Abstract
Autosomal dominant polycystic kidney disease (ADPKD) is an inherited disorder associated with multiple cyst formation in the different organs. Development of pancreatic cyst in ADPKD is often asymptomatic and is associated with no complication. A 38-year-old man with ADPKD was presented with six episodes of acute pancreatitis and two episodes of cholangitis in a period of 12 months. Various imaging studies revealed multiple renal, hepatic and pancreatic cysts, mild ectasia of pancreatic duct, dilation of biliary system and absence of biliary stone. He was managed with conservative treatment for each attack. ADPKD should be considered as a potential risk factor for recurrent acute and/or chronic pancreatitis and cholangitis.
Keywords: Acute pancreatitis, Autosomal dominant polycystic kidney disease, cholangitis
INTRODUCTION
Autosomal dominant polycystic kidney disease (ADPKD) is an inherited disorder mainly associated with renal cyst formation and renal function deterioration.[1] ADPKD may also provoke cyst formation in other organs such as liver, spleen and pancreas.[2] Development of these cysts not only may cause tissue dysfunction in the affected organs, but also their pressure effects may cause dysfunctions on the neighboring structures. Herein, the authors present a rare case of ADPKD with renal, hepatic and pancreatic cysts associated with recurrent acute pancreatitis and cholangitis.
CASE REPORT
A 38-year-old man was transferred to the emergency department (Alzahra hospital, Isfahan University of Medical Sciences) with an acute abdominal pain, nausea and vomiting in early September 2010. His abdominal pain was mainly localized in the epigastric region and had a tendency to worsen in the supine position.
He was a known case of ADPKD with multiple renal cysts since 12 years ago. The patient had been hospitalized five times in our center in the past 11 months with the same symptoms and with the diagnosis of acute pancreatitis that each time he had been managed with conservative treatments. Multiple hepatic cysts had been detected in the past year during pancreatitis workup. He had also a history of stent placement and retrieval for two times because of stricture formation in common bile duct and consequent cholangitis.
Physical examination revealed generalized jaundice, tachycardia and tenderness in upper abdomen. Laboratory study was demonstrated in Table 1. There was no evidence of gallstone in abdominal ultrasonography. Abdominal computed tomography (CT) scan, magnetic resonance cholangiopancreatography (MRCP) and abdominal magnetic resonance imaging (MRI) revealed multiple renal, hepatic and pancreatic cysts, mild ectasia of pancreatic duct, dilation of biliary system and absence of biliary stone [Figures 1–4].
Table 1.
Laboratory findings at admission
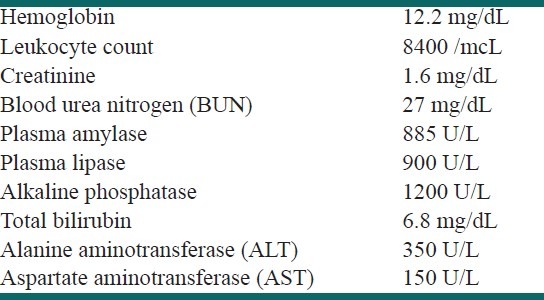
Figure 1.
Double contrast abdominal computed tomography scan showed mild ectasia of pancreatic duct
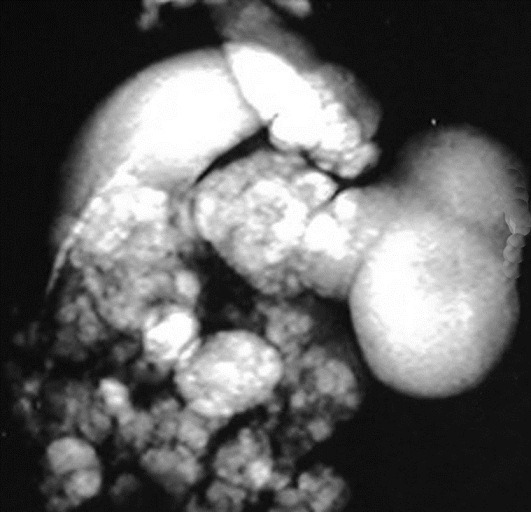
Figure 4.
Coronal MRI images revealed large kidneys, multiple hepatic, renal and pancreatic cysts and dilatation of biliary system
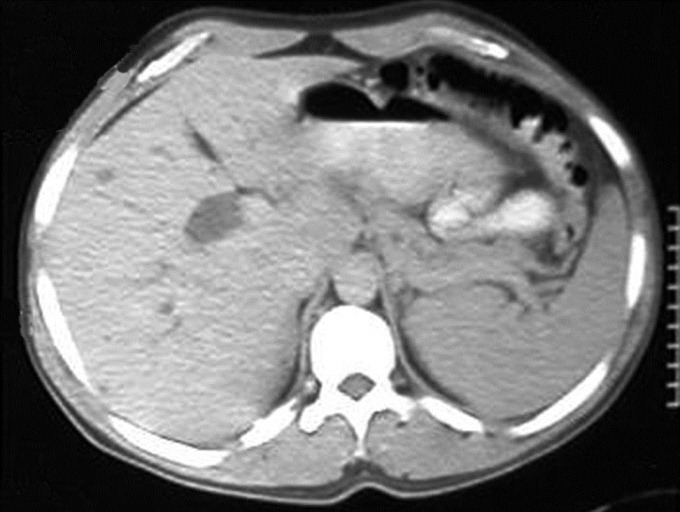
Figure 2.
Magnetic resonance cholangiopancreatography demonstrated dilatation of intrahepatic biliary ducts
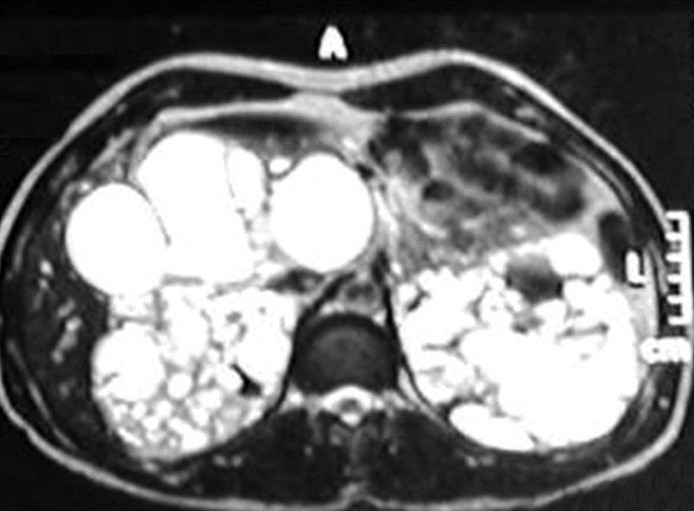
Figure 3.
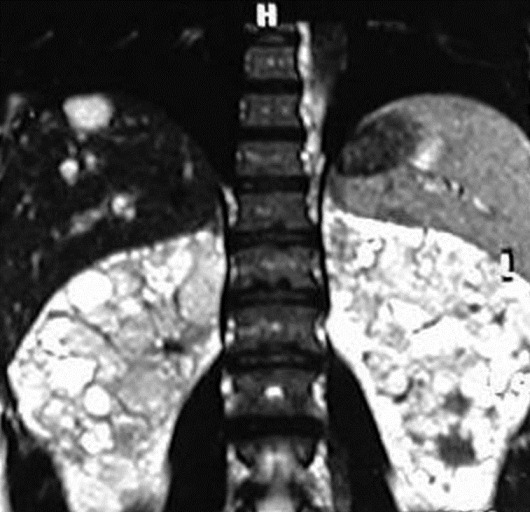
Axial MRI images revealed large kidneys, multiple hepatic, renal and pancreatic cysts and dilatation of biliary system
With the diagnosis of acute pancreatitis, the patient was treated with conservative treatments included hydration and antibiotics. We also evaluated the patient for intracranial, cardiac and gastrointestinal association of ADPKD which revealed no considerable finding. He was discharged after a week with remarkable decrease in clinical and laboratory impairments and without need for surgery. After three months as the patient had recurrent cholangitis he underwent a liver transplantation. Two months later, he was hospitalized again with another attack of acute pancreatitis.
DISCUSSION
ADPKD is a genetically inherited disease, which may lead to chronic renal failure through developing multiple renal cysts.[1] As it has a gradual course and a late onset of symptomatic phase, the diagnosis is usually delayed until middle ages.[3] Cyst formation is the main fact in ADPKD which is not limited to kidneys and may also afflict other organs including liver, spleen and pancreas.[2]
Pancreatic cysts are often diagnosed in middle-aged patients.[3] These cysts are tiny and therefore are often asymptomatic and associated with no complication in patients with ADPKD.[4] Malka et al., presented the first case of complicated pancreatic cyst in a patient with ADPKD, which caused chronic pancreatitis and chronic abdominal pain.[4]
Abdominal or flank pain is one of most common presentations of ADPKD and may occur whenever in the course of disease. This pain may be due to compression effects of cysts on the afflicted organ; however, it is important to differentiate it from the other causes such as nephrolithiasis, cholelithiasis, hemorrhage inside the cysts and the obstructive complications.[5,6]
Basar et al. reported a case of recurrent pancreatitis in a patient with ADPKD, pancreatitis cysts and pancreas divisum.[2] In our patient more than a decade after diagnosis of ADPKD obstructive effects of multiple hepatic and pancreatic cysts caused recurrent cholangitis and pancreatitis, respectively. The diagnosis of acute pancreatitis in this patient was established upon typical pain and high serum levels of amylase and lipase. Renal function tests were not remarkably out of normal ranges, therefore, high serum levels of amylase and lipase were only consequent to acute pancreatitis. Moreover, high enzyme levels lowered within days after conservative treatment.
Various imaging modalities are available for diagnosis of cysts and their complications in ADPKD. In our patient, recurrent episodes of pancreatitis and cholangitis caused dilation of pancreatic duct and biliary system which was obvious in CT, MRCP and MRI.
Conservative therapy in the majority of patients with pancreatitis is the first line and the proper treatment; but in ADPKD patients, renal or hepatic failure can complicate the pancreatitis and therefore surgical intervention may be required.[6–9]
Our patient underwent a liver transplant due to recurrent cholangitis and hepatic failure. Surgical resection of cysts was not possible as the cysts were scattered all over the liver; however patient returned with another episode of acute pancreatitis after liver transplant as a result of pancreatic duct obstruction caused by pancreatic cysts.
In conclusion, development of hepatic and pancreatic cysts in ADPKD can lead to the obstruction of biliary system and pancreatic duct and therefore ADPKD should be considered as a potential risk factor for recurrent acute and/or chronic pancreatitis and cholangitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Patel V, Chowdhury R, Igarashi P. Advances in the pathogenesis and treatment of polycystic kidney disease. Curr Opin Nephrol Hypertens. 2009;18:99–106. doi: 10.1097/MNH.0b013e3283262ab0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Başar O, Ibiş M, Uçar E Ertuğrul I, Yolcu OF, Köklü S, et al. Recurrent pancreatitis in a patient with autosomal-dominant polycystic kidney disease. Pancreatology. 2006;6:160–2. doi: 10.1159/000090258. [DOI] [PubMed] [Google Scholar]
- 3.Davies F, Coles GA, Harper PS, Williams AJ, Evans C, Cochlin D. Polycystic kidney disease re-evaluated: A population-based study. Q J Med. 1991;79:477–85. [PubMed] [Google Scholar]
- 4.Malka D, Hammel P, Vilgrain V, Fléjou JF, Belghiti J, Bernades P. Chronic obstructive pancreatitis due to a pancreatic cyst in a patient with autosomal dominant polycystic kidney disease. Gut. 1998;42:131–4. doi: 10.1136/gut.42.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bajwa ZH, Sial KA, Malik AB, Steinman TI. Pain patterns in patients with polycystic kidney disease. Kidney Int. 2004;66:1561–9. doi: 10.1111/j.1523-1755.2004.00921.x. [DOI] [PubMed] [Google Scholar]
- 6.Chauveau D, Fakhouri F, Grünfeld JP. Liver involvement in autosomal-dominant polycystic kidney disease: therapeutic dilemma. J Am Soc Nephrol. 2000;11:1767–75. doi: 10.1681/ASN.V1191767. [DOI] [PubMed] [Google Scholar]
- 7.Newman KD, Torres VE, Rakela J, Nagorney DM. Treatment of highly symptomatic polycystic liver disease. Preliminary experience with a combined hepatic resection-fenestration procedure. Ann Surg. 1990;212:30–7. doi: 10.1097/00000658-199007000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirchner GI, Rifai K, Cantz T, Nashan B, Terkamp C, Becker T, et al. Outcome and quality of life in patients with polycystic liver disease after liver or combined liver-kidney transplantation. Liver Transpl. 2006;12:1268–77. doi: 10.1002/lt.20780. [DOI] [PubMed] [Google Scholar]
- 9.Sarrami AH, Baradaran-Mahdavi MM, Meidani M. Precise recognition of liver inflammatory pseudotumor may prevent an unnecessary surgery. Int J Prev Med. 2012;3:432–4. [PMC free article] [PubMed] [Google Scholar]


