Abstract
INTRODUCTION
Nearly 1 in 40 of the population seeks medical advice related to a shoulder problem every year. The majority pertain to rotator cuff pathology. Prior to intervention in such patients it is imperative to define whether the tendons are intact or torn. Ultrasonography has become an essential adjunct to clinical assessment in diagnosing rotator cuff tears. This study was designed to investigate if a surgeon using a portable ultrasonography machine in a one-stop shoulder clinic could significantly reduce the time a patient waited from initial outpatient presentation to the end of the treatment episode (be it surgery, injection or conservative management).
METHODS
A total of 77 patients were allocated to one of two groups: Group A, consisting of 37 patients who were assessed and had ultrasonography as outpatients, and Group B, consisting of 40 patients who were assessed and referred for departmental ultrasonography where appropriate. Three clear outcome groups were defined: those who required surgical repair, those who had irreparable tears and those who declined surgery.
RESULTS
For all outcomes (surgery, irreparable tears and conservative treatment), the patients in Group A all completed their clinical episodes significantly quicker than those in Group B (p<0.02). As well as the time saving benefits, there was a substantial financial saving for Group A. By performing ultrasonography in the outpatients department, those patients avoided the requirement of departmental imaging (£120) and subsequent follow-up appointments (£73) to discuss results and management, resulting in a saving of nearly £200 per patient.
CONCLUSIONS
The use of a portable ultrasonography machine by an orthopaedic surgeon can significantly reduce the time to treatment and the financial cost for patients with rotator cuff tears.
Keywords: Shoulder, Ultrasonography, Outpatient, Tendon, Tear, Surgeon
Ultrasonography has become an essential adjunct to clinical examination when assessing patients with suspected rotator cuff pathology.1–6 The advantages of portable shoulder ultrasonography are that the surgeon can evaluate the integrity of the rotator cuff immediately in a one-stop clinic. This allows an efficient and effective treatment plan to be initiated. Shoulder ultrasonography is non-invasive, has virtually no side effects and allows the rotator cuff to be visualised dynamically during rotation and elevation of the shoulder. It is cost effective and time efficient and allows patients to see their own pathology, leading to better understanding of the disease process and a constructive discussion on the merits of treatment.
It has shown previously that a surgeon using portable ultrasonography in a one-stop clinic can accurately demonstrate whether there is a full thickness tear of the rotator cuff with a sensitivity of 96.2% and a specificity of 95.4%.1 This is as accurate as any series performed by a sonographically trained radiologist. This study set out to determine if there is any benefit in time efficiency and cost effectiveness from a one-stop clinic.
Methods
Patients attending the same shoulder clinic between November 2007 and July 2008 were allocated to one of two clinicians with a specialist interest in the shoulder. This process occurred as part of the standard outpatient allocation but did not involve patient pre-selection by either clinician. The clinicians had worked adjacent to each other in the same clinic for over eight years. As part of his standard initial assessment, one clinician performed his own ultrasonography examination of the shoulder in a one-stop clinic. Patients at this clinic formed Group A. The second clinician made a clinical diagnosis based on objective clinical findings and referred patients for departmental ultrasonography were appropriate. These patients formed Group B.
After discussion with the local trust research and ethics department, ethics approval was not sought for the following reasons: the retrospective study was comparing two clinical practices that were already well established within the trust and therefore did not change current practices, and it did not affect patient allocation or subsequent management in any way.
The primary assessment tool was the length of time from first clinic attendance to surgery. This was determined from a clinical notes review. The secondary assessment tool was length of time from first clinic assessment to non-surgical treatment or discharge. Finally, the difference in costs between the two patient pathways (Groups A and B) was calculated using the standard costs of clinic attendances and sonographic evaluation obtained from the trust’s coding department in line with National Health Service (NHS) figures. These assessments were made from clinical records by the third investigator, who had played no part in the clinical episodes of any of the patients.
The endpoint was defined as the date of surgery, the date of discharge from follow-up or the date that a clear decision to treat conservatively was documented in the case notes. A retrospective time period of eighteen months was chosen to ensure that all patients included in the study would have completed the episode of treatment related to the diagnosis being studied.
The inclusion criteria for the study were a clinical diagnosis of rotator cuff disease based on a history of true shoulder pain, made worse by reach, with positive impingement signs on a Neer, Hawkins—Kennedy or Jobe test. A total of 104 patients fitted these criteria.
Patients were excluded if they had incomplete clinical notes; if the dates of first attendance, ultrasonography appointments, subsequent clinical attendances and surgery had not been clearly recorded; if they requested deferral of surgery; and if they were lost to follow-up. A further 27 of the index 104 patients were excluded on these grounds, leaving 77 patients once all the inclusion and exclusion criteria had been applied.
The average age of the study patients was 62.4 years (range: 41—85 years). There was a slight preponderance of women with 45 compared with 32 men. It was clear that the patients were divided into three distinct outcomes. Thirty-eight underwent surgery (rotator cuff repair, subacromial decompression or debridement). Fifteen patients had an irreparable tear of the tendon. Twenty-four either refused surgery or were treated conservatively with an injection or physiotherapy. The demographics of each group are shown in Table 1.
Table 1.
Patient demographics
| Surgery | Irreparable tear | Conservative management | ||||
| Group A | Group B | Group A | Group B | Group A | Group B | |
| Number of patients | 20 | 18 | 7 | 8 | 10 | 14 |
| Average age (years) | 56.9 | 62.7 | 68.3 | 75.0 | 66.2 | 57.4 |
| Male-to-female ratio | 1:1 | 5:4 | 3:4 | 1:3 | 3:7 | 2:5 |
Results
The mean time from first clinical attendance to surgery for patients in Group A was 95.7 days and in Group B it was 205.3 days (Table 2). In effect, patients in the one-stop clinic halved their time to surgery or saved three months of the patient journey. This difference was statistically significant (p=0.002).
Table 2.
Mean interval from initial outpatient review to endpoint
| Outcome | |||
| Surgery | Irreparable tear | Conservative management | |
| Group A | 95.7 days | 16.4 days | 6.5 days |
| Group B | 205.3 days | 138.9 days | 95.4 days |
There was a significant cost saving for Group A. The NHS tariff for 2008—2009 gave the cost of a first clinical appointment as £149, subsequent outpatient charges were £73 and the cost of departmental ultrasonography of the shoulder was £120. As the one-stop scans were not reimbursed, this gave a pre-operative cost of £149 for Group A and £342 for Group B.
Not all patients with a clinical diagnosis of rotator cuff pathology were treated surgically. The patient journey for those who had an irreparable tear was an average of 16.4 days in Group A and 138.9 days in Group B. This difference was statistically significant (p=0.015). The reason why Group A did not register as zero days was that one patient required magnetic resonance imaging to confirm that the tear rated as massive on ultrasonography was actually not operable.
Of the 24 patients who either turned down surgery or had conservative treatment, those in Group A had a journey of 6.5 days and those in Group B 95.4 days. This was statistically significant (p=0.001). The reason that Group A did not have a journey of zero days was that a single patient requested a follow-up review after a subacromial injection.
The data were analysed using SPSS® version 17 (SPSS Inc, Chicago, IL, US) to compare the outcomes of Groups A and B. An independent t-test was used. Figures 1—3 clearly demonstrate the statistically significant differences between the time to treatment of the two patient groups for all three outcomes (surgery: p=0.002, irreparable tear: p=0.015, conservative management: p=0.001).
Figure 1.
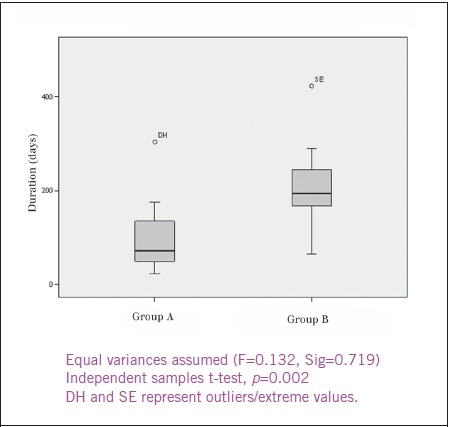
Interval from initial outpatient review to endpoint for patients with an outcome of surgery
Figure 2.
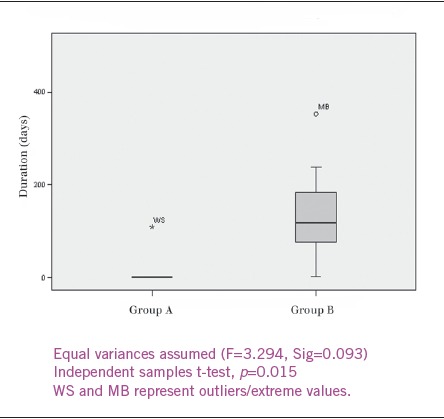
Interval from initial outpatient review to endpoint for patients with an outcome of irreparable tear
Figure 3.
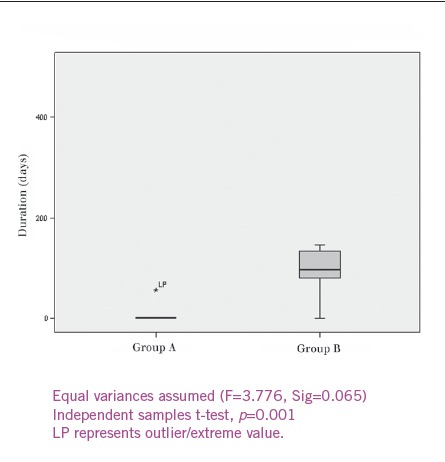
Interval from initial outpatient review to endpoint for patients with an outcome of conservative management
Discussion
The prevalence of adults attending primary care for new shoulder pain is now 1% per annum7 and 2.4% for acute and chronic shoulder problems.8 For the modern orthopaedic surgeon, 30—70% of the referrals received from primary care are for rotator cuff related disease.9,10 In such patients it is imperative to define whether the rotator cuff is torn. If a tear is present, it is necessary to establish the anatomy and the extent of the tear (small <1cm, medium 1—3cm, large 3—5cm or massive >5cm). This information allows a management strategy to be agreed between the patient and the surgeon, including need for surgery, arthroscopic or open, day case or inpatient, rehabilitation, immobilisation and return to work and activities, success rates and possible complications.
In a setting where the surgeon has access to portable ultrasonography, this informed discussion can occur at the initial presentation. Ultrasonography performed by a surgeon at the first clinic attendance is an accurate technique for diagnosing rotator cuff tears. It is comparable to magnetic resonance imaging.1—8,11—14 The senior author, a surgeon, has published results of ultrasonography for 143 consecutive patients in his outpatient clinic. In 78 patients who subsequently went on to have surgery for full thickness tears, 3 were under-diagnosed and 3 were over-diagnosed. This correlates to a sensitivity and positive predictive value of 96.2% and a specificity and negative predictive value of 95.4%.15 Surgeons’ use of portable ultrasonography is slowly gaining favour in continental Europe and America. It is still rare in the UK where patients are more commonly referred to the radiology department.
If the diagnosis of a rotator cuff tear can be confirmed or excluded at the first visit to the shoulder clinic, the need for further imaging and follow-up clinics is negated. For the majority of patients in this study, portable ultrasonography saved time for both the patient and the surgeon. It also meant that a firm diagnosis and management plan could be formulated and discussed with the patient and any queries answered at the time of the initial consultation.
The financial implications are also clear. The NHS tariffs for 2008—2009 quote the cost of a new patient outpatient clinic as £149 and a follow-up appointment as £73. The quoted tariff for outpatient ultrasonography is £120. In the eight-month period, 40 patients were sent for departmental ultrasonography. Had these patients had ultrasonography at the one-stop clinic (ie no need for departmental ultrasonography and subsequent follow-up appointment), there would have been a saving of £193 per patient. This correlates to a financial saving of £11,580 over one year. In an orthopaedic department such as ours, with three consultants and three senior assistants (fellows, extended role physiotherapists and surgical care practitioners) trained in the technique, this could save approximately £70,000 per year.
This study could be criticised in that the portable ultrasonography performed in clinic was not charged. However, two clinic appointments were still saved. Therefore, even if the scans had been charged, there would still be a financial saving of £146 per patient or £8,760 per year per surgeon or over £52,000 per department. This is still a considerable saving.
The modern portable ultrasonography machines cost between £15,000 and £40,000, with a mid-range model that is more than adequate to diagnose rotator cuff pathology costing approximately £20,000. This should make the equipment affordable to an orthopaedic department that is saving between £50,000 and £70,000 a year. Clearly, the purchase of the portable ultrasonography machine and subsequent training of the surgeon requires a considerable initial financial commitment. However, with the financial savings indicated above, a mid-range device could pay for its self after approximately two years, with only one surgeon using it.
Conclusions
This study has shown that the use of a portable ultrasonography machine by a suitably trained orthopaedic surgeon in a one-stop shoulder clinic can significantly reduce the time to treatment and the financial cost for patients with rotator cuff tears.
References
- 1.Al-Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008;90:889–892. doi: 10.1302/0301-620X.90B7.20481. [DOI] [PubMed] [Google Scholar]
- 2.Crass JR, Craig EV, Thompson RC, Feinberg SB. Ultrasonography of the rotator cuff: surgical correlation. J Clin Ultrasound. 1984;12:487–491. doi: 10.1002/jcu.1870120806. [DOI] [PubMed] [Google Scholar]
- 3.Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005;87:1,305–1,311. doi: 10.2106/JBJS.D.02100. [DOI] [PubMed] [Google Scholar]
- 4.Middleton WD, Edelstein G, Reinus WR, et al. Ultrasonography of the rotator cuff: technique and normal anatomy. J Ultrasound Med. 1984;3:549–551. doi: 10.7863/jum.1984.3.12.549. [DOI] [PubMed] [Google Scholar]
- 5.Middleton WD, Teefey SA, Yamaguchi K. Sonography of the rotator cuff: analysis of interobserver variability. Am J Roentgenol. 2004;183:1,465–1,468. doi: 10.2214/ajr.183.5.1831465. [DOI] [PubMed] [Google Scholar]
- 6.Ziegler DW. The use of in-office, orthopaedist-performed ultrasound of the shoulder to evaluate and manage rotator cuff disorders. J Shoulder Elbow Surg. 2004;13:291–297. doi: 10.1016/j.jse.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331:1,124–1,128. doi: 10.1136/bmj.331.7525.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology (Oxford) 2006;45:215–221. doi: 10.1093/rheumatology/kei139. [DOI] [PubMed] [Google Scholar]
- 9.Macfarlane GJ, Hunt IM, Silman AJ. Predictors of chronic shoulder pain: a population based prospective study. J Rheumatol. 1998;25:1,612–1,615. [PubMed] [Google Scholar]
- 10.Oh LS, Wolf BR, Hall MP, et al. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52–63. doi: 10.1097/BLO.0b013e31802fc175. [DOI] [PubMed] [Google Scholar]
- 11.Shahabpour M, Kichouh M, Laridon E, et al. The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. Eur J Radiol. 2008;65:194–200. doi: 10.1016/j.ejrad.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Teefey SA, Hasan SA, Middleton WD, et al. Ultrasonography of the rotator cuff. A comparison of ultrasonograhic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498–504. [PubMed] [Google Scholar]
- 13.Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors. Am J Roentgenol. 2005;184:1,768–1,773. doi: 10.2214/ajr.184.6.01841768. [DOI] [PubMed] [Google Scholar]
- 14.Teefey SA, Rubin D, Middleton WD, et al. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708–716. [PubMed] [Google Scholar]
- 15.Kayser R, Hampf S, Pankow M, et al. Validity of ultrasound examinations of disorders of the shoulder joint. Ultraschall Med. 2005;26:291–298. doi: 10.1055/s-2005-858525. [DOI] [PubMed] [Google Scholar]


