Abstract
INTRODUCTION
Single port/incision laparoscopic surgery (SPILS) is a modern advancement toward stealth surgery. Despite the paucity of high-quality scientific studies assessing its effectiveness, this procedure is being used increasingly. This review aims to describe commonly used techniques for SPILS appendicectomies (SPILA), to summarise complication rates in the literature and to provide discussion on indications and implementation.
METHODS
All available databases including the Cochrane Central Register of Controlled Trials, MEDLINE® and Embase™ were searched in February 2011 and cross-referenced for available English literature describing SPILA in patients of any age.
RESULTS
Three broad technical approaches are described: procedures using laparoscopic instruments through a single skin incision in the abdominal wall, regardless of the number of fascial incisions, with or without the additional use of percutaneous sutures or wires to ‘assist’ the operation, and hybrid procedures, in which the appendix is exteriorised using a single incision laparoscopically assisted operation but subsequently divided using a conventional ‘open’ appendicectomy technique. Complication rates seem to be highest in SPILA procedures unassisted by sutures or wires.
CONCLUSIONS
Future research assessing the efficacy of single incision laparoscopic procedures should consider variation in technique as a possible factor affecting outcome.
Keywords: Single, Incision, Laparoscopic, Appendicectomy, Techniques
Single port/incision laparoscopic surgery (SPILS) is a modern advancement toward stealth surgery. The effectiveness of these procedures remains to be proved by well-conducted scientific trials. Increasing interest in novel concepts in surgery is leading to a rise in the number and variation of procedures being performed, and literature reporting them. As appendicectomy is a commonly performed therapeutic procedure, it lends itself neatly as an operation with which to compare current technical approaches to SPILS.
The aims of this review were to provide a brief description of the surgical techniques currently used in performing single port/incision laparoscopic appendicectomy (SPILA), briefly review complications reported in the literature on SPILA and provide general discussion on SPILA and SPILS.
Methods
All available databases including the Cochrane Central Register of Controlled Trials, MEDLINE® and Embase™ were searched in February 2011 and cross-referenced for available English literature describing SPILA in patients of any age. The search was conducted using the keywords: single and one incision/port/trocar/site, invisible, scarless, scar free or transumbilical. There was no restriction on publication date. Papers included reports of patients admitted for emergency or interval appendicectomies for acute or chronic appendicitis, complicated or simple. Articles were excluded if they provided an inadequate description of surgical methodology, insufficient data on outcomes or if they were ‘experimental’ reports with fewer than five patients.
Results
The database query yielded 79 references. One randomised controlled trial and thirty-eight case series met the inclusion criteria.1–39 All studies reviewed had similar patient inclusion criteria, including both acute cases and interval appendicectomy. There were minor variations in exclusions, including previous surgery, body mass index and ASA (American Society of Anesthesiologists) grade. Most series excluded complicated cases of appendicitis. In those series in which a few complicated cases were operated on, outcomes were not reported separately. Studies had varying sample sizes ranging from 7 to 262. The total number of SPILA performed across the studies was 2,656.
Surgical techniques
All studies reported a single skin incision through the umbilicus except four,1–4 in which surgeons performed an infraumbilical incision. The literature broadly describes three approaches to SPILA referred to throughout this review as:
〉 SPILA unassisted: any procedure using specialised or conventional laparoscopic instruments through a single skin incision in the abdominal wall, regardless of the number of fascial incisions
〉 SPILA assisted: as SPILA with the additional use of percutaneous sutures or wires to ‘assist’ the operation
〉 Hybrid: any procedure in which the appendix was exteriorised using a single incision, laparoscopically assisted operation but divided subsequently using a conventional ‘open’ appendicectomy technique
SPILA unassisted
Twenty studies4–23 including 584 patients met the definition criteria for ‘SPILA unassisted’ approaches. The use of special multi-conduit ports was reported in four studies4–7 (Fig 1). Vidal et al made a 25mm transverse, infraumbilical, suprapubic incision in order to place a SILS flexible laparoscopic port (SILS™ port, Covidien, Norwalk, CT, US) in 20 patients.4 A 5mm 30º laparoscopic camera was used with 5mm graspers and flexible scissors to dissect the mesoappendix. The appendix was divided using a multifire stapler (Endo GIA™ 30, Covidien). Kössi and Luostarinen performed a transumbilical version of the same procedure using the SILS™ port but used straight and curved graspers, and ligated the appendix with an absorbable suture material (Endoloop®, Ethicon Inc, Somerville, NJ, US) before sharply dividing the appendix with laparoscopic scissors.5 SILS devices were removed preceding extraction of the appendix.
Figure 1.
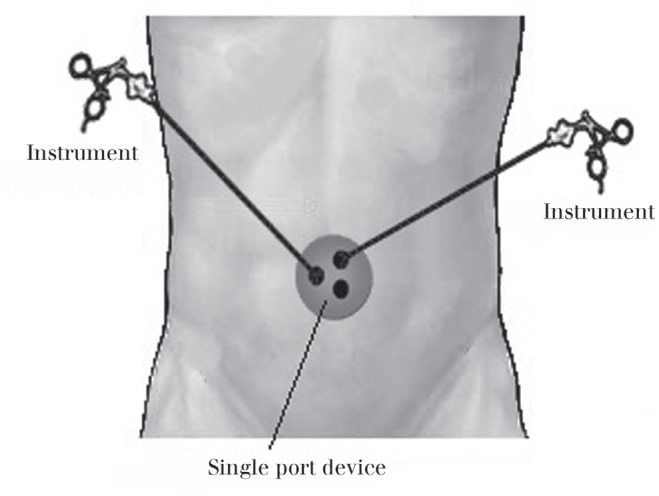
Multi-luminal, single port device placed transumbilically
Fourteen ‘SPILA unassisted’ studies described the use of conventional laparoscopic equipment without commercially available, specialised ‘single ports’. Techniques placing multiple ports through closely spaced fascial incisions with a single abdominal skin incision were reported in ten studies.8–17 Generally, papers described the introduction of three trocars through the fascia, two providing channels for instruments and one providing access for a 5—10mm laparoscopic camera with an angulated lens. In studies where three ports were not placed, a third instrument, often a grasper, was placed directly though a fascial stab incision.8,9 A single study used only two 5mm ports, though which a 4mm 30º camera, bipolar cautery and absorbable suture material could be placed.10 The authors enlarged one of their port sites to retrieve the appendix.
Dapri et al described a transumbilical SPILA technique using curved instruments whereby a single 11mm trocar alongside a 5mm instrument (introduced through stab incision) were contained within a purse string suture in the umbilical fascia to provide a ‘tight seal’.11 A separate 5mm opening for additional instruments was made outside the purse string within the umbilical fascia. Rothenburg et al placed a 3mm single instrument through a separate stab wound incision or 3mm port suprapubically to aid the SPILA procedure.12 Palanivelu et al achieved successful SPILA procedures in children with only a 15mm trocar and double channel endoscope.18
The ‘surgical glove’ method (in which trocars are placed through the holes of a surgical glove with cut fingertips and the ‘device’ is subsequently applied to a retractor inserted into the abdomen through a single transumbilical incision) was described by Park et al,19 Kim et al20 and Lee et al21 in 20, 43 and 75 patients respectively (Fig 2). The surgical glove can be considered an improvised multi-luminal single port device. CO2 insufflation was achieved through the glove in at least two of the studies.
Figure 2.
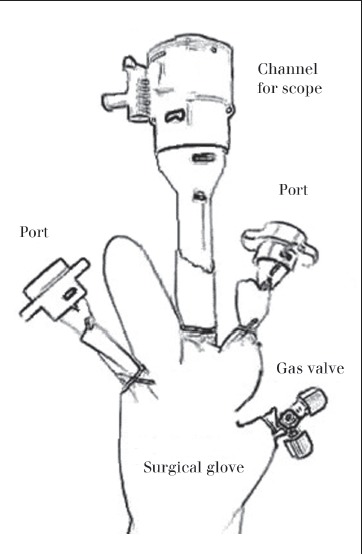
Improvised single port device using surgical glove
SPILA assisted
Five studies1,24—27 reported SPILA procedures that were ‘assisted’ with a transabdominal sling suture, or wire, to suspend the appendix (Fig 3). All studies described the introduction of instruments through a single umbilical incision with a single port or multiple closely spaced ports. Suspension of the appendix was achieved with various methods. Jiang et al suspended the root of the appendix intracorporeally with fine copper wire once identified.24 Roberts achieved suspension of the appendix by creating an innovative, intracorporeal ‘pulley’.1 An ‘air’ loop was tied in the internal anterior wall of the abdomen that functioned as an axle through which a separate ‘string’ with a looped end was threaded and passed around the appendix; the opposite end rested outside the umbilical port.
Figure 3.
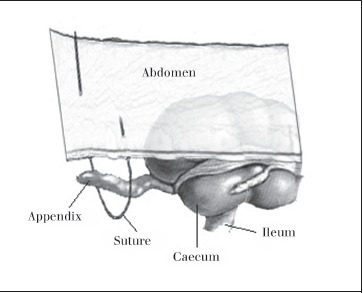
Suspensory suture passed through abdominal wall and around appendix to create sling
Three studies25–27 used suture material introduced percutaneously. Akgür et al placed a 16G angiographic catheter transabdominally in the lower right quadrant through which a folded polypropylene suture could be introduced to function as a ‘grasper’.25 Ateş et al26 and Lee et al27 inserted a suture in the right lower quadrant percutaneously and subsequently through the mesoappendix under visualisation of a laparoscope. The tip of the needle was then exteriorised, allowing the appendix to be pulled toward the abdominal wall. Following dissection of the mesoappendix, the authors of all three studies ligated the appendix with a fishermen’s knot tied extracorporeally, allowing the appendix to be divided intracorporeally over the ligature, with laparoscopic scissors.
Hybrid
Fourteen articles2,3,28—39 reported a hybrid approach to appendicectomy in which a single abdominal incision facilitated the use of laparoscopic equipment to exteriorise the appendix, subsequently allowing a conventional ‘open’ appendicectomy to be performed. All authors described the use of a single transumbilical port through which a laparoscope with a working channel was used to identify and exteriorise the appendix. Open appendicectomy was performed, the appendix coagulated, iodised and repositioned. Most authors explicitly mentioned reinflating the abdomen after returning the appendix to assess haemostasis.
Complication rates
No mortality was recorded for any of the procedures. The highest number of intraoperative complications, including serosal injury, intra-abdominal haemorrhage and perforation, was reported by Muensterer et al (4/75, 5%)9 and the highest rate by Palanivelu et al (2/8, 25%).18 Both groups of authors describe the SPILS unassisted approach to SPILA.
Generally, there were very few wound infections reported in the literature. The highest rates were reported by Min et al (2/10, 20%)13 and Visnjic et al (4/29, 14%),28 using ‘SPILA unassisted’ and ‘hybrid’ methods respectively. The highest number of postoperative complications overall was reported by Valla et al (10/200, 5%),3 who used a ‘hybrid’ approach to SPILA. The highest rates, however, were reported in papers using the ‘SPILA unassisted’ technique (2/10, 20%).13 There were six intra-abdominal abscesses across all of the studies: five were reported in four ‘SPILA unassisted’ papers9,11,19,21 and one in a ‘hybrid’ paper.29
In total, complication rates appear to be highest for those procedures in which SPILA is not assisted by sutures or wire. Table 1 summarises complications reported in the literature according to technique.
Table 1.
Complications reported in the literature, stratified according to technique
| SPILS unassisted (20 studies) |
SPILS assisted (5 studies) |
Hybrid (14 studies) |
|
| Intra-operative | 9/584 (1.54%) | 1/409 (0.24%) | 1/1,511 (0.07%) |
| Serosal injury | 1 | 0 | 1 |
| Haemorrhage | 7 | 0 | 0 |
| Perforation | 1 | 0 | 0 |
| Other | 0 | 0 | 0 |
| Undefined | 0 | 1 | 0 |
| Post-operative | 39/584 (6.68%) | 10/409 (2.44%) | 47/1,511 (3.11%) |
| Wound infection | 17 | 1 | 15 |
| Wound haematoma | 2 | 0 | 4 |
| Intra-abdominal abscess | 5 | 0 | 1 |
| Intra-abdominal fluid | 3 | 0 | 6 |
| Intra-abdominal haemorrhage | 2 | 0 | 0 |
| Ileus | 3 | 1 | 0 |
| Other | 4 | 8 | 11 |
| Undefined | 3 | 0 | 10 |
| Total complications | 48/584 (8.22%) | 11/409 (2.69%) | 48/1,511 (3.18%) |
| Conversion | 20/584 (3.42%) | 7/409 (1.71%) | 61/1,511 (4.04%) |
| To conventional | 16 | 0 | 16 |
| To open operation | 4 | 7 | 45 |
| Additional trocar use | 25 | 13 | 54 |
| Mortality | 0 (0%) | 0 (0%) | 0 (0%) |
Discussion
In its early days, laparoscopic appendicectomy failed to gain unequivocal acceptance by the surgical community. Today, it is a commonly practised and accepted emergency procedure.40
Although claims of enhanced recovery and pain as well as blood loss and complication reduction as compared with conventional laparoscopic and open procedures have yet to be substantiated objectively, single port/incision laparoscopic procedures are increasingly being performed.4,12,23 Although level 1 and 2 evidence is still awaited, there are a lot of available data suggesting that it could be a safe and reproducible method of surgery. Currently, there are clinical trials being conducted that will provide important level 1 evidence for this new approach. (See http://clinicaltrials.gov/.)
The surgical technologies industry has developed a vast range of multi-conduit, single port devices and specialised laparoscopic instruments with flexible handles and tips. This equipment may be useful in more complex procedures by restoring some of the triangulation lost with a single port approach when compared with conventional laparoscopic surgery. However, ‘hybrid’ methods such as removal of the appendix extracorporeally in appendicectomy may be an alternative to expensive intracorporeal devices.
Generally, studies identified for this review described a single umbilical skin incision with single or multiple fascial incisions to achieve access to the peritoneal cavity. Reduced scarring is the most evident advantage of SPILS. Optimal cosmetic results are obtained through intraumbilical incision as the scar will be concealed within the umbilicus but a major concern may be injury to the epigastric vessels.41 Advantages to infraumbilical or suprapubic incisions include safety and reduced risk of incisional hernia.42 SPILS may increase hernia risk as they necessitate midline fascial incisions. Furthermore, some authors consider large single fascial incisions to be more traumatic than a few 5mm or 12mm wounds by dilating trocars.5
As it is based loosely on current practice, surgeons may embrace SPILS more willingly than other novel surgical procedures (eg natural orifice transluminal endoscopic surgery [NOTES]). Intraoperative procedure-related challenges include instrument crowding (‘sword fighting’) and cross-over, limited ‘inline’ single axis view and inadequate retraction (overcome by the ‘hybrid’ approach).43
Problems inherent to SPILA include concerns over accidental tears when manipulating friable appendices, resulting in abdominal contamination, and port site contamination, given that the inflamed appendix makes direct contact with the wound (especially with ‘hybrid’ methods).30 Navigating instruments in obese patients, in whom the umbilicus ceases to function as a useful landmark for distance to target organ, can further increase the difficulty of the procedure.43
Complication rates obtained from SPILA case series appear similar to conventional laparoscopic and open appendicectomy procedures.40 At the beginning of the learning curve, patient selection is essential to avoid conversions and lengthy operating times. It is therefore reasonable to assume that patients in the current literature are of favourable selection operated on by experienced and motivated surgeons, meaning any trends noted are not entirely valid. ‘SPILA unassisted’ procedures are possibly the most technically challenging of the three approaches described. This may account for the higher intraoperative and postoperative complication rates. A similar case may be made for other SPILS procedures.
There is a known bias of publication with novel techniques in surgery whereby positive findings are often published ahead of negative.44 The majority of published literature on SPILA is only two years old and therefore negative results are not so likely to have been published yet.
Conclusions
As an umbrella term for a wider range of operations including liver resection, colectomy, splenectomy and cholecystectomy, SPILS may be a bridge between standard laparoscopic techniques and complete stealth surgery (ie NOTES, which still faces technical and technological limitations). SPILS does not incur the safety problems associated with opening and closing viscera (oesophagus, vagina, colon) and can be converted quickly and easily to multiport laparoscopic or open surgery.
Although feasible, it is technically challenging. Once the learning curve is over, adequately powered randomised controlled trials will be needed to investigate whether the benefits to the patient overcome the technical and technological cost. At present, meta-analysis is not possible. Due to the nature of the currently available evidence, it is difficult to comment specifically on which technical approaches to SPILA are most effective and difficult to generalise for other SPILS procedures. In assessing the efficacy of SPILS, future research should give consideration to the variation in procedural technique as this may alter outcomes.
References
- 1.Roberts KE. True single-port appendectomy: first experience with the ‘puppeteer technique’. Surg Endosc. 2009;23:1,825–1,830. doi: 10.1007/s00464-008-0270-9. [DOI] [PubMed] [Google Scholar]
- 2.Hong ZJ, Fan HL, Kuo SM, et al. Preliminary report of one-port laparoscopy-assisted extracorporeal appendectomy in adult appendicitis. J Med Sci. 2009;29:135–138. [Google Scholar]
- 3.Valla J, Ordorica-Flores RM, Steyaert H, et al. Umbilical one-puncture laparoscopic-assisted appendectomy in children. Surg Endosc. 1999;13:83–85. doi: 10.1007/s004649900906. [DOI] [PubMed] [Google Scholar]
- 4.Vidal O, Ginestà C, Valentini M, et al. Suprapubic single-incision laparoscopic appendectomy: a nonvisible-scar surgical option. Surg Endosc. 2011;25:1,019–1,023. doi: 10.1007/s00464-010-1307-4. [DOI] [PubMed] [Google Scholar]
- 5.Kössi J, Luostarinen M. Initial experience of the feasibility of single-incision laparoscopic appendectomy in different clinical conditions. Diagn Ther Endosc. 2010 doi: 10.1155/2010/240260. 240260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chandler NM, Danielson PD. Single-incision laparoscopic appendectomy vs multiport laparoscopic appendectomy in children: a retrospective comparison. J Pediatr Surg. 2010;45:2,186–2,190. doi: 10.1016/j.jpedsurg.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Ying-zhang MA, Jiang-fan ZH, Man-zhu XU, et al. Transumbilical laparoscopic appendectomy by using a tri-channel trocar technique. J Laparosc Surg. 2008;13:319–320. [Google Scholar]
- 8.Saber AA, Elgamal MH, El-Ghazaly TH, et al. Simple technique for single incision transumbilical laparoscopic appendectomy. Int J Surg. 2010;8:128–130. doi: 10.1016/j.ijsu.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Muensterer OJ, Puga Nougues C, Adibe OO, et al. Appendectomy using single-incision pediatric endosurgery for acute and perforated appendicitis. Surg Endosc. 2010;24:3,201–3,204. doi: 10.1007/s00464-010-1115-x. [DOI] [PubMed] [Google Scholar]
- 10.Chouillard E, Dache A, Torcivia A, et al. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010;24:1,861–1,865. doi: 10.1007/s00464-009-0860-1. [DOI] [PubMed] [Google Scholar]
- 11.Dapri G, Casali L, Dumont H, et al. Single-access transumbilical laparoscopic appendectomy and cholecystectomy using new curved reusable instruments: a pilot feasibility study. Surg Endosc. 2011;25:1,325–1,332. doi: 10.1007/s00464-010-1304-7. [DOI] [PubMed] [Google Scholar]
- 12.Rothenberg SS, Shipman K, Yoder S. Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech. 2009;19:695–698. doi: 10.1089/lap.2009.0148. [DOI] [PubMed] [Google Scholar]
- 13.Min IC, Kim DJ, Jang LC, et al. Single incision three ports laparoscopic appendectomy. J Korean Soc Endosc Laparosc Surg. 2009;12:84–87. [Google Scholar]
- 14.Tam YH, Lee KH, Sihoe JD, et al. A surgeon-friendly technique to perform single-incision laparoscopic appendectomy intracorporeally in children with conventional laparoscopic instruments. J Laparoendosc Adv Surg Tech. 2010;20:577–580. doi: 10.1089/lap.2010.0034. [DOI] [PubMed] [Google Scholar]
- 15.Chow A, Purkayastha S, Nehme J, et al. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2,567–2,574. doi: 10.1007/s00464-010-1004-3. [DOI] [PubMed] [Google Scholar]
- 16.Chow A, Purkayastha S, Paraskeva P. Appendicectomy and cholecystectomy using single-incision laparoscopic surgery (SILS): the first UK experience. Surg Innov. 2009;16:211–217. doi: 10.1177/1553350609344413. [DOI] [PubMed] [Google Scholar]
- 17.Dutta S. Early experience with single incision laparoscopic surgery: eliminating the scar from abdominal operations. J Pediatr Surg. 2009;44:1,741–1,745. doi: 10.1016/j.jpedsurg.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Palanivelu C, Rajan P, Rangarajan M, et al. Transumbilical endoscopic appendectomy in humans: on the road to NOTES: a prospective study. J Laparoendosc Adv Surg Tech. 2008;18:579–582. doi: 10.1089/lap.2007.0174. [DOI] [PubMed] [Google Scholar]
- 19.Park JH, Hyun KH, Park CH, et al. Laparoscopic vs transumbilical single-port laparoscopic appendectomy; results of prospective randomized trial. J Korean Surg Soc. 2010;78:213–218. [Google Scholar]
- 20.Kim HJ, Lee JI, Lee YS, et al. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010;24:2,765–2,769. doi: 10.1007/s00464-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 21.Lee JA, Sung KY, Lee JH, Lee do S. Laparoscopic appendectomy with a single incision in a single institute. J Korean Soc Coloproctol. 2010;26:260–264. doi: 10.3393/jksc.2010.26.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim JW, Park JS, Chang IT, et al. The initial experience with a single incision laparoscopic appendectomy. J Korean Soc Coloproctol. 2009;25:312–317. [Google Scholar]
- 23.Ponsky TA, Diluciano J, Chwals W, et al. Early experience with single-port laparoscopic surgery in children. J Laparoendosc Adv Surg Tech. 2009;19:551–553. doi: 10.1089/lap.2009.0092. [DOI] [PubMed] [Google Scholar]
- 24.Jiang CH, Yao N, Fang XM, et al. Clinical application with laparoscopic appendectomy in single-port and suspension method. J Laparosc Surg. 2008 [Google Scholar]
- 25.Akgür FM, Olguner M, Hakgüder G, Ateş O. Appendectomy conducted with single port incisionless-intracorporeal conventional equipment-endoscopic surgery. J Pediatr Surg. 2010;45:1,061–1,063. doi: 10.1016/j.jpedsurg.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 26.Ateş O, Hakgüder G, Olguner M, Akgür FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007;42:1,071–1,074. doi: 10.1016/j.jpedsurg.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 27.Lee SY, Lee HM, Hsieh CS, Chuang JH. Transumbilical laparoscopic appendectomy for acute appendicitis: a reliable one-port procedure. Surg Endosc. 2011;25:1,115–1,120. doi: 10.1007/s00464-010-1326-1. [DOI] [PubMed] [Google Scholar]
- 28.Visnjic S. Transumbilical laparoscopically assisted appendectomy in children: high-tech low-budget surgery. Surg Endosc. 2008;22:1,667–1,671. doi: 10.1007/s00464-007-9680-3. [DOI] [PubMed] [Google Scholar]
- 29.Koontz CS, Smith LA, Burkholder HC, et al. Video-assisted transumbilical appendectomy in children. J Pediatr Surg. 2006;41:710–712. doi: 10.1016/j.jpedsurg.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 30.Petnehazy T, Saxena A, Ainoedhofer H, et al. Single-port appendectomy in obese children: an optimal alternative? Acta Paediatr. 2010;99:1,370–1,373. doi: 10.1111/j.1651-2227.2010.01791.x. [DOI] [PubMed] [Google Scholar]
- 31.Sesia SB, Haecker FM, Kubiak R, Mayr J. Laparoscopy-assisted single-port appendectomy in children: is the postoperative infectious complication rate different? J Laparoendosc Adv Surg Tech. 2010;20:867–871. doi: 10.1089/lap.2010.0180. [DOI] [PubMed] [Google Scholar]
- 32.D’Alessio A, Piro E, Tadini B, Beretta F. One-trocar transumbilical laparoscopic-assisted appendectomy in children: our experience. Eur J Pediatr Surg. 2002;12:24–27. doi: 10.1055/s-2002-25096. [DOI] [PubMed] [Google Scholar]
- 33.Rispoli G, Armellino MF, Esposito C. One-trocar appendectomy. Surg Endosc. 2002;16:833–835. doi: 10.1007/s00464-001-9107-5. [DOI] [PubMed] [Google Scholar]
- 34.Esposito C. One-trocar appendectomy in pediatric surgery. Surg Endosc. 1998;12:177–178. doi: 10.1007/s004649900624. [DOI] [PubMed] [Google Scholar]
- 35.Satomi A, Tanimizu T, Takahashi S, et al. One-port laparoscopy-assisted appendectomy in children with appendicitis: experience with 100 cases. Pediatr Endosurg Innov Tech. 2001;5:371–377. [Google Scholar]
- 36.Martínez AP, Bermejo MA, Cortś JC, et al. Appendectomy with a single trocar through the umbilicus: results of our series and a cost approximation. Cir Pediatr. 2007;20:10–14. [PubMed] [Google Scholar]
- 37.Meyer A, Preuss M, Roesler S, et al. Transumbilical laparoscopic-assisted ‘one-trocar’ appendectomy — TULAA — as an alternative operation method in the treatment of appendicitis. Zentralbl Chir. 2004;129:391–395. doi: 10.1055/s-2004-820388. [DOI] [PubMed] [Google Scholar]
- 38.Guanà R, Gesmundo R, Maiullari E, et al. Treatment of acute appendicitis with one-port transumbilical laparoscopic-assisted appendectomy: a six-year, single-centre experience. Afr J Paediatr Surg. 2010;7:169–173. doi: 10.4103/0189-6725.70419. [DOI] [PubMed] [Google Scholar]
- 39.Pappalepore N, Tursini S, Marino N, et al. Transumbilical laparoscopic-assisted appendectomy (TULAA): a safe and useful alternative for uncomplicated appendicitis. Eur J Pediatr Surg. 2002;12:383–386. doi: 10.1055/s-2002-36846. [DOI] [PubMed] [Google Scholar]
- 40.Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010;10 doi: 10.1002/14651858.CD001546.pub3. CD001546. [DOI] [PubMed] [Google Scholar]
- 41.Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg. 2004;239:182–185. doi: 10.1097/01.sla.0000109151.53296.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barry M, Winter DC. Laparoscopic port site hernias: any port in a storm or a storm in any port? Ann Surg. 2008;248:687–689. doi: 10.1097/SLA.0b013e3181883cea. [DOI] [PubMed] [Google Scholar]
- 43.Canes D, Desai MM, Aron M, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008;54:1,020–1,029. doi: 10.1016/j.eururo.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 44.Ioannidis JP. Effect of the statistical significance of results on the time to completion and publication of randomized efficacy trials. JAMA. 1998;279:281–286. doi: 10.1001/jama.279.4.281. [DOI] [PubMed] [Google Scholar]


