Abstract
INTRODUCTION
Acute chylous peritonitis, a rare condition, is defined as an abrupt chylous fluid accumulation in the peritoneal space in the absence of a significant underlying pathology. Diagnosis is difficult due to abrupt onset and accompanying acute abdomen signs.
PRESENTATION OF CASE
Here we presented the case of a 32-year-old female patient who underwent laparoscopy due to acute abdomen findings and was diagnosed with acute chylous peritonitis. No underlying pathologies were detected, and only irrigation and drainage were applied. She was discharged unproblematically with a low-fat diet and somatostatin administration. No recurrence occurred, and no other pathologies were encountered during her 9-month visit.
DISCUSSION
Chylous fluid accumulation is reported to arise from various etiological factors such as trauma, chronic liver diseases, tuberculosis, filariasis, radiation, abdominal aorta surgery, different peritoneal infection and extended lymph node dissections. We have presented an acute chylous peritonitis case that was admitted with acute abdomen findings and followed up and treated with laparoscopy.
CONCLUSION
In conclusion, this case demonstrates the effectiveness of laparoscopy in acute abdomen cases in which a specific preoperative diagnosis cannot be made. Aspiration of the fluid and drainage comprise a sufficient therapy if a focus cannot be found. Postoperative somatostatin use may be beneficial.
Keywords: Acute chylous peritonitis, Laparoscopy, Acute abdomen
1. Introduction
Acute chylous peritonitis is defined as the onset of acute abdomen findings due to abrupt chylous fluid accumulation in the peritoneal space.1,2 A few cases have been presented in the literature. Preoperative diagnosis is difficult due to acute abdomen findings, and acute chylous peritonitis is usually confused with pathologies such as acute appendicitis, organ perforation, ovarian torsion and pelvic inflammatory disease. In this paper, we report a chylous peritonitis case that was admitted with acute abdomen findings and underwent laparoscopy because the etiology could not be fully explained. Diagnosis and treatment approaches are discussed given the current literature.
2. Presentation of case
A 32-year-old female patient (weight 64 kg, height 162 cm, and body mass index = 24.3 kg/m2) was admitted to our hospital with complaints of abdominal and low back pain and fatigue lasting for 24 h. She stated that the pain did not diminish, but increased; she felt the pain extensively and severely in all abdominal regions, mainly in the right lower quadrant. She had no history of systemic diseases, operations, or trauma. She did not have irregular or delayed menstruation. She was not using alcohol or cigarettes. Her physical examination revealed a body temperature of 37.2 °C, a pulse rate of 84/min, and a blood pressure of 110/80 mmHg. She looked pale. The abdomen was mildly distended and bowel sounds were hypoactive. There was significant tenderness and rebound, especially in the right lower quadrant. Biochemistry results were as follows: white blood cell count, 10.8 × 109/μL; hemoglobin, 10.9 g/dL; aspartate aminotransferase, 23 U/L; alanine aminotransferase, 25 U/L; urea, 18 mg/dL; creatinine, 0.7 mg/dL; sodium, 139 mmol/L; potassium, 3.8 mmol/L; beta human chorionic gonadotropin, 0.1 mL U/mL; blood amylase, 93 U/L; blood lipase, 238 U/L; urinary amylase, 107 U/L.
Thoracic and abdominal plain radiographies were featureless. Abdominal ultrasonography revealed widespread fluid, especially in the lower quadrants, and inflammation was detected in the mesenteric and perirenal fat planes. Computed tomography (CT) also revealed widespread peritoneal fluid and widespread inflammation in the mesenteric fat planes, together with retroperitoneal fluid on the right (Fig. 1). Laparoscopy was planned for the patient due to acute abdomen findings.
Fig. 1.
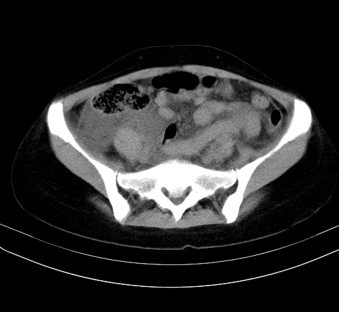
Preoperative computed tomography. Intraabdominal fluid and inflammation in intestinal mesentery.
The abdomen was accessed with a periumbilical 10 mm trocar; a milky fluid was observed, especially in the pelvis and the right side of the abdomen. This fluid extended posterior of the duodenum from the posterior side of the right colon (Fig. 2). Approximately 2 L of fluid were aspirated. Accessing the abdomen using an additional two 5 mm trocar permitted exploration of all of the abdomen, intestinal segments, pelvic organs, appendix, retroperitoneal area, the posterior side of the stomach, and the pancreas. Gastrocolic and gastrohepatic ligament were opened in order to evaluate posterior part of the stomach, pancreas and cisterna chyli localizations. Right colon was partially mobilized. No surgical pathologies that could explain the clinical condition (perforation, pancreatitis, appendicitis, gynecological pathologies, cholecystitis, ischemia findings, diverticulitis) were detected. Lymphatic drainage was not observed. Specimens were obtained for biochemical and bacterial analysis. Two active drains were placed in the pelvis and the subhepatic area, and the procedure was terminated.
Fig. 2.

A milky appearance of the fluid in laparoscopy.
The postoperative drainage amount was 300 cc on the first day, and amount that gradually decreased thereafter. One of the drainage tubes was removed on the third day, and another on the seventh day. The patient was administered somatostatin (somatosan 3 mg, CuraMED Pharma, Karlsruhe, Germany) for 5 days postoperatively. Somatostatin was administered to patient through continuous intravenous infusion at a dose of 3 mg per 12 h. The patient, who had begun to feed orally on postoperative day 2, was recommended to follow a low-fat diet for one month. The triglyceride level in the intrabdominal fluid was found as 1212 mg/dL. Growth did not occur in the bacteriology examination. Follow-up achieved with oncological markers (á-fetoprotein, carcinoembryonic antigen and carbonic anhydrase 19–9), chest X-ray and CT scan of the abdomen (6 and 9 months). No abnormalities were diagnosed. The patient was unproblematic on postoperative follow-up.
3. Discussion
Chylous fluid accumulation in the intraabdominal cavity is defined as a chylous acid; its incidence has been reported as 1/20,000 of cases who admit to the hospital. Chylous fluid accumulation is reported to arise from various etiological factors such as trauma, chronic liver diseases, tuberculosis, filariasis, radiation, abdominal aorta surgery, different peritoneal infection and extended lymph node dissections. Its incidence has been suggested to be increasing, given an increase in major surgical interventions in recent years.3 The first case in which chylous fluid appeared acutely in the absence of a definite etiological factor was presented by Murphy in 1887, and 71 total cases of acute chylous peritonitis cases were reported as of 2008.1,4 Only three cases of acute chylous peritonitis reported since 2008 appear in PubMed.
How chylous peritonitis develops acutely and spontaneously is controversial. In some patients, it was considered to arise from lymphatic fluid extravasation due to a sudden pressure increase in the lymph canals after a heavy meal. Findings were reported to appear even 2–3 days after the meal in these patients. In most cases, a pain begins suddenly as a cramp and gradually increases, becoming most prominent in the right lower quadrant and pelvis. Chylous fluid may accumulate in those areas, causing the reported pain. However, the main cause of the pain is the strain from the fluid, especially in the right retroperitoneal area and mesentery, rather than the presence of the chylous fluid per se. In most cases, the presence of tenderness and rebound leads the patients to be diagnosed with acute appendicitis.5,6 In our case, a history of a heavy meal rich from fat could not be obtained, although we questioned the patient in the postoperative period as well. The clinical findings for the reported patients are similar to those reported in the literature.
Making a diagnosis is quite hard in patients lacking etiological factors like a previous surgery or tumor. The preoperative diagnosis is usually acute appendicitis, pancreatitis, ovarian torsion, perforation, or mesenteric ischemia.5–9 Ultrasonography and computed tomography findings are not very specific, and usually include intra-abdominal fluid, mesenteric edema, and inflammation. Fluid density is not more than water density, and thus the main benefit of tomography is the ability to distinguish chylous peritonitis from other causes of acute abdomen. When a specific focus cannot be found, control tomography is recommended 3–6 months later for a specific diagnosis.10,11 Biochemical analysis of the intraabdominal fluid may be carried out, and diagnostic tools such as lymphangiography and lymphoscintigraphy may be used if chylous ascites have developed slowly and the clinical condition is not severe. A milky appearance of the fluid obtained from the abdomen and triglyceride levels 2- to 8-fold greater than plasma levels are significant diagnostic tools.3,4,12 Such a diagnosis is usually not considered in cases that develop acute abdomen findings, and therefore it is not practical to use these methods. Cytology may be used to detect malignant cells.3 Intraoperative strategy must be tried to determine in acute chylous peritonitis cases. If malignant cells are detected in cytology, etiology may be researched and treatment may be done laparoscopically, if needed. However threshold to switch to open surgery must be kept low. If a malignant focus cannot be detected in that kind of cases, another approach is performing only lymph node biopsy and exploring the focus postoperatively. Cytologic examination could not be done in our patient as she underwent an urgent surgery due to acute abdomen findings. But, no pathologies were detected on computed tomography and tumor markers obtained at the 6 and 9-month postoperative follow-up.
The most appropriate treatment for chylous peritonitis is to detect the underlying etiology and treat it. Successful results have been reported with total parenteral nutrition and somatostatin administration in the cases in which the clinical condition developed slowly.13 Laparotomy is recommended in cases who admit with acute abdomen findings, due to advantages such as making a correct diagnosis, finding the underlying cause and making a ligation of the disrupted lymphatic channel. Focus of the lymphatic leakage cannot be usually detected in acute chylous peritonitis cases. This is possible and leakage area may be sutured in very rare cases. However, laparotomy is a severe procedure given current developments in laparoscopic techniques. Laparoscopy is a widely used and recommended procedure today in acute abdomen cases and in cases in which a preoperative, specific diagnosis cannot be made. A 2011 Cochrane analysis reported that the use of laparoscopy in such cases increased specific diagnosis rates and decreased the duration of hospital stay. The use of laparoscopy has gradually increased in recent years for the treatment of many abdominal pathologies.14–16 We have liberally used laparoscopy in cases with acute abdominal pain and irritation findings when we could not make a specific diagnosis. A specific preoperative diagnosis could not be made with the reported patients; she was subjected to laparoscopy due to acute abdomen findings and to make a surgical intervention if needed. Although there are no case reports indicating that leakage area was laparoscopically found and sutured, we consider that it is possible in experienced hands.
Patients with chylous peritonitis are recommended to follow a low-fat diet for approximately one month after discharge. There is not an exact follow up period for these cases in the literature. Despite the presence of the papers reporting a 24-month follow up period, this time is 6 months in most case reports.1,2,4 Our patient was followed up for 9 months for this reason and we consider that this follow up period is sufficient to detect a malignant etiology.
4. Conclusion
In conclusion, we have presented an acute chylous peritonitis case that was admitted with acute abdomen findings and followed up and treated with laparoscopy. This case demonstrates the effectiveness of laparoscopy in acute abdomen cases in which a specific preoperative diagnosis cannot be made. All intestinal mesentery, the posterior of the stomach and the pancreas must be controlled during laparoscopy in order to find a potential source of the lymphatic leakage and to make repairs when needed. Aspiration of the fluid and drainage comprise a sufficient therapy if a focus cannot be found. Postoperative somatostatin use may be beneficial. Patients must be followed for approximately six months to detect potential etiological factors.
Conflict of interest statement
We confirm that we have no conflict of interest in relation to this work.
Funding
We confirm that we have no conflict of interest and any study sponsors in relation to this work.
Ethical approval
We confirm that written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Halil Özgüç, MD was contributed in study design, data collections, analysis, and writing of this article. Mustafa Narmanlı, MD, and Mehmet Kürşat Keskin, MD were contributed in data collections and analysis of this article.
References
- 1.Vettoretto N., Odeh M., Romessis M., Pettinato G., Taglietti L.M., Giovanett I. Acute abdomen from chylous peritonitis: a surgical diagnosis case report and literature review. European Surgical Research. 2008;41:54–57. doi: 10.1159/000129599. [DOI] [PubMed] [Google Scholar]
- 2.Mishin I., Ghidirim G., Vozian M. Acute spontaneous chylous peritonitis: report a case. Journal of Gastrointestinal and Liver Diseases. 2010;3:333–335. [PubMed] [Google Scholar]
- 3.Cardenas A., Chopra S. Chylous ascites. American Journal of Gastroenterology. 2002;97:1896–1900. doi: 10.1111/j.1572-0241.2002.05911.x. [DOI] [PubMed] [Google Scholar]
- 4.Madding G.F., Richard F., McLaughlin F., McLaughlin R.F. Acute chylous peritonitis. Annals of Surgery. 1958;147:419–422. doi: 10.1097/00000658-195803000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith E., Edmund E.K., Croagh D., Spain L.A., Farrel S. Acute chylous ascites mimicking acute appendicitis in a patient with pancreatitis. World Journal of Gastroenterology. 2009;14:4849–4852. doi: 10.3748/wjg.15.4849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang F.C., Hsu S.D., Chen C.W., Chen T.W. Spontaneous chylous peritonitis mimicking acute appendicitis: A case report and review of literature. World Journal of Gastroenterology. 2006;12:154–156. doi: 10.3748/wjg.v12.i1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Georgiou G.K., Harissis H., Mitsis M., Batsis H., Fatouros M. Acute chylous peritonitis due to acute pancreatitis. World Journal of Gastroenterology. 2012;18:1987–1990. doi: 10.3748/wjg.v18.i16.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adas G., Karatepe O., Battal M., Dogan Y., Karyagar S., Kutlu A. Coughing may lead to spontaneous chylothorax and chylous ascites. Case Reports in Gastrroenterology. 2007;1:178–183. doi: 10.1159/000108950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazili F.M., Khawaja F.I. Acute chylous peritonitis simulating acute appendicitis: a case report and review of the literature. Annals of Saudi Medicine. 1999;19:236–238. doi: 10.5144/0256-4947.1999.236. [DOI] [PubMed] [Google Scholar]
- 10.Hibbeln J.F., Wehmueller M.D., Wilbur A.C. Chylous ascites: CT and ultrasound appearance. Abdominal Imaging. 1995;20:138–140. doi: 10.1007/BF00201522. [DOI] [PubMed] [Google Scholar]
- 11.Wachsberg R.H., Kohnoe S., Takahashi I. Chyloperitoneum: CT diagnosis. Clinical Imaging. 1994;18:273–274. doi: 10.1016/0899-7071(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 12.Kohnoe S., Takahashi I., Kawanaka H., Mori M., Okadome K., Sugimachi K. Combination of preoperative lymphangiography using lipiodol and intraoperative lymphangiography using Evans Blue facilitates the accurate identification of postoperative chylous fistula. Surgery Today. 1993;23:929–931. doi: 10.1007/BF00311375. [DOI] [PubMed] [Google Scholar]
- 13.Huang Q., Jiang Z.W., Jiang J., Li N., Li J.S. Chylous ascites: treated with total parenteral nutrition and somatostatin. World Journal of Gastroenterology. 2004;10:2588–2591. doi: 10.3748/wjg.v10.i17.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanna A., Adani G.L., Anania G., Donini A. The role of laparoscopy in patients with suspected peritonitis: experience of a single institution. Journal of Laparoendoscopic and Advanced Surgical Techniques Part A. 2003;13:17–19. doi: 10.1089/109264203321235412. [DOI] [PubMed] [Google Scholar]
- 15.Gaitan H.G., Reveiz L., Farquhar C. Laparoscopy for the management of acute lower abdominal pain in women of childbearing age. Cochrane Database of Systemic Reviews. 2011;19:CD007683. doi: 10.1002/14651858.CD007683.pub2. Review. [DOI] [PubMed] [Google Scholar]
- 16.Dominquez L.C., Sanabria A., Vega V., Osorio C. Early laparoscopy for the evaluation of nonspecific abdominal pain: a critical appraisal of the evidence. Surgical Endoscopy. 2011;25:10–18. doi: 10.1007/s00464-010-1145-4. [DOI] [PubMed] [Google Scholar]


