Abstract
Background
Bile duct injury is a rare complication of cholecystectomy. The aims of this study were to analyse the mechanism and outcome of biliary complications and determine the Northern Ireland incidence of bile duct injury over the last decade.
Methods
Annual numbers of cholecystectomies were obtained from the Northern Ireland Hospital Inpatient System database. Bile duct injury referrals to a hepatobililary unit over an 11-year period from 2000 were reviewed. Mechanism and recognition of injury, referral interval, management and outcome were analysed.
Results
The annual incidence of laparoscopic cholecystectomy in Northern Ireland increased from 0.038% in 1995 to 0.101% in 2009. Thirty-five patients with biliary complications from cholecystectomy were referred from 2000. The incidence of bile duct injury associated with laparoscopic cholecystectomy during this period was 0.2%. Only 26% of injuries were recognised intra-operatively, only 40% were referred immediately and 91% required operative intervention.
Conclusion
The incidence of laparoscopic cholecystectomy has increased in Northern Ireland. The incidence of bile duct injuries over the last 11 years was 0.2%. Recognition and referral were delayed in most cases. The majority of injuries required operative management and long-term follow-up.
Keywords: Bile duct injury, Cholecystectomy, Laparoscopic Cholecystectomy
INTRODUCTION
Bile duct injury during cholecystectomy is an iatrogenic catastrophe associated with significant morbidity, mortality, adverse quality of life and high rates of litigation1. Laparoscopic cholecystectomy is now considered the gold standard treatment for symptomatic gallstones. Higher rates of bile duct injury have been reported in the laparoscopic era2.
The aims of this study were to determine the incidence of biliary complications following cholecystectomy in Northern Ireland and review the mechanism, recognition, referral, management and outcome of biliary injuries.
PATIENTS AND METHODS
Population-based information was collected from the “Hospital Inpatient System” (HIS) in Northern Ireland to determine the annual incidence of benign biliary surgical practice since records commenced in the province in 1995. Northern Ireland has a relatively stable population and a single Hepatobiliary unit. Patients referred to this unit for the management of bile duct injuries sustained at cholecystectomy during the last 11 years were identified and their case notes reviewed.
The mechanism and recognition of injury, referral interval, management and outcome were analysed. The calculation of the incidence of bile duct injury was made based on the total number of bile duct injury referrals to the Hepatobiliary unit and the total number of laparoscopic cholecystectomies carried out in Northern Ireland over this period.
RESULTS
Incidence of cholecystectomy & biliary complications
The population of Northern Ireland increased by approximately 6% during the last decade. The annual incidence of laparoscopic cholecystectomy almost trebled from 0.038% in 1995 to 0.101% in 2009. Open cholecystectomy rates have remained relatively stable (figure 1).
Fig 1.
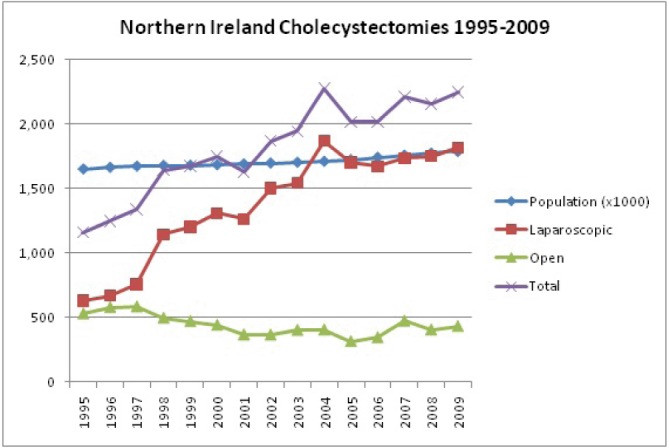
Annual numbers of cholecystectomies in Northern Ireland 1995-2009
Over an 11-year period from 2000, 35 patients with bile duct injuries sustained during cholecystectomy were referred. There were 21 female and 14 male patients with a mean age of 51.1 years (range 19-81 years, median 51 years). Injuries were classified according to the Strasberg et al method3 (table 1).
TABLE 1.
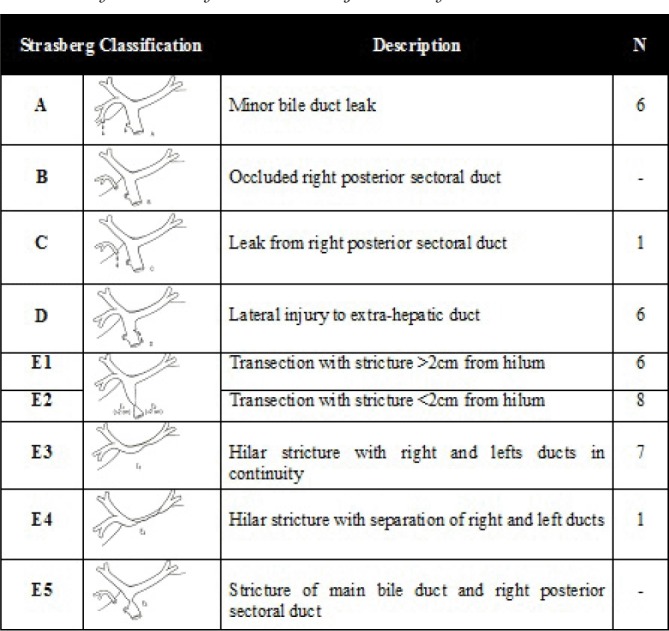
Classification of bile duct injuries referred 2000–2010
The incidence of bile duct injury associated with laparoscopic cholecystectomy was 0.2%.
Surgery, recognition and time of referral
Twenty-eight injuries were sustained during laparoscopic cholecystectomy (of which 8 were recognised and converted to open). One injury was sustained after open conversion and was recognised intra-operatively. A further 4 patients had laparoscopic converted to open cholecystectomy but the injury was not recognised until the post-operative period. Two injuries were sustained at open cholecystectomy – both of which were recognised post-operatively. A consultant surgeon was the principal operator in all but one case.
Only 9 injuries were recognised at the time of surgery, 1 of which was diagnosed on cholangiography – the only intra-operative cholangiogram performed in this series. Fourteen cases were referred immediately (within 7 days of injury). Thirteen cases were ‘early’ referrals (within 6 weeks) and the remaining 8 injuries were considered ‘late’ referrals (after 6 weeks).
PRESENTATION, MANAGEMENT & OUTCOME
Type A - 6 patients
Four patients had a cystic duct stump leak (without distal bile duct obstruction) (figure 2). Two patients had leaks from a minor radical duct in the gallbladder fossa. One patient presented with abdominal pain after 2 weeks and had percutaneous drainage of a bile collection with no persistent leak on follow-up MRCP. Five presented with biliary peritonitis in the early post-operative period and 1 was also jaundiced. Laparotomy and placement of drains were performed in 5 cases. Oversewing of a leaking radical duct was carried out in 1 patient. In 1 case, laparotomy was eventually performed after unsuccessful laparoscopic drainage and ERCP. One patient required ERCP and stenting after open drainage. All patients made a good recovery, remaining asymptomatic with normal liver function tests during follow-up periods ranging from 6 weeks to 36 months.
Fig 2.
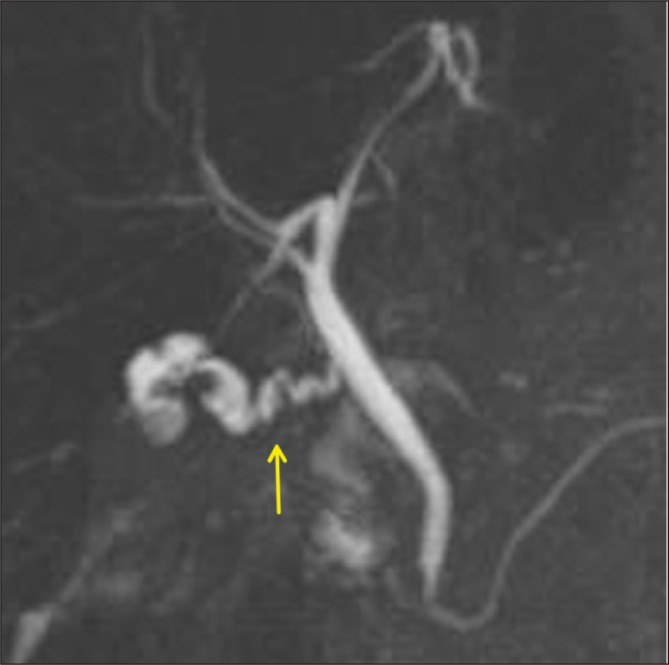
MRCP demonstrating a Type A cystic duct leak
Type B
There were no Type B injuries.
Type C – 1 patient
This patient presented 3 weeks post-operatively with a biliary leak and jaundice. ERCP showed leak of contrast with no filling of the right intrahepatic ducts. A stent was placed and removed 1 year later. Follow-up MRCP suggested a persistent bile leak and less prominent right intrahepatic ducts. On referral to the Hepatobiliary unit, management was conservative as the patient was asymptomatic with normal liver function tests. He remains well at 3 years.
Type D – 6 patients
One Type D injury was recognised intra-operatively and after open conversion a T-tube and large drain were inserted. A further laparotomy with T-tube replacement and drainage was performed due to biliary peritonitis. Although MRCP at 8 months showed a slight kink in the hepatic duct there were no symptoms or biliary obstruction and liver function tests were normal.
One patient presented post-operatively with a significant bile leak from the drain and was successfully treated with ERCP and stenting. The other 4 patients, 1 of whom was also jaundiced, presented with biliary peritonitis. Of these, 2 had failed endoscopic stenting and all 4 required laparotomy. One patient had a choledochojejunostomy performed at 9 days by the primary surgeon. This was revised after 2 weeks before referral to the Hepatobiliary unit where she was treated conservatively for a persistent bile leak and sepsis. Two patients had T-tube insertion and 1 injury was suture repaired. Follow-up ranged from 2-8 years. Three patients complained of persistent pain during follow-up but liver function tests in all cases were satisfactory.
Type E – 22 patients
Eight type E injuries were recognised intra-operatively - 1 occurring after conversion to open. Four had primary suture repair over a T-tube by the initial surgeon. One of these required a hepaticojejunostomy after 1 year for a Bismuth type 3 stricture. One patient developed a stricture at 1 year requiring hepaticojejunostomy at 5 years. Both remain well after 7 and 3 year follow-up respectively. The other 2 patients are well with no stricture at 2 and 4 years.
The other 4 recognised injuries were referred for immediate hepaticojejunostomy. Three of these patients also had associated vascular injuries to the right hepatic artery. Two of these were well with normal liver function after 2 years. The other patient (who also had repair of a transected right hepatic artery) had mild derangement of liver function but remains asymptomatic after 2 years.
Eleven type E injuries presented in the early post-operative period (figure 3). Eight patients presented with biliary peritonitis of which 2 were also jaundiced. The other 3 presented with painless jaundice. Four were referred immediately, 4 early and 3 were considered late referrals. All required hepaticojejunostomy. One had a hepaticojejunostomy performed by the primary surgeon which strictured after 3 years requiring revision. One patient also had an injury to the right hepatic artery and developed hepatic necrosis, anastomotic stricturing, cirrhosis and ultimately required a right hepatectomy. One patient has been treated conservatively for intermittent cholangitis since surgery. The remaining 9 patients are well with normal liver function during follow-up periods ranging from 2 months to 9 years.
Fig 3.
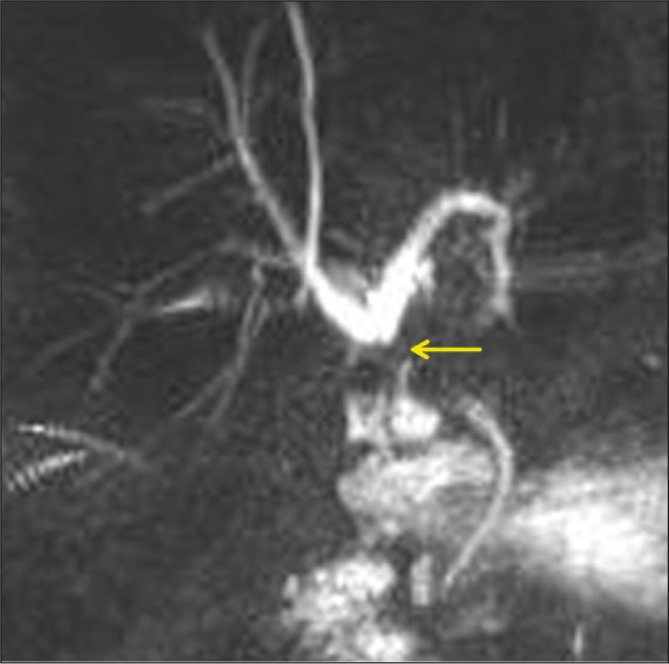
MRCP demonstrating a Type E3 injury. This required hepaticojejunostomy.
The remaining 3 injuries presented with jaundice/cholangitis later in the follow-up period. All were found to have a stricture on ERCP, requiring stenting. One required hepaticojejunostomy 10 years after cholecystectomy and is well with normal LFTS. Another had hepaticojejunostomy performed after 1 year and is well after 1 year follow-up. The remaining patient has not required operative intervention after 5 years of follow-up.
Hepaticojejunostomy (Blumgart technique) was performed in patients requiring biliary reconstruction4. A retrocolic Roux-en-Y jejunal loop was anastomosed to the bile duct confluence after extending the left hepatic duct opening to maximise the anastomotic circumference. One patient also required re-implantation of the right posterior sectoral duct.
DISCUSSION
The rate of cholecystectomy continues to rise since the introduction of the laparoscopic approach. The incidence of bile duct injury associated with laparoscopic cholecystectomy in Northern Ireland over the last decade was 0.2% - lower than reported rates of 0.4-0.7%2.
Calculation of the incidence of biliary injury was based on the assumption that all patients were referred to the Hepatobiliary unit. Whilst it is likely that all major injuries were referred it must be recognised that further complications such as minor Type A leaks may have been managed at the primary hospital without referral to the Hepatobiliary unit.
There were 32 injuries referred to this unit during a previous 7-year study period (1992-1998)5. Considering the steadily increasing number of cholecystectomies rate over the last decade, this may suggest that the overall biliary complication rate has reduced. However a direct comparison of incidence could not be made due to incomplete cholecystectomy data for the previous period.
It has been reported that only 25-32.4% of bile duct injuries are recognised at the index surgery2. Our data is consistent with this but, significantly, only 26% of injuries were recognised at cholecystectomy compared with 41% in the previous series. Of the more severe Type D and E injuries, only 1 (17%) and 8 (36%) were recognised respectively which again is less than previously (78% and 50% respectively). Only 14 (40%) injuries were referred immediately. Twelve (37%) were ‘early’ and 8 (23%) ‘late’ referrals. The decreased recognition rate may have implications regarding timeliness of referral and therefore outcome. It is well recognised that immediate recognition, hepatobiliary referral and repair are associated with improved outcomes1, 2, 6.
Biliary complications range from minor ductal leaks, often managed non-operatively, to proximal transectional injuries requiring major biliary and occasionally vascular reconstruction. Several classification methods have been proposed but the Strasberg method remains the most commonly used1, 2, 6, 7. Type E injuries involve the common hepatic/bile duct and are considered more severe, usually necessitating hepaticojejunostomy with increased morbidity and mortality. There were 22 Type E injuries during this study period compared with 10 between 1992-1998. Furthermore, there were 8 severe proximal injuries (Type E3/E4) involving the hilar confluence and 4 injuries involving transection of the right hepatic artery8. Concomitant right hepatic artery injury occurs more often with severe proximal biliary injury and is associated with increased morbidity including hepatic ischaemia and right hemihepatectomy9.
Only 3 patients (9%) were managed without open surgery. Of 11 patients who had a laparotomy prior to referral, 7 required a further open procedure including 1 patient who had revision of a hepaticojejunostomy. Twenty-one (95%) of the Type E injuries required hepaticojejunostomy, one of whom later developed hepatic necrosis necessitating a right hepatectomy. All are committed to a minimum of 10 years of follow-up to exclude late stricturing and cirrhosis10,11. This emphasises the considerable morbidity associated with bile duct injury. There were no mortalities in this series.
Bile duct injury should be regarded as preventable. The commonest cause of injury is mis-identification of biliary anatomy. Preventative techniques include correct anatomical orientation with dissection lateral to the ‘line of safety’, identification of the ‘safety zone’, ‘critical view of safety’, and cross-checking3,12–14.
If dissection and orientation are difficult, early open conversion is recommended though it is worth noting that there were 3 open injuries in this series – one of which occurred after conversion. If excessive inflammation and fusion of the tissue planes are encountered, safety strategies such as partial cholecystectomy or cholecystostomy should be utilised.
Patients presenting in the early post-cholecystectomy period with biliary leak, peritonitis and/or jaundice should be considered to have sustained a biliary injury. Delay in diagnosis is associated with increased morbidity. Once diagnosed, resuscitation, external drainage and control of sepsis should be established. The patient should be immediately referred to a hepatobiliary surgeon for further management as early repair is associated with lower morbidity and mortality, shorter duration of treatment and improved quality of life15–18. Inadequate and delayed management may lead to severe complications including sespis and multi-organ failure in the acute phase or late biliary stricture and cirrhosis.
CONCLUSION
The incidence of biliary injury following laparoscopic cholecystectomy in Northern Ireland over the last 11 years was low – 0.2%. However, there were delays in the recognition and referral of most injuries and the majority required further operative management. Careful anatomical orientation, cross-checking and dissection are recommended to prevent such injuries. Prompt hepatobiliary referral should be sought upon recognition.
Acknowledgments
The authors acknowledge Dr Sharon Jamison, Hospital Statistician, Northern Ireland Department of Health for the provision of cholecystectomy data.
The authors have no conflict of interest.
REFERENCES
- 1.Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93(2):158–68. doi: 10.1002/bjs.5266. [DOI] [PubMed] [Google Scholar]
- 2.Lau WY, Lai EC, Lau SH. Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg. 2010;80((1-2)):75–81. doi: 10.1111/j.1445-2197.2009.05205.x. [DOI] [PubMed] [Google Scholar]
- 3.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101–25. [PubMed] [Google Scholar]
- 4.Blumgart LH, Bauer HU. Surgery of the Liver and Biliary Tract. Edinburgh: Churchill Livingstone; 1994. Hilar and intrahepatic biliary-enteric anastomosis. In: Blumgart LH, editor; pp. 1051–67. [Google Scholar]
- 5.Bingham J, McKie LD, McLoughlin J, Diamond T. Biliary complications associated with laparoscopic cholecystectomy – an analysis of common misconceptions. Ulster Med J. 2000;69(2):106–11. [PMC free article] [PubMed] [Google Scholar]
- 6.Jablonska B, Lampe P. Iatrogenic bile duct injuries: Etiology, diagnosis and management. World J Gastroenterol. 2009;15(33):4097–104. doi: 10.3748/wjg.15.4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lau WY, Lai EC. Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int. 2007;6(5):459–63. [PubMed] [Google Scholar]
- 8.Davidoff AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD, Baker ME, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215(3):196–202. doi: 10.1097/00000658-199203000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li F, Frilling A, Nadalin S, Paul A, Malago M, Broelsch CE. Management of concomitant hepatic artery injury in patients with iatrogenic major bile duct injury after laparoscopic cholecystectomy. Br J Surg. 2008;95(4):460–5. doi: 10.1002/bjs.6022. [DOI] [PubMed] [Google Scholar]
- 10.Bottger T, Junginger T. Long-term results after surgical treatment of iatrogenic injury of the bile ducts. Eur J Surg. 1991;157(8):477–80. [PubMed] [Google Scholar]
- 11.Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A. The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg. 1996;224((2)):162–7. doi: 10.1097/00000658-199608000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diamond T, Mole DJ. Anatomical orientation and cross-checking – the key to safer laparoscopic cholecystectomy. Br J Surg. 2005;92((6)):663–64. doi: 10.1002/bjs.4992. [DOI] [PubMed] [Google Scholar]
- 13.Taniguchi Y, Ido K, Kimura K, Yoshida Y, Ohtani M, Kawamoto C, et al. Introduction of a ‘safety zone’ for the safety of laparoscopic cholecystectomy. Am J Gastroenterol. 1993;88(8):1258–61. [PubMed] [Google Scholar]
- 14.Strasberg SM, Brunt LM. Rationale and Use of the Critical View of Safety in Laparoscopic Cholecystectomy. J Am Coll Surg. 2010;211(1):132–8. doi: 10.1016/j.jamcollsurg.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 15.Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289(13):1639–44. doi: 10.1001/jama.289.13.1639. [DOI] [PubMed] [Google Scholar]
- 16.Stewart L, Way LW. Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the result of treatment. Arch Surg. 1995;130((10)):1123–1128. doi: 10.1001/archsurg.1995.01430100101019. [DOI] [PubMed] [Google Scholar]
- 17.Thomson BN, Parks RW, Madhavan KK, Wigmore SJ, Garden OJ. Early specialist repair of biliary injury. Br J Surg. 2006;93(2):216–20. doi: 10.1002/bjs.5194. [DOI] [PubMed] [Google Scholar]
- 18.Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290(16):2168–73. doi: 10.1001/jama.290.16.2168. [DOI] [PubMed] [Google Scholar]


