Abstract
Information processing bias was evaluated in a sample of 25 older adults with generalized anxiety disorder (GAD) over the course of 12 weeks of escitalopram pharmacotherapy. Using the CANTAB Affective Go/No Go test, treatment response (as measured by the Hamilton Anxiety Rating Scale, Penn State Worry Questionnaire, and Generalized Anxiety Disorder Severity Scale) was predicted from a bias score (i.e., difference score between response latencies for negative and positive words) using mixed-models regression. A more positive bias score across time predicted better response to treatment. Faster responses to positive words relative to negative words were associated with greater symptomatic improvement over time as reflected by scores on the GADSS. There was a trend towards significance for PSWQ scores and no significant effects related to HAMA outcomes. These preliminary findings offer further insights into the role of biased cognitive processing of emotional material in the manifestation of late-life anxiety symptoms.
Keywords: Generalized Anxiety Disorder, Aging, Attention, Information Processing Bias, Escitalopram
Information processing biases have been implicated as both causal and maintenance factors in cognitive models of anxiety(e.g., Beck & Clark, 1997; Mogg & Bradley, 2005). For example, among younger and middle-aged adults, attention bias for threat-relatedstimuli has been linked to anxiety symptomatology, including symptoms of Generalized Anxiety Disorder(GAD; Becker, Rinck, Margraf, & Roth, 2001; Bradley, Mogg, Millar, & White, 1995; Bradley, Mogg, White, Groom, & de Bono, 1999; Mogg, Bradley, Williams, & Mathews, 1993). In fact, it has been demonstrated that measures of attention bias can predict treatment outcome among persons with GAD (Mogg, Bradley, Millar, & White, 1995). There is also some evidence that information processing biases can be altered with pharmacotherapy (Mogg, Baldwin, Brodrick, & Bradley, 2004). Preliminary research on attention training programs suggests that reductions in the magnitude of an attention bias towards threatening information can lead to reductions in anxiety symptoms, further suggesting that information processing biases play a role in the development or maintenance of GAD (e.g., Amir, Beard, Burns, & Bomyea, 2009; Hazen, Vasey, & Schmidt, 2009).Although progress has been made in this area, we know very little about whether these relationships between affective biases and anxiety are observed in older populations.
Among older adults without anxiety disorders, there is evidence for a bias toward positive material. Research on healthy aging suggests that older adults tend to attend to and remember positive information relative to neutral or negative information, a phenomenon that has been dubbed “the positivity effect” (cf. Mather & Carstensen, 2005). According to Socioemotional Selectivity Theory, this bias for positive information is not accidental; rather, it is theorized to reflect a shift of motivational goals with age from a focus on the acquisition of knowledge and information to the maintenance of emotional well-being (Carstensen, Isaacowitz, & Charles, 1999; Charles & Carstensen, 2007). It is thought that this change occurs due to age-related shifts in time perspective, such that individuals become more acutely aware of the limited nature of time as they grow older.
Despite the general developmental trend to focus upon the positive in later life, many older adults struggle with anxiety. The prevalence of anxiety in community-living older adults is as high as 10%, with most research indicating that GAD is the most common anxiety disorder in late life(Bryant, Jackson, & Ames, 2008; Flint, 2005). Onset of the disorder typically occurs in early adulthood, though some individuals develop it in later life (Chou, 2009). Among the elderly, GAD is associated with increased functional impairment and poorer quality of life (e.g., Porensky et al., 2009; Wetherell et al., 2004). The onset or maintenance of later-life GAD has been attributed to the quality and quantity of psychosocial stressors that are commonly faced by the elderly (e.g., de Beurs et al., 1999), as well as vulnerability to cognitive decline (particularly in the domain of executive functioning; e.g., Mohlman & Gorman, 2005) due to advanced age.
Although evidence supports the use of various elements of cognitive behavioral therapy for treating anxiety disorders, including GAD, in younger and middle-aged adults, these interventions are substantially less effective in older adults, with effect sizes approximately half of those detected in younger or middle-aged samples (Covin, Ouimet, Seeds, & Dozois, 2008; Gould, Coulson, & Howard, 2012). This suggests the possibility of age-related differences in factors affecting the development and maintenance of anxiety.
One such factor could be information processing biases, yet research in this area is relatively new. To date, completed studies have examined the associations between attention bias and anxiety in older people. Two published studies (Fox & Knight, 2005; Lee & Knight, 2009) showed that older adults (who underwent an anxious mood induction or were high in trait anxiety, respectively) showed greater attention to anxiety-related or negatively-valenced stimuli. Another study examining selective attention in fear of falling showed that older adults with fear of falling had greater difficulty disengaging from fall-relevant words than did those without fear of falling (Brown, White, Doan, & de Bruin, 2011). Utilizing an emotional Stroop paradigm to evaluate attention bias among anxious older adults, Price and colleagues (in press) found that older adults who habitually worry demonstrated a bias for threat-related information. Price, Eldreth, and Mohlman (2011) also used thee Stroop task to examine the neural substrates of attention bias among older adults with GAD. This latter study was the first to include a clinically diagnosed sample. Results indicated that late-life GAD is associated with an attention bias for negative information. The aforementioned findings are largely consistent with the biases for threat-related information observed among anxious younger adults.
The present study is part of a larger project examining the efficacy of treatment for older adults with GAD. We were interested in whether information processing biases serve as a predictor of treatment outcome. Harmer and colleagues (2009) have suggested that “antidepressants work by remediating negative affective biases […] relatively quickly following drug administration” (p. 102). Given evidence that interpretation biases among patients with GAD can be changed through short-term SSRI pharmacotherapy (e.g., Mogg et al., 2004), and that information processing biases can predict treatment outcome (e.g., Mogg et al., 1995),we sought to explore whether information processing biases over the course of a 12-week open-label medication trial for anxiety were associated with treatment outcome among older adults with GAD. We chose to use the Cambridge Neuropsychological Test Automated Battery (CANTAB) Affective Go-No Go (AGN) test(Cambridge Cognition, 2006; Murphy et al., 1999) to evaluate differences in speed of classifying positive and negative words. The CANTAB AGN is a set-shifting task requiring affective labeling and inhibitory control (see further description below, under “Study Tasks”). Specifically, we hypothesized that faster processing of positive words relative to negative words would be associated with better treatment outcome (i.e., lower levels of anxiety over time) among treatment-seeking patients with GAD.
Method
Participants
Participants in the present study were 25 older adults (age 60 years or older) with a principal or co-principal (i.e., most severe) diagnosis of GAD according to criteria established by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IVTR; American Psychiatric Association, 2000) who were awaiting randomization into a study evaluating the effects of cognitive-behavioral therapy as an augmentation to pharmacotherapy. GAD diagnosis was established using the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1995); the interclass correlation coefficient for the GAD diagnosis among raters was 0.70, indicating acceptable reliability. All participants were treated with 12 weeks of open-label escitalopram (10mg, increased to 20mg at 4 weeks as tolerated if response was not achieved at the lower dose). Participants were not permitted to receive psychotherapy or other anxiolytic pharmacotherapy, although some participants who were taking benzodiazepines or sleep medications were allowed to remain on these medications at a consistent low dose. A board-certified geriatric psychiatrist monitored the participants’ response to escitalopram and made adjustments as needed. Participants were recruited from clinics at the University of California, San Diego, as well as other community medical practices, senior centers, and through flyers, posters, and advertisements. Exclusion criteria were dementia or cognitive impairment (as defined as a score of 25 or less on the Mini-Mental Status Exam, or MMSE; Folstein, Folstein, & McHugh, 1975), history of bipolar disorder or psychosis, substance abuse within the past 6 months, inability or unwillingness to discontinue other pharmacotherapy or psychotherapy, and serious medical conditions that would interfere with study participation or result in contraindication to escitalopram (e.g., oxygen-dependent chronic obstructive pulmonary disease, congestive heart failure, active cancer treatment, end-stage liver or kidney disease). Informed consent was obtained and documented on signed forms for all participants. Enrolled participants were compensated $100 for their participation.
Participants were fifteen women and ten men with a mean age of 68.8 years (SD = 7.6). The racial composition of the sample was predominantly White (80%), with 12% Latino, 4% Asian, and 4% African-American. Participants had a mean of 16.4 years (SD = 2.5) of education. A plurality of participants were married (36%), and 20% were never married, 20% were widowed, 16% were divorced, 4% were separated, and 4% were cohabitating. Sixteen percent had a comorbid diagnosis of major depression and 40% had any comorbid Axis I disorder. Enrolled participants reported taking other medications in addition to the escitalopram prescribed for this study, some of which belong in classes that may affect cognition. These medication classes, along with percentage of participants who reported taking a medication in the class, include: analgesic combination (12%), anticonvulsant (4%), antihistamine (24%), benzodiazepine (24%), beta blocker (12%), cholinergic receptor blocker (4%), opiate agonist (4%), and sedative/hypnotic (8%).
Measures
Anxiety symptoms were monitored by three trained raters over a 12 week period using the Hamilton Anxiety Rating Scale (HAMA; Hamilton, 1959), Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990), and Generalized Anxiety Disorder Severity Scale (GADSS; Shear, Belnap, Mazumdar, Houck, & Rollman, 2006). Two of the raters had Masters degrees in psychology. A third rater earned a Masters degree over the course of the study.
The HAMA is a 14-item interview-rated measure of anxiety primarily assessing somatic symptoms (i.e., physical complaints related to anxiety). It is considered the “gold standard” outcome measure in studies of GAD pharmacotherapy treatment. It has been validated in samples of older patients with GAD and normal community volunteers (Beck, Stanley, & Zebb, 1999; Diefenbach et al., 2001). A HAMA score of 17 or greater was an inclusion criterion for the study. The HAMA was completed during assessments at weeks 0, 1, 2, 3, 4, 6, 8, 10, and 12. The interclass correlation coefficient among raters was 0.93, indicating excellent reliability.
The PSWQ is a widely used, 16-item self-report questionnaire designed to measure excessive and uncontrollable worry. It has been validated in samples of older adults diagnosed with GAD (Beck, Stanley, & Zebb, 1995; Stanley, Novy, Bourland, Beck, & Averill, 2001). Participants completed the PSWQ at weeks 0 and 12 to reduce participant burden. One participant was missing PSWQ data at week 0; random effects regression takes missing data into account, but we also ran the models using last observation carried back and results did not change.
The GADSS is a recently developed, 6-item interviewer-rated measure of GAD symptoms that has shown good reliability, discriminant validity, and sensitivity to treatment in older adults (Andreescu et al., 2008; Weiss et al., 2009). The GADSS was completed on the same schedule as the interview-based HAMA. Interrater reliability was established by co-rating patient training videotapes until at least 80% agreement was reached. Due to loss of a computer file, the intraclass correlation coefficient among raters is not available.
Study Tasks
To assess information processing bias, participants completed the CANTAB AGN test (Murphy et al., 1999) at weeks 0, 2, 4, 8, and 12. The AGN test, designed to evaluate decision-making ability and response control, is a 10-minute task requiring information processing of emotional words. Affectively-valenced words are presented one at a time in blocks of 18 words (i.e., nine positive and nine negative words).Each word is presented for 300 ms, followed by a 900 ms inter stimulus interval. The test uses a total of eight blocks. Participants are initially instructed to respond by pressing the space bar when they see positive words (e.g., hopeful), but not when they see negative words (e.g., glum). After two blocks requiring responses to positive words, participants are then instructed to respond when they see a negative word. Valence category alternates every two blocks (i.e., the test follows a PPNNPPNN pattern). Before beginning the test, participants are given the opportunity to practice for two blocks.
In order to evaluate information processing bias, we compared response latency (i.e., the time between presentation of a stimulus and response) to positive and negative words. We examined the difference in latency for positive and negative words by subtracting the response latency for negative words from the response time for positive words (+Latency minus −Latency). A positive difference indicates that participants responded more quickly to negative words in relation to positive words.
Data Analytic Strategy
The information processing bias variable was Winsorized. Any missing AGN test data was replaced with last observation carried forward. One participant’s data was omitted due to invalid responding. Descriptive statistics were calculated for all variables and outcomes at all time points. T-tests comparing pre-treatment and week 12 scores were conducted. Outcomes were anxiety, worry, and GAD symptoms as measured by the HAMA, PSWQ, and GADSS, respectively. Repeated measures mixed-effect regression models were conducted to examine the longitudinal association between anxiety and affective information processing bias over the 12-week treatment period. In these models, time was a categorical variable representing number of weeks in treatment (0–12). Information processing bias, which was time varying, was included in the models and centered on the baseline mean. We ran separate models for each outcome variable. The time by bias interaction was included in the model to examine how these predicted change in anxiety symptomatology over time. The covariance structure was unstructured.
Results
Descriptive Statistics and Change over Treatment
Means, standard deviations, and pre-post comparisons of the clinical and AGN variables at each time point are presented in Table 1. At baseline, participants reported moderate levels of anxiety, worry, and GAD symptoms. Paired t-tests comparing week 0 and 12 means suggest that participants had significant decreases on the HAMA, t(24) = 12.47, p< .01, PSWQ, t(23) = 2.93, p< .01, and GADSS, t(24) = 5.12, p< .01. There were no significant changes in information processing bias over the treatment period, t(24) = 0.67, p = .51.
Table 1.
Means and Standard Deviations of Scores on Measures of Somatic Anxiety, Pathological Worry, and Generalized Anxiety Disorder Symptoms Over Time
| Week 0 | Week 2 | Week 4 | Week 8 | Week 12 | Week 0 to 12 | p | |
|---|---|---|---|---|---|---|---|
| Comparison (t) | |||||||
| HAMA | 21.63 | 14.36 | 15.14 | 12.57 | 11.17 | 12.47 | <.01 |
| (3.61) | (4.65) | (5.43) | (5.29) | (4.49) | |||
| PSWQ | 55.23 | - | - | - | 51.56 | 2.93 | <.01 |
| (10.95) | - | - | - | (11.07) | |||
| GADSS | 14.80 | 12.40 | 11.84 | 10.32 | 10.44 | 5.15 | <.01 |
| (3.75) | (3.74) | (4.50) | (3.85) | (3.78) | |||
| + Latency (ms) | 564.74 | 573.51 | 596.50 | 565.33 | 575.49 | −1.14 | .27 |
| (90.97) | (106.72) | (126.66) | (95.82) | (97.46) | |||
| − Latency (ms) | 578.43 | 595.23 | 587.29 | 577.98 | 580.89 | −0.28 | .82 |
| (98.29) | (110.42) | (108.81) | (91.38) | (93.28) | |||
| + Latency (ms) minus | −5.69 | −13.72 | 17.21 | −4.65 | 2.60 | 0.67 | .51 |
| − Latency (ms) | (49.56) | (40.12) | (48.25) | (31.93) | (32.95) | ||
| + Commission errors | 5.32 | 3.20 | 3.68 | 3.48 | 3.96 | 1.62 | .18 |
| (4.87) | (3.03) | (3.90) | (3.22) | (5.30) | |||
| + Omission errors | 2.72 | 1.64 | 2.68 | 1.12 | 1.84 | 2.00 | .06 |
| (3.48) | (2.27) | (4.03) | (1.81) | (3.14) | |||
| − Commission errors | 2.92 | 2.80 | 2.28 | 2.96 | 2.28 | 1.16 | .26 |
| (3.23) | (2.38) | (1.72) | (2.68) | (2.41) | |||
| − Omission errors | 1.60 | 2.24 | 2.04 | 1.44 | 1.16 | 1.39 | .18 |
| (1.73) | (2.13) | (2.32) | (1.61) | (1.91) |
Note: HAMA = Hamilton Anxiety Rating Scale; PSWQ = Penn State Worry Questionnaire; GADSS = Generalized Anxiety Disorder Symptom Scale; + Latency = latency to identify positive words (ms); − Latency = latency to identify negative words (ms).
Linear Mixed Models
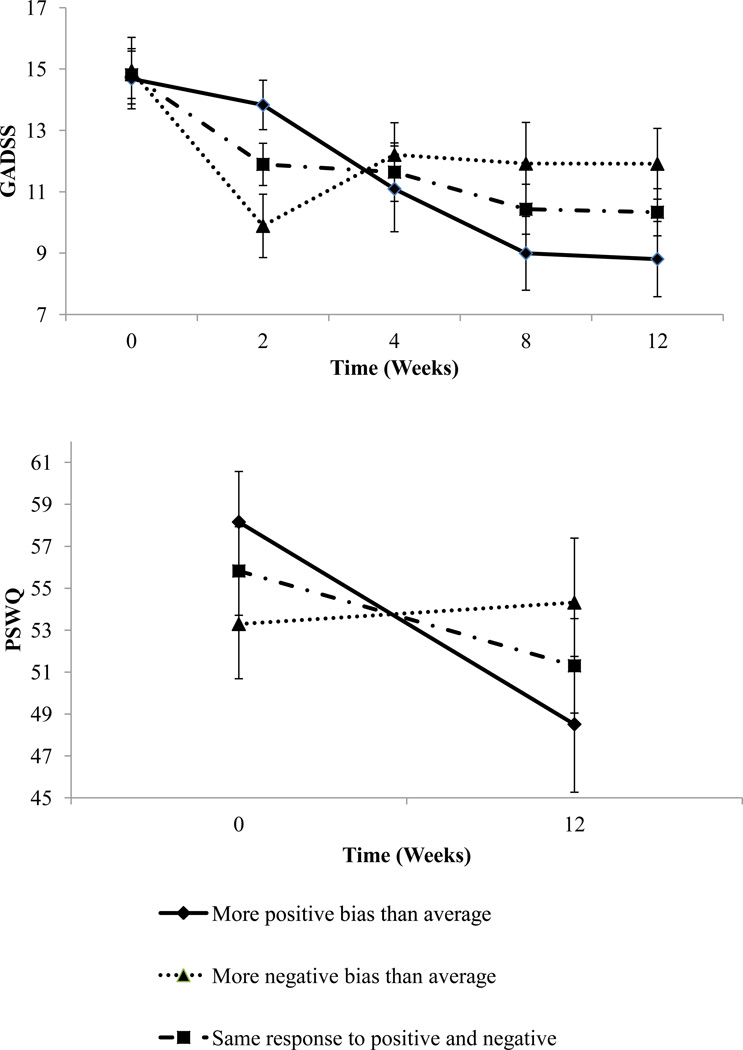
The information response bias by time interaction was significant for GAD symptoms as measured by the GADSS, F(1,24) = 4.28; p = .009. For worry symptoms as measured by the PSWQ, the information response bias by time interaction showed a trend towards significance, F(1,24) = 4.01;p= .06. Figure 1 displays the predicted means and standard errors at each time point for those at the mean with respect to information processing bias and those at +/− 1 SD. Both of these interactions suggest that quicker response to positive words relative to negative words was associated with greater symptomatic improvement over time. The information response bias was not associated with clinical improvement in somatic anxiety symptoms as measured by the HAMA, F(1,24) = 0.87; p = .49.
Figure 1.
Predicted scores on the GADSS and PSWQ for individuals at the mean and one standard deviation above and below the mean difference in latency of response to positive and negative words.
Discussion
To our knowledge, the current study represents the first attempt to examine emotionally biased information processing in older adults with a clinical anxiety disorder diagnosis over the course of treatment. Overall, these preliminary results suggest that biased processing of affective material, as measured by a difference score calculated by subtracting the response latency for negative words from the response latency for positive words, is related to response to psychopharmacological treatment for geriatric GAD. In particular, our findings suggest that faster responses to positive words were associated with greater reduction in GAD symptoms, as measured by the GADSS, over time. There was also a trend towards significance for worry symptoms to improve, as measured by changes in the PSWQ. Interestingly, information processing biases were not associated with a reduction in anxiety symptoms as measured by the HAMA over time. We speculate that because the HAMA primarily measures somatic anxiety, such as cardiac symptoms and gastrointestinal distress, it is not as closely related to information processing biases as is worry.
The buffering effects of focusing on positive information is consistent with findings from the healthy aging literature on the positivity effect (e.g., Carstensen & Mikels, 2005), in which non-disordered older adults show a consistent preference for positive information relative to neutral or negative information. This preferential processing of positive information is thought to be associated with improved emotion regulation abilities in later life. For example, Labouvie-Vief and colleagues (2007) have hypothesized that, at least among individuals without psychiatric disorders, older adults strategically employ selective attention for positive information to optimize their affective experience (cf. Charles & Carstensen, 2007 for a review on emotion regulation and aging). The present study provides preliminary support for the idea that relatively faster processing of positive material may predict better response to medication for the treatment of GAD in geriatric populations.
Some methodological issues may have affected our findings. First, consistent with the hypothesis-generating nature of this pilot investigation, we examined three different outcome variables in a relatively small sample of participants. We therefore had low power to detect significant associations, and not surprisingly, findings were not uniform across the three outcome measures. This may represent real differences in the impact of type of symptoms measured, as suggested above, or it may be an artifact of the small sample size. As in any repeated measures design, there is the possibility that practice effects for the AGN task influenced the findings; lack of a placebo-treated control group may exacerbate this problem. It should further be noted that scores on the HAMA decreased substantially between baseline and week 2, suggesting the presence of a strong placebo effect. On a related note, norms for the AGN task among older adult and/or anxious respondents were unavailable. Furthermore, although a multiple baseline design could have strengthened our methodology, time demands and other experimental constraints related to the pilot status of this study prevented its use. Future research utilizing these or similar methods should also ensure that participants rate task words for valence and arousal to ensure the adequacy of the stimuli in a geriatric GAD sample. A more comprehensive study might include other measurements of a participant’s affective labeling, set-shifting, and inhibitory control abilities in order to make stronger conclusions about the mechanisms underlying observed relationships.
In addition, due to the constraints of the parent study, we were unable to include a young adult comparison group. Future research would benefit from performing direct comparisons with a non-clinical older adult sample and/or an anxious younger adult sample. Within the sample of the present study, close to one-fifth of participants were assigned a comorbid diagnosis of depression. It is relatively common for depressive and anxious symptoms to overlap, especially in later life, but the unique and differential effects of depression versus anxiety on cognitive processing in older adulthood remain to be better understood. As a result, the practical and theoretical benefits and consequences of using a sample with comorbid diagnoses should be carefully considered in future research, especially in studies of information processing biases. Moreover, the inclusion of participants with major depression may have resulted in higher GADSS scores than are often reported for older adults with GAD; these higher scores, in turn, may explain why findings were significant for this measure. Additionally, ongoing measures of symptoms associated with the secondary disorder (in this case, major depression) should be utilized for monitoring and investigative reasons.
Despite these shortcomings, all of which could be addressed in future research, we believe the current study offers exciting preliminary findings about relationships between affective information processing bias and response to pharmacological intervention among older adults with an anxiety disorder. Strengths of the present study include use of a clinical sample with GAD diagnoses ascertained by the SCID and use of several different outcome measures, which may reflect different processes that could be investigated more thoroughly in future research. The CANTAB AGN, while not previously used in studies of adults with GAD, is a commercially available computerized instrument that measures speed and accuracy of processing both positive and negative words and could easily be used in replication studies. Participants underwent multiple assessments, allowing for the use of more powerful data analytic tools. Finally, participants in this study were evaluated in the context of treatment according to a controlled, consistent pharmacotherapy protocol.
The results from this preliminary study offer a glimpse into the nature of the relationships between affective information processing biases and anxiety symptoms in older adults, while raising important questions and avenues for future research. Although preferential attention for positive information is frequently observed in non-disordered older adults, it has been unclear whether the information processing bias among older adults with anxiety disorders would manifest as a lack of the positivity bias seen in same-aged, non-disordered peers, or as a negativity bias similar to that observed in younger adults with anxiety disorders. Recent research has shown that, similar to findings in the younger adult literature, older adults with GAD demonstrate attention biases for threat-related information (e.g., Brown et al., 2011; Lee & Knight, 2009; Price et al., 2011). To our knowledge, this is the first study to evaluate associations between information processing bias and anxiety during active treatment for late-life GAD. At least in this preliminary study on a small sample, quicker processing of positive words relative to negative words was associated with better response to pharmacotherapy for GAD.
Additional research in this area will shed light on cognitive factors that influence the etiology, maintenance, and treatment of anxiety in older adults. Clearly, results from this study should be replicated in a larger sample. It would also be interesting to examine whether cognitive-behavioral therapy or other treatments targeting information processing biases influence the observed relationships between bias and anxiety symptomatology. There is evidence that indicates information processing biases are altered through participation in CBT for anxiety disorders in younger people (e.g., Mathews, Mogg, Kentish, & Eysenck, 1995; Mattia, Heimberg, & Hope, 1993; Teachman, Marker, & Smith-Janik, 2008). Recent advances in cognitive bias modification have shown that attention biases are malleable directly, with resulting improvement in anxiety symptoms (e.g., Amir et al., 2009). Since conventional CBT may not be as effective in older adults with anxiety disorders as in younger clients (Covin et al., 2008; Gould et al., 2012), cognitive bias modification may prove a more effective non-pharmacological alternative for anxious older adults.
-
!!
Cognitive processing of emotional words was evaluated in a sample of 25 older adults with generalized anxiety receiving pharmacotherapy.
-
!!
We measured biased processing by subtracting the speed of response to negative words from the speed of response to positive words.
-
!!
Faster responses to positive words relative to negative words were associated with better response to medication.
-
!!
Findings represent a step toward understanding the role of emotional information processing bias in anxiety in later life.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreescu C, Belnap BH, Rollman BL, Houck P, Ciliberti C, Muzumdar S, Shear MK, Lenze EJ. Generalized anxiety disorder severity scale validation in older adults. American Journal of Geriatric Psychiatry. 2008;16:813–818. doi: 10.1097/JGP.0b013e31817c6aab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Clark DA. An information processing model of anxiety: Reconsidering the role of automatic and strategic processes. Behaviour Research and Therapy. 1997;35:49–58. doi: 10.1016/s0005-7967(96)00069-1. [DOI] [PubMed] [Google Scholar]
- Beck JG, Stanley MA, Zebb BJ .Psychometric properties of the Penn State Worry Questionnaire. Journal of Clinical Geropsychology. 1995;1:33–42. [Google Scholar]
- Beck JG, Stanley MA, Zebb BJ .Effectiveness of the Hamilton Anxiety Rating Scale with older generalized anxiety disorder patients. Journal of Clinical Geropsychology. 1999;5:281–290. [Google Scholar]
- Becker ES, Rinck M, Margraf J, Roth WT. The emotional Stroop effect in anxiety disorders: General emotionality or disorder specificity? Journal of Anxiety Disorders. 2001;15:147–159. doi: 10.1016/s0887-6185(01)00055-x. [DOI] [PubMed] [Google Scholar]
- Bradley BP, Mogg K, Millar N, White J. Selective processing of negative information: Effects of clinical anxiety, concurrent depression, and awareness. Journal of Abnormal Psychology. 1995;104:532–536. doi: 10.1037//0021-843x.104.3.532. [DOI] [PubMed] [Google Scholar]
- Bradley BP, Mogg K, White J, Groom C, de Bono J. Attentional bias for emotional faces in generalized anxiety disorder. The British Journal of Clinical Psychology. 1999;38:267–278. doi: 10.1348/014466599162845. [DOI] [PubMed] [Google Scholar]
- Brown LA, White P, Doan JB, de Bruin N. Selective attentional processing to fall-relevant stimuli among older adults who fear falling. Experimental Aging Research. 2011;37:330–345. doi: 10.1080/0361073X.2011.568833. [DOI] [PubMed] [Google Scholar]
- Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: Methodological issues and a review of the literature. Journal of Affective Disorders. 2008;109:233–250. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Cambridge Cognition. Cambridge Neuropsychological Test Automated Battery manual. Cambridge, UK: Cambridge Cognition Limited; 2006. [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Mikels JA. At the intersection of emotion and cognition: Aging and the positivity effect. Current Directions in Psychological Science. 2005;14:117–121. [Google Scholar]
- Charles ST, Carstensen LL. Emotion regulation and aging. In: Gross JJ, editor. Handbook of emotion regulation. New York, NY: Guilford Press; 2007. pp. 307–327. [Google Scholar]
- Chou KL. Age at onset of generalized anxiety disorder in older adults. American Journal of Geriatric Psychiatry. 2009;17:455–464. doi: 10.1097/jgp.0b013e31818f3a93. [DOI] [PubMed] [Google Scholar]
- Covin R, Ouimet AJ, Seeds PM, Dozois DJ .A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders. 2008;22:108–116. doi: 10.1016/j.janxdis.2007.01.002. [DOI] [PubMed] [Google Scholar]
- deBeurs E, Beekman ATF, van Balkom AJLM, Deeg DJH, van Dyck R, van Tilburg W. Psychological Medicine. 1999;29:583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, Stanley MA, Beck JG, Novy DM, Averill PM, Swann AC. Examination of the Hamilton Scales in assessment of anxious older adults: A replication and extension. Journal of Psychopathology Behavioral Assessment. 2001;23:117–124. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Flint AJ. Generalised anxiety disorder in elderly patients: Epidemiology, diagnosis, and treatment options. Drugs and Aging. 2005;22:101–114. doi: 10.2165/00002512-200522020-00002. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fox L, Knight B. The effects of anxiety on attentional processes in older adults. Aging & Mental Health. 2005;9:585–593. doi: 10.1080/13607860500294282. [DOI] [PubMed] [Google Scholar]
- Gould RL, Coulson MC, Howard RJ. Efficacy of cognitive behavioral therapy for anxiety disorders in older people: A meta-analysis and meta-regression of randomized controlled trials. Journal of the American Geriatrics Society. 2012;60:218–29. doi: 10.1111/j.1532-5415.2011.03824.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Harmer CJ, Goodwin GM, Cowen PJ. Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. British Journal of Psychiatry. 2009;195:102–108. doi: 10.1192/bjp.bp.108.051193. [DOI] [PubMed] [Google Scholar]
- Hazen RA, Vasey MW, Schmidt NB. Attentional retraining: A randomized clinical trial for pathological worry. Journal of Psychiatric Research. 2009;43:627–633. doi: 10.1016/j.jpsychires.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Labouvie-Vief G, Diehl M, Jain E, Zhang F. Six-year change in affect optimization and affect complexity across the adult life span: A further examination. Psychology and aging. 2007;22(4):738. doi: 10.1037/0882-7974.22.4.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee LO, Knight BG. Attentional bias for threat in older adults: Moderation of the positivity bias by trait anxiety and stimulus modality. Psychology and Aging. 2009;24:741–747. doi: 10.1037/a0016409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Shear MK, Dew MA, Miller MD, Pollock BG, Reynolds CF. Efficacy and tolerability of citalopram in the treatment of late-life anxiety disorders: Results from an 8-week randomized, placebo-controlled trial. American Journal of Psychiatry. 2005;162:146–150. doi: 10.1176/appi.ajp.162.1.146. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rollman BL, Shear MK, Dew MA, Pollock BG, Ciliberti C, Reynolds CF. Escitalopram for older adults with generalized anxiety disorder. Journal of the American Medical Association. 2009;301:295–303. doi: 10.1001/jama.2008.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather M, Carstensen LL. Aging and motivated cognition: The positivity effect in attention and memory. Trends in Cognitive Science. 2005;9:496–502. doi: 10.1016/j.tics.2005.08.005. [DOI] [PubMed] [Google Scholar]
- Mathews A, Mogg K, Kentish J, Eysenck M. Effect of psychological treatment on cognitive bias in generalized anxiety disorder. Behaviour Research and Therapy. 1995;33:293–303. doi: 10.1016/0005-7967(94)e0022-b. [DOI] [PubMed] [Google Scholar]
- Mattia JI, Heimberg RG, Hope DA. The revised Stroop color-naming task in social phobics. Behaviour Research and Therapy. 1993;31:305–313. doi: 10.1016/0005-7967(93)90029-t. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP. Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive Therapy & Research. 2005;29:29–45. [Google Scholar]
- Mogg K, Bradley BP, Millar N, White J. A follow-up study of cognitive bias in generalized anxiety disorder. Behaviour Research and Therapy. 1995;33:927–935. doi: 10.1016/0005-7967(95)00031-r. [DOI] [PubMed] [Google Scholar]
- Mogg K, Baldwin DS, Brodrick P, Bradley P. Effect of short-term SSRI treatment on cognitive bias in generalised anxiety disorder. Psychopharmacology. 2004;176:466–470. doi: 10.1007/s00213-004-1902-y. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP, Williams R, Mathews A. Subliminal processing of emotional information in anxiety and depression. Journal of Abnormal Psychology. 1993;102:304–311. doi: 10.1037//0021-843x.102.2.304. [DOI] [PubMed] [Google Scholar]
- Mohlman J, Gorman JM. The role of executive functioning in CBT: A pilot study with anxious older adults. Behaviour Research and Therapy. 2004;43:447–465. doi: 10.1016/j.brat.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, Paykel ES. Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine. 1999;29:1307–1321. doi: 10.1017/s0033291799001233. [DOI] [PubMed] [Google Scholar]
- Porensky EK, Dew MA, Karp JF, Skidmore E, Rollman BL, Shear MK, Lenze EJ. The burden of late-life generalized anxiety disorder: Effects on disability, health-related quality of life, and healthcare utilization. American Journal of Geriatric Psychiatry. 2009;17:473–482. doi: 10.1097/jgp.0b013e31819b87b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Eldreth DA, Mohlman J. Deficient prefrontal attentional control in late-life generalized anxiety disorder: An fMRI investigation. Translational Psychiatry. 2011;1(e46):1–8. doi: 10.1038/tp.2011.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Siegle G, Mohlman J. Emotional Stroop performance in older adults: Effects of habitual worry. American Journal of Geriatric Psychiatry. doi: 10.1097/JGP.0b013e318230340d. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurmans J, Comijs H, Emmelkamp PMG, Gundy CMM, Weijnen I, van den Hout M, van Dyck R. Effectiveness of cognitive-behavioral therapy and sertraline versus a waitlist control group for anxiety disorders in older adults. American Journal of Geriatric Psychiatry. 2006;14:255–263. doi: 10.1097/01.JGP.0000196629.19634.00. [DOI] [PubMed] [Google Scholar]
- Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL .Generalized anxiety disorder severity scale (GADSS): A preliminary validation study. Depression and Anxiety. 2006;23:77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- Stanislaw H, Todorov N. Calculation of signal detection theory measures. Behavior Research Methods, Instruments, & Computers. 1999;31:137–149. doi: 10.3758/bf03207704. [DOI] [PubMed] [Google Scholar]
- Stanley MA, Novy DM, Bourland SL, Beck JG, Averill PM. Assessing older adults with generalized anxiety: A replication and extension. Behaviour Research and Therapy. 2001;39:221–235. doi: 10.1016/s0005-7967(00)00030-9. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, Smith-Janik SB. Automatic associations and panic disorder: Trajectories of change over the course of treatment. Journal of Consulting and Clinical Psychology. 2008;76:988–1002. doi: 10.1037/a0013113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BJ, Calleo J, Rhoades HM, Novy DM, Kunik ME, Lenze EJ, Stanley MA. The utility of the Generalized Anxiety Disorder Severity Scale (GADSS) with older adults in primary care. Depression and Anxiety. 2009;26:E10–E15. doi: 10.1002/da.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherell J, Thorp SR, Patterson TL, Golshan S, Jeste DV, Gatz M. Quality of life in geriatric generalized anxiety disorder: A preliminary investigation. Journal of Psychiatric Research. 2004;38:305–312. doi: 10.1016/j.jpsychires.2003.09.003. [DOI] [PubMed] [Google Scholar]