Abstract
Background:
Phantom limb pain (PLP) is approximately a common condition after limb amputation, which potentially affects the quality of life. We aimed to evaluate anxiety and depression in patients with amputated limbs suffering from PLP and to compare these psychological dysfunctions with that of patients with non-phantom chronic pain.
Methods:
A total number of 16 male amputees with PLP and 24 male age-matched patients with non-phantom chronic pain were recruited in this study, which was performed at Khatam-Al-Anbia Pain Clinic, Tehran, Iran. A validated Persian version of the hospital anxiety and depression scale (HADS) was used to compare two psychological dysfunctions – anxiety and depression – between the two groups of study.
Results:
The mean of total anxiety score was significantly lower in patients with PLP (8.00 ± 3.93 vs. 11.25 ± 5.23; P = 0.041) and the prevalence of anxiety caseness (HADS-A score ≥ 11) was also lower in the PLP group (25% vs. 58.3%; P = 0.112, power = 31.7%). The mean of total depression score was 7.69 ± 5.51 and 9.38 ± 6.11 in patients of PLP and chronic pain groups, respectively (P = 0.340, power = 15%). Consequently, the prevalence of depression caseness (HADS-D score ≥ 11) was lower in PLP patients (37.5% vs. 50%; P = 0.710, power = 8%).
Conclusion:
Our results indicate that depression and anxiety are not more common in PLP patients, whereas they are more prevalent in subjects with non-phantom chronic pain. These lower levels of anxiety and depression in PLP compared with chronic pain is a new finding that needs to be evaluated further, which may lead to new insights into the pathogenesis of phantom pain in further studies.
Keywords: Anxiety, chronic pain, depression, hospital anxiety and depression scale, phantom limb pain
INTRODUCTION
Phantom limb pain (PLP) is classified as a kind of neuropathic pain that is induced after nerve injury. It is an after effect of amputation occurring in up to 50-85% of the patients,[1–3] and often leads to significant impairment in occupational and social functioning.[4] Daily pain is reported by 48% of patients with PLP[5] and it is supposed that these symptoms potentially affect their quality of life. More importantly, emotional factors are influential in patients’ experience of prolonged pain in a phantom limb after amputation.[6] On the one hand, it is likely that phantom pain develops poor health-related quality of life such as emotional problems including anxiety and depression. On the other hand, it is also possible that poor quality of life due to emotional problems induces phantom pain[7] and some conditions, such as anxiety and depression, may themselves worsen PLP.[1,8–10]
Although some psychological investigations have been performed in patients suffering from PLP, controversial findings have been reported. Although multiple psychological modalities have been attempted in managing PLP[11–19] and psychotherapy was reported to yield good results,[11] Katz and Melzack[20] found no significant difference in standardized tests of psychological dysfunction between patients who experienced phantom pain and those who did not. They concluded that the pain is more likely to vary with the experience of pre-amputation pain, even retaining many of its characteristics. A review of the literature on measures used to diagnose psychopathology found that many measures include items that confound emotional distress with the physical disorder and thus overestimate it.[21,22]
The Hospital Anxiety and Depression Scale (HADS)[23] is a popular instrument among researchers from different nations and cultures. It is estimated that since the period 1996-2002, the number of HADS papers that have been published has increased almost fourfold.[24] A recent review of the literature on the validity of HADS clearly indicates that it is a well-performed questionnaire in assessing the symptom severity and caseness of anxiety disorders and depression in somatic, psychiatric, and primary care patients and even in the general population. However, the prevalence and severity of these psychological dysfunctions have not been compared in PLP patients with other chronic pain sufferers. Previous comparative studies have focused on the comparison of psychiatric disorders in PLP patients with non-pain amputees in which the effect of pain itself was assessed.[20,22] Therefore, the aim of our study was to evaluate anxiety and depression in patients with amputated limbs suffering from phantom pain and to compare these psychological disorders with those of patients with non-phantom chronic pain using the HADS questionnaire. Thus, in contrast to previous investigations, it could be possible to evaluate the effect of amputation instead of the pain itself.
METHODS
Patients’ enrollment
This prospective analytical cross-sectional study was conducted in Khatam-Al-Anbia Pain Clinic, Tehran, Iran, between 2008 and 2010. A total number of 16 male amputees consecutively participated in the study as the PLP group. For this purpose, patients with upper and lower limb amputations between the ages of 25 years and 65 years with traumatic amputations and with PLP (at least five points on a Visual Analogue Scale [VAS] for at least 3 months) were included. PLP was defined as pain perceived at parts of an extremity that were no longer present. Therefore, the presence of PLP and phantom sensation was based on the answers to the following questions: (i) Do you feel the amputated part of your limb? (ii) Do you feel pain in the amputated part of your limb? If the answer to the second question was “yes” the severity of the pain was investigated using the VAS (0-10 cm).
As a control group, 24 male age-matched patients who were experiencing non-phantom chronic pain were recruited and evaluated at the same period of time. Those eligible were men aged 25 years or older with neuropathic pain of at least 3 months in duration caused by trauma or surgery, with allodynia or hyperalgesia, and with an average weekly pain intensity score greater than five on a 10 cm VAS.
It must be noted that all of the patients were administered the same analgesic protocol, had a stable analgesic regimen, and were followed in the Khatam-Al-Anbia Pain Clinic. The study was approved by the medical ethics committee of Khatam-Al-Anbia Hospital. Patients were told that their data and the results of their assessment were being using for research purposes, and each patient provided written informed consent.
Baseline assessment
After each patient fulfilled the eligible criteria, a list of demographic, baseline, and pain characteristics were asked, which were recorded at the time of enrollment. These variables consisted of age, marital status, educational level, body mass index (BMI), and pain characteristics including duration, average, highest and lowest intensity, and aggravating factors (e.g., somatic, psychotic, prolonged fix position, changed position, prolonged rest).
Pain intensity measurements were taken at baseline for all of the 40 recruited patients using a 10 cm VAS.[25] The patients were instructed to record the highest, the lowest, and the average intensity of their pain within the last 4 weeks prior to the study enrollment. They were asked to point out each intensity on a 10 cm VAS, which theoretically ranged between 0 and 10, where 0 indicates no pain and 10 corresponds to the worst pain imaginable. All the assessments were conducted by the same physician.
Psychological assessment
The HADS was used to assess two psychological dysfunctions – anxiety and depression – in two groups of the patients. It has been shown that HADS provides clinically meaningful results as a psychological screening tool, in clinical group comparisons and in studies with several aspects of disease and quality of life. As mentioned previously, the validity of this questionnaire was previously evaluated and it was indicated that HADS is a well-performed questionnaire in assessing the symptom severity and caseness of anxiety disorders and depression in chronic pain sufferers.
The Persian version of the HADS questionnaire was first validated by Montazeri et al. in 2003.[26] They showed that the Iranian version of the HADS questionnaire was generally acceptable to almost all patients. Checking the reliability of the HADS, Cronbach's alpha coefficient was found to be 0.78 for the anxiety subscale and 0.86 for the depression subscale. Using the known groups’ comparison and convergent analysis, the Persian version of the HADS questionnaire was shown to be valid. Moreover, both anxiety and depression subscales discriminated well between subgroups of their sampled patients with different statuses.
The HADS questionnaire contains 14 items and consists of two subscales: Anxiety and depression. Each subscale consists of seven items, where the odd-numbered questions belong to the anxiety subscale (HADS-A) and the even items belong to the depression subscale (HADS-D). Each item is rated on a four-point scale (scored between 0 and 3), giving maximum scores of 21 for anxiety and depression. The higher the score, the more severe the psychological dysfunction. In addition, the total score of each subscale could be categorized using some cutoff points. Scores of 11 or more on either subscale are considered to be a significant ‘case’ of psychological morbidity, whereas scores of 8-10 represent ‘borderline’ and 0-7 represent ‘normal’.[27] All the 40 participants were asked to complete the HADS questionnaire, following which the scores were calculated for each subscale for each patient.
Statistical analysis
A sample size of 16 patients in each group was calculated to detect a difference of two units in the total score of the HADS questionnaire in each subscale with an estimation of 5% for type I error and 20% for type II error based on a two-sided Independent Samples t-test.
Descriptive statistics were used to determine frequency and percentage for categorical variables, and mean and standard deviation (SD) for continuous measurements. After checking the normal distribution with the Kolmogorov-Smirnov test, the differences in patient characteristics and HADS scores (including each item and total scores) between the PLP group and non-phantom chronic pain patients were analyzed with the Mann–Whitney U test, Independent Samples t-test, Fisher's Exact test, and the Chi-square test, as appropriate. A P value of 0.05 or less was considered statistically significant for all analyses. Analyses were performed with the Statistical Package for the Social Sciences, version 16 (SPSS Inc., Chicago, IL, USA).
RESULTS
Baseline characteristics
Sixteen male patients with PLP and 24 age-matched males who suffered from non-phantom chronic pain were recruited in this study. A complete list of demographic, baseline, and pain characteristics of the patients are shown in Table 1. The mean age of the patients with PLP was 48.88 ± 7.47 year, which was similar to that of chronic pain sufferers (48.63 ± 9.42 year, P = 0.930). Most of the patients in both the groups were married and educated. Other baseline characteristics including marital and educational statuses are summarized in Table 1.
Table 1.
Comparison of the baseline and pain characteristics between the two groups of the study
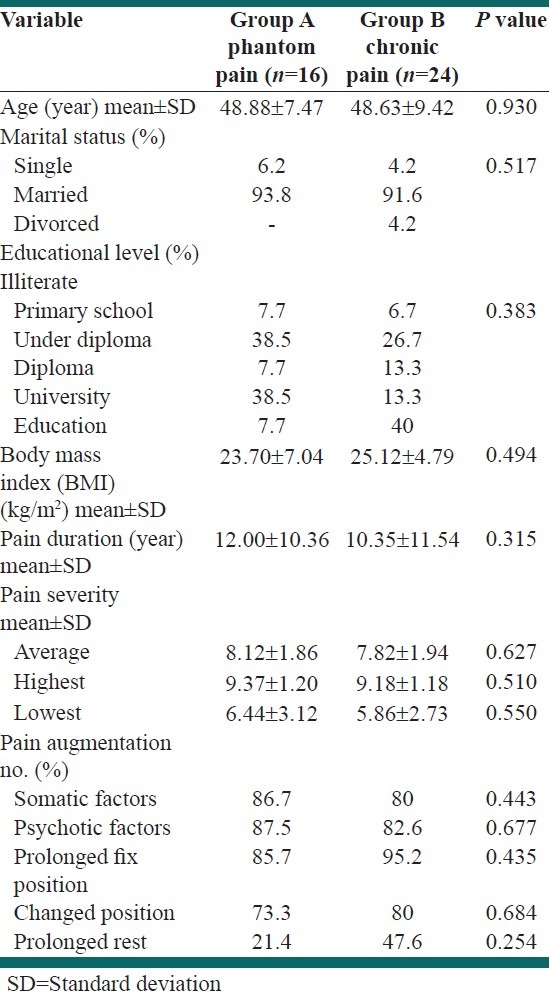
Regarding pain characteristics, the mean duration of pain was 12.00 ± 10.36 year in PLP patients, which was not significantly different from the pain duration in the other group (10.35 ± 11.54 year, P = 0.315). Using VAS, the mean of the average severity of pain was found to be 8.12 ± 1.86 and 7.82 ± 1.94 in phantom pain and non-PLP patients, respectively (P = 0.627). Although psychotic factors were the most involved pain-aggravating factors in the PLP group (87.5%), prolonged fix position was more responsible for worsening of pain in patients of Group B (95.2%). Other pain characteristics are listed in Table 1.
Anxiety
The results of HADS scores in each item and overall anxiety and depression status are shown and compared between the two groups of the study in Table 2. As is seen, the mean of HADS scores for each of the seven items of anxiety (HADS-A) is higher in patients of group B who suffered from non-PLP chronic pain, which is in favor of a more severe anxiety. Consequently, the mean of total anxiety score was significantly lower in patients with PLP (8.00 ± 3.93 vs. 11.25 ± 5.23; P = 0.041).
Table 2.
Comparison of the hospital anxiety and depression scale scores in each item and overall anxiety and depression status between two groups of the study
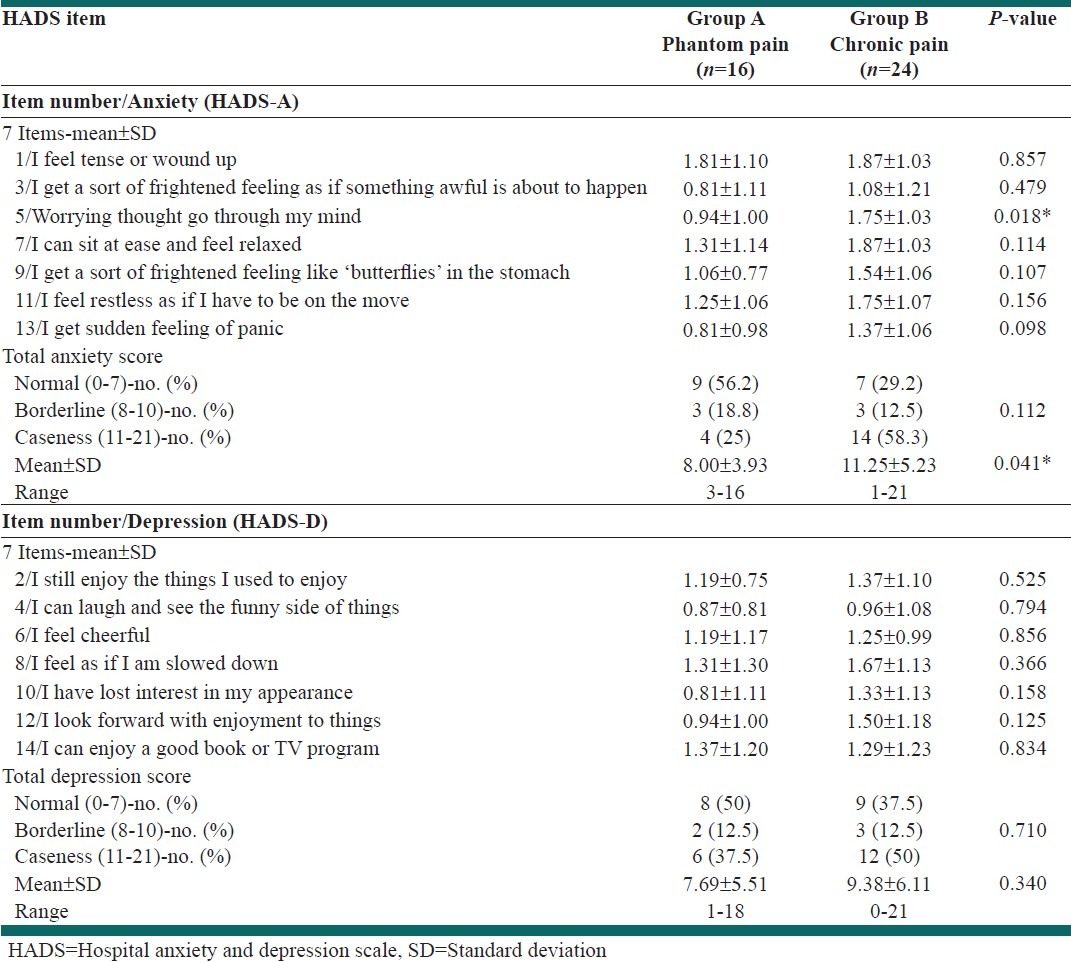
Moreover, when the total anxiety score is categorized using the proposed cutoff points of previous studies,[27] the prevalence of anxiety caseness (HADS-A score ≥ 11) was found to be higher in chronic pain sufferers (58.3% vs. 25%; P = 0.112, power = 31.7%).
Depression
As listed in Table 2, except for item number 14, the other HADS scores of six items in the depression subcategory (HADS-D) were also higher in patients with non-phantom chronic pain, which was in favor of a more severe depressed mood. The mean of total depression score was 7.69 ± 5.51 and 9.38 ± 6.11 in patients of the PLP and chronic pain groups, respectively. However, this difference was not statistically significant ( P = 0.340, calculated power = 15%).
When the total depression score is categorized using the proposed cutoff points of previous studies,[27] the prevalence of depression caseness (HADS-D score ≥ 11) was also found to be lower in patients with phantom pain (37.5% vs. 50%; P = 0.710, power = 8%).
DISCUSSION
As an approximately common condition after limb amputation, PLP serves as a disabling chronic pain syndrome for which regular pain treatment is seldom effective. This painful condition may be the result of inappropriately stored or chronically activated pain memories that continue to disturb the subject even after the disease or injury has been successfully treated or the limb has been amputated.[28–31] On the other hand, it seems that both the amputation of a limb and the consequent phantom pain may affect quality of life, especially with regard to psychological functions. The incidence of anxiety and depression symptoms after amputation has been reported to be 37% and 20%,[32] respectively, and even as high as 41%[33–36] and much higher than the rates in the community.[37,38] Alongside these considerable prevalence rates, there are some other evidences that show these psychological dysfunctions are not more prevalent among those amputees reporting phantom pain. Moreover, research in this field is difficult because of the different measurement tools used for anxiety and depression as well as the lack of prospective studies.[4] In the present study, it was hypothesized that the prevalence rates and scores of anxiety and depression could be more common in patients with PLP compared with non-phantom chronic pain sufferers. Regarding the proposed cutoff points for the caseness of anxiety and depression in the HADS questionnaire, 25% and 37.5% of our patients with PLP fulfilled the criteria, respectively. These prevalence rates were in agreement with the current reports[33–36] . Nevertheless, our results indicate that depression and anxiety are more common in PLP patients, and these conditions are more prevalent in non-phantom chronic pain sufferers.
In 1973, Parkes suggested that emotional and psychological factors are dominant in patients’ with prolonged pain due to phantom limb after amputation.[6] In another study using the HADS scale, Badura-Brzoza et al.[39] declared that patients after limb amputation achieved a higher score in HADS-A and HADS-D compared with the control group and concluded that higher levels of anxiety and depression are noticed in patients suffering from PLP.
In contrast, Katz and Melzack found no significant difference in psychological dysfunction between patients who experienced phantom pain and those who did not.[20] In another study by Fisher and Hanspal,[22] the HADS score was compared between 29 PLP patients with 64 non-phantom pain amputees with the mean time of post-amputation of 9.7 years. The mean reported HADS scores in their study were 4.66 and 3.45 for anxiety and depression subscales, respectively. They concluded that only a few patients experienced emotional distress after amputation, and anxiety is being reported more often than depression.[22] In agreement with the studies of Katz and Melzack[20] and Fisher and Hanspal,[22] our results also confirmed the lower prevalence of depression and anxiety in patients with PLP compared with the control group. However, it should be noted that in the study of Katz and Melzack[20] and Fisher and Hanspal,[22] the control group consisted of amputees who did not experience any PLP, whereas in our study the patients with non-phantom chronic pain were considered as the control subjects. Moreover, compared to their results, the mean score of anxiety and depression was higher in our PLP patients (8.00 and 7.69, respectively) though it was considerably lower when compared with that of chronic pain sufferers (11.25 and 9.38, respectively).
A longitudinal study by Singh et al.[40] even showed that there is a dramatic drop in the incidence of psychological symptoms in individuals after amputation by the time of discharge from a rehabilitation ward. They have concluded that it may be due to adjustment after the emotional stress of limb loss as well as the learning of new skills to adjust to life after amputation.[40] This explanation could be also indicated in our patients, as they received different special cares at our pain clinic, too. However, in another more recent study by Singh et al.,[41] it was shown that after an initial drop in incidence of depression and anxiety symptoms after amputation, there is then an increase again after 2-3 years post amputation. In contrast, our evaluated PLP patients had a mean duration of 12 years post amputation and still showed a lower prevalence of anxiety and depression.
To the best of our knowledge, our study is the first one to compare the prevalence of anxiety and depression in PLP patients with a sample of non-phantom chronic pain sufferers. In addition to the lesser mean scores of these psychological dysfunctions by the HADS questionnaire, it was shown that the caseness of anxiety (25% vs. 58.3%) and depression (37.5% vs. 50%) were also lower in PLP patients compared with subjects with chronic pain. A review of the literature reveals that the considerable prevalence of depression in chronic pain sufferers has been previously found in some investigations such as that of Magni et al. in subjects with chronic musculoskeletal pain where the authors suggest a two-way relationship: depression may promote chronic pain and chronic pain may promote depression.[42]
Similar to most of the previous studies, one of the important limitations of our study was the cross-sectional design and lack of longitudinal assessment. In addition, the low statistical power in the comparison of depression score emphasizes the need for a higher sample size in further investigations.
CONCLUSION
The results of our study suggest that although the prevalence rates of anxiety and depression are considerable in patients with PLP, they were not as frequent as what is observed in non-phantom chronic pain sufferers. These lower levels of anxiety and depression in PLP compared to chronic pain is a new finding, which needs to be further evaluated and may lead to new insights into the pathogenesis of phantom pain in further studies.
ACKNOWLEDGMENT
We would like to express our thanks to Dr. Ali Kabir for his support in designing the study, management of the project, and useful comments on the primary and final draft of the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Jensen TS, Krebs B, Nielsen J, Rasmussen P. Immediate and long-term phantom limb pain in amputees: Incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain. 1985;21:267–78. doi: 10.1016/0304-3959(85)90090-9. [DOI] [PubMed] [Google Scholar]
- 2.Nikolajsen L, Staehelin JT. Phantom limb pain. Curr Rev Pain. 2000;4:166–70. doi: 10.1007/s11916-000-0052-0. [DOI] [PubMed] [Google Scholar]
- 3.Iacono RP, Linford J, Sandyk R. Pain management after lower extremity amputation. Neurosurgery. 1987;20:496–500. doi: 10.1227/00006123-198703000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: A review. Disabil Rehabil. 2004;26:837–50. doi: 10.1080/09638280410001708869. [DOI] [PubMed] [Google Scholar]
- 5.Kooijman CM, Dijkstra PU, Geertzen JH, Elzinga A, van der Schans CP. Phantom pain and phantom sensations in upper limb amputees: An epidemiological study. Pain. 2000;87:33–41. doi: 10.1016/S0304-3959(00)00264-5. [DOI] [PubMed] [Google Scholar]
- 6.Parkes CM. Factors determining the persistence of phantom pain in the amputee. J Psychosom Res. 1973;17:97–108. doi: 10.1016/0022-3999(73)90010-x. [DOI] [PubMed] [Google Scholar]
- 7.van der Schans CP, Geertzen JH, Schoppen T, Dijkstra PU. Phantom pain and health-related quality of life in lower limb amputees. J Pain Symptom Manage. 2002;24:429–36. doi: 10.1016/s0885-3924(02)00511-0. [DOI] [PubMed] [Google Scholar]
- 8.Jensen TS, Krebs B, Nielsen J, Rasmussen P. Phantom limb, phantom pain and stump pain in amputees during the first 6 months following limb amputation. Pain. 1983;17:243–56. doi: 10.1016/0304-3959(83)90097-0. [DOI] [PubMed] [Google Scholar]
- 9.Sherman RA, Sherman CJ. Prevalence and characteristics of chronic phantom limb pain among American veterans. Results of a trial survey. Am J Phys Med. 1983;62:227–38. [PubMed] [Google Scholar]
- 10.Frazier SH. Psychiatric aspects of causalgia, the phantom limb, and phantom pain. Dis Nerv Syst. 1966;27:441–50. [PubMed] [Google Scholar]
- 11.Lindesay J. Validity of the General Health Questionnaire (GHQ) in detecting psychiatric disturbance in amputees with phantom pain. J Psychosom Res. 1986;30:277–81. doi: 10.1016/0022-3999(86)90003-6. [DOI] [PubMed] [Google Scholar]
- 12.Sherman RA, Gall N, Gormly J. Treatment of phantom limb pain with muscular relaxation training to disrupt the pain – Anxiety – Tension cycle. Pain. 1979;6:47–55. doi: 10.1016/0304-3959(79)90139-8. [DOI] [PubMed] [Google Scholar]
- 13.Dougherty J. Relief of phantom limb pain after EMG biofeedback-assisted relaxation: A case report. Behav Res Ther. 1980;18:355–7. doi: 10.1016/0005-7967(80)90095-9. [DOI] [PubMed] [Google Scholar]
- 14.Siegel EF. Control of phantom limb pain by hypnosis. Am J Clin Hypn. 1979;21:285–6. doi: 10.1080/00029157.1979.10403984. [DOI] [PubMed] [Google Scholar]
- 15.Cedercreutz C. Hypnotic treatment of phantom sensations in 100 amputees. Acta Chir Scand. 1954;107:158–62. [PubMed] [Google Scholar]
- 16.Oakley DA, Whitman LG, Halligan PW. Hypnotic imagery as a treatment for phantom limb pain: Two case reports and a review. Clin Rehabil. 2002;16:368–77. doi: 10.1191/0269215502cr507oa. [DOI] [PubMed] [Google Scholar]
- 17.Belleggia G, Birbaumer N. Treatment of phantom limb pain with combined EMG and thermal biofeedback: A case report. Appl Psychophysiol Biofeedback. 2001;26:141–6. doi: 10.1023/a:1011391223713. [DOI] [PubMed] [Google Scholar]
- 18.Frischenschlager O, Pucher I. Psychological management of pain. Disabil Rehabil. 2002;24:416–22. doi: 10.1080/09638280110108841. [DOI] [PubMed] [Google Scholar]
- 19.Manchikanti L, Singh V. Managing phantom pain. Pain Physician. 2004;7:365–75. [PubMed] [Google Scholar]
- 20.Katz J, Melzack R. Pain ‘memories’ in phantom limbs: Review and clinical observations. Pain. 1990;43:319–36. doi: 10.1016/0304-3959(90)90029-D. [DOI] [PubMed] [Google Scholar]
- 21.Sherman R, Camfield M, Arena J. The effect of presence or absence of pain on low back pain patients’ answers to questions on the MMPI's HY, HS and D scales. J Milit Psychol. 1995;7:28–38. [Google Scholar]
- 22.Fisher K, Hanspal RS. Phantom pain, anxiety, depression, and their relation in consecutive patients with amputated limbs: Case reports. BMJ. 1998;316:903–4. doi: 10.1136/bmj.316.7135.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Snaith RP, Zigmond AS. The hospital anxiety and depression scale manual. NFER: Nelson, Windsor; 1994. [Google Scholar]
- 24.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 25.Cleeland CS, Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–38. [PubMed] [Google Scholar]
- 26.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 28.Flor H. Painful memories. Can we train chronic pain patients to ‘forget’ their pain? EMBO Rep. 2002;3:288–91. doi: 10.1093/embo-reports/kvf080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whalley MG, Farmer E, Brewin CR. Pain flashbacks following the July 7th 2005 London bombings. Pain. 2007;132:332–6. doi: 10.1016/j.pain.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 30.Ray AL, Zbik A. Cognitive behavioral therapies and beyond. In: Tollison CD, Satterhwaite JR, Tollsion JW, editors. Practical Pain Management. 3rd ed. Philadelphia: Lippincott; 2001. pp. 189–209. [Google Scholar]
- 31.Schneider J, Hofmann A, Rost C, Shapiro F. EMDR and phantom limb pain, theoretical implications, case study, and treatment guidelines. J EMDR Pract Res. 2007;1:45. [Google Scholar]
- 32.Hawamdeh ZM, Othman YS, Ibrahim AI. Assessment of anxiety and depression after lower limb amputation in Jordanian patients. Neuropsychiatr Dis Treat. 2008;4:627–33. doi: 10.2147/ndt.s2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desmond DM, MacLachlan M. Affective distress and amputation-related pain among older men with long-term, traumatic limb amputations. J Pain Symptom Manage. 2006;31:362–8. doi: 10.1016/j.jpainsymman.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 34.Cansever A, Uzun O, Yildiz C, Ates A, Atesalp AS. Depression in men with traumatic lower part amputation: A comparison to men with surgical lower part amputation. Mil Med. 2003;168:106–9. [PubMed] [Google Scholar]
- 35.Eaton WW. Epidemiologic evidence on the comorbidity of depression and diabetes. J Psychosom Res. 2002;53:903–6. doi: 10.1016/s0022-3999(02)00302-1. [DOI] [PubMed] [Google Scholar]
- 36.Atherton R, Robertson N. Psychological adjustment to lower limb amputation amongst prosthesis users. Disabil Rehabil. 2006;28:1201–9. doi: 10.1080/09638280600551674. [DOI] [PubMed] [Google Scholar]
- 37.Crawford JR, Henry JD, Crombie C, Taylor EP. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2001;40:429–34. doi: 10.1348/014466501163904. [DOI] [PubMed] [Google Scholar]
- 38.Weissman MM, Myers JK. Affective disorders in a US urban community: The use of research diagnostic criteria in an epidemiological survey. Arch Gen Psychiatry. 1978;35:1304–11. doi: 10.1001/archpsyc.1978.01770350030002. [DOI] [PubMed] [Google Scholar]
- 39.Badura-Brzoza K, Matysiakiewicz J, Piegza M, Rycerski W, Niedziela U, Hese RT. Sociodemographic factors and their influence on anxiety and depression in patients after limb amputation. Psychiatr Pol. 2006;40:335–45. [PubMed] [Google Scholar]
- 40.Singh R, Hunter J, Philip A. The rapid resolution of depression and anxiety symptoms after lower limb amputation. Clin Rehabil. 2007;21:754–9. doi: 10.1177/0269215507077361. [DOI] [PubMed] [Google Scholar]
- 41.Singh R, Ripley D, Pentland B, Todd I, Hunter J, Hutton L, et al. Depression and anxiety symptoms after lower limb amputation: The rise and fall. Clin Rehabil. 2009;23:281–6. doi: 10.1177/0269215508094710. [DOI] [PubMed] [Google Scholar]
- 42.Magni G, Moreschi C, Rigatti-Luchini S, Merskey H. Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain. 1994;56:289–97. doi: 10.1016/0304-3959(94)90167-8. [DOI] [PubMed] [Google Scholar]


