Abstract
Background:
To test if social support and ethnicity mediate/moderate the association between religion involvement and subjective health in the United States.
Methods:
This is a secondary analysis of National Survey of American Life, 2003. Hierarchical regression was fit to a national household probability sample of adult African Americans (n = 3570), Caribbean Blacks (n = 1621), and Whites (n = 891). Frequency of church attendance, positive/negative church-based social support, ethnicity, and subjective health (overall life satisfaction and self-rated mental health) were considered as predictor, mediator, moderator and outcome, respectively.
Results:
Frequency of church attendance had a significant and positive association with mental health and life satisfaction among all ethnic groups. Frequency of church attendance was also correlated with positive and negative social support among all ethnic groups. Church-based social support fully mediated the association between frequency of church attendance and overall life satisfaction among African Americans but not among Caribbean Blacks, or Whites. Church-based social support, however, partially mediated the association between frequency of church attendance and overall mental health among African Americans but not among Caribbean Blacks or Whites.
Conclusion:
Ethnicity shapes how church-based social support mediates the association between religious involvement and subjective health. Our results showed a moderating mediation effect of ethnicity and social support on the religious involvement-subjective health linkage, in a way that it is only among African Americans that social support is a pathway for the beneficial health effect of religious involvement.
Keywords: Ethnicity, life satisfaction, mental health, religion involvement, social support, subjective health
INTRODUCTION
The protective effect of religious involvement on health has received a considerable amount of scholarly attention.[1] Higher religious involvement is associated with a wide range of physical health outcomes, including blood pressure,[2] immune function,[3] and also all-cause mortality.[4,5] McCullough et al. confirmed the association between religious involvement and higher longevity by a meta-analysis.[6]
Religious involvement is associated with both physical and mental health.[7,8] Frequency of church attendance is one of the proxies of religious involvement, which has been shown to be associated with a better mental health,[8] subjective well-being,[9] physical functioning,[10] and general health.[11–13]
More recently, the interest of scholarly researchers has shifted from the measurement of the association to searching for the active ingredients in the religious involvement (mediators), and also the characteristics that determine the degree of benefit of the religious involvement (moderators).[8,12,14] In other words, instead of asking about the effect of religious involvement on health, “how and when” questions are the subject of debate.[13]
Although social support and ethnicity have been shown to act as mediator and moderator of the above association, respectively,[12] we still need more data on the interplay between these factors on health. There are different reasons that justify the need for more studies on the relation between religious involvement, social support, and health in different ethnicities. Literature shows that organization and programmatic emphases within churches are ethnic specific and this may affect the religion–health link within each racial group. We already know that religious activity and participation clearly varies by ethnicity,[15] and the structure and mission of most congregations are often tailored to their constituents based on ethnicity.[16] Empirical data has also confirmed variation for the associations between religious participation and health across populations.[8,11] One example is the study by Krause,[12] which showed that in comparison to Whites, Blacks are more likely to receive the health-related benefits of religion.
By including ethnicity, religion involvement, positive and negative church-based social support and subjective health, this study tested the hypothesis that positive and negative support mediates the association between frequency of church attendance and subjective health [Figure 1]. We tested our model separately among Caribbean Blacks, African Americans, and non-Hispanic Whites to test if ethnicity is a moderator for this mediation.
Figure 1.
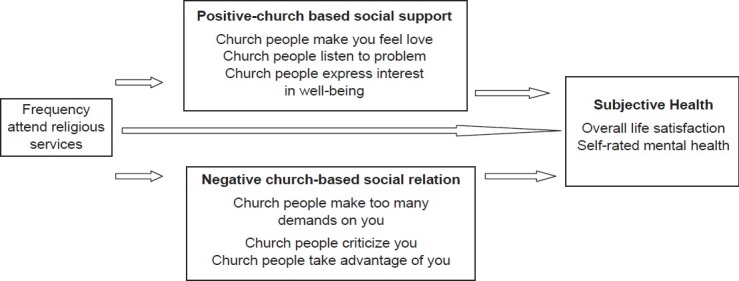
Conceptual model of the current study proposes that positive and negative church based social support may mediate the effect of church attendance on subjective health
METHODS
Survey
This was a secondary analysis of the National Survey of American Life (NSAL). NSAL data was collected by the Program for Research on Black Americans at the University of Michigan's Institute for Social Research from 2001 to 2003. Study design and sampling have been described in detail elsewhere (Jackson et al.[17]). The study has been approved by the University of Michigan Institutional Review Board.
Participants
A total of 6082 face-to-face interviews were conducted with persons aged 18 or older, including 3570 African Americans, 1621 Blacks of Caribbean descent, and 891 non-Hispanic Whites. The Black sample in this study is a national representative sample. We did not exclude any participant who was “not at all religious”. As earlier discussed by Krause (2000), those who report “not at all religious” may have abandoned religion as a result of the unpleasant interaction they encountered in church settings.
Interview
The interviews were face-to-face and conducted within participants’ homes. Participants received compensation for participating in this study. The overall response rate was 72.3%. Response rate was 70.7% for African Americans, 77.7% for Black Caribbeans, and 69.7% for non-Hispanic Whites.
Measures
Church attendance
Respondents were asked “How often do you usually attend religious services”? Would you say nearly every day, at least once a week, a few times a month, a few times a year, or less than once a year? The response items included: (1) Less than once a year, (2) A few times a year, (3) A few times a month – 1 to 3 times, (4) At least once a week – 1 to 3 times, and (5) Nearly every day – 4 or more times a week. We entered frequency of religious attendance to our model as a continuous variable, ranging from 1 to 5.
A meta-analysis has shown that health effect of religious behaviors such as church attendance may be stronger than that of religious attitudes (i.e. interest in or importance of religion).[18] Similar to our study, most previous studies in the field have used a single item measure of religious involvement frequent religious attendance.[19–22] However, researchers have differently operationalized religion involvement in their data analysis. Musick et al.[19] defined frequent attendees as individuals who report attending religious services once a month or more, and Strawbridge et al.,[20] and Hill et al.[21] have defined them as those who go to religious services once a week or more.
Self-rated life satisfaction
Respondents were asked “In general how satisfied are you with your life as a whole these days? Would you say that you are very satisfied, somewhat satisfied, somewhat dissatisfied, or very dissatisfied?” Responses included four items from very satisfied, somewhat satisfied, somewhat dissatisfied, and very dissatisfied.
Self-rated mental health
Participants were asked “How would you rate your overall mental health – excellent, very good, good, fair, or poor”? Responses included five items from excellent, very good, good, fair, and poor. Higher score means a better overall mental health.
McDowell reviewed applications of the single-item health indicators in 2010 and reported that single items have been applied to several aspects of health and well-being including life satisfaction.[23] As empirical studies have shown that such questions are capable of explaining variance in mortality, even after adjustment for conventional risk factors and other clinical information, they are frequently used in surveys. The US Institute of Medicine has considered them within the list of national health outcome indicators.[24]
There are several formats for measuring single items for subjective health.[25–28] The fifth variant of these questions (Summary Self-Rating Question) as categorized by McDowell is a common format and has been used here.[29] This format has been frequently used previously.[30–32] Test retests reliability for single items range from 0.7 to 0.8 for brief time intervals.[29] Validity results commonly have shown surprisingly high correlations between single-item indicators and much longer scales. Convergent correlations have been reported with life satisfaction scales, with anxiety and depression measures, and with general health measures such as the Health Utilities Index. Correlations range from 0.5 to around 0.75, suggesting that a substantial amount of the variance in much longer scales can be captured by a single question.[29] Numerous longitudinal studies have confirmed predictive validity associations between self-rating scores and subsequent mortality, even after controlling for other risk factors. Idler and Benyamini[24] showed that 23 of 27 studies reported that a self-rating question explained variance in mortality after controlling for age, socioeconomic status, and in several studies, chronic conditions and selected medical risk factors.
These single-item scales are attractive for surveys because they are cost-effective and simple to apply. Some respondents have difficulty in merging multiple issues into a single average rating. These items may be prone to response shift especially when the question is phrased in terms of comparisons with other people their age.[31,32] These scales are also more sensitive than multi-item scales to contextual effects from the preceding questions in a survey.[29]
Positive church-based social support
This was measured by three items. Respondents were asked ‘How often do the people in your church (1) make you feel loved and cared for, (2) listen to you talk about your private problems and concerns, and (3) express interest and concern in your well-being?’ Response categories range from “very often’ to ‘never’ with higher values on this index indicating higher levels of emotional support. Cronbach's alpha for this 3-item index is 0.72.
Negative church-based social support
Negative interaction is also measured by an index of three items. Respondents were asked ‘Other than your (spouse/partner) how often do your church members: (1) make too many demands on you?, (2) criticize you and the things you do?, and (3) try to take advantage of you?’ The response categories for these questions were ‘very often’, ‘fairly often’, ‘not too often’, and ‘never’. Higher values on this index indicate higher levels of negative interaction with family members (Cronbach's alpha = 0.75).
Statistical note
First we estimated the measure of association between frequency of church attendance, positive and negative church-based social support, and subjective health. Then, for each outcome and each ethnicity, a hierarchical regression model was applied to test the study hypothesis. 95% confidence intervals (95% CI) were reported for Beta. Standard Errors were estimated using Jacknife replication method. To adjust for weights and complex design, Stata 12.0 was used for statistical analysis and P less than 0.05 was considered as statistically significant.
RESULTS
Frequency of church attendance was significantly associated with higher life satisfaction among all ethnic groups. Frequency of church attendance was significantly correlated with positive and negative social support among all ethnicities.
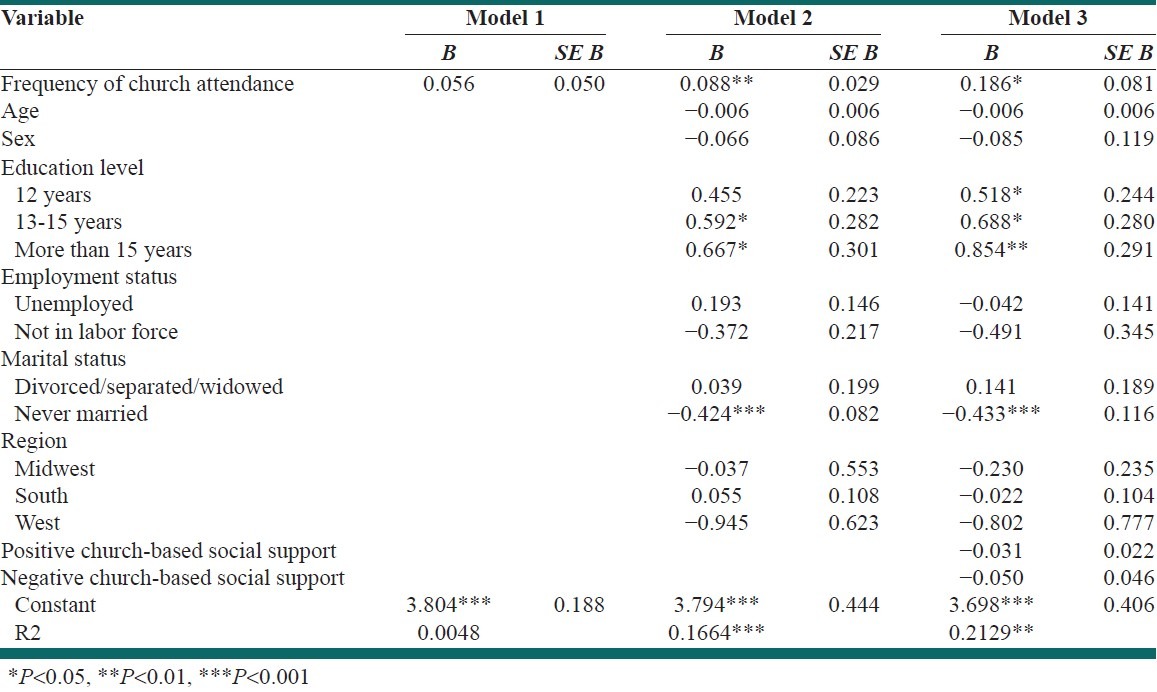
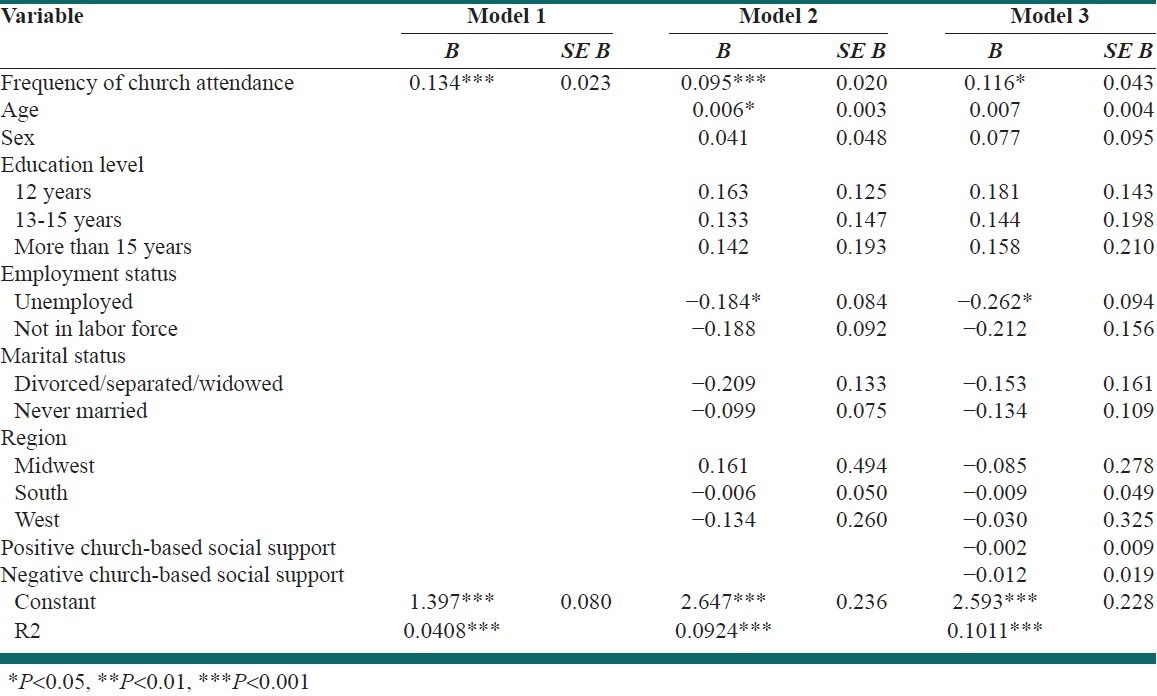
Self-rated mental health among Afro-Caribbeans
As Table 1 shows, among Afro-Caribbeans, frequency of church attendance was not a significant predictor of Self-rated mental health in the first model. However, in all other models, it remained a significant predictor of our outcome. Positive and negative social support neither significantly correlated with self rated mental health, nor did it mediate its association with frequency of church attendance. Our final model, which was statistically significant, explained 21% of the variance of this outcome in this population.
Table 1.
Summary of hierarchical regression models of self-rated mental health among Afro-Caribbeans
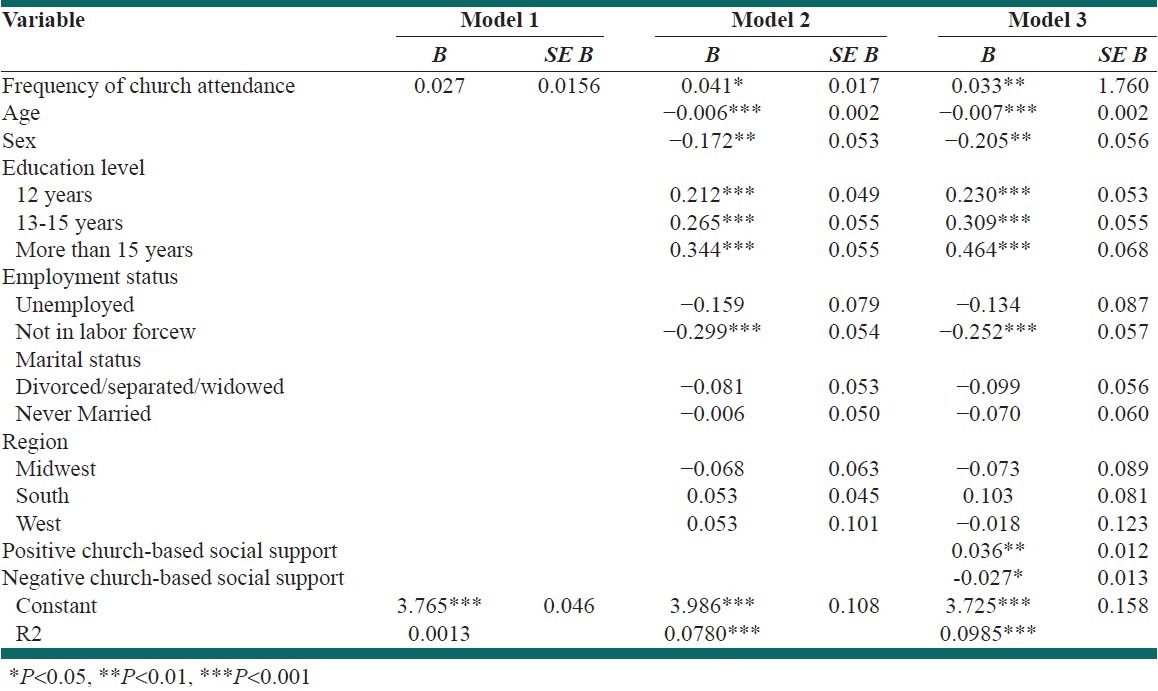
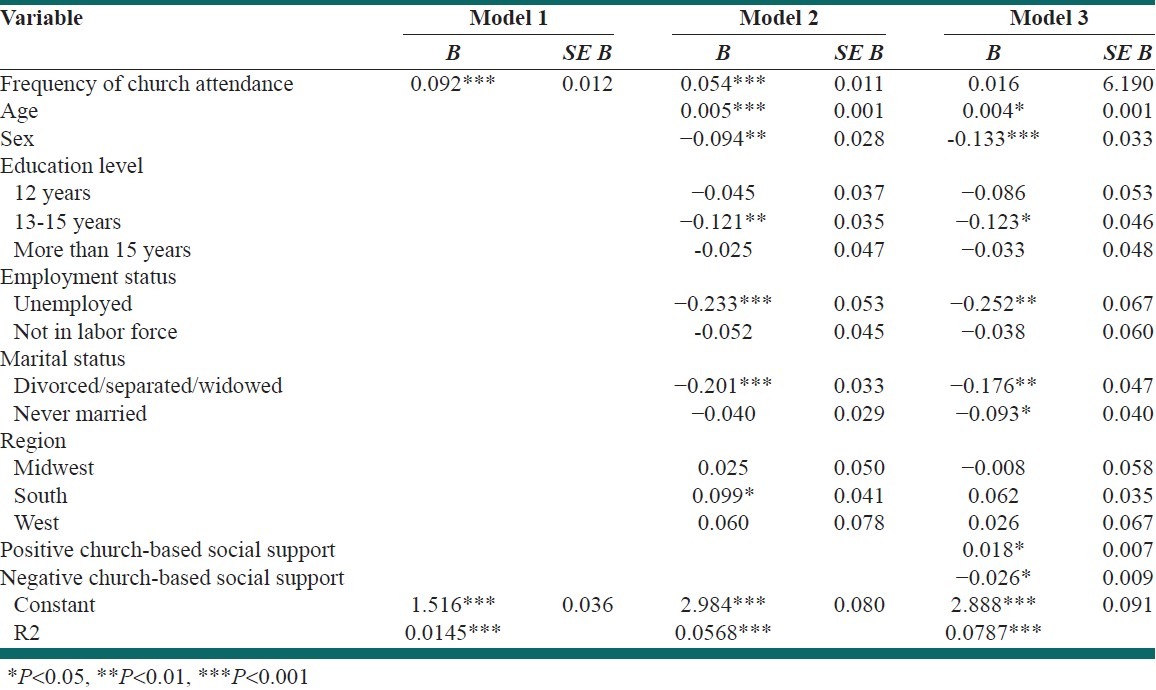
Self rated physical health among African Americans
Among African Americans, frequency of church attendance was a significant predictor of self-rated mental health in all of our models. In our final model, both positive and negative church-based social Support were significantly associated with self-rated physical health. There was not enough evidence to show negative church-based social support mediates our association of interest. Our final model, which was statistically significant, explained 9.8% of the variance of self-rated mental health among African Americans [Table 2].
Table 2.
Summary of hierarchical regression models of self-rated mental health among African Americans
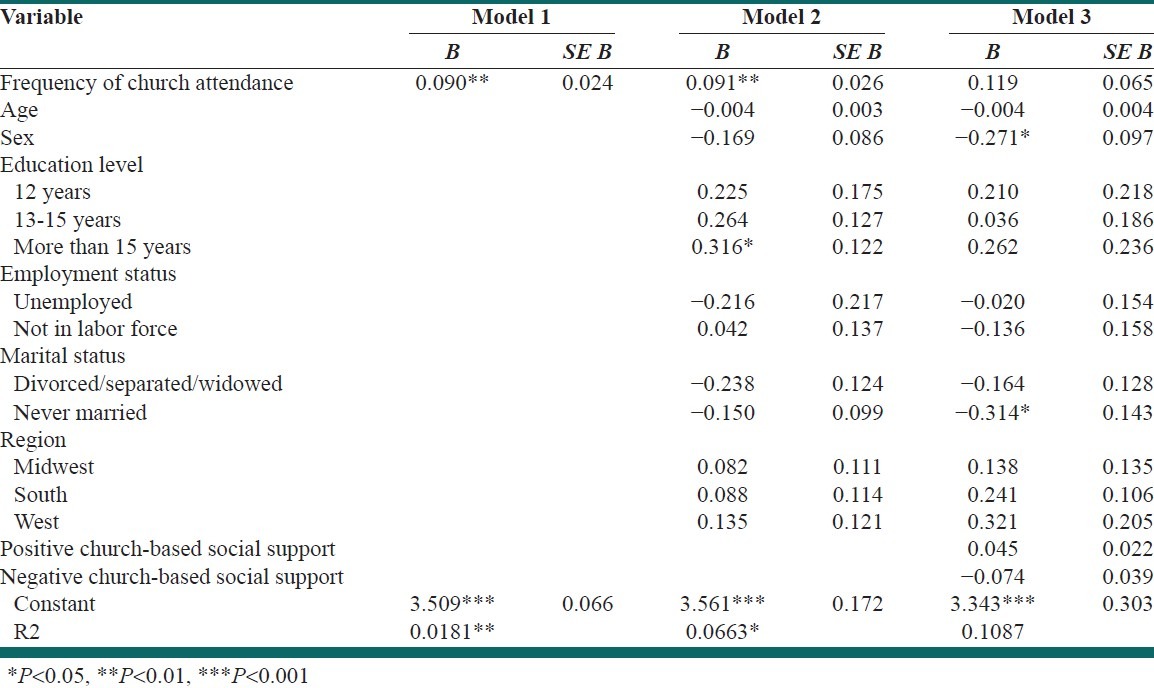
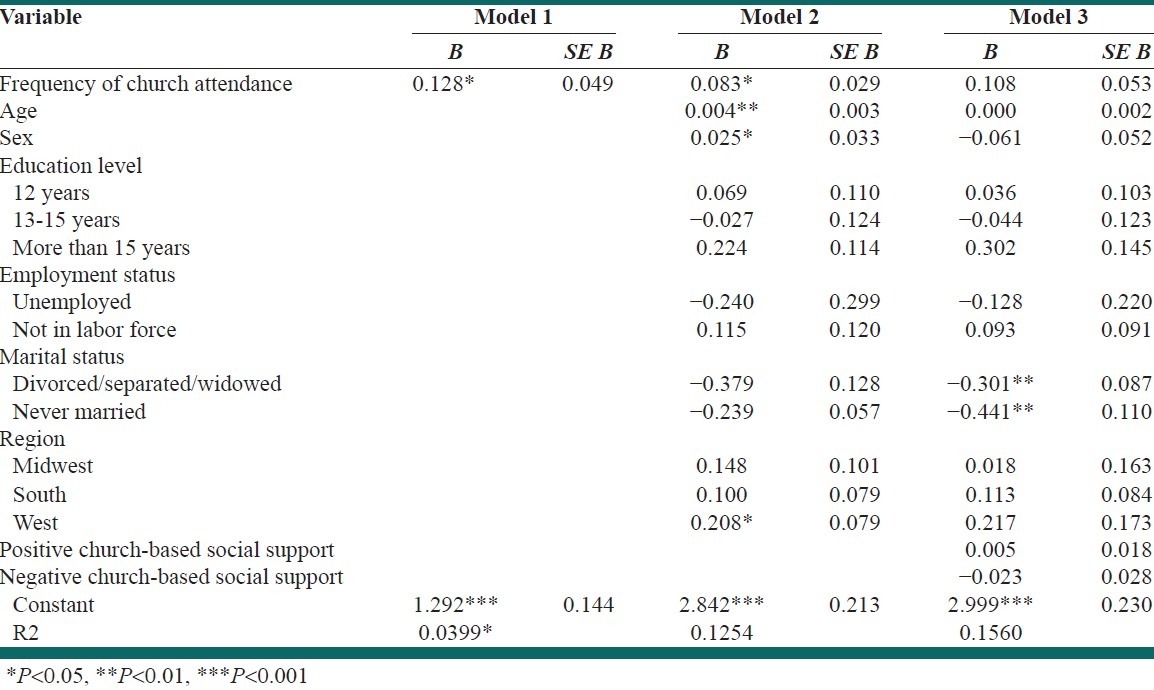
Self-rated mental health among non-Hispanic Whites
Among non-Hispanic Whites, frequency of church attendance became a predictor of self-rated mental health in our first and second but not final model. In our final model, neither frequency of church attendance, nor positive or negative church-based social support were significantly associated with self-rated mental health. The first and the second, but not the last model, were statistically significant [Table 3].
Table 3.
Summary of hierarchical regression models of self-rated mental health among non-Hispanic Whites
Overall life satisfaction among Afro-Caribbeans
As depicted in Table 4, among Afro-Caribbeans, frequency of church attendance was a significant predictor of overall life satisfaction in all models. Positive and negative social support were not significantly correlated with overall life satisfaction. Our final model, which was statistically significant, explained 10.1% of the variance of the outcome.
Table 4.
Summary of hierarchical regression models of overall life satisfaction among Afro-Caribbeans
Overall life satisfaction among African Americans
Among African Americans, frequency of church attendance was a significant predictor of overall life satisfaction in first and second but not the last model. Positive and negative social support were significantly correlated with overall life satisfaction and they fully mediated the association between frequency of church attendance and overall life satisfaction. All models were statistically significant and the final one explained 7.8% of the variance of the outcome [Table 5].
Table 5.
Summary of hierarchical regression models of overall life satisfaction among African Americans
Overall life satisfaction among non-Hispanic Whites
Among non-Hispanic Whites, frequency of church attendance was a predictor of overall life satisfaction in our first and second but not final model. In our final model, neither frequency of church attendance, nor positive or negative church-based social support were significantly associated with self-rated mental health. Only the first and second models, but not the last model, were statistically significant [Table 6].
Table 6.
Summary of hierarchical regression models of overall life satisfaction among non-Latino Whites
DISCUSSION
This study showed that church-based social support is a mediator for religion among African Americans. Our study suggested that such a pathway may not necessarily work for Afro-Caribbeans and Whites. By other means, based on the findings of the current study, mediating role of church-based social support depends on ethnicity. This seems important because most of the literature tends to include all ethnicities of Blacks and use Blacks and African Americans interchangeably.
We documented a full mediation of the association between frequency of church attendance and overall life satisfaction by church-based social support only among African Americans but not among Caribbean Blacks or White Americans. Lincoln et al.[33] argued the possibility that social and psychological factors may operate differently within specific racial and ethnic groups. It is not necessarily the salience of a particular variable that explains how race and ethnicity may be linked to health and well-being, but rather the unique manner with which social and psychological processes operate for distinct racial and ethnic groups. In National Comorbidity Survey, for Whites negative interaction and for African Americans positive social support were stronger predictors of psychological distress, respectively.
The assumption of “the similarity between African Americans and Whites” may be the result of absence of studies on race/ethnic differences. Previous authors have argued that similar studies need to compare different racial and ethnic groups by running similar models to different ethnicities to look for possible differences.[31,32,34] Lincoln et al. argues that failure to account for the social and cultural factors that characterize the life circumstances of African Americans and other racial/ethnic groups fosters the unfounded belief that social theories and models are equivalent across groups. They argued that the unique social and cultural conditions evident within each ethnic group may constitute specific risk and protective factors that are essential for understanding the nature and patterns of social interaction and how they interrelate with other factors to influence health outcomes.[33]
Studies have shown that higher social support is associated with better physical and mental health.[35] The literature has proposed many mechanisms for favorable effects of positive social support including but not limited to the buffering effect of social support on stress. Social support from others can also help individuals to redirect the negative impact from stressors by helping to evaluate the situation as one that is not beyond the individual's control and help provide positive solutions to the problem. This process further increases the individual's estimation of self.[34] Those who attend church more frequently will spend more time with church-based fellows as a way to temporarily remove oneself From stressful situations and will have more opportunity to talk about their problems. This study, however, did not measure stress.
Social interactions may play a unique role in general well-being of the human, easily because human being is a social species.[36] Ability to share ideas, hopes and dreams with similar others, or with those who would serve as mentors, is pivotal in the attainment of mastery or a sense of control over one's own environment. Similarly, when material resources are scarce, the provision of shared resources from others who understand can ease the tensions that accompany economic hardship. However, if the material help is accompanied by harsh criticism or a condescending, blame-ridden attitude, the receiver of such help is more likely to perceive the material help received as a judgment against her own weakness or inability to take care of her own responsibilities, rather than as a true “helping hand”.[33]
Interestingly, different theories may explain the effect of the same constructs on health. For instance, working on religiosity and social support on Whites and Blacks, one study Has shown that social support hypothesis can explain the protective effect of social support on health similarly among Blacks and Whites, however, it seems that religious consolation hypothesis only can be supported among Blacks.[37] Again, although further research is needed in this area, we already know that Blacks and Whites have different network transactions in their networks,[38,39] which is in part related to their different network composition.[40,41]
To conclude, ethnicity may shape how church-based social interaction translates to better subjective health of people. Social support mediates the religion involvement – health linkage among African Americans, but this mediation does not exist among Afro-Caribbeans and non-Hispanic Whites. Thus, any program using church-based social support to increase subjective health, should consider ethnicity.
ACKNOWLEDGMENT
This was a secondary analysis on public-access data set of National Survey of American Life (NSAL). NSAL is mainly funded by National Institute of Mental Health (NIMH), and has been conducted by the Institute of Social Research, University of Michigan. Data was downloaded from Interuniversity Consortium for Political and Social Research (ICPSR), University of Michigan.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Levin JS, Chatters LM. Religion, health, and psychological well- being: Findings from three national surveys. J Aging Health. 1998;10:504–31. doi: 10.1177/089826439801000406. [DOI] [PubMed] [Google Scholar]
- 2.Koenig HG, George LK, Hays JC, Larson DB, Cohen HJ, Blazer DG. The relationship between religious activities and blood pressure in older adults. Int J Psychiatry Med. 1998;28:189–213. doi: 10.2190/75JM-J234-5JKN-4DQD. [DOI] [PubMed] [Google Scholar]
- 3.Koenig HG, Cohen HJ, George LK, Hays JC, Larson DB, Blazer DG. Attendance at religious services, interleukin-6, and other biological indicators of immune function in older adults. Int J Psychiatry Med. 1997;27:233–50. doi: 10.2190/40NF-Q9Y2-0GG7-4WH6. [DOI] [PubMed] [Google Scholar]
- 4.Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and US Adult mortality. Demography. 1999;36:273–85. [PubMed] [Google Scholar]
- 5.Oman D, Kurata JH, Strawbridge WJ, Cohen RD. Religious attendance and cause of death over 31 years. Int J Psychiatry Med. 2002;32:69–89. doi: 10.2190/RJY7-CRR1-HCW5-XVEG. [DOI] [PubMed] [Google Scholar]
- 6.McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: A meta-analytic review. Health Psychol. 2000;19:211–22. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 7.Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: Linkages to physical health. Am Psychol. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 8.Chatters LM, Taylor RJ, Jackson JS, Lincoln KD. Religious coping among African Americans, caribbean blacks and non-hispanic whites. J Community Psychol. 2008;36:371–86. doi: 10.1002/jcop.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ardelt M. Effects of religion and purpose in life on elders’ subjective well-being and attitudes toward death. J Relig Gerontol. 2003;14:55–77. [Google Scholar]
- 10.Idler E, Kasl S. Religion, disability, depression, and the timing of death. Am J Sociol. 1992;97:1052–79. [Google Scholar]
- 11.Drevenstedt G. Race and ethnic differences in the effects of religious attendance on subjective health. Rev Relig Res. 1998;39:245–63. [Google Scholar]
- 12.Krause N. Church-based social support and health in old age: Exploring variations by race. J Gerontol B Psychol Sci Soc Sci. 2002;57:S332–47. doi: 10.1093/geronb/57.6.s332. [DOI] [PubMed] [Google Scholar]
- 13.Levin S, Markides KS. Religion and health in Mexican Americans. J Relig Health. 1985;24:60–9. doi: 10.1007/BF01533260. [DOI] [PubMed] [Google Scholar]
- 14.Ross K, Handal PJ, Clark EM, Vander Wal JS. The relationship between religion and religious coping: Religious coping as a moderator between religion and adjustment. J Relig Health. 2009;48:454–67. doi: 10.1007/s10943-008-9199-5. [DOI] [PubMed] [Google Scholar]
- 15.Chaves ML, Higgins M. Comparing the community involvement of black and white congregations. J Sci Study Relig. 1992;31:425–40. [Google Scholar]
- 16.Ammerman N. Tatom bible believers: Fundamentalists in the modern world. New Jersey: Rutgers University Press; 1987. [Google Scholar]
- 17.Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The national survey of American life: A study of racial, ethnic and cultural influences on mental disorders and mental health. Int J Methods Psychiatr Res. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Witter RA, Stock WA, Okun MA, Haring MJ. Religion and subjective well-being in adulthood: A quantitative synthesis. Rev Relig Res. 1985;26:332–42. [Google Scholar]
- 19.Musick MA, House JS, Williams DR. Attendance at religious services and mortality in a national sample. J Health Soc Behav. 2004;45:198–213. doi: 10.1177/002214650404500206. [DOI] [PubMed] [Google Scholar]
- 20.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87:957–61. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill TD, Angel JL, Ellison CG, Angel RJ. Religious attendance and mortality: An 8-year follow-up of older Mexican Americans. J Gerontol B Psychol Sci Soc Sci. 2005;60:S102–9. doi: 10.1093/geronb/60.2.s102. [DOI] [PubMed] [Google Scholar]
- 22.Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health practices, mental health, and stable marriages. Ann Behav Med. 2001;23:68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- 23.Headey BW, Kelley J, Wearing AJ. Dimensions of mental health: Life satisfaction, positive affect, anxiety, and depression. Soc Indic Res. 1993;29:63–82. [Google Scholar]
- 24.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 25.Andrews FM. Social indicators of perceived life quality. Soc Indic Res. 1974;1:279–99. [Google Scholar]
- 26.Andrews FM, Crandall R. The validity of measures of self-reported well-being. Soc Indic Res. 1976;3:1–19. [Google Scholar]
- 27.Knäuper B, Turner PA. Measuring health: Improving the validity of health assessments. Qual Life Res. 2003;12:81–9. doi: 10.1023/a:1023589907955. [DOI] [PubMed] [Google Scholar]
- 28.Verbrugge LM. A global disability indicator. J Aging Stud. 1997;11:337–62. [Google Scholar]
- 29.McDowell I. Measuring health: A guide to rating scales and questionnaires. 3rd ed. New York: Oxford University Press; 2006. [Google Scholar]
- 30.Bélanger A, Berthelot JM, Guimond E, Houle CA. Head-to-head comparison of two generic health status measures in the household population: McMaster Health Utilities Index (Mark3) and the EQ-5D. Ottawa, Canada: Statistics Canada Report; 2002. pp. 1–62. [Google Scholar]
- 31.McDowell I. Measures of self-perceived well-being. J Psychosom Res. 2010;69:69–79. doi: 10.1016/j.jpsychores.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Hunt MO. The Individual, society, or both.? A comparison of black, latino, and white beliefs about the causes of poverty. Soc Forces. 1996;75:293–332. [Google Scholar]
- 33.Lincoln KD, Chatters LM, Taylor RJ. Psychological distress among black and white Americans: Differential effects of social support, negative interaction and personal control. J Health Soc Behav. 2003;44:390–407. [PMC free article] [PubMed] [Google Scholar]
- 34.Hunt MO, Jackson PB, Powell B, Steelman LC. Color- blind: The treatment of race and ethnicity in social psychology. Soc Psychol Q. 2000;63:352–64. [Google Scholar]
- 35.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–84. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 36.Portes A. Social capital: Its origins and application in modern sociology. Annu Rev Sociol. 1998;24:1–14. [Google Scholar]
- 37.Ferraro KF, Koch JR. Religion and health among black and white adults: Examining social support and consolation. J Sci Study Relig. 1994;33:362–75. [Google Scholar]
- 38.Mutran E. Intergenerational family support among blacks and whites: Response to culture or to socioeconomic differences. J Gerontol. 1985;40:382–9. doi: 10.1093/geronj/40.3.382. [DOI] [PubMed] [Google Scholar]
- 39.Strogatz DS, James SA. Social support and hypertension among blacks and whites in a rural, southern community. Am J Epidemiol. 1986;124:949–56. doi: 10.1093/oxfordjournals.aje.a114484. [DOI] [PubMed] [Google Scholar]
- 40.Taylor RJ, Chatters LM, Jackson JS. Changes over time in support network involvement among black Americans. In: Taylor RJ, Jackson JS, Chatters LM, editors. Family life in black America. Thousand Oaks CA: Sage Publications; 1997. pp. 293–316. [Google Scholar]
- 41.Billingsley A. Climbing jacob's ladder: Enduring legacy of African American families. New York: Simon and Schuster; 1992. [Google Scholar]


