Abstract
Problem
In Malaysia, human immunodeficiency virus (HIV) infection is highly concentrated among people who inject opioids. For this reason, the country undertook a three-phase roll-out of a methadone maintenance treatment (MMT) programme. In Phase 3, described in this paper, MMT was implemented within prisons and retention in care was assessed.
Approach
After developing standard operating procedures and agreement between its Prisons Department and Ministry of Health, Malaysia established pilot MMT programmes in two prisons in the states of Kelantan (2008) and Selangor (2009) – those with the highest proportions of HIV-infected prisoners. Community-based MMT programmes were also established in Malaysia to integrate treatment activities after prisoners’ release.
Local setting
Having failed to reduce the incidence of HIV infection, in 2005 Malaysia embarked on a harm reduction strategy.
Relevant changes
Standard operating procedures were modified to: (i) escalate the dose of methadone more slowly; (ii) provide ongoing education and training for medical and correctional staff and inmates; (iii) increase the duration of methadone treatment before releasing prisoners; (iv) reinforce linkages with community MMT programmes after prisoners’ release; (v) screen for and treat tuberculosis; (vi) escalate the dose of methadone during treatment for HIV infection and tuberculosis; and (vii) optimize the daily oral dose of methadone (> 80 mg) before releasing prisoners.
Lessons learnt
Prison-based MMT programmes can be effectively implemented but require adequate dosing and measures are needed to improve communication between prison and police authorities, prevent police harassment of MMT clients after their release, and improve systems for tracking release dates.
Résumé
Problème
En Malaisie, l’infection par le virus de l'immunodéficience humaine (VIH) est fortement présente chez les personnes qui s'injectent des opioïdes. Pour cette raison, le pays a entrepris la mise en place en trois phases d'un programme de traitement de maintien à la méthadone (TMM). Dans la phase 3, décrite dans ce document de travail, le TMM a été mis en place au sein des prisons, et on a évalué la rétention dans les soins.
Approche
Après avoir élaboré des modes opératoires normalisés et obtenu un accord entre son administration pénitentiaire et son ministère de la Santé, la Malaisie a mis au point des programmes de TMM pilotes dans deux prisons des États de Kelantan (2008) et de Selangor (2009), là où les proportions de détenus infectés par le VIH sont les plus fortes. Des programmes de TMM communautaires ont également été créés en Malaisie pour intégrer des activités de maintien après la libération de prisonniers.
Environnement local
N'ayant pas réussi à réduire l'incidence de l'infection par le VIH, la Malaisie a lancé en 2005 une stratégie de réduction des risques.
Changements pertinents
Les modes opératoires normalisés ont été modifiés pour: (i) augmenter plus lentement la dose de méthadone, (ii) offrir en permanence des informations et une formation au personnel médical et pénitentiaire et aux détenus, (iii) allonger la durée du traitement à la méthadone avant de libérer les prisonniers, (iv) renforcer les liens avec les programmes de TMM communautaires après la libération de prisonniers, (v) dépister et traiter la tuberculose, (vi) augmenter la dose de méthadone pendant le traitement contre l'infection par le VIH et la tuberculose, et (vii) optimiser la dose orale quotidienne de méthadone (> 80 mg) avant de libérer les prisonniers.
Leçons tirées
Les programmes de TMM en milieu carcéral peuvent être efficacement mis en œuvre, mais ils nécessitent un dosage adéquat et des mesures sont nécessaires pour améliorer la communication entre les autorités pénitentiaires et policières, pour éviter les tracasseries policières des patients suivant un TMM après leur libération et pour optimiser les systèmes de suivi des dates de libération.
Resumen
Situación
En Malasia, la infección por el virus de la inmunodeficiencia humana (VIH) se concentra principalmente entre las personas que se inyectan opiáceos. Por este motivo, el país ha comenzado a introducir un programa de tres fases para el tratamiento de mantenimiento con metadona (TMM). En la tercera fase, descrita en este artículo, se aplicó el TMM en prisiones y se evaluó la atención ininterrumpida a los pacientes.
Enfoque
Tras desarrollar unos procedimientos operativos estándar y un acuerdo con el departamento de prisiones y el Ministerio de sanidad, Malasia estableció programas piloto de TMM en dos prisiones en los estados de Kelantan (2008) y Selangor (2009), en las que se dan las proporciones más altas de presos seropositivos. También se establecieron programas TMM de base comunitaria con objeto de integrar las actividades terapéuticas tras la puesta en libertad de los presos.
Marco regional
Tras fracasar el intento de reducir la incidencia de la infección por el VIH, Malasia se embarcó en el año 2005 en una estrategia de reducción de daños.
Cambios importantes
Se modificaron los procedimientos operativos estándar para: (i) aumentar la dosis de metadona más lentamente; (ii) proporcionar educación continua y formación para el personal médico y del correccional, así como para los reclusos; (iii) aumentar la duración del tratamiento con metadona antes de la puesta en libertad de los presos; (iv) reforzar los vínculos con los programas TMM de base comunitaria tras la puesta en libertad de los presos; (v) diagnosticar y tratar la tuberculosis; (vi) aumentar la dosis de metadona durante el tratamiento contra la infección por VIH y la tuberculosis; y (vii) optimizar la dosis oral diaria de metadona (> 80 mg) antes de poner en libertad a los presos.
Lecciones aprendidas
Es posible aplicar programas de TMM con base en las prisiones eficazmente, pero se requiere una dosificación adecuada y la adopción de medidas para mejorar la comunicación entre las autoridades policiales y de prisiones, prevenir el acoso policial a los usuarios de TMM tras su puesta en libertad y mejorar los sistemas de seguimiento de las fechas de liberación.
ملخص
المشكلة
يتركز فيروس العوز المناعي البشري (HIV) في ماليزيا بشدة بين الأشخاص الذين يتعاطون المواد الأفيونية المفعول عن طريق الحقن. ولهذا السبب، نفذ البلد عملية نشر تتكون من ثلاث مراحل لبرنامج العلاج الصياني بالميثادون (MMT). وفي المرحلة الثالثة، الوارد وصفها في هذه الورقة، تم تنفيذ العلاج الصياني بالميثادون داخل السجون وتم تقييم الاستبقاء في الرعاية.
الأسلوب
أنشأت ماليزيا بعد وضع إجراءات التشغيل المعيارية والاتفاق بين إدارة السجون ووزارة الصحة بها برامج رائدة للعلاج الصياني بالميثادون في سجنين في ولاياتي كيلانتان (2008) وسيلانغور (2009) – اللتين تضمان أعلى نسب للسجناء المصابين بعدوى فيروس العوز المناعي البشري. وتم أيضاً وضع برامج مجتمعية للعلاج الصياني بالميثادون في ماليزيا لدمج أنشطة العلاج بعد الإفراج عن السجناء.
المواقع المحلية
بعد الفشل في خفض الإصابة بعدوى فيروس العوز المناعي البشري، شرعت ماليزيا في عام 2005 في تنفيذ استراتيجية للحد من الأضرار.
التغيّرات ذات الصلة
تم تعديل إجراءات التشغيل المعيارية للأغراض التالية: (1) زيادة جرعة الميثادون على نحو أكثر بطئاً؛ (2) توفير التثقيف والتدريب المستمرين للعاملين في المجال الطبي والإصلاحي والنزلاء؛ (3) زيادة مدة العلاج بالميثادون قبل الإفراج عن السجناء؛ (4) تعزيز الربط بين البرامج المجتمعية للعلاج الصياني بالميثادون بعد الإفراج عن السجناء؛ (5) تحري السل وعلاجه؛ (6) زيادة جرعة الميثادون أثناء علاج عدوى فيروس العوز المناعي البشري والسل؛ (7) رفع آثار الجرعة الفموية اليومية من الميثادون (> 80 مليغرام) إلى أقصى حد ممكن قبل الإفراج عن السجناء.
الدروس المستفادة
يمكن تنفيذ برامج العلاج الصياني بالميثادون داخل السجون على نحو فعّال ولكنها تتطلب جرعات كافية ولابد من اتخاذ إجراءات لتحسين الاتصال بين سلطات السجون والشرطة ومنع مضايقة الشرطة للمترددين على العلاج الصياني بالميثادون بعد الإفراج عنهم وتحسين نظم تتبع تواريخ الإفراج.
摘要
问题
在马来西亚,艾滋病毒(HIV)感染高度集中于注射阿片类药物的人群中。因此,国家开展分三阶段推出的美沙酮维持治疗(MMT)计划。在本文所描述的第三阶段中,MMT治疗在监狱中实施,并对保持治疗率进行评估。
方法
在制定监狱部门和卫生部之间的标准操作程序以及协议之后,马来西亚在吉兰丹(2008)和雪兰莪州(2009)的两个监狱中建立试点MMT项目——这两个监狱的囚犯的HIV感染比例最高。在马来西亚也建立以社区为基础的MMT计划,从而将囚犯释放之后的治疗活动融为一体。
当地状况
因为未能减少艾滋病毒感染的发生率,2005 年马来西亚开始推行减少伤害战略。
相关变化
标准操作程序被修改为:(1)更缓慢地提升美沙酮剂量;(2)为医疗和矫正人员和囚犯提供持续的教育和培训;(3)在释放囚犯之前,增加美沙酮治疗时间;(4)加强囚犯释放后与社区MMT项目的联系;(5)筛查并治疗结核病;(6)提升在HIV感染和结核病治疗中美沙酮的剂量;(7)在释放囚犯之前,最优化美沙酮日常口服剂量(> 80毫克)。
经验教训
基于监狱的MMT计划可以有效地实施,但需要足够的剂量和措施,以此改善监狱和警察当局之间的沟通,防止警察骚扰释放之后的MMT救济对象,改善跟踪释放日期的系统。
Резюме
Проблема
В Малайзии инфекция вируса иммунодефицита человека (ВИЧ) наиболее часто встречается среди людей, вводящих внутривенно опиоидные препараты. По этой причине в стране приступили к трехэтапному развертыванию программы по метадоновой поддерживающей терапии (МПТ). На третьем этапе, описанном в настоящей статье, МПТ проводилась в тюрьмах и оценивалось удержание в программе лечения.
Подход
После составления программы мероприятий и согласования между Департаментом по исполнению наказаний и Министерством здравоохранения в Малайзии утвердили пилотные программы по МПТ в двух тюрьмах в штатах Келантан (2008 г) и Селангор (2009 г), на которые приходится наибольший процент ВИЧ-инфицированных заключенных. В Малайзии были также утверждены территориальные программы по МПТ в целях интеграции лечебной деятельности после освобождения заключенных.
Местные условия
Не добившись сокращения заболеваемости ВИЧ-инфекцией, в 2005 г. в Малайзии приступили к реализации стратегии по снижению вреда.
Осуществленные перемены
В программу мероприятий были внесены изменения с целью: (i) более медленного повышения дозы метадона; (ii) постоянного обучения и подготовки медицинского персонала и служащих исправительных учреждений, а также лиц, содержащихся под стражей; (iii) увеличения продолжительности метадоновой терапии до освобождения заключенных; (iv) укрепления связей с территориальными программами по МПТ после освобождения заключенных; (v) выявления и лечения туберкулеза; (vi) повышения дозы метадона во время лечения ВИЧ-инфекций и туберкулеза; и (vii) оптимизации ежедневной пероральной дозы метадона (> 80 мг) до освобождения заключенных.
Выводы
Тюремные программы по МПТ могут реализовываться эффективно, однако требуют соответствующего дозирования. Также необходимы меры по улучшению взаимодействия между администрацией исправительных учреждений и правоохранительными органами, меры по предотвращению притеснения со стороны правоохранительных органов пациентов МПТ после их освобождения и меры по улучшению системы отслеживания дней, когда заключенные освобождаются из заключения.
Introduction
In 2005, Malaysia, a middle-income country, was in the throes of one of south-eastern Asia’s most explosive epidemics of human immunodeficiency virus (HIV) infection. The epidemic was largely concentrated among people who inject drugs, especially opioids, who comprised more than 1.3% of the population between the ages of 15 and 64 years. Nearly half of all new HIV infections in Malaysia occur among people who inject opioids. In light of this and of the lack of progress towards achieving the Millennium Development Goal of reducing the rate of HIV infection, Malaysia introduced needle and syringe exchange programmes and methadone maintenance treatment (MMT) programmes in 2005 as part of a harm reduction strategy targeting people who inject opioids.1
MMT, an evidence-based therapy for opioid dependence, has been associated with numerous benefits. In addition to reducing opioid use, it lowers risky practices, HIV transmission and criminal behaviour.2 Within prisons, MMT has been shown to dramatically reduce deaths from drug overdose,3 which is the leading direct cause of death over the two weeks that immediately follow release from prison.4 Despite this evidence of their benefits in the community5,6 and in criminal justice settings,7–11 MMT programmes have expanded very slowly and continue to have low coverage. In this report we describe how Malaysia initiated MMT within two prisons and examine the obstacles that hampered implementation and retention in care after prisoners’ release. Such lessons may be useful in other settings where plans to establish harm reduction programmes for HIV-infected individuals who inject opioids are under way.
Setting and approach
In Malaysia, which has a population of 28.3 million, an estimated 205 000 people inject illicit drugs and 78 419 people have HIV infection. The country has approximately 43 000 prisoners and an incarceration rate of 174 per 100 000. Testing of prisoners for HIV is mandatory; about 6% of them test positive.12
Malaysia’s initial experience with the implementation of needle and syringe exchange programmes and MMT programmes has been described elsewhere.13,14 The MMT programme was rolled out in three phases. In Phase I, MMT was introduced in specialty clinics for people with drug dependence, and in Phase II it was expanded to primary care settings. In 2006 prison officials including the Director-General of the Malaysian Prisons Department, made a site visit to Iranian prisons to learn more about the use of MMT in an Islamic context. By 2007, Malaysia’s Prisons Department had decided to pilot an MMT programme in an attempt to reduce HIV infection and reincarceration rates. In partnership with the Ministry of Health and leading national and international experts, the department developed standard operating procedures for deployment of MMT in prisons by adapting the operating procedures in place for community-based MMT. The standard operating procedures for prisons called for initiation of MMT from 3 to 6 months before a prisoner’s release, slow escalation of the methadone dose because of the danger of intolerance to opioids, and the establishment of mechanisms for referring patients to community-based MMT after their release from prison. In this paper we present the data from Phase III, which consisted of the rollout of methadone in the two prisons in Malaysia with the highest prevalence of HIV infection among their inmates.
The first pilot MMT study began in Pengkalan Chepa prison, in the state of Kelantan, in 2008. Later the same year the programme was expanded to Kajang prison, in the state of Selangor. Participants in both pilot programmes were observed for 12 months. We first used MMT in prisoners who were HIV-infected to facilitate their medical care after their release. Because prison health programmes in Malaysia were at an early stage of development, the United Nations Office on Drugs and Crime funded intensive training for prison clinicians and correctional staff, as well as for community-based MMT programme providers. Officials from the Prisons Department and physicians prescribing methadone in the prison and community were selected for this training.
For the analysis we divided the factors that stood as deterrents and facilitators to the implementation of these prison-based MMT programmes into three categories: patient-, staff- and institution-level factors. We conducted one-on-one interviews with clients, both in the prison before their release and regularly after their release, to assess their experiences with the programme. Focus groups of 8 prisoners released from Pengkalan Chepa and 11 released from Kajang prison who had remained on MMT were conducted to gather more detailed information about their experiences with methadone treatment. We also spoke with prison physicians prescribing methadone about their experiences throughout the course of the pilot programme.
Patient-level factors
Under the former standard operating procedures, the daily starting dose of 5 mg of methadone was escalated by 5 mg every 3 to 4 days. In Pengkalan Chepa we found that this escalation rate was too rapid; many patients experienced severe nausea, vomiting and somnolence. For this reason, in Kajang we escalated the dose by 5 mg every 7 days rather than every 5, and no patients experienced these symptoms. We had to extend treatment duration to more than 3 months to allow sufficient time to escalate the daily dose of methadone to more than 80 mg before a prisoner’s release. Ongoing training of physicians and patients was required to ensure that escalation of the dose of methadone was individualized in accordance with each patient’s symptoms. We also observed high rates of abstinence syndrome and in several cases had to increase the dose of methadone. This occurred most often in patients who were receiving anti-tuberculosis agents or antiretroviral therapy (ART), both of which can markedly reduce methadone levels.2 About one fourth of the MMT programme participants in both prisons had to be treated for tuberculosis. This was a surprisingly high percentage, although the incidence of tuberculosis is known to be high among HIV-infected prisoners. Patients who were released from prison on a daily methadone dose of more than 80 mg had better treatment retention rates 12 months after release than those who were released on a lower dose (Table 1).15 This finding has also been observed in community-based MMT programmes.16
Table 1. Characteristics of HIV-infected participants in methadone maintenance treatment (MMT) programmes and outcomes observed before and after their release from prison, Kajang and Pengkalan Chepa prisons (Selangor and Kelantan states, respectively), Malaysia, 2008–2009.
| Characteristic | No. (%) of participants |
|
|---|---|---|
| Pengkalan Chepa prison (n = 42) | Kajang prison (n = 30) | |
| Year MMT programme initiateda | 2008 | 2009 |
| Sex | ||
| Male | 42 (100) | 30 (100) |
| Ethnicity | ||
| Malay | 40 (95.2) | 22 (73.3) |
| Indian | 2 (4.8) | 6 (20.0) |
| Chinese | 0 (0) | 2 (6.7) |
| Religion | ||
| Muslim | 40 (95.2) | 22 (73.3) |
| Hindu | 2 (4.8) | 4 (13.3) |
| Christian | 0 (0) | 3 (10.0) |
| Buddhist | 0 (0) | 1 (3.3) |
| Employed full time before incarceration | ||
| Yes | 24 (57.1) | 16 (53.3) |
| No | 38 (36.9) | 13 (43.3) |
| Highest level of education | ||
| Elementary | 11 (26.2) | 5 (16.3) |
| Some secondary | 19 (45.2) | 16 (53.3) |
| Completed secondary or higher | 12 (28.6) | 9 (30.0) |
| Age in years, mean (SD) | 33.7 (6.7) | 37.1 (7.0) |
| Have injected illicit drugs | ||
| Yes | 42 (100) | 29 (96.7) |
| No | 0 (0) | 1 (3.3) |
| Years of incarceration, mean (SD) | 1.2 (0.6) | 1.0 (0.5) |
| Years of incarceration over lifetime, mean (SD) | 5.6 (3.9) | 6.6 (4.2) |
| Years since diagnosis of HIV infection, mean (SD) | 6.1 (5.7) | 8.3 (6.5) |
|
Met criteria for moderate to severe major depressive disorderb |
18 (42.9) |
12 (40.0) |
| Outcome | ||
| Before release | (n = 42) | (n = 30) |
| Discontinued methadone, because: | 12 (28.6) | 3 (10.0) |
| side-effects (nausea, vomiting) | 4 (10.0) | 0 (0) |
| death (from HIV-related causes) | 3 (7.1) | 3 (10.0) |
| transfer to community-based MMT | 2 (4.8) | 0 (0) |
| breach of contract (discord with staff) | 2 (4.8) | 0 (0) |
| no longer interested in treatment | 1 (2.4) | 0 (0) |
| After release | (n = 30) | (n = 27) |
| Had difficulty accessing MMT, because: | 10 (23.9) | 8 (26.7) |
| forced to relocate (corrective police orders) | 3 (10.0) | 2 (7.4) |
| harassed by police at MMT sites (with or without re-arrest) | 7 (23.3) | 6 (22.2) |
| Still on MMT at 12 months | 18 (60.0) | 10 (37.0) |
| Released on ≤ 80 mg daily | 7/17 (41.2) | 2/14 (14.2) |
| Released on > 80 mg daily | 11/13 (84.6) | 8/13 (61.5) |
HIV, human immunodeficiency virus; SD, standard deviation.
a All values in the table are absolute numbers followed by percentages in parentheses except in this row where they indicate the year.
b Depression scored using the Clinical Epidemiological Scale for Depression (CES-D).
Most prisoners were unwilling to have their HIV status disclosed to their families but requested that their families be educated about the benefits of MMT. Many prisoners were poorly connected with their families because of their opioid dependence and believed that being “treated” would help them to restore their broken family ties. Prisoners’ relatives seemed to appreciate being taught about MMT, yet some of them quarantined former prisoners within the household and treated them with distrust. Finally, despite knowing that MMT has long-term benefits, many patients expected to have all opioids eventually discontinued.
Staff-level factors
At first the primary care physicians in the prison were reluctant to initiate MMT because they felt uncomfortable treating opioid dependence. This was resolved through one-on-one supervision and training, which covered the rationale behind MMT, appropriate dosing of the drug, its adverse side-effects, its pharmacokinetic interactions, and the logistical issues involved in providing for patients’ transitional care. Physicians and patients both wanted to keep doses “low” because they feared the “addictive” effects of MMT. A daily dose of more than 80 mg was established to reduce under-prescribing. In the planning stage there were concerns about possible diversion and overdose; these concerns did not materialize after the standard operating procedures pertaining to clinical care were developed. In Pengkalan Chepa, patients on MMT were initially quarantined while their methadone dose was escalated, but since no adverse effects were observed, this practice was later discontinued. Occasionally, inmates and prison staff engaged in anti-methadone rhetoric that discouraged patients on MMT from continuing their therapy. To overcome this problem and reinforce treatment goals, separate educational sessions for inmates and staff were conducted periodically, generally 3 to 6 months after initiation of the pilot programme.
Educational sessions on the benefits of MMT had to be held repeatedly because of the turnover in prison staff. The highest-ranking prison officials supported the MMT programme, but the high turnover in lower-ranking staff threatened to undermine it. To allay their doubts and address their concerns, we reassured officials that the pilot studies were being monitored and provided programmatic feedback and interactive discussions quarterly. Although all prison officials should receive standardized training, continuing training and monitoring were instructive and helpful in avoiding disruption of the MMT programme as a result of frequent changes in staff.
Institutional-level factors
One critical facilitator and four institutional deterrents were observed during the implementation of MMT programmes. Central to success was the support of the Director-General of the Prisons Department, who was involved from the inception of the programme. Four institutional deterrents, however, also acted as hindrances. First, local police could impose corrective measures without notifying the Prisons Department. For example, they could order prisoners to be relocated to a remote area after their release. Last minute coordination was required to ensure that community-based prisoners had access to a site offering MMT. As a result, relocated patients were less likely to be retained in treatment. Second, the exact date of a prisoner’s release was not always known in advance. All patients on MMT were therefore instructed to inform prison staff of their treatment so that their release from prison could be delayed until after their next dose of MMT and the prison physician had had a chance to have their MMT records transferred to a community MMT site. Third, “lock-downs” – periods when staff put a stop to all movement within the prison for security reasons – threatened to impede prisoners’ access to MMT, and physicians responded in anticipation of such events by distributing methadone directly to their cells. Finally, some community-based MMT programmes reduced patients’ methadone dose after release from prison because they mistakenly considered it too high. Hence, the staff of community-based MMT sites must be made aware of the importance of a high enough maintenance dose of methadone and of the need to escalate the dose in patients released from prison receiving 80 mg or less a day.
Post-release continuity of care
Ensuring continuity of care after release from prison remains difficult because patient supervision lies outside the prison system. Since most MMT programmes are located in urban settings, individuals returning to rural settings had to either forfeit MMT or agree to travel to a community MMT site. A travel distance of more than 25 km was associated with lower retention in treatment. As community-based MMT programmes expand to rural areas, so too can prison-based MMT programmes. Linking patients to MMT upon release was not difficult when the pre-release paperwork was completed in advance and properly transmitted to the community MMT site, especially when accompanied by a phone call to ensure receipt.
Despite education of family members about MMT, reuniting patients with their families often proved problematic; many patients were met with hostility by their relatives. Innovative, culturally-specific educational sessions should be provided before and after release to reduce family conflict around MMT. Re-integration with the family is the most critical aspect of re-entry into society. For patients lacking family support, however, transitional services that provided assistance with reintegration into society (e.g. employment, housing, care for HIV infection, etc.) were just as important in ensuring their retention in MMT.
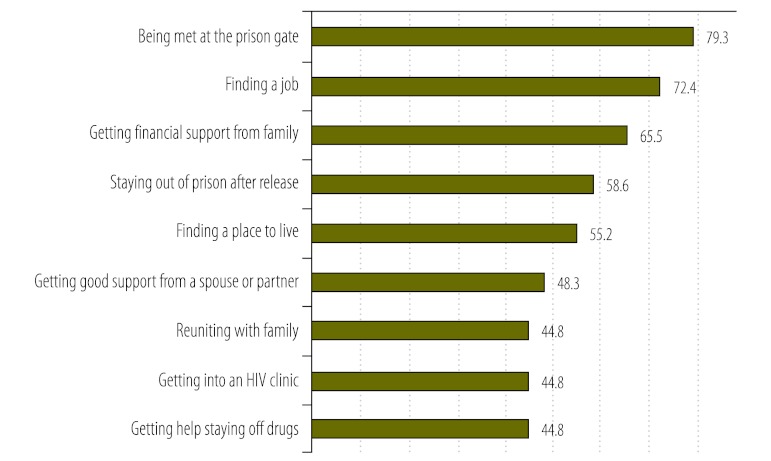
Finally, retention in care was hindered by arrest and harassment of MMT clients by police near MMT sites. Some patients reported they avoided coming to receive their methadone on days when police were waiting outside the programme, or, in some cases, that they discontinued it completely to avoid being detained or bribed. As a result, police were subsequently educated about the benefits of MMT. On the whole, however, prisoners did not report lack of continuity of MMT as their main problem upon re-entering society. Fig. 1 provides a list of the problems they considered most important. Staying off illicit drugs was not highest among them.12
Fig. 1.
Most common difficulties (%) reported by participants in methadone maintenance treatment (MMT) programmes, Kajang and Pengkalan Chepa prisons (Selangor and Kelantan states, respectively), Malaysia, 2008–2009
Conclusion
Prison-based MMT holds considerable promise for reducing HIV infection rates among prison inmates and the general population (Box 1). Implementing MMT in prisons is not easy, although the difficulties are not insurmountable. Other evidence-based opioid agonists, such as buprenorphine or extended-release naltrexone, are used to treat opioid dependence, although transitioning to a community programme may be more difficult with naltrexone, which is administered only once a month.17 Experiences in Malaysia could prove useful in other countries with high rates of opioid dependence and HIV infection among prison inmates. Future interventions should not, however, focus on MMT as an intervention for exclusive use immediately before a prisoner’s release from prison. Instead, MMT should be leveraged throughout the period of incarceration not only to ensure continuity of care for MMT programme participants, but also to ensure adequate MMT dosing before release from prison and avoid the risky injection of opioids within prisons.
Box 1. Summary of main lessons learnt.
Initiation of methadone within prison requires slow, individualized dosing.
Linking individuals to MMT in the community requires strong relationships between prison- and community-based clinics and improved communication between prison and police authorities.
Post-release retention on MMT can be hampered by police harassment near MMT sites and forced relocation laws, which are major deterrents to continuity of care and relapse prevention.
Funding:
This research was supported by research grants from the National Institute on Drug Abuse for research (R01 DA025943, Altice, PI) and a grant from the University of Malaya (HIRGA E000001-20001, Kamarulzaman), as well as a National Institute on Drug Abuse career development award (K24 DA017072, Altice).
Competing interests:
None declared.
References
- 1.Malaysia country advocacy brief: injecting drug use and HIV. Geneva: Joint United Nations Programme on HIV/AIDS; 2009. [Google Scholar]
- 2.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:367–87. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hedrich D, Alves P, Farrell M, Stöver H, Møller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107:501–17. doi: 10.1111/j.1360-0443.2011.03676.x. [DOI] [PubMed] [Google Scholar]
- 4.Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105:1545–54. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz RP, Highfield DA, Jaffe JH, Brady JV, Butler CB, Rouse CO, et al. A randomized controlled trial of interim methadone maintenance. Arch Gen Psychiatry. 2006;63:102–9. doi: 10.1001/archpsyc.63.1.102. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz RP, Kelly SM, O’Grady KE, Mitchell SG, Peterson JA, Reisinger HS, et al. Attitudes toward buprenorphine and methadone among opioid-dependent individuals. Am J Addict. 2008;17:396–401. doi: 10.1080/10550490802268835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dolan KA, Wodak AD, Hall WD. Methadone maintenance treatment reduces heroin injection in New South Wales prisons. Drug Alcohol Rev. 1998;17:153–8. doi: 10.1080/09595239800186951. [DOI] [PubMed] [Google Scholar]
- 8.Howells C, Allen S, Gupta J, Stillwell G, Marsden J, Farrell M. Prison based detoxification for opioid dependence: a randomised double blind controlled trial of lofexidine and methadone. Drug Alcohol Depend. 2002;67:169–76. doi: 10.1016/S0376-8716(02)00024-8. [DOI] [PubMed] [Google Scholar]
- 9.Kerr T, Jurgens R. Methadone maintenance therapy in prisons: reviewing the evidence. Montreal: Canadian HIV/AIDS Legal Network; 2004. [Google Scholar]
- 10.Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abuse Treat. 2009;37:277–85. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorta A. Monitoring the New South Wales methadone program: 1986–1991. New South Wales: Department of Corrective Services; 1992. [Google Scholar]
- 12.Choi P, Kavasery R, Desai MM, Govindasamy S, Kamarulzaman A, Altice FL. Prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Int J STD AIDS. 2010;21:416–23. doi: 10.1258/ijsa.2009.009180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reid G, Kamarulzaman A, Sran SK. Malaysia and harm reduction: the challenges and responses. Int J Drug Policy. 2007;18:136–40. doi: 10.1016/j.drugpo.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Noordin NM, Merican MI, Rahman HA, Lee SS, Ramly R. Substitution treatment in Malaysia. Lancet. 2008;372:1149–50. doi: 10.1016/S0140-6736(08)61479-8. [DOI] [PubMed] [Google Scholar]
- 15.Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013 doi: 10.1016/j.drugalcdep.2013.01.005. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohamad N, Bakar NH, Musa N, Talib N, Ismail R. Better retention of Malaysian opiate dependents treated with high dose methadone in methadone maintenance therapy. Harm Reduct J. 2010;7:30. doi: 10.1186/1477-7517-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: a review and call for evidence-based treatment for released prisoners. Am J Drug Alcohol Abuse. 2011;37:12–21. doi: 10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]