequency of celiac autoantibodies in a group of vitiligo patients compared with control.
Methods:
This was a cross sectional case control study that involved 128 individuals, 64 vitiligo patients and 64 individuals as control group. The means age of participants was 30.3 ± 14.4 years. IgA anti Endomysial antibody and IgA anti-glutaminase antibody were measured by ELISA method in the serum of all participants. Data were analyzed by SPSS software version 15.
Results:
The serum of two vitiligo patients (3.1%) was positive for antibodies. All control groups were seronegative for these antibodies (P < 0.05). There was no significant effect of sex and job on seropositivity.
Conclusion:
There may be a relationship between celiac disease and vitiligo. This may indicate a common basic autoimmune mechanism that is an explanation for few case reports that gluten free diets were effective in the treatment of vitiligo patients. Both T test and exact fisher test showed no effect of age, sex and job on seropositivity of these patients (P = 0.56 and P = 0.74, respectively)
Keywords: Autoantibodies, celiac disease, gluten free diet, vitiligo
INTRODUCTION
Vitiligo is an acquired disorder in which patches of depigmented skin and overlying hair, and mucous membranes, are the result of progressive autoimmune loss of melanocytes from the involved areas.[1] Vitiligo affecting between 0.5-2% of the general population.[2] the specific causes of vitiligo remain obscure, and no common environmental triggers have yet been identified. Many theories have been put forward in this regard; autoimmune theory is the most popular one.
The risk of developing autoimmune disorders such as thyroid diseases, diabetes mellitus, and pernicious anemia are increased in patients who are affected by vitiligo.[3–17] The frequency of coincidence of vitiligo and Addison's disease and autoimmune chronic gastritis has been reported from 0.6% to 50% in different studies.[5–19]
Vitiligo has frequently been described in association with autoimmune diseases, particularly autoimmune thyroid diseases like Graves’ disease and autoimmune hypothyroidism.[20]
Celiac disease is a common immune-mediated enteropathy with a prevalence of approximately 1% within the U.S and European populations. The minimum prevalence of gluten sensitivity among the general population of northern and southern Iran is 1:104.[21] Serum immunoglobulin A-class tissue transglutaminase (TTGA) and Endomysial antibody (EMA) tests play a key role in the diagnostic evaluation of celiac disease. High serologic IgA tissue transglutaminase antibodies (TTGA) are exclusively associated with celiac disease.[22]
The relationship between celiac disease and vitiligo is controversial. Some authors have described cases of vitiligo in patients with celiac disease,[19,21] but one serological screening study for celiac disease in patients with vitiligo did not show any correlation between these two immunological disorders[23]
On the other hand, improvement of some disorders like dermatitis herpetiformis,[24] psoriasis,[25] and even vitiligo,[26] in those who were seropositive for celiac auto antibodies, has been reported by gluten free diet.
The aim of this research was to study the relationship between vitiligo and celiac disease. If this study show increased frequency of celiac autoantibodies in vitiligo patients, the second aim would be to try gluten free diet in these patients in future studies.
METHODS
This study included 64 patients diagnosed as vitiligo and 64 individuals without skin disease as control. The study was cross-sectional and the patients were selected using simple sampling method. This study was approved by ethical committee of Isfahan university of medical sciences.
This study was performed in AlZahra Hospital and Sedigheh tahereh Skin Diseases and Leishmaniasis Research Center, Isfahan university of Medical Sciences, Isfahan, Iran in 2008. The control group matched with case group according to age and sex, and selected from healthy people.
Demographic data such as patients age, sex, job and medical history including history of autoimmune disease (skin or other organ), and history of gastrointestinal disease were collected by a Questioner. Characteristics of vitiligo such as clinical type (localized or generalized, stable or progressive) and severity (percentage of body surface area involvement) were recorded in questionnaires.
Individuals who used medication such as sulfasalazin, captopril, phenytoin, valproic acid and D-penicillamin for other medical condition were excluded. Other exclusion criterias were history of anaphylaxis, diabetes mellitus type 1, autoimmune hepatitis, dermatitis herpetiform, psoriasis, and erythma nodosom and alopecia areata.
IgA anti endomysial and IgA anti transglutaminas antibodies were measured with ELISA method.
Data were analyzed by T-test and fisher exact test using SPSS version 13 software.
RESULTS
The mean age of participants were 30.3 ± 14.4 year. Each group consisted of 41 (64.1%) female and 23 (35.9%) male. Table 1 shows the characteristics of vitiligo patients. There was no significant differences between case and control group, regarding age and sex [Table 2]. Two female (3.1%) from vitiligo patients were seropositive for both anti Endomysial and anti transglutaminase antibodies. None of the control group were seropositive for these autoantibodies. (P < 0.05)
Table 1.
Characteristics of vitiligo patients
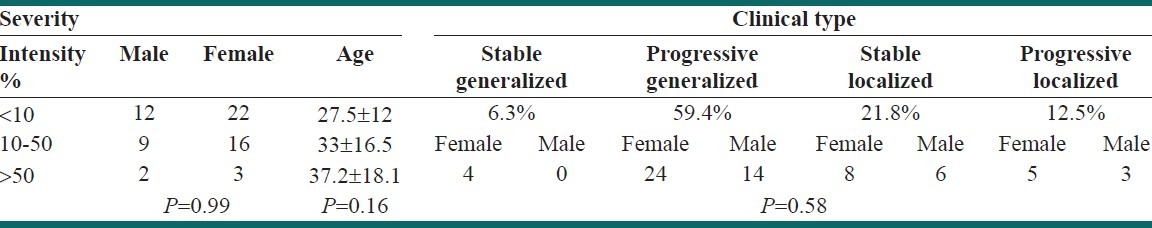
Table 2.
Frequency of celiac disease autoantibodies in case and control
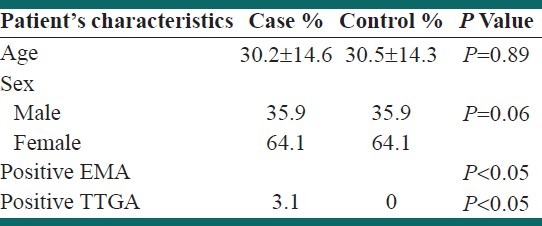
The t-test showed no effect of age on seropositivity for celiac antibody in vitiligo patient. (P = 0.56). The exact fisher test also showed no significant effect of sex and job on seropositivity of these patients (P = 0.56 and P = 0.74, respectively).
DISCUSSION
In the current study, IgA antibodies to endomysium and transglutaminas was detectable in 3.1% of patients with vitiligo. All control group were seronegative for these antibodies (P < 0.05) the age sex and job had no significant effect on seropositivity of patients.
Until now, the results of studies about the relationship between vitiligo and celiac disease are controversial. Seyhan in 2011, compared Sixty-one patients (21 children) with vitiligo and 60 healthy volunteers. Eleven patients with vitiligo (18.0%) and 1 control (1.7%) were seropositive for celiac disease.[27] In another study by this author, 9.1% of Fifty-five children and adolescents with celiac disease, had vitiligo.[28] In 1897 Volta et al. found no seropositive cases for celiac disease, among 198 patients with vitiligo.[22]
A survey of more than 2,600 unselected Caucasian patients with generalized vitiligo and their close relatives found that, the frequency of five autoimmune antibodies were significantly elevated in vitiligo probands and their first-degree relatives. These associations indicate that vitiligo shares common genetic aetiologic links with these autoimmune disorders (autoimmune thyroid disease, pernicious anemia, Addison's disease, systemic lupus erythematosus, and probably inflammatory bowel disease.).[3]
In contrast, in the same reaserch there was no significant increases in the frequencies of alopecia areata, type 1 diabetes mellitus, multiple sclerosis, myasthenia gravis, psoriasis, rheumatoid arthritis, scleroderma and Sjogren's syndrome, among the vitiliginous patients, suggesting that the diseases do not share the same common susceptibility genes.[3]
The seropositivity for celiac disease in vitiligo may show a common genetic basis for these disorders. This may be observed among peoples in some regions of the world. For example in our study in Iran and seyhan study in Turkey, the vitiligo patients were more seropositive, in comparison with the control group, but in volta study in Italy no seropositivity for celiac disease autoantibodies was found in these patients.[22,27]
There has been one case report about remission of vitiligo after starting gluten free diet in a child who was seropositive for celiac autantibody.[25] This indicates that both of these autoimmune diseases may be stimulated by a common signal in immune system that is triggered by gluten rich diet. Future basic study in this regard may lead to finding effective treatment modalities for vitiligo and celiac diseases.
CONCLUSION
The celiac disease autoantibodies are more common in serum of vitiligo patients compared with normal individuals suggesting common pathophysiologic autoimmune pathway for both diseases. To better evaluate the relationship between these two diseases, performing a large prospective study is recommended.
Footnotes
Source of Support: This study was conducted as a thesis funded by Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None declared
REFERENCES
- 1.Spritz RA. The genetics of generalized vitiligo and associated autoimmune diseases. J Dermatol Sci. 2006;41:3–10. doi: 10.1016/j.jdermsci.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Passeron T, Ortonne JP. Physiopathology and genetics of vitiligo. J Autoimmun. 2005;25:63–8. doi: 10.1016/j.jaut.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Barona MI, Arrunátegui A, Falabella R, Alzate A. An epidemiologic casecontrol study in a population with vitiligo. J Am Acad Dermatol. 1995;33:621–5. doi: 10.1016/0190-9622(95)91282-7. [DOI] [PubMed] [Google Scholar]
- 4.Kovacs SO. Vitiligo. J Am Acad Dermatol. 1998;38:647–66. doi: 10.1016/s0190-9622(98)70194-x. [DOI] [PubMed] [Google Scholar]
- 5.Zauli D, Tosti A, Biasco G, Miserocchi F, Patrizi A, Azzaroni D, et al. Prevalence of autoimmune atrophic gastritis in vitiligo. Digestion. 1986;34:169–72. doi: 10.1159/000199325. [DOI] [PubMed] [Google Scholar]
- 6.Frati R, Frati C, Sassano PP, Antonaci A. Vitiligo, autoimmune thyroiditis: A rare thyroid cancer arising with bone metastases on maxillofacial area. J Exp Clin Cancer Res. 1999;18:85–7. [PubMed] [Google Scholar]
- 7.Hegedus L, Heidenheim M, Gervil M, Hjalgrim H, Høier-Madsen M. High frequency of thyroid dysfunction in patients with vitiligo. Acta Derm Venereol. 1994;74:120–3. doi: 10.2340/0001555574120123. [DOI] [PubMed] [Google Scholar]
- 8.Iacovelli P, Sinagra JL, Vidolin AP, Marenda S, Capitanio B, Leone G, et al. Relevance of thyroiditis and of other autoimmune diseases in children with vitiligo. Dermatology. 2005;210:26–30. doi: 10.1159/000081479. [DOI] [PubMed] [Google Scholar]
- 9.Mandry RC, Ortiz LJ, Lugo-Somolinos A, Sánchez JL. Organ-specific autoantibodies in vitiligo patients and their relatives. Int J Dermatol. 1996;35:18–21. doi: 10.1111/j.1365-4362.1996.tb01609.x. [DOI] [PubMed] [Google Scholar]
- 10.Schallreuter KU, Lemke R, Brandt O, Schwartz R, Westhofen M, Montz R, et al. Vitiligo and other diseases: Coexistence or true association. Hamburg study on 321 patients? Dermatology. 1994;188:269–75. doi: 10.1159/000247164. [DOI] [PubMed] [Google Scholar]
- 11.Kakourou T, Kanaka-Gantenbein C, Papadopoulou A, Kaloumenou E, Chrousos GP. Increased prevalence of chronic autoimmune (Hashimoto's) thyroiditis in children and adolescents with vitiligo. J Am Acad Dermatol. 2005;53:220–3. doi: 10.1016/j.jaad.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 12.Zettinig G, Tanew A, Fischer G, Mayr W, Dudczak R, Weissel M. Autoimmune diseases in vitiligo: Do anti-nuclear antibodies decrease thyroid volume? Clin Exp Immunol. 2003;131:347–54. doi: 10.1046/j.1365-2249.2003.02089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Betterle C, Caretto A, De Zio A, Pedini B, Veller-Fornasa C, Cecchetto A, et al. Incidence and significance of organ-specific autoimmune disorders (clinical, latent or only autoantibodies) in patients with vitiligo. Dermatologica. 1985;171:419–23. doi: 10.1159/000249466. [DOI] [PubMed] [Google Scholar]
- 14.Kurtev A, Dourmishev AL. Thyroid function and autoimmunity in children and adolescents with vitiligo. J Eur Acad Dermatol Venereol. 2004;18:109–11. doi: 10.1111/j.1468-3083.2004.00728.x. [DOI] [PubMed] [Google Scholar]
- 15.Mason CP, Gawkrodger DJ. Vitiligo presentation in adults. Clin Exp Dermatol. 2005;30:344–5. doi: 10.1111/j.1365-2230.2005.01779.x. [DOI] [PubMed] [Google Scholar]
- 16.Shriya Dave, D’ Souza Mariette, Thappa Devinder Mohan, Reddy K. S, Bobby Zachariah Bobby. High Frequency of Thyroid Dysfunction in Indian Patients with Vitiligo. Indian J Dermatology. 2003;48:68–72. [Google Scholar]
- 17.Daneshpazhooh M, Mostofizadeh GM, Behjati J, Akhyani M, Robati RM. Anti-thyroid peroxidase antibody and vitiligo. A controlled study. BMC Dermatol. 2006;22:889–92. doi: 10.1186/1471-5945-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collin P, Reunala T. Recognition and management of the cutaneous cutaneous manifestations of celiac disease: A guide for dermatologist. Am J Clin Dermatol. 2003;4:13–20. doi: 10.2165/00128071-200304010-00002. [DOI] [PubMed] [Google Scholar]
- 19.Reunala T, Collin P. Diseases associated with dermatitis herpetiformis. Br J Dermatol. 1997;136:315–8. [PubMed] [Google Scholar]
- 20.Alkhateeb A, Fain PR, Thody A, Bennett DC, Spritz RA. Epidemiologyof vitiligo and associated autoimmune diseases in Caucasian probands and their families. Pigment Cell Res. 2003;16:208–14. doi: 10.1034/j.1600-0749.2003.00032.x. [DOI] [PubMed] [Google Scholar]
- 21.Akbari MR, Mohammadkhani A, Fakheri H, Javad Zahedi M. Screening of the adult population in Iran for coeliac disease: Comparison of the tissue-transglutaminase antibody and anti-endomysial antibody tests. Eur J Gastroenterol Hepatol. 2006;18:1181–6. doi: 10.1097/01.meg.0000224477.51428.32. [DOI] [PubMed] [Google Scholar]
- 22.Volta U, Bardazzi F, Zauli D, DeFranceschi L, Tosti A, Molinaro N, et al. Serological screening for coeliac disease in vitiligo and alopecia areata. Br J Dermatol. 1997;136:801–2. doi: 10.1111/j.1365-2133.1997.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 23.Leonard J, Haffenden G, Tucker W, Unsworth J, Swain F, McMinn R, et al. Gluten challenge in dermatitis herpetiformis. N Engl J Med. 1983;308:816–9. doi: 10.1056/NEJM198304073081406. [DOI] [PubMed] [Google Scholar]
- 24.Michaelsson G, Gerden B, Hagforsen E, Nilsson B, Pihl-Lundin I, Kraaz W, et al. Psoriasis patients with antibodies to gliadin can be improved by a gluten-free diet. Br J Dermatol. 2000;1:42–51. doi: 10.1046/j.1365-2133.2000.03240.x. [DOI] [PubMed] [Google Scholar]
- 25.Rodríguez-García C, González-Hernández S, Pérez-Robayna N, Guimerá F, Fagundo E, Sánchez R. Repigmentation of vitiligo lesions in a child with celiac disease after a gluten-free diet. Pediatr Dermatol. 2011;28:209–10. doi: 10.1111/j.1525-1470.2011.01388.x. [DOI] [PubMed] [Google Scholar]
- 26.Donaldson MR, Book LS, Leiferman KM, Zone JJ, Neuhausen SL. Strongly positive tissue transglutaminase antibodies are associated with Marsh 3 histopathology in adult and pediatric celiac disease. J Clin Gastroenterol. 2008;42:256–60. doi: 10.1097/MCG.0b013e31802e70b1. [DOI] [PubMed] [Google Scholar]
- 27.Seyhan M, Kandi B, Akbulut H, Selımoğlu MA, Karincaoğlu M. Is celiac disease common in patients with vitiligo. Turk J Gastroenterol. 2011;22:105–6. doi: 10.4318/tjg.2011.0169. [DOI] [PubMed] [Google Scholar]
- 28.Seyhan M, Erdem T, Ertekin V, Selimoglu MA. The mucocutaneous manifestations associated with celiac disease in childhood and adolescence. Pediatr Dermatol. 2007;24:28–33. doi: 10.1111/j.1525-1470.2007.00328.x. [DOI] [PubMed] [Google Scholar]


