Abstract
Two studies assessed the role of self-compassion as a moderator of the relationship between physical health and subjective well-being in the elderly. In Study 1, 132 participants, ranging in age from 67–90 years, completed a questionnaire that assessed their perceptions of their physical health, self-compassion, and subjective well-being. Participants who were in good physical health had high subjective well-being regardless of their level of self-compassion. However, for participants with poorer physical health, self-compassion was associated with greater subjective well-being. In Study 2, 71 participants between the ages of 63 and 97 completed a questionnaire assessing self-compassion, well-being, and their willingness to use assistance for walking, hearing, and memory. Self-compassionate participants reported being less bothered by the use of assistance than those low in self-compassion, although the relationship between self-compassion and willingness to use assistive devices was mixed. These findings suggest that self-compassion is associated with well-being in later life and that interventions to promote self-compassion may improve quality of life among older adults.
Keywords: self-compassion, well-being, aging
Life expectancy has nearly doubled in the past century as a result of advances in medical care, improved sanitation, and industrialization. As a result, most people in Western societies now live long enough to experience various physical, cognitive, and social changes that accompany aging, some of which may undermine their well-being and life satisfaction in later life (Mirowsky & Ross, 1992). With increasing age, the likelihood of experiencing stressors such as the death of a partner or friend, declining mental and physical health, dependency on one’s children, and lowered ability to engage in enjoyable and fulfilling activities increases (Baltes & Baltes, 1990; Lee & Markides, 1990; Manton, 1990; Singer, Verhaeghen, Ghisletta, Lindengerger, & Baltes, 2003).
Because older people show great variability in how they cope with aging, research has investigated potential mediators and moderators of the link between people’s objective circumstances and their subjective quality of life (Cheng, 2004; George, 2006; Kunzmann, Little, & Smith 2000). The role of factors such as perceived control, social support, and self-esteem has been investigated to understand the connection between objective and subjective well-being in old age. For example, maintaining a sense of control is related to well-being and life satisfaction throughout life (Bailis & Chipperfield, 2002; Ferguson, & Goodwin, 2010; Baltes, Staudinger, & Lindenberger, 1999; Bandura, 1997; Rodin, Timko, & Harris, 1985; Schulz & Heckhausen, 1999; Skinner, 1996), but as people age they often cannot control the consequences of the aging process and must adapt to their changing circumstances. Likewise, social support predicts well-being throughout the lifespan, and research indicates that people who have more social support experience fewer physical and mental declines as they age (Adelmann, 1994; Glass, Mendes de Leon, Marottoli, & Berkman, 1999; Harlow & Cantor, 1996; Seeman, Lusignolo, Albert & Berkman, 2001; Young & Glasglow, 1998).
Similarly, self-esteem relates positively to life satisfaction among older adults (Fagerstrom et al., 2007). Given that cross-sectional and longitudinal data show that self-esteem declines with age (Ranzjin, Keeves, Luszcz, & Feather, 1998; Robins, Trzesniewski, Tracy, Gosling, & Potter, 2002), the fact that subjective well-being increases with age suggests that many older adults engage in strategies that help to preserve well-being despite lower self-esteem. For example, older people may use more effective coping and emotion regulation strategies than younger people (Baltes & Baltes, 1990; Brandstaedter & Greve, 1994; Carstensen, Isaacowitz, & Charles, 1999). Furthermore, Erikson (1968) suggested that older adults are more accepting of themselves and, thus, have less of a need to self-aggrandize and self-promote.
Our focus in this paper is on the role that self-compassion may play in accounting for differences in well-being among older individuals. According to Neff (2003a, p. 224), self-compassion involves “being open to and moved by one’s own suffering, experiencing feelings of caring and kindness toward oneself, taking an understanding, nonjudgmental attitude toward one’s inadequacies and failures, and recognizing that one’s experience is part of the common human experience.” People who are self-compassionate treat themselves kindly when things go wrong, do not exacerbate their negative emotions by personalizing their difficulties, and maintain a more objective perspective on their situation. Just as people show compassion to loved ones who experience difficulties in life, self-compassionate individuals respond to their own problems with self-directed kindness and concern rather than with self-criticism, pity, or broad personalization (Neff, 2003b). Unlike self-esteem, which is based on favorable judgments of one’s personal characteristics and social acceptability, self-compassion does not depend on viewing oneself positively and, in fact, may be most beneficial when events undermine one’s sense of competence, control, or value. Furthermore, unlike self-esteem, self-compassion is not associated with self-aggrandizement or narcissism (Leary, Tate, Adams, Allen, & Hancock, 2007; Neff & Vonk, 2009).
Self-compassion may contribute in important ways to understanding well-being in older people because differences in how people react to age-related changes in health, mental capacity, and life circumstances may reflect how compassionately they treat themselves when problems arise. Adopting a self-compassionate mindset should affect how older adults feel about aging and themselves, as well as their reactions to inevitable challenges, failures, and losses. Furthermore, unlike many predictors of well-being, self-compassion can be taught to people who are particularly self-critical (Gilbert & Procter, 2006).
Studies of young adults show that self-compassion correlates highly with mental health and adjustment, including lower depression, lower anxiety, and higher life satisfaction (Neff, 2003b). Self-compassion also has positive associations with happiness, optimism, positive affect, wisdom, personal initiative, curiosity, and agreeableness, and a negative relationship with neuroticism (Neff, Rude, & Kirkpatrick, 2007b). These findings show self-compassion to be related to adaptive functioning, particularly in the face of failures, losses, and life stress (Leary et al., 2007). Importantly, the relationships between self-compassion and psychological well-being are independent of those of self-esteem (Leary et al., 2007; Neff, 2003b). Indeed, research suggests that self-compassion may uniquely predict well-being more strongly than self-esteem (Leary et al., 2007).
Experimental studies of self-compassion have also shown that self-compassion moderates reactions to negative or difficult situations, helping people to react with greater equanimity toward themselves, other people, and the difficulties that they experience. Although self-compassionate responses could also be interpreted as indifference, indulgence, or a refusal to accept responsibility, on the contrary, people who are self-compassionate are more likely to accept responsibility for their mistakes and failures and to take initiative when personal changes are needed than those who are less self-compassionate (Leary et al., 2007, Neff et al., 2007a). A self-compassionate stance allows people to accept responsibility and to move on rather than engaging in denial, defensiveness, or excessive self-blame.
Although research has shown that self-compassion moderates reactions to stressful events among young adults, no research has examined self-compassion among older people. Based on research on younger people, we have every reason to expect that self-compassion predicts well-being in older people as well. In fact, self-compassion may become increasingly important for well-being as people age. Some of the changes that older adults commonly experience, such as memory failures and the inability to perform everyday tasks, lead some individuals to become self-critical and angry, castigating themselves and bemoaning their lowered ability to function as they once did (Mirowsky & Ross, 1992). However, adopting a self-compassionate mindset should help people be more accepting of their lapses, failures, and inadequacies. Other negative experiences, such as the loss of a loved one, may evoke anger or despair even without self-blame, and self-compassion should buffer the impact of these events as well. Self-compassion seems to protect people both when they are personally responsible for the negative event and when the event is beyond their control (Leary et al., 2007, Study 1). Thus, self-compassion may help older people deal with an array of negative events and circumstances.
Even when older adults are not yet experiencing negative life changes, self-compassion may play a role in how they prepare for the future. Aging can be a looming stressful event for those approaching the later part of life. Some people, including those who are high in trait self-esteem (Sneed & Krauss Whitbourne, 2001), may deny or ignore the possibility of negative changes for as long as possible. However, people who are high in self-compassion should be more likely to act proactively. Just as compassion directed towards others leads people to promote the others’ welfare proactively, self-compassion should lead people to take better care of themselves. For example, because they accept their failings, problems, and inadequacies with greater equanimity, self-compassionate older adults may be more likely to follow medical advice that will promote their long-term health and seek medical assistance more quickly when they need it. Self-compassionate older adults may also be more willing to accept assistance from others because they are less likely to deny their problems and more likely to take responsibility for their well-being. All of these considerations suggest that self-compassion may be linked to greater well-being in later life.
Two studies tested the relationship between self-compassion and well-being in older adults. Study 1 tested the hypothesis that self-compassion moderates the relationship between physical health and subjective well-being such that self-compassion should buffer participants who report poorer physical health from experiencing a decline in subjective well-being. Study 2 investigated the relationship between self-compassion and people’s willingness to engage in health-promoting behaviors. We hypothesized that self-compassion is positively related to willingness to use more physical assistance, and that highly self-compassionate participants are less embarrassed by using such assistance. Finding support for these hypotheses would contribute to growing evidence that teaching people to be more self-compassionate may lead to more adaptive emotions and behaviors in the face of adversity.
Study 1
Study 1 examined the relationship between physical health, self-compassion, and well-being in older adults. Because older people who are more self-compassionate should weather the negative effects of aging more gracefully, self-compassion should be associated with a variety of indices of well-being. Furthermore, the effects of self-compassion should be strongest when people are experiencing negative life events. Thus, we predicted that self-compassion would moderate the relationship between physical health and subjective well-being such that individuals who have poorer health will benefit the most from being self-compassionate.
Method
Participants
The participants were 132 adults (58 male, 72 female) between the ages of 67 and 90 years. Participants were recruited from a volunteer registry provided by the Duke Center for Aging. This registry contains contact information for approximately 2,000 volunteers over the age of 60 who are interested in participating in research studies. In our sample, 98% of the participants were Caucasian. Of the 132 participants, 83 were married, 6 were single, 15 were divorced, and 28 were widowed. Only 10 of the participants reported not having children.
Procedure
The Duke Center for Aging provided contact information for 359 adults over the age of 65 living in the local area. These individuals were mailed letters that described the study (which was described as a study of “Self-image, Life Circumstances, and Reactions to Aging”) and asked them to contact the researcher if they were interested in participating. Participants were told that the questionnaire would require 45–60 minutes of their time for which they would receive $10.00 and that they could participate by either having the questionnaire mailed to them (along with return postage) or coming to campus to complete the questionnaire. Of the 359 people contacted, all 138 who responded requested that the questionnaire packet be mailed to them. The questionnaire packets included a page of instructions, the informed consent form, a payment form, a questionnaire booklet containing the measures described below, and a return envelope. Of the 138 questionnaires that were returned, 6 were discarded due to extensive missing data. Participants who returned the questionnaire packet were mailed a check for $10.00.
Measures
Means, standard deviations, and Cronbach’s alpha coefficients for the following measures are reported in Table 1.
Table 1.
Correlations for Study 1
| M | SD | α | SC | Pain | GH | M | H | P | GWB | SA | EP | LS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SC | 3.69 | .52 | .87 | ||||||||||
| Pain | 2.27 | 1.02 | .85 | −.25** | |||||||||
| GH | 3.72 | .80 | .74 | .17* | −.62** | ||||||||
| M | 23.4 | .54 | .93 | .05 | −.66** | .63** | |||||||
| H | 5.52 | 1.46 | .78 | .03 | −.26** | .27** | .21* | ||||||
| P | 3.40 | 1.83 | NA | .03 | .39** | −.36** | −.31** | −.11 | |||||
| GWB | 4.87 | .64 | .91 | .49** | −.54** | .50** | .34** | .29** | −.26** | ||||
| SA | 3.66 | .85 | .73 | .27** | −.52** | .64** | .47** | .29** | −.16 | .59** | |||
| EP | .32 | .82 | .95 | −.25** | .30** | −.24** | −.20* | −.03 | .07 | −.30** | −.14 | ||
| LS | 5.28 | 1.18 | .84 | .31** | −.36** | .40** | .30** | .11 | −.27** | .67** | .55** | −.27** | |
| SF | 4.50 | .88 | .84 | .28** | −.52** | .46** | .46** | .12 | −.24** | .56** | .41** | −.27** | .44** |
Note.
p < .05,
p < .01
Variable Names: Self-compassion (SC), General Health (GH), Mobility (M), Hearing (H), Number of Medical Problems (P), General Well-Being (GWB), Successful Aging (SA), Emotional Problems (EP), Life Satisfaction (LS), and Social Functioning (SF)
Self-compassion
Self-compassion was measured using the Self-Compassion Scale (Neff, 2003b). This scale includes 26 items designed to measure three components of self-compassion: self-kindness (e.g., “I’m kind to myself when I’m unhappy or experiencing suffering”), common humanity (e.g., “When I’m down, I remind myself that there are lots of other people in the world feeling like I am”), and mindfulness (e.g., “When something painful happens, I try to take a balanced view of the situation”). Responses are given on a 5-point scale from almost never to almost always and were averaged to create an index of self-compassion.
Pain
Self-reports of pain were obtained using the bodily pain subscale of the SF-36 (Ware & Sherbourne, 1992; see Brazier et al., 1992 for information regarding reliability and validity). Participants reported how much pain they had experienced in the past four weeks on a 6-point scale from never to very severe and how much their pain interfered with their everyday life on a 5 point scale from not at all to extremely. These items were averaged to create a measure of pain.
General health
Self-reports of general health were obtained using the general health subscale of the SF-36 (Ware & Sherbourne, 1992). Participants answered four questions assessing their health in relation to other people. For example, participants responded to “I am as healthy as anybody I know” on a 5-point scale from definitely true to definitely false. These four questions were averaged to create an index of general health.
Mobility
Self-reports of mobility were obtained using the physical functioning subscale of the SF-36 (Ware & Sherbourne, 1992). Participants were asked how much their health limited them in 10 activities over the past 4 weeks on a 3-point scale (yes, limited a lot; yes, limited a little; and no, not limited at all). The activities included: vigorous activities such as running, moderate activities such as moving a table, lifting or carrying groceries, climbing several flights of stairs, climbing one flight of stairs, bending, kneeling or stooping, walking more than a mile, walking several blocks, and less vigorous activities such as walking one block and bathing or dressing. These items were summed to get an index of mobility.
Hearing
Participants were asked “Do you have difficulty hearing other people when they speak to you face-to-face?” and “Do you have difficulty hearing other people when they speak to you over the phone?” Responses were given on a 4-point scale from always to never with higher scores indicating better hearing. These two items were summed to create a measure of hearing.
Number of medical problems
Participants were asked to indicate if they had problems with or had been diagnosed with cataracts, hypertension, arthritis, depression, asthma, coronary heart disease, high cholesterol, back pain, diabetes, cancer, stroke, or osteoporosis. These items were summed to create a total medical problems score.
General well-being
Sixteen items from the General Well-being Index (Dupuy, 1984) measured psychological well-being. Example items were “Have you been in firm control of your behavior, thoughts, emotions, or feelings?,” “Has your daily life been full of things that are interesting to you?,” and “How happy, satisfied, or pleased have you been with your personal life?” Response scales varied, but in all cases, higher numbers indicated more positive well-being, and these items were standardized and averaged to create an index of well-being. This average was then back-transformed to create an index of well-being using the original scale metric.
Successful aging
The degree to which participants believed that they were aging well was measured with the five items from the Attitude toward Own Aging scale (Lawton, 1975; Liang & Bollen, 1983). Questions included “I am aging successfully,” “As people get older, they are less useful,” and “I am as happy now as I was when I was younger.” Participants responded on a 5-point scale from strongly agree to strongly disagree and the 5 items were averaged to create an index of successful aging.
Emotional problems
The role-emotional subscale of the SF-36 assessed whether emotional problems had interfered with work or daily activities in the past 4 weeks (Ware & Sherbourne, 1992). The 3 items asked whether emotional problems had led participants to cut down on the amount of time they spent on work or other activities, accomplished less than they would have liked, and did not do work or other activities as carefully as usual. Respondents answered yes or no to each item and items were averaged to create an index of emotional problems.
Life satisfaction
Participants completed the Satisfaction with Life Scale (Diener, Emmons, Larsen, & Griffin, 1985). This scale includes 5 items that are answered on 7-point response scales ranging from strongly agree to strongly disagree. The items were averaged to create an index of life satisfaction.
Social functioning
Participants completed the social functioning subscale of the SF-36 (Ware & Sherbourne, 1992). These 2 items assess the extent to which physical health and emotional problems interfered with normal social activities in the past 4 weeks on a 5-point scale. The scale was scored so that higher numbers reflect less interference and better social functioning. The two items were averaged to create an index of social functioning.
Results
Table 1 shows correlations between all pairs of variables. As can be seen, self-compassion correlated moderately with all of the indices of psychological and social well-being (e.g., general well-being, successful aging, emotional problems, life satisfaction, social functioning) but less so with the indices of physical health, with the exception of pain, which correlated negatively with self-compassion. Importantly, the mean self-compassion score (M = 3.69) was approximately .7 units higher than the mean found with college student samples in previous studies.
All continuous predictors were zero-centered and interaction terms were created by multiplying self-compassion by each predictor. Two predictors, mobility and hearing, were skewed in a positive direction; therefore, we dichotomized both variables. Participants who reported above average mobility (score of 23.4 or higher) received a score of 1, and participants with below average mobility were given a 0. Because the measure of hearing was based on only 2 questions, participants who reported that they “rarely” or “never” had trouble hearing people face-to-face or over the phone were assigned a 1 and participants who reported “always” or “sometimes” to either question were assigned a 0.
To test the hypothesis that self-compassion moderates the relationship between physical health and psychological/emotional well-being, a series of hierarchical multiple regression analyses was conducted to test the main effects of self-compassion, health indicators, and their interactions on each measure of well-being. In each analysis, self-compassion was entered on Step 1, the health indicators (pain, general health, number of problems, hearing, and mobility) were entered on Step 2, and the 2-way interactions between self-compassion and each health indicator were entered in Step 3 (Table 2). Significant interactions were decomposed using the Johnson-Neyman (J-N) technique (Potthoff, 1964) to identify the point along the regression line at which differences between groups reached significance. Preacher, Curran, and Bauer (2006) described how the J-N approach should be used to probe interactions in multiple linear regression. As opposed to the traditional “pick-a-point” approach, the J-N technique provides information about the effect of a predictor variable (x) on an outcome variable (y) across the entire range of the moderating variable. The J-N technique yields regions of significance that show the range of values for which the proposed moderator variable significantly moderates the relationship of x on y. Instead of testing specific simple slopes, the regions of significance provide an inferential test of all possible simple slopes of x on y. However, for the purpose of graphing these interactions, the pick-a-point approach is necessary. The x-axis is anchored by the lowest and highest observed values of the predictor variable, and the moderator variable is graphed at the values of −1 SD, the mean and +1SD. In all cases an alpha level of .05 was used to determine the point at which the two regression lines begin to significantly differ.
Table 2.
Study 1: Hierachical Multiple Regression Analyses Predicting Psychological Well-Being from Self-compassion and Indices of Physical Health (Number of Problems, Hearing, Mobility, Pain, and General Health)
| Predictor | Measures of Psychological Well-Being
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| General Well-Being | Life Satisfaction | Successful Aging | Emotional Problems | Social Functioning | ||||||
|
| ||||||||||
| ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1 | .24*** | .09*** | .06** | .07** | .08** | |||||
| SC | .49*** | .30*** | .25** | −.26** | .27** | |||||
| Step 2 | .27*** | .17*** | .42*** | .12** | .22*** | |||||
| Problems | −.12 | −.17* | .13 | .12 | −.06 | |||||
| Hearing | .08 | −.08 | .03 | .08 | .01 | |||||
| Mobility | −.05 | .07 | .07 | .01 | .10 | |||||
| Pain | −.28** | −.08 | −.14 | .26* | −.22* | |||||
| GenHealth | .25** | .22* | .56*** | −.06 | .21* | |||||
| Step 3 | .06** | .08** | .01 | .07 | .02 | |||||
| SC x Problems | .03 | .09 | −.04 | −.20* | −.02 | |||||
| SC x Hearing | .04 | .10 | .07 | −.13 | −.10 | |||||
| SC x Mobility | .24 | .38* | −.02 | −.08 | .17 | |||||
| SC x Pain | .19* | .27* | .08 | −.01 | .07 | |||||
| SC x GenHealth | −.19* | −.17 | −.03 | .18 | .12 | |||||
| Total R2 | .57*** | .35*** | .49*** | .25*** | .32*** | |||||
| n | 128 | 126 | 129 | 129 | 127 | |||||
Note.
p < .05.
p < .01.
p <.001.
General Well-Being
A hierarchical multiple regression analysis using general well-being as the outcome variable revealed a main effect of self-compassion, pain, number of problems, and general health. In addition to the fact that participants who were higher in self-compassion scored higher in general well-being than participants who were low in self-compassion (t (127) = 6.35, p <.001, β = .49), participants with lower levels of pain (t (122) = −3.15, p =.002, β = −.28), fewer physical problems (t (122) = −1.74, p =.084, β = −.12), and better general health (t (122) = 2.93, p =.004, β = .25) reported higher general well-being.
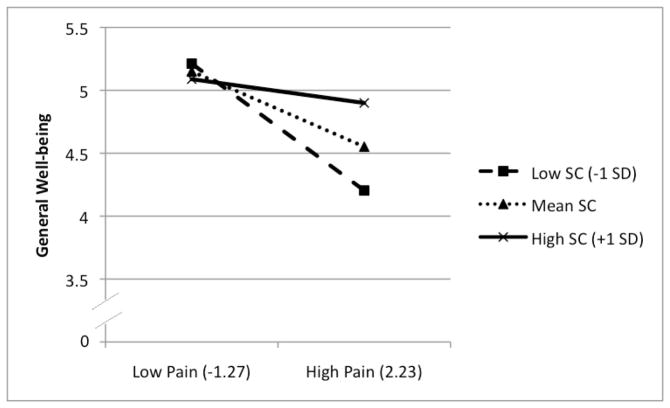
As predicted, these effects were qualified by significant interactions. As shown in Figure 1, among participants who were high in pain, those who scored high in self-compassion reported higher well-being than participants who scored low in self-compassion (t (117) = 2.24, p =.027, β = .19). Using the J-N technique, we calculated, in standard deviation units, the range of self-compassion values for which pain significantly predicted general well-being. Analyses showed that when self-compassion was at or above .46 SD above the mean, reported pain was significantly related to general well-being. It is also possible to reverse the focal predictor (pain) and moderator (self-compassion) to determine the range of pain scores for which self-compassion predicts well-being. Analyses showed that when reported pain was at or above .97 SD below the mean, participants higher in self-compassion had significantly higher well-being than those with low self-compassion. In other words, self-compassion was associated with greater well-being only among participants who experienced a relatively high amount of pain.
Figure 1.
Study 1: Interaction of self-compassion and pain on general well-being
Note. Graph shows moderating effects of self-compassion on the relationship between reported pain and general well-being. Values on the x-axis are the lowest and highest standardized observed values for reported pain.
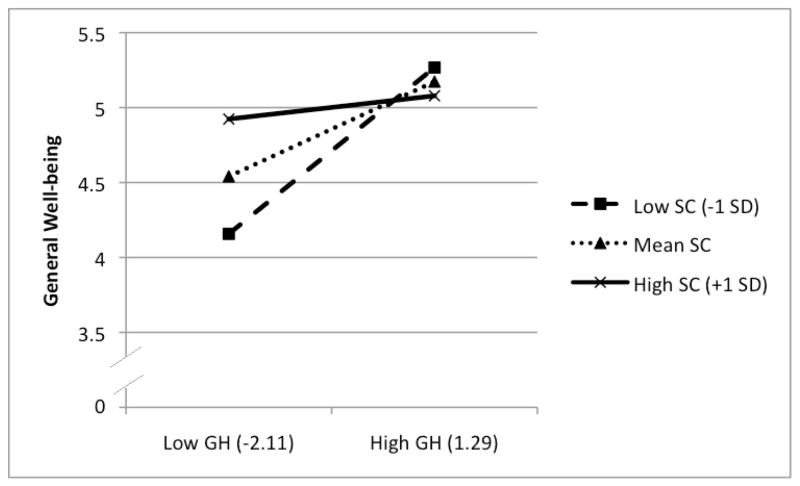
Similarly, participants who reported low general health but were self-compassionate reported higher well-being than participants low in self-compassion (t (117) = −2.20, p =.03, β = −.19). Self-compassion scores of .37 SD above the mean or higher significantly moderated the effect of general health on general well-being. Reversing general health and self-compassion, we can see the point along the general health dimension at which self-compassion makes a difference. As illustrated by Figure 2, self-compassion significantly predicted well-being for participants who had general health scores falling at or below 1 SD above the mean. The poorer one’s health, the more strongly related self-compassion was to maintaining well-being.
Figure 2.
Study 1: Interaction of self-compassion and general health ratings on general well-being
Note. Graph shows moderating effects of self-compassion on the relationship between reported general health and general well-being. Values on the x-axis are the lowest and highest standardized observed values for general health.
The self-compassion by mobility interaction showed that when self-compassion was at or below .41 SD above the mean, participants with greater mobility reported higher well-being than participants with lower mobility (t (117) = 1.89, p =.061, β = .24). Given that mobility was a dichotomous variable, we cannot identify the point along the mobility scale at which self-compassion becomes relevant. This interaction shows that having poor mobility can be detrimental to well-being and this relationship is magnified when people are low in self-compassion.
Life Satisfaction
Main effects showed that participants who were higher in self-compassion (t (125) = 3.52, p <.001, β = .30), had fewer physical problems (t (120) = −1.96, p =.053, β = −.17), or reported better general health (t (120) =2.10, p =.038, β = .22) reported higher life satisfaction.
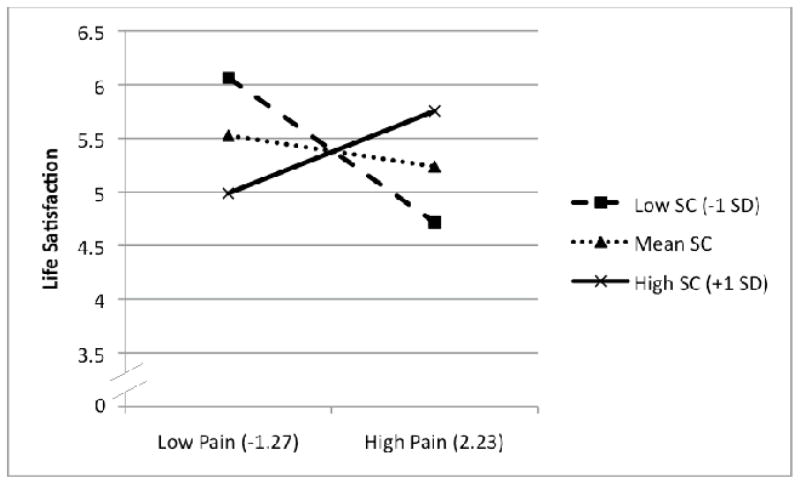
A self-compassion by pain interaction (see Figure 3) showed that pain significantly predicted life satisfaction when self-compassion was .71 SD below the mean or higher (t (115) = 2.52, p =.013, β = .27). Stated differently, participants who reported relatively low pain reported high life satisfaction regardless of their self-compassion scores. However, high self-compassionate participants reported significantly higher life satisfaction than low self-compassionate participants when their reported pain was .25 SD below the mean or higher. Viewing the interaction in the other direction, pain was unrelated to emotional problems and life satisfaction among people who were high in self-compassion but significantly related to these indices of well-being among people who were low in self-compassion.
Figure 3.
Study 1: Interaction of self-compassion and pain on life satisfaction
Note. Graph shows moderating effects of self-compassion on the relationship between reported pain and life satisfaction. Values on the x-axis are the lowest and highest standardized observed values for reported pain.
The self-compassion by mobility interaction showed that when self-compassion was at or below .66 SD above the mean, participants with greater mobility reported higher life satisfaction than participants with less mobility (t (115) = 2.43, p =.017, β = .38). This interaction shows that having poor mobility is associated with lower life satisfaction for older people who are low in self-compassion.
Social Functioning
Analysis of reported social functioning revealed main effects of self-compassion, pain, and general health. Participants who were higher in self-compassion (t (129) = 3.20, p <.001, β = .27), lower in reported pain (t (124) = −2.06, p =.042, β = −.22), or higher in general health (t (124) = 2.04, p =.044, β = .21) reported better social functioning. No interactions were obtained.
Emotional Problems
The analysis of emotional problems showed that participants who were lower in self-compassion (t (128) = −3.01, p = .003, β = −.26) or higher in reports of pain (t (123) = 2.26, p =.026, β = .26) reported more emotional problems. A significant self-compassion by number of medical problems interaction (t (118) = −2.16, p =.033, β = −.20) showed that when self-compassion was .21 SD below the mean or higher, the number of reported physical problems predicted emotional problems. Put another way, when reported physical problems were at or above .83 SD below the mean, participants higher in self-compassion reported fewer emotional problems than participants low in self-compassion (see Figure 4). In sum, self-compassion was related to fewer emotional problems for participants who reported more physical problems.
Figure 4.
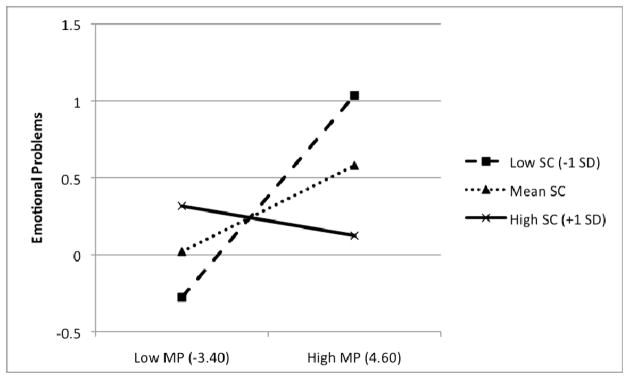
Study 1: Interaction of self-compassion and number of medical problems (MP) on emotional problems
Note. Graph shows moderating effects of self-compassion on the relationship between number of medical problems and emotional problems. Values on the x-axis are the lowest and highest standardized observed values for number of reported medical problems.
Successful Aging
Participants who were high in self-compassion (t (128) = 2.87, p = .005, β = .25), or high in general health (t (123) = 6.34, p < .001, β = .56) reported aging more successfully. None of the two-way interactions were significant.
Discussion
As hypothesized, indicators of physical health and self-compassion were both related to measures of well-being among older adults. Of course, the fact that people who report poorer health have lower subjective well-being is unsurprising. Furthermore, the main effects of self-compassion on general well-being, life satisfaction, social functioning, emotional problems, and successful aging are consistent with research on young adults showing that self-compassionate people report more positive emotions and reactions (Leary et al., 2007; Neff et al., 2007a).
More importantly, the presence of significant interactions showed that, as predicted, self-compassion was particularly beneficial for participants who reported more negative life circumstances. Of the 6 significant interactions, 3 were obtained for the measure of general well-being, showing that participants high in self-compassion experienced higher well-being even when reporting greater physical pain, poorer general health, and lower mobility.
Although self-compassion was related to positive outcomes across the board, the interactions suggest that self-compassion may be particularly important for people experiencing negative life events. Self-compassion seems to be a powerful moderator of the relationship between physical health and subjective well-being and helps to explain variance in how people deal with the negative aspects of getting older. People who respond to these problems self-compassionately should have a greater chance of maintaining well-being throughout later life.
Study 2
Study 1 showed that self-compassion may protect older individuals who experience negative life events from a decline in well-being. In part, this effect is probably due to the coping strategies that are inherent in the self-compassionate mindset (Allen & Leary, 2010). However, the possibility exists that, in addition to coping differently with negative events after they occur, self-compassionate people engage in patterns of behavior that promote their well-being under difficult circumstances. Just as people show others compassion by treating them in ways that offer help, encourage healthful behaviors, and promote their well-being, self-compassionate people may treat themselves in similar caring ways.
For example, research on self-compassion shows that people who are higher in self-compassion take more initiative when dealing with their personal failings than less self-compassionate people do (Neff, Hsieh, & Dejitterat, 2005; Neff et al., 2007b). Consequently, older adults who score high in self-compassion might be more likely to admit when they are having difficulties, to seek assistance for their problems, and to be less resistant and defensive to receiving help when needed, while also doing everything that they can reasonably do for themselves. Study 2 examined whether older people who are higher in self-compassion are more willing to use assistive devices such as walkers, wheelchairs, and hearing aids as well as to engage in memory tactics that will improve their cognitive performance. We predicted that self-compassionate people should be more accepting of their limitations and more inclined to take proactive measures to improve well-being than people who are lower in self-compassion.
Method
Participants
Participants were 71 individuals (16 male, 54 female, and 1 not indicated) who were recruited from a local independent living facility. Participants ranged in age from 63 to 97 years. They were compensated $10 for their participation.
Procedure
Participants were recruited through a local independent living facility. The study was announced in the center’s newsletter and advertised on flyers in the main building. Participants were told that the survey would take 45–60 minutes and that they would be paid $10.00 for participating. Participants picked up questionnaires from a box in the center’s mail room, completed the surveys in their residences, and returned them to the front desk at the facility in sealed envelopes. Of the 72 surveys returned, only 1 was discarded due to poor mental status. Checks were mailed directly to the participants.
Measures
Means, standard deviations, and Cronbach’s alpha coefficients (reported only for scale measures) for are shown in Table 3.
Table 3.
Correlations for Study 2
| M | SD | α | SC | DEP | I | AS | WD | WP | WW | WB | WC | HD | HR | HB | HC | MD | MT | MB | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SC | 3.68 | .50 | .69 | ||||||||||||||||
| DEP | 1.13 | .14 | .73 | −.32** | |||||||||||||||
| I | 1.15 | .50 | .90 | −.26* | .40** | ||||||||||||||
| AS | 2.36 | .76 | .64 | .29* | −.50** | −.39** | |||||||||||||
| WD | 1.55 | 1.11 | -- | −.08 | .39** | .81** | .37** | ||||||||||||
| WP | 1.39 | .86 | -- | −.07 | .14 | .31* | .15 | .57** | |||||||||||
| WW | 1.45 | 1.13 | -- | .05 | .24* | .25* | .17 | .59** | .52** | ||||||||||
| WB | 1.84 | 1.13 | -- | −.31* | .61** | .44** | .50** | .52** | .54** | .36** | |||||||||
| WC | 1.53 | .84 | -- | −.19 | .32* | .24 | .36** | .41** | .50** | .23 | .79** | ||||||||
| HD | 2.24 | 1.14 | -- | .03 | .17 | −.01 | .30* | .09 | .04 | .22 | .16 | .19 | |||||||
| HR | 2.43 | .96 | -- | −.17 | .05 | −.05 | .16 | .07 | .21 | .26* | .14 | .24 | .66** | ||||||
| HB | 1.64 | .92 | -- | −.05 | .42** | .14 | .35* | .14 | −.05 | .22 | .21 | .16 | .64** | .49** | |||||
| HC | 2.25 | 1.16 | -- | −.07 | .17 | −.02 | .30* | −.06 | −.10 | .00 | .19 | .22 | .67** | .59** | .67** | ||||
| MD | 2.78 | 1.00 | -- | −.06 | .25* | .16 | .10 | .22 | .05 | .20 | .20 | .33* | .25* | .25* | .23 | .17 | |||
| MT | 2.93 | .92 | -- | .26* | .04 | .04 | .01 | .12 | .18 | .14 | .12 | .19 | .25* | .17 | .20 | .17 | .14 | ||
| MB | 2.97 | .89 | -- | −.03 | .30* | .13 | .31** | .02 | −.03 | .01 | .16 | .14 | .19 | .16 | .23 | .32** | .47** | .21 | |
| MC | 1.94 | .92 | -- | −.17 | .30* | −.02 | .15 | −.07 | .10 | .03 | .23 | .11 | .10 | .04 | .25* | .21 | .31* | .21 | .36** |
Note.
p < 0.05,
p < 0.01
Variable Names: Self-compassion (SC), Depression (DEP), Impairment (I), Aging Successfully (AS), Walking Difficulty (WD), Use of Another Person for Assistance (WP), Use of a Walker for Assistance (WW), Bothered by Walking Difficulty (WB), Effort to Conceal Walking Difficulty (WC), Hearing Difficulty (HD), Asking People to Repeat Themselves (HR), Bothered by Hearing Difficulty (HB), Effort to Conceal Hearing Difficulty (HC), Memory Difficulty (MD), Use of Memory Tricks and Strategies for Assistance (MT), Bothered by Memory Difficulty (MB), and Effort to Conceal Memory Difficulty (MC).
Self-compassion
After receiving feedback from participants in Study 1 that the Self-Compassion Scale (Neff, 2003b) seemed too long, we shortened the original 26-item scale to 12 items that included the four items that loaded highest on each of the three factors (self-kindness, common humanity, and mindfulness). The shortened scale correlated 0.91 with the original 26-item scale, and the mean of the shortened scale was 3.68 (compared to 3.69 for the original scale in Study 1). However, the reliability for the shortened scale was .69 as compared to .87 for the full version used in Study 1. After the current study was conducted, Raes, Pommier, Neff, and Van Gucht (in press) created a different 12-item version of the Self-compassion Scale with a reported reliability of .87, suggesting that it might be a more reliable scale than the shortened scale created here. Given that all 26 items were administered in Study 1, the two shortened self-compassion scales can be compared within that study to assess their relative reliability with an older population. Our shortened scale had an alpha coefficient of .73 and correlated .95 with the full version of the scale, whereas the version created by Raes et al. (in press) had a reliability coefficient of .75 and correlated .95 with the long version of the scale. These comparisons show that the two brief versions of the Self-Compassion Scale are essentially equivalent in assessing self-compassion in older adults. However, the reliability of the scales is slightly lower than what is typically found in younger samples.
Geriatric Depression Scale
This 15-item scale was found to have 92% sensitivity and 89% specificity when evaluated against depression diagnostic criteria (Kurlowicz & Greenberg, 2007). Ten items on the scale indicate presence of depression when answered positively (“Do you feel your life is empty”), while the rest indicate depression when answered negatively (“Are you basically satisfied with your life?”). Every depressive answer was scored as a 2 and each non-depressed answer was given a 1, and then the ten items were averaged.
Level of impairment
Participants were asked questions about their general health and daily activities. Participants rated the degree to which they require help with personal care, cutting food, getting in and out of bed or a chair, getting dressed, getting up and down stairs, and bathing themselves on a scale of 1 (not at all) to 5 (a lot). The six items were averaged to create index of impairment.
Aging successfully
The Attitude toward Own Aging Scale (Lawton, 1975; Liang & Bollen, 1983) described earlier was again used.
Physical and mental difficulties
Participants rated their level of difficulty walking without assistance, hearing without a hearing aid, and remembering people’s names. Participants responded on a 5-point scale from not at all difficult to extremely difficult.
Use of assistance
Participants responded on a 5-point scale (from never or almost never to almost always) to questions assessing their use of various forms of assistance: using a walker for stability when walking from one place to another, using another person for stability when walking from one place to another, asking people to repeat what they are saying, and using mnemonic tricks, strategies, or techniques to remember things.
Bothered by assistance
Participants rated how much it bothered them to use assistance on a 5-point scale from not at all to extremely for walking, hearing, and memory problems. Participants who felt that they did not need assistance skipped these questions, thus analyses were performed only on participants who indicated needing assistance for walking (n = 57), hearing (n = 69), and memory problems (n = 72).
Public concealment
Participants rated how often they tried to hide that they needed assistance using a 5 point scale from almost never to almost always for walking, hearing, and memory problems. Participants who did not need assistance opted out of the question, so the analyses were performed only on participants who indicated needing assistance for walking (n = 55), hearing (n = 71), and memory problems (n = 72).
Mental status
Participants completed the Short Portable Mental Status Questionnaire (Pfeiffer, 1975) to assess level of cognitive functioning and eliminate participants who may suffer from dementia. Questions assess general knowledge of current events such as “Who is the current President of the U.S.?” as well as understanding of time and place such as “What is the date today?” If a participant responded incorrectly to four or more of the 10 questions, his or her data were eliminated from the analyses.
Results
General Well-Being
Correlations among all variables examined are presented in Table 3. As can be seen, self-compassion was positively correlated with aging successfully, and negatively correlated with depression and impairment. These correlations are consistent with the results of previous research and Study 1 in showing that self-compassion is associated with higher well-being.
Use of Assistive Devices and Memory Tactics
Self-compassion was not correlated with participants’ ratings of the difficulty they have walking, hearing, or remembering. As in Study 1, hierarchical multiple regression analyses were used to examine the effects of self-compassion, ratings of difficulty in a particular domain (walking, hearing, remembering), and their interactions on participants’ willingness to use assistance for these problems and their efforts to hide their need for assistance from other people. As before, predictors were zero-centered and interaction terms were created using the zero-centered items (Tables 4–6). Once again, the J-N technique was used to decompose significant interactions as described earlier.
Table 4.
Study 2: Hierarchical Multiple Regression Analyses Predicting Use of Assistance from Self-compassion and Walking Difficulty
| Walking Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Predictor | Use a Walker | Another Person | Embarrassment | Public Concealment | ||||
|
| ||||||||
| ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1 | .43*** | .40*** | .39*** | .20** | ||||
| SC | .11 | −.07 | −.26** | −.18 | ||||
| WD | .65*** | .63*** | .55*** | .39** | ||||
| Step 2 | .05** | .04* | .00 | .01 | ||||
| SC x WD | .24** | −.20* | .01 | .11 | ||||
| Total R2 | .48*** | .44*** | .39*** | .21*** | ||||
| n | 70 | 69 | 55 | 53 | ||||
Note.
p < .05.
p < .01.
p <.001.
Table 6.
Study 2: Hierarchical Multiple Regression Analyses Predicting Use of Assistance from Self-compassion and Memory Difficulty
| Memory Outcomes | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Predictor | Use of Memory Tricks and Strategies | Embarrassment | Public Concealment | |||
|
| ||||||
| ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1 | .06 | .23*** | .14** | |||
| SC | .21 | −.06 | −.20 | |||
| MD | .15 | .47*** | .30** | |||
| Step 2 | .08* | .00 | .00 | |||
| SC x MD | −.28* | −.09 | −.09 | |||
| Total R2 | .14* | .23*** | .14** | |||
| n | 71 | 71 | 71 | |||
Note.
p < .05.
p < .01.
p <.001.
Mobility
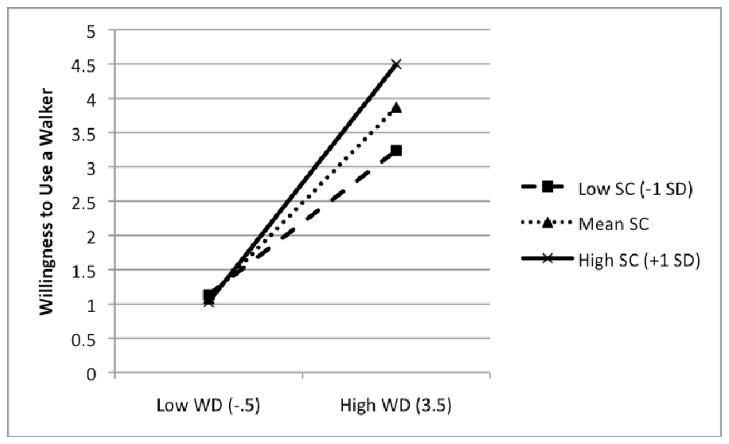
Separate analyses were conducted to predict people’s willingness to use a walker and another person as a function of self-compassion, self-reported difficulty with walking, and their interaction. (We had planned to examine willingness to use a wheelchair, but the number of participants who used a wheelchair [n = 4] was too low to yield valid conclusions.) A significant main effect for rated difficulty walking on willingness to use both a walker and another person showed, not surprisingly, that the more difficulty people have walking, the more likely they are to use a walker (t (68) = 7.08, p <.001, β = .65) and another person (t (67) = 6.69, p <.001, β = .63).
These main effects were qualified by significant interactions. A significant interaction between self-compassion and difficulty walking was obtained on the willingness to use a walker (t (67) = 2.59, p =.012, β = .23). The interaction was interpreted using the J-N procedure to determine the level of self-compassion at which walking difficulty predicts willingness to use a walker. Also, the focal predictor (walking difficulty) and moderator (self-compassion) were switched to show the level of walking difficulty at which self-compassion significantly moderates willingness to use a walker. When self-compassion was 2.24 SD below the mean or less, walking difficulty significantly predicted less willingness to use a walker. When participants had little difficulty walking, self-compassion was unrelated to participants’ willingness to use a walker. However, among participants whose ratings of walking difficulty were more than 1.1 SD above the mean, participants who were higher in self-compassion were more likely to use a walker than those who were lower in self-compassion (see Figure 5).
Figure 5.
Study 2: Interaction of self-compassion and walking difficulty on willingness to use a walker.
Note. Graph shows moderating effects of self-compassion on the relationship between reported walking difficulty and willingness to use a walker. Values on the x-axis are the lowest and highest standardized observed values for reported walking difficulty.
A significant interaction between self-compassion and difficulty walking was also obtained on willingness to use another person for physical support (t (66) = −2.09, p =.041, β = −.19). When self-compassion was 2.14 SD above the mean or higher, walking difficulty significantly predicted willingness to use another person for support. When participants had little difficulty walking, self-compassion was unrelated to participants’ willingness to use another person for support. However, contrary to expectations, when participants had trouble walking (difficulty ratings greater than 1.2 SD above the mean), participants who were lower in self-compassion were more likely to use another person for support than participants who were higher in self-compassion.
Participants were asked two questions assessing how much it bothered them to use assistance and whether they tried to hide the fact that they needed assistance from other people. (Participants who reported that they did not need assistance to walk were eliminated from this analysis.) Among participants who needed help walking, difficulty walking predicted both how much needing assistance bothered the individuals (t (53) = 5.08, p <.001, β = .55) and how much they tried to hide their need for assistance (t (51) = 3.13, p =.003, β = .39). More importantly, self-compassion was negatively related to how much it bothered people to use assistance walking (t (53) = −2.46, p =.017, β = −.26).
Hearing
Hierarchical multiple regression analysis was used to predict people’s willingness to ask others to repeat themselves as a function of self-compassion, self-reported hearing acuity, and their interaction. Self-compassion significantly predicted how often participants asked others to repeat themselves, t (69) = −2.22, p =.030, β = −.20). Hierarchical regression analyses were also performed on willingness to use a hearing aid, but no significant effects were obtained. Additionally, self-compassion did not predict how much using a hearing aid bothered participants or participants’ attempts to hide the fact they had trouble hearing.
Memory
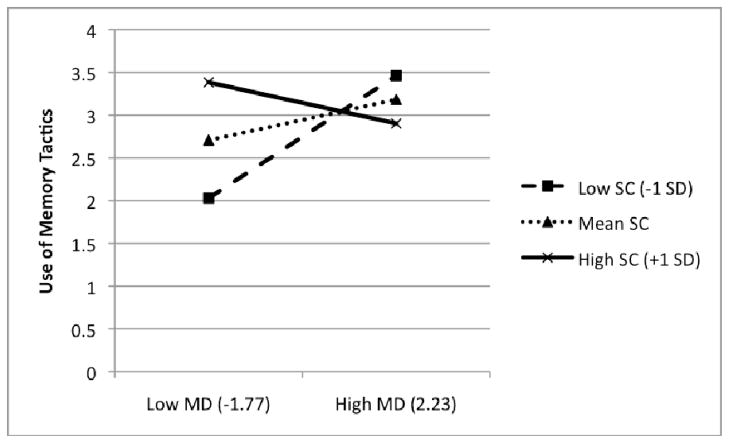
A significant interaction of self-compassion and difficulty remembering people’s names was obtained on the frequency with which participants used “tricks” to help them remember (t (68) = −2.44, p =.018, β = −.27). Memory difficulty significantly predicted willingness to use “tricks” for participants with self-compassion scores that were .42 SD below the mean or higher. Reframed, when memory difficulty was less than .34 SD above the mean, participants who were higher in self-compassion were more likely to report using tricks and strategies to help them remember than participants lower in self-compassion (see Figure 6).
Figure 6.
Study 2: Interaction of self-compassion and memory difficulty on use of tactics to help memory
Note. Graph shows moderating effects of self-compassion on the relationship between reported memory difficulty and use of tactics to help memory. Values on the x-axis are the lowest and highest standardized observed values for reported memory difficulty.
Discussion
Although many people use assistive devices to walk or hear as they age, such devices are sometimes stigmatizing because they can draw attention to one’s deficits and make one “look old” (Martin, Leary, & Rejeski, 2000). However, people who need assistance but refuse to use it may be at risk for falling, broken hips, and further loss of independence. We had expected that people who are higher in self-compassion would be more willing to use assistance due to their lower defensiveness about their personal limitations, their ability to deal with such limitations with greater equanimity, and their desire to promote their own well-being (Neff et al., 2005; Neff et al., 2007b). After all, a compassionate person would encourage an older friend to use such assistance when it was needed, and we expected that self-compassionate older people would do the same for themselves.
The results partially supported this hypothesis. Participants scoring higher in self-compassion were more willing to ask people to repeat themselves when they could not hear what others said, and among people who had difficulty walking, those who were higher in self-compassion were more willing to use a walker. These results support the notion that self-compassionate people are more accepting of their physical limitations and more willing to take steps to maintain their well-being (Neff, 2003a; Neff et al., 2007b; Leary et al., 2007).
Self-compassion also moderated the relationship between memory difficulty and use of mnemonic tricks and strategies. For participants who reported having fewer problems with their memory, higher self-compassion was related to greater use of tactics to help them remember. The direction of this effect was unexpected in that self-compassion was related to the use of such tactics among people who had fewer memory problems. One possible explanation is that when people begin to have difficulty remembering things, self-compassionate people are motivated to slow the process of memory decline and thus more likely to utilize mnemonic tactics. For participants high in self-compassion, memory difficulty was irrelevant in the use of memory tricks and strategies whereas for those who were lower in self-compassion, less memory difficulty was associated with lower use of tricks and strategies. Research has shown that self-compassion is associated with taking personal initiative and the desire to maintain a fulfilling life (Neff et al., 2007b), and efforts to improve one’s memory may help to maintain neural plasticity and slow memory decline (Erickson et al., 2007; Valenzuela & Sachdev, 2006).
One finding was notably inconsistent with predictions. Among people who had trouble walking, those who were high in self-compassion were less willing than people low in self-compassion to use another person for mobility. This finding is particularly puzzling given that, as predicted, high self-compassion was associated with greater willingness to use a walker. Perhaps using a walker for support has a different symbolic or social meaning than using a person, which connotes dependence on other people. Although self-compassionate people treat themselves kindly and take initiative to improve their lives (Leary et al., 2007; Neff et al., 2005; Neff et al., 2007a; Neff et al., 2007b), no research has directly examined whether self-compassion is related to a willingness to rely on other people to deal with negative events. The fact that self-compassionate participants were less willing to use other people to walk suggests that people who are high in self-compassion may rely less on other people for help with their problems (or at least desire to rely less on others). Highly self-compassionate individuals may also behave more autonomously, leading them to rely on their own abilities in difficult situations. Research is needed to examine this possibility as well as to investigate how older people who are low versus high in self-compassion construe different kinds of physical assistance.
One finding supported the prediction that older people who are higher in self-compassion are less bothered by using assistance than people who are low in self-compassion. Participants who scored higher in self-compassion reported being less bothered by needing assistance to walk than those low in self-compassion, possibly because they accept their limitations and see their difficulties as part of normal human experience rather than as unique and isolating (Neff, 2003a; Neff et al., 2007a; Leary et al., 2007). However, self-compassion was not related to the degree to which people wanted to hide their problems from others.
General Discussion
Overall, self-compassion moderated the relationship between physical health and subjective well-being among older adults in ways that were consistent with the conceptualization of self-compassion and with previous research. Self-compassion was broadly associated with positive outcomes, and, as predicted, self-compassion appeared to be particularly beneficial for people who reported poorer physical health. Adopting a self-compassionate mindset allows people to cope with myriad difficulties and stressors by treating themselves with care and kindness, viewing their circumstances as part of the greater human experience, and not allowing themselves to be carried away by strong emotions (Neff, 2003a).
Because self-compassionate older adults promote their own well-being and cope better with negative health outcomes, we hypothesized that they might engage in behaviors that lower the likelihood that they will experience those negative outcomes in the first place. We examined using assistance as a behavior that might differentiate how low and high self-compassionate people deal with certain age-related changes. The findings were mixed. High self-compassion was associated with greater willingness to use a walker, asking others to repeat themselves, and using memory tricks, but lower willingness to use other people for physical support while walking. Research is needed to understand the kinds of help that self-compassionate people are and are not likely to seek. The results did show, however, that older adults who were high in self-compassion were less bothered by the use of assistance than those who were low in self-compassion. This finding is consistent with research showing that self-compassionate people react less strongly to failure and embarrassing situations (Leary et al., 2007).
These studies are the first to address self-compassion in an older population. Given the physical and mental difficulties that accompany aging, the benefits of self-compassion should be magnified among older people. Although other variables, such as self-acceptance and mindfulness, may also be important variables during this phase of life, self-compassion involves a personal concern for one’s well-being that should perpetuate kind self-directed behaviors. Importantly, the Self-compassion Scale (both the original measure and our 12-item adaptation) performed reasonably well, providing evidence that the measure is reliable and valid among older participants. More importantly, we found that the average self-compassion score for older adults is approximately .7 points higher than the college student population. Although this comparison is purely cross-sectional, self-compassion may increase over the lifespan as people become more experienced in dealing with life’s challenges. Future studies addressing the longitudinal nature of this relationship would be a valuable addition to the literature.
These findings showed a consistent link between self-compassion and well-being in older age, but additional research is needed to understand fully the processes by which a self-compassionate mindset promotes adjustment. Part of the answer probably lies in how self-compassionate people cope with stressful events (Allen & Leary, 2010), but as noted, self-compassion may also relate to how well people take care of themselves. We did not find clear support for a link between self-compassion and proactive self-care, but our studies examined only a narrow range of proactive, preventative behaviors. Future research should examine possible differences in how self-compassion relates to self-care over a broader array of domains and behaviors. For example, preliminary findings suggest that people who are higher in self-compassion are more likely to take care of their health, seek medical attention when needed, and follow their doctors’ orders (Terry & Leary, in press).
Although this research focused on individual differences in self-compassion, other studies have shown that inducing a self-compassionate mindset also leads to more positive emotional, cognitive, and behavioral responses (Adams & Leary, 2007; Leary et al, 2007). Additionally, two longer interventions have focused on teaching people how to incorporate self-compassion skills into their daily lives. Gilbert and Proctor (2006) developed a compassionate mind training intervention for participants who were high in shame and self-criticism, and Germer and Neff are developing an 8-week program to teach self-compassion skills (Neff, personal communication). Given the link between self-compassion and well-being in older ages, researchers should consider developing a self-compassion intervention that focuses on promoting a compassionate response to the aging process.
These studies are the first to examine the role of self-compassion in the lives of older adults. Additional work is needed to extend these findings and address certain limitations. First, all measures of health and functioning were based on self-reports completed in participants’ homes, which prevented any control over the time that participants spent on the study or the conditions under which it was completed. Furthermore, because we relied solely on self-reports, future work may wish to collect more objective indicators of health and well-being. For our purposes, participants’ perceptions of their health and well-being were of interest because people’s reactions to health problems are based on how they construe them. Even so, it is of interest to know how actual illness and disability are related to these processes. In addition, our samples consisted primarily of well-functioning older individuals and did not include many participants who had severe medical or psychological problems. Our findings suggest that self-compassion might be even more important for people with very serious illnesses and disabilities, but that hypothesis will require more diverse samples of older adults.
Despite these limitations, these studies show clearly that self-compassion is related to well-being among older adults, especially for those who report more physical problems. Additionally, they suggest that self-compassion may play a role in older people’s use of assistance, which has implications for preventive care in older adults. Furthermore, these findings suggest that interventions that promote self-compassion might enhance well-being in the elderly, particularly among older people who are self-critical or despondent with respect to their changing health, abilities, or life circumstances.
Table 5.
Study 2: Hierarchical Multiple Regression Analyses Predicting Use of Assistance from Self-compassion and Hearing Difficulty
| Hearing Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Predictor | Ask Others to Repeat Themselves | Use of a Hearing Aid | Embarrassment | Public Concealment | ||||
|
| ||||||||
| ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1 | .46*** | .70*** | .64*** | .41** | ||||
| SC | −.20* | −.03 | .02 | −.14 | ||||
| HD | .67*** | .84*** | .80*** | .64*** | ||||
| Step 2 | .01 | .00 | .00 | .03 | ||||
| SC x HD | −.08 | −.01 | .07 | .18 | ||||
| Total R2 | .47*** | .70*** | .64*** | .44*** | ||||
| n | 71 | 56 | 71 | 68 | ||||
Note.
p < .05.
p < .01.
p <.001.
Acknowledgments
Ashley Batts Allen was supported by the National Institute on Aging NRSA award AG034716.
Contributor Information
Ashley Batts Allen, Department of Psychology and Neuroscience, Duke University.
Eleanor R. Goldwasser, Penn State College of Medicine
Mark R. Leary, Department of Psychology and Neuroscience, Duke University
References
- Adams CE, Leary MR. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. Journal of Social and Clinical Psychology. 2007;26:1120–1144. [Google Scholar]
- Adelmann PK. Multiple roles and psychological well-being in a national sample of older adults. Journal of Gerontology. 1994;49:277–285. doi: 10.1093/geronj/49.6.s277. [DOI] [PubMed] [Google Scholar]
- Allen AB, Leary MR. Self-compassion, stress, and coping. Social and Personality Psychology Compass. 2010;4:107–118. doi: 10.1111/j.1751-9004.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailis DS, Chipperfield JG. Compensating for losses in perceived personal control over health: A role for collective self-esteem in healthy aging. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2002;57:531–539. doi: 10.1093/geronb/57.6.p531. [DOI] [PubMed] [Google Scholar]
- Baltes PB, Baltes MM. Successful aging: Perspectives from the behavioral sciences. New York: Cambridge University Press; 1990. Psychological perspectives on successful aging: The model of selective optimization with compensation. In P. B. Baltes & M. M. Baltes (Eds.) pp. 1–34. [Google Scholar]
- Baltes PB, Staudinger UM, Lindenberger U. Lifespan psychology: Theory and application to intellectual functioning. Annual Review of Psychology. 1999;50:471–507. doi: 10.1146/annurev.psych.50.1.471. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W H Freeman/Times Books/Henry Holt & Co; 1997. [Google Scholar]
- Brandtstadter J, Greve W. The aging self: Stabilizing and protective processes. Developmental Review. 1994;14:52–80. doi: 10.1006/drev.1994.1003. [DOI] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. British Medical Journal. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54:165–181. doi: 10.1037/0003-066X.54.3.165. [DOI] [PubMed] [Google Scholar]
- Cheng S-T. Age and subjective well-being revisited: A discrepancy perspective. Psychology and Aging. 2004;19:409–415. doi: 10.1037/0882-7974.19.3.409. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Dupuy HJ. The Psychological General Well-Being (PGWB) Index. In: Wenger NK, Mattson ME, Furberg CD, Elinson J, editors. Assessment of quality of life in clinical trials of cardiovascular therapies. New York: Le Jacq Publishing; 1984. pp. 170–183. [DOI] [PubMed] [Google Scholar]
- Erickson KI, Colcombe SJ, Wadhwa R, Bherer L, Peterson MS, Scalf PE, et al. Training-induced plasticity in older adults: Effects of training on hemispheric asymmetry. Neurobiology of Aging. 2007;28:272–283. doi: 10.1016/j.neurobiolaging.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Erikson EH. Identity: youth and crisis. Oxford England: Norton & Co; 1968. [Google Scholar]
- Fagerstrom C, Borg C, Balducci C, Burholt V, Wenger CG, Ferring D, et al. Life satisfaction and associated factors among people aged 60 years and above in six European countries. Applied Research in Quality of Life. 2007;2:33–50. doi: 10.1007/s11482-007-9028-0. [DOI] [Google Scholar]
- Ferguson SJ, Goodwin AD. Optimism and well-being in older adults: The mediating role of social support and perceived control. The International Journal of Aging and Human Development. 2010;71:43–68. doi: 10.2190/AG.71.1.c. [DOI] [PubMed] [Google Scholar]
- George LK. Perceived Quality of Life. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. 6. Amsterdam Netherlands: Elsevier; 2006. pp. 320–336. [DOI] [Google Scholar]
- Gilbert P, Procter S. Compassionate Mind Training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology and Psychotherapy. 2006;13:353–379. doi: 10.1002/cpp.507. [DOI] [Google Scholar]
- Glass TA, Mendes de Leon C, Marottoli RA, Berkman LF. Population based study of social and productive activities as predictors of survival among elderly Americans. British Medical Journal. 1999;319:478–483. doi: 10.1136/bmj.319.7208.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlow RE, Cantor N. Still participating after all these years: A study of life task participation in later life. Journal of Personality and Social Psychology. 1996;71:1235–1249. doi: 10.1037/0022-3514.71.6.1235. [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Little TD, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychology and Aging. 2000;15:511–526. doi: 10.1037/0882-7974.15.3.511. [DOI] [PubMed] [Google Scholar]
- Kurlowicz L, Greenberg SA. The Geriatric Depression Scale. The Hartford Institute for Geriatric Nursing, New York University College of Nursing; 2007. [Google Scholar]
- Lawton MP. The Philadelphia Geriatric Center Morale Scale: A revision. Journal of Gerontology. 1975;30:85–89. doi: 10.1093/geronj/30.1.85. [DOI] [PubMed] [Google Scholar]
- Leary MR, Tate EB, Adams CE, Batts Allen A, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology. 2007;92:887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Lee DJ, Markides KS. Activity and mortality among aged persons over an eight-year period. Journals of Gerontology. 1990;45:39–42. doi: 10.1093/geronj/45.1.s39. [DOI] [PubMed] [Google Scholar]
- Liang J, Bollen KA. The structure of the Philadelphia Geriatric Center Morale Scale: A reinterpretation. Journal of Gerontology. 1983;38:181–189. doi: 10.1093/geronj/38.2.181. [DOI] [PubMed] [Google Scholar]
- Manton KG. Mortality and morbidity. In: Binstock RH, George KL, editors. Handbook of aging and social sciences. 3. San Diego, CA: Academic Press; 1990. pp. 64–89. [Google Scholar]
- Martin KA, Leary MR, Rejeski WJ. Self-presentational concerns in older adults: Implications for health and well-being. Basic and Applied Social Psychology. 2000;22:169–179. [Google Scholar]
- Mirowsky J, Ross CE. Age and depression. Journal of Health and Social Behavior. 1992;33:187–205. doi: 10.2307/2137349. [DOI] [PubMed] [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity. 2003a;2:223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003b;2:85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- Neff KD, Hsieh Y-P, Dejitterat K. Self-compassion, achievement goals, and coping with academic failure. Self and Identity. 2005;4:263–287. doi: 10.1080/13576500444000317. [DOI] [Google Scholar]
- Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. Journal of Research in Personality. 2007a;41:139–154. doi: 10.1016/j.jrp.2006.03.004. [DOI] [Google Scholar]
- Neff KD, Rude SS, Kirkpatrick KL. An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality. 2007b;41:908–916. doi: 10.1016/j.jrp.2006.08.002. [DOI] [Google Scholar]
- Neff KD, Vonk R. Self-compassion versus global self-esteem: Two different ways of relating to oneself. Journal of Personality. 2009;77:23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of American Geriatrics Society. 1975;23:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Potthoff RF. On the Johnson-Neyman technique and some extensions thereof. Psychometrika. 1964;29:241–256. doi: 10.1007/BF02289721. [DOI] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy. doi: 10.3102/10769986031004437. in press. [DOI] [PubMed] [Google Scholar]
- Ranzijn R, Keeves J, Luszcz M, Feather NT. The role of self-perceived usefulness and competence in the self-esteem of elderly adults: Confirmatory factor analyses of the Bachman revision of Rosenberg’s Self-Esteem Scale. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1998;53:96–104. doi: 10.1093/geronb/53b.2.p96. [DOI] [PubMed] [Google Scholar]
- Robins RW, Trzesniewski KH, Tracy JL, Gosling SD, Potter J. Global self-esteem across the life span. Psychology and Aging. 2002;17:423–434. doi: 10.1037/0882-7974.17.3.423. [DOI] [PubMed] [Google Scholar]
- Rodin J, Timko C, Harris S. The construct of control: Biological and psychological correlates. In: Eisdorfer C, Lawton MP, Maddox GL, editors. Annual review of gerontology and geriatrics. Vol. 5. New York: Springer; 1985. pp. 3–55. [PubMed] [Google Scholar]
- Rosenberg M. Measurement of self-esteem. In: Rosenberg M, editor. Society and the adolescent self image. New York: Princeton University Press; 1965. pp. 297–307. [Google Scholar]
- Schulz R, Heckhausen J. Aging, culture and control: Setting a new research agenda. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1999:139–145. doi: 10.1093/geronb/54b.3.p139. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur Studies of Successful Aging. Health Psychology. 2001;20:243–255. doi: 10.1037//0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- Singer T, Verhaeghen P, Ghisletta P, Lindenberger U, Baltes PB. The fate of cognition in very old age: Six-year longitudinal findings in the Berlin Aging Study (BASE) Psychology and Aging. 2003;18:318–331. doi: 10.1037/0882-7974.18.2.318. [DOI] [PubMed] [Google Scholar]
- Skinner EA. A guide to constructs of control. Journal of Personality and Social Psychology. 1996;71:549–570. doi: 10.1037/0022-3514.71.3.549. [DOI] [PubMed] [Google Scholar]
- Sneed JR, Krauss Whitbourne S. Identity processing styles and the need for self-esteem in middle-aged and older adults. International Journal of Aging & Human Development. 2001;52:311–321. doi: 10.2190/A9M0-TRR6-PVEQ-05ND. [DOI] [PubMed] [Google Scholar]
- Terry ML, Leary ML. Self-compassion, self-regulation, and health. Self and Identity (in press) [Google Scholar]
- Valenzuela MJ, Sachdev P. Cognitive leisure activities, but not watching TV, for future brain benefits. Neurology. 2006;67:729–729. doi: 10.1212/01.wnl.0000239615.49557.63. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- Young FW, Glasglow N. Voluntary social participation and health. Research on Aging. 1998;20:339–363. doi: 10.1177/0164027598203004. [DOI] [Google Scholar]