Abstract
The transition from medical student to junior doctor is well recognised to be a difficult and stressful period. To ease this transition, most UK universities have a work-shadowing period (WSP), during which students can learn practical skills needed for forthcoming employment. The aim of this study was to evaluate the WSP at Queen’s University Belfast, and gain the views of both students and Foundation Programme Supervisors and Directors (FPSDs). The study utilised both qualitative (focus groups) and quantitative (questionnaires) approaches. The FPSDs completed a specific questionnaire designed for this study, while the students completed the university’s internal quality assurance questionnaire. Twenty-eight of the 37 (76%) FPSDs and 106 / 196 (54%) students completed the questionnaires. Focus groups were conducted with up to 10 students in each group in both a regional centre and a district general hospital at the start and the end of the WSP as well as 8 weeks into working life. The transcripts of the focus groups were analysed and themes identified. A number of deficiencies with the current WSP were identified, including concerns about the use of log books, the timing of the attachment and relatively low levels of supervision provided by senior hospital staff members. As a result, students felt unprepared for commencing work, with particular mention given to medical emergencies, prescribing, and the emotional aspects of the job. A number of recommendations are made, including the need for more senior input to ensure better student attendance, participation and clinical interaction. Furthermore, students should be offered additional supervised responsibility for delivery of patient care and more experiential learning with respect to drug prescribing and administration. The study also suggests that more needs to be done to help ease the emotional and psychological stresses of the early FY1 period. These issues have been resolved to a large extent with the introduction of the new final year Student Assistantship module in the academic year 2010-2011.
INTRODUCTION
One of the major aims of medical school is to lay the educational foundations for a lifelong career and equip junior doctors for the first stage in their working lives1. However, concern exists that the transition from student to doctor is too abrupt and, thus, is a cause of great stress,2, 3. In order to help bridge this gap, most medical schools in the United Kingdom (UK) incorporate a work-shadowing period (WSP), when final year students can spend time with existing junior doctors4. However, there is no set defined duration or timing for the period and, as such, it varies across medical schools.
New graduates have reported that they feel under-prepared and inadequately equipped for work life5, and this has resulted in some medical students requesting further training6. As such, there remains a significant gap between undergraduate training and what is required of the newly qualified doctor2. Nonetheless, despite the obvious importance attached to this period of training, there has been concern about student engagement with work-shadowing attachments7. The importance of work-shadowing and student assistantships are highlighted in the latest edition of Tomorrow’s Doctors8.
The aim of this study was to evaluate the work-shadowing attachment at Queen’s University Belfast (QUB) by gaining the views of both Foundation Programme Supervisors and Directors (FPSDs) and final year students at the time of their transition to the Foundation Programme.
METHODS
Approval for the study was obtained from the Research Ethics Committee of the School of Medicine, Dentistry and Biomedical Sciences, QUB.
At QUB, all final year students complete a 4-week work-shadowing attachment during the month of May and after completion of the final year clinical examinations (Figure 1). During this time, students are generally assigned to the hospital where they will be employed as FY1 trainees and are expected to ‘shadow’ the existing FY1 trainees in order to gain the necessary experience to ease the transition from medical student to practising doctor. The students are assessed by means of a logbook, which contains a range of clinically relevant tasks and procedures commonly undertaken by FY1 trainees.
Fig 1.
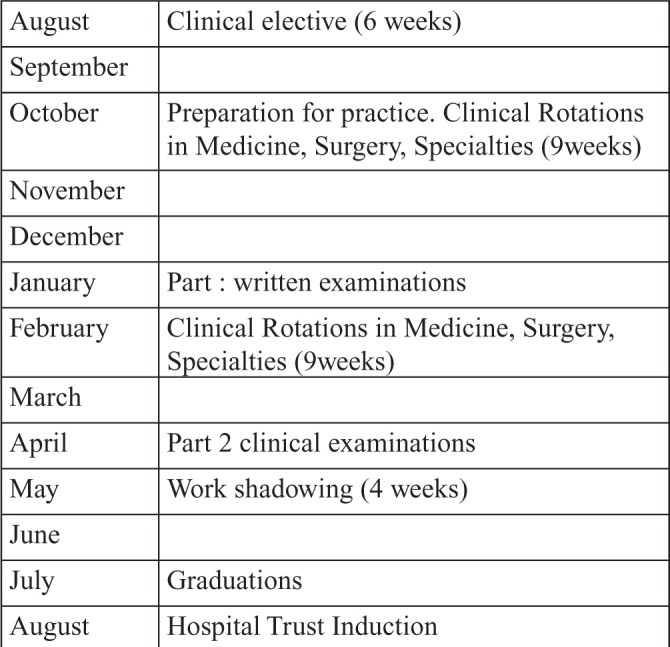
Structure of Final Year.
This study utilised both qualitative (focus groups) and quantitative (questionnaires) methodologies and was carried out during the academic year 2007-2008. Two questionnaires were used in this study. The first was the standard QUB WSP evaluation questionnaire, which was issued to all students at the end of the attachment. The second was sent to all FPSDs who were working in the hospitals in Northern Ireland on behalf of the Northern Ireland Medical and Dental Training Agency. Both questionnaires utilised a Likert scale, ranging from ‘strongly agree’ to ‘strongly disagree’, as well as open-ended questions.
Focus group sessions with the medical students / trainees were undertaken on three occasions: at the start of the WSP, at the end of the WSP and then eight weeks into the FY1 year. Two groups of selected trainees (n=10), who were assigned either to a district general hospital or a large teaching hospital, agreed to participate. In total, therefore, there were six focus groups. Each focus group discussion was recorded and transcribed. These transcripts were then screened to assess for trends and themes, which were believed to be representative of the sample populations. This was achieved with the help of a qualitative data analysis software programme (NVivo qualitative data analysis software; QSR International Pty Ltd. Version 8, 2008), which helped to identify trends and code passages of the transcript into different categories.
RESULTS
Foundation Programme Supervisors and Directors’ (FPSD) questionnaire
Twenty-eight of the thirty-seven (76%) FPSDs replied to the questionnaire. The responses to the Likert scale questions are summarised in Tables 1a and 1b. Table 1a contains the questions that dealt specifically with the students - there was strong agreement that the WSP benefited the students in terms of skills and helped them to acclimatise to working life. Data relating to wider issues, including assessment, hospital Trust responsibility, and timing of the attachment and induction, are summarised in Table 1b. Overall, there were strong beliefs expressed that the logbook was not an acceptable form of assessment.
Table 1a.
Results obtained from the FPSDs questionnaire from questions specifically about the students.
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| Students find the work shadowing period a useful experience | 39.3% (11) | 50.0% (14) | 10.7% (3) | 0.0% (0) | 0.0% (0) |
| Students need the work shadowing period to acclimatise to the work environment | 71.4% (20) | 21.4% (6) | 3.6% (1) | 3.6% (1) | 0.0% (0) |
| Students make the most of the work shadowing period | 17.9% (5) | 28.6% (8) | 28.6% (8) | 25.0% (7) | 0.0% (0) |
| Students should be employed and paid for the work shadowing period | 10.7% (3) | 3.6% (1) | 25.0% (7) | 35.7% (10) | 25.0% (7) |
| During the work shadowing period students integrate into the ward | 28.6% (8) | 32.1% (9) | 28.6% (8) | 10.7% (3) | 0.0% (0) |
| Student attendance is good during the work shadowing period | 28.6% (8) | 53.6% (15) | 14.3% (4) | 3.6% (1) | 0.0% (0) |
| The learning outcomes for the work shadowing period are usually met by all students | 14.3% (4) | 42.9% (12) | 39.3% (11) | 0.0% (0) | 3.6% (1) |
| During the work shadowing period students improve their communication skills | 17.9% (5) | 21.4% (6) | 46.4% (13) | 14.3% (4) | 0.0% (0) |
| During the work shadowing period students improve their clinical skills | 21.4% (6) | 35.7% (10) | 32.1% (9) | 10.7% (3) | 0.0% (0) |
| During the work shadowing period students improve their practical skills | 21.4% (6) | 53.6% (15) | 17.9% (5) | 7.1% (2) | 0.0% (0) |
| Students deserve a ‘relaxed’ period so soon after the final MB examinations | 3.6% (1) | 21.4% (6) | 25.0% (7) | 46.4% (13) | 3.6% (1) |
Table 1B.
Results obtained from the FPSDs questionnaire from questions about assessments, trust responsibility, timing of the attachment and induction.
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| There are no problems with the current work shadowing period system | 10.7% (3) | 21.4% (6) | 32.1% (9) | 32.1% (9) | 3.6% (1) |
| The timing of the work shadowing period is appropriate | 14.3% (4) | 71.4% (20) | 3.6% (1) | 7.1% (2) | 3.6% (1) |
| During the work shadowing period, the students should no longer be the responsibility of the university and should now be accountable to the health trust / hospital | 7.1% (2) | 14.3% (4) | 7.1% (2) | 46.4% (13) | 25.0% (7) |
| The work shadowing period should occur simultaneously with the hospital induction | 21.4% (6) | 10.7% (3) | 14.3% (4) | 35.7% (10) | 17.9% (5) |
| Adequate supervision is given to students during the work shadowing period | 10.7% (3) | 46.4% (13) | 25.0% (7) | 14.3% (4) | 3.6% (1) |
| The duration of the work shadowing period is appropriate | 10.7% (3) | 60.7% (17) | 21.4% (6) | 7.1% (2) | 0.0% (0) |
| The log book adequately evaluates the student’s performance during the work shadowing period | 3.6% (1) | 17.9% (5) | 39.3% (11) | 39.3% (11) | 0.0% (0) |
| Once the log book is completed students have shown the competencies needed to be an F1 doctor | 3.6% (1) | 7.1% (2) | 17.9% (5) | 60.7% (17) | 10.7% (3) |
| The log book is the best way to formally assess students during the work shadowing period | 3.6% (1) | 14.3% (4) | 32.1% (9) | 50.0% (14) | 0.0% (0) |
| The log book alters the focus of the students from learning to gaining signatures | 14.3% (4) | 60.7% (17) | 14.3% (4) | 10.7% (3) | 0.0% (0) |
| The signatures in the log book gained by the students indicate that the students have genuinely completed/performed the task which has been signed off | 7.1% (2) | 14.3% (4) | 35.7% (10) | 42.9% (12) | 0.0% (0) |
| The completion of a log book could occur in significantly less time than the actual work shadowing period | 3.6% (1) | 57.1% (16) | 21.4% (6) | 17.9% (5) | 0.0% (0) |
The views of the FPSDs were also sought on several issues, including student attendance and the use of logbooks, using open-ended questions. The respondents recognised that student attendance was variable, in part due to the timing of the attachment. Some FPSDs felt that the WSP should be undertaken just prior to commencement of employment, and they emphasised the importance of student integration into the workplace-based clinical teams. Whilst some FPSDs felt that the logbooks encouraged students to document events and recognise learning outcomes, many felt that the logbooks did not accurately mirror the work that the students had completed, as the logbooks did not take account of the number of tasks or, indeed, the quality of the work performed. Some FPSDs believed that obtaining signatures in the logbook, rather than acquiring competence in the necessary skills, became the students’ focus. Alternatives, including use of workplace-based assessments, were suggested by some of the FPSDs.
Students’ Questionnaire
There were 106 (54%) questionnaires returned by the 196 students who completed the WSP in May 2008. The results are summarised in Table 2. Overall, the students reported that they found it a useful experience and that supervision was acceptable for ward-based tasks.
Table 2.
Results of the Students’ Questionnaire.
| Strongly Agree | Agreed | No strong views | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| I found the workshadowing a useful experience. | 39% | 58% | 2% | 1% | 0% |
| The programme was well organised. | 22% | 58% | 15% | 5% | 0% |
| I was allowed to undertake common administrative ward tasks under supervision. | 39% | 60% | 0% | 1% | 0% |
| I was able to understand the documentation of patient records and hospital request forms. | 37% | 62% | 1% | 0% | 0% |
| I was able to improve my communication skills within the hospital environment. | 27% | 58% | 15% | 0% | 0% |
| I was able to undertake commonly performed practical procedures under supervision. | 36% | 62% | 1% | 1% | 0% |
| I was able to keep an accurate log of the tasks and practical procedures undertaken. | 29% | 64% | 7% | 0% | 0% |
| I was able to practice my clinical skills and gain clinical experience. | 31% | 58% | 8% | 3% | 0% |
| There was sufficient time available to complete the programme. | 39% | 56% | 4% | 1% | 0% |
| I completed all the tasks commonly performed by an F1 doctor. | 27% | 59% | 9% | 3% | 2% |
| I found the ward staff co-operative while I was completing this programme. | 39% | 57% | 4% | 0% | 0% |
| The learning outcomes were stated clearly. | 28% | 60% | 8% | 4% | 0% |
| The learning outcomes were met. | 26% | 66% | 8% | 0% | 0% |
Results from the focus groups
The six transcripts were analysed and the following themes emerged.
1.What students expected to gain from their WSP and what they actually gained
In the first set of focus groups, the participants’ ideas about what they expected to achieve from the attachment focused mainly on gaining confidence and skills in procedures. Most students, however, were not so confident that the completion of the work-shadowing objectives would make them ready for commencing work as a FY1 in August. In the second set of focus groups there were mixed reactions from the students about how prepared they were for work following the WSP. Most students enjoyed the attachment, and recognised that they were better prepared for starting work as a result of it, but overall still felt nervous about the prospect of starting working in August. In the third set of focus groups most respondents believed that there had still been too big a bridge between being a student and working life.
2.Discussion around attendance and timing of the WSP
At the first focus group students showed optimism regarding their potential attendance during the forthcoming WSP. They appeared keen to engage with the learning opportunities on offer, and seemed to view it as a way of easing fears about their future employment. However, a minority of the students seemed not so keen to attend, foreseeing the closeness of the WSP to their recent final examinations and the lack of examination results as potential mental barriers. In the second focus group the students admitted that attendance was incomplete, particularly during the final two weeks. In the third focus group the trainees felt that it would have been more beneficial if they had been encouraged to participate in more ‘out-of-hours’ work. Students also suggested that the current system could be improved by having a shorter and more intense WSP, which was closer to the actual date of commencing work, with more consultant input and more responsibility for patient care.
3.Logbooks
Most students did not value the use of the logbooks, stating that having to complete the book highlighted the fact that they were still students and, as such, it was demotivating. Also despite full attendance and hard work, a student could still have an incomplete log book, giving the impression of poor attendance or, indeed, lack of effort. Alternative suggestions to the log books included having consultants giving a pass/fail mark or shadowing the FY1 all day and then completing a diary which the FY1 could sign off at the end of each day.
4.Interaction with staff
The students were generally happy with the interaction with the ward staff. In particular, the FY1 trainees and nursing staff were regarded as very helpful. The students were satisfied with the supervision at ward level when performing individual tasks. However, they felt that, due to limited senior doctor input at ward level, there was a lack of direction about their role on the ward.
5.Other Issues
Several students felt that the WSP did not help them to deal with the emotional aspects of the job, although they seemed to accept that this was something that could be learned through working on the job. A further problem mentioned by the students was the lack of experience in drug prescribing.
DISCUSSION
This study has highlighted a number of themes in relation to work-shadowing, both of a positive and negative nature.
Preparation
The importance of the WSP, in relation to acclimatisation to the work environment and improving students’ skills, was stressed by both the students and the FPSDs. The focus groups highlighted some specific areas in which the students did not feel prepared, which is in keeping with previous work1, 2. Management of emergencies was one such situation and previous work has reported that increased exposure to emergencies in undergraduate years could reduce such apprehension9.
Several students also felt that they were not emotionally well enough prepared for many aspects of the job. Emotional distress in the transition period is associated with higher levels of depression and anxiety3 and personal life problems10. Consequently, it is important that medical schools recognise the emotional problems associated with starting life as a junior doctor and attempt to address these issues.
A further concern raised by the students was their perceived lack of responsibility for patient management, despite reported benefits from student involvement in patients’ care11. This lack of accountability to the patients further inhibited the students’ attendance and participation by creating a mentality of ‘if I am not involved I will not be missed.’ Furthermore, students with reduced responsibility and accountability are more prone to unprofessionalism and medical error and, as such, it is important that medical students are accepted as junior colleagues and are given some responsibilities, albeit recognising that patient safety is paramount8,12.
A lack of confidence in drug prescribing was mentioned by the students. Every day in a ‘typical’ NHS hospital approximately 7,000 individual drug doses are administered, of which 70% are prescribed by first year graduates and senior house officers, despite having little experience of such responsibility prior to graduation13. Furthermore, less than a third of recent graduates felt adequately prepared to prescribe, with many others feeling insecure in providing enough information about treatments to guide patients to make informed decisions14. Illing and colleagues15, in their review of how well prepared medical graduates are to practise, highlighted that there were gaps in their knowledge in relation to prescribing and calculating dosage, and indeed, pharmacology in general.
Attendance and supervision
Most students reported that they had received adequate supervision when performing practical procedures and common administrative ward tasks. The importance of appropriate supervision is not only beneficial for the students’ learning and comfort, but can have positive effects on patient outcome16. However, the focus groups provided more in-depth analysis, with students stating that they would have appreciated more consultant input. The effectiveness of clinical teachers is related to their skills and knowledge17. Interestingly only 57 per cent of FPSDs agreed that adequate supervision was given to students during the work shadowing period. However, the students in this study are not alone in requesting more senior input, with house officers, senior house officers and registrars expressing similar views18,19. The students in the focus groups cited the lack of senior input as having a negative effect on attendance. Indeed, students are often demotivated by the perception that seniors have a low level of commitment to supervision20. The main complaint from the focus groups in relation to supervision seemed to be the lack of direction in terms of whom to shadow. The implementation of the European Working Time Directive has led to the development of complex rotas for junior doctors and introduction of ‘Hospital at Night’ teams. Assignment to these teams may facilitate more active participation by the work-shadowing students and more access to management of emergency situations.
Timing and duration of attachment
The FPSDs were in general agreement that the timing was appropriate. However, the focus group participants had different opinions, citing that they were distracted by just finishing examinations and not having the results, making it difficult for them to put the importance of the attachment into context. The students thought that the optimal timing for the attachment was just before starting work, as they believed this would promote greater retention of knowledge and attendance. However, it is important to recognise that at this stage the students would have already graduated from the university. In addition, with the current system, if a student has not successfully completed the WSP in May, he/she has an opportunity to undertake a further attachment during the month of June.
The students were specifically asked in the focus groups what they thought about the duration of the attachment and most expressed the view that it was too long. This is in direct contrast to the views of the majority of FPSDs who believed that the duration of the attachment was appropriate.
Logbooks
The evidence obtained from this study suggests that both the students and the FPSDs feel that the logbook has major flaws. A supervisor’s signature in the logbook may not be an accurate reflection of a student’s competency in that task21. It has been suggested that the completion of logbooks does not impact on learning as it may encourage students to do what is necessary to complete their training rather than collecting information in a way that might be useful for their future career22. As such, it is unrealistic to accept the conventional logbook as the principal and only measure of procedural experience or competence23.
Tomorrow’s Doctors 2009
Recently, a further edition of the GMC’s Tomorrow’s Doctors has been published8. This highlights the need for medical students to have more opportunities to gain knowledge and skills with patients in clinical placements, and encourages the development of Student Assistantships in the final year, in which “a student, assisting a junior doctor and under supervision, undertakes most of the duties of an FY1 doctor.” Assistantships should be above and separate to the WSP, which is when the student spends “a period working with the FY1 who is in the post they will take up when they graduate.” The WSP should also consist of ‘protected time’ distinct from induction. The document also states that the WSP should normally last at least one week and take place as close to the point of employment as possible. In May 2011, Queen’s University replaced the final year WSP with a novel Student Assistantship and many of the issues identified in our WSP study have now been addressed. An evaluation of that Student Assistantship is planned.
CONCLUSIONS
This study has highlighted a number of deficiencies with the current WSP, including the focus on the use of log books, the timing of the attachment, relatively low levels of supervision provided by senior hospital staff members, and students feeling particularly unprepared for medical emergencies, prescribing, and the emotional aspects of the job. The majority of FPSDs shared views with the students on the usefulness of the attachment, the limitations of the logbooks, that not having exam results served as an obstacle to the students’ involvement, and that students’ skills improve during the attachment. However, there were clear disagreements between the students and FPSDs on the timing and duration of the attachment, and about student attendance.
To help ease the transition to working life students should have clearer directions about whom to shadow and have the opportunity to work with the ‘Hospital at Night’ team. Currently, as part of the Student Assistantship, work is underway to introduce workplace-based assessments similar to those used by doctors-in-training. These should supersede the log book as the formal assessment and could also help condition the students for post-graduate training. Use of simulated training environments would allow students to gain experience about medical emergencies, and drug prescribing and administration in a safe environment. QUB’s introduction of a longer student assistantship for the 2012 graduates should help ease students’ worry about the duration of attachment. Finally, further study is also needed to assess the extent of the emotional and psychological impacts of the early FY1 period, as well as mechanisms to ease this transition.
The authors have no conflict of Interest.
REFERENCES
- 1.Goldacre MJ, Lambert T, Evans J, Turner G. Pre-registration house officers’ views on whether their experience at medical school prepared them well for their jobs: national questionnaire survey. BMJ. 2003;326(7397):1011–2. doi: 10.1136/bmj.326.7397.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berridge EJ, Freeth D, Sharpe J, Roberts CM. Bridging the gap: supporting the transition from medical student to practising doctor--a two-week preparation programme after graduation. Med Teach. 2007;29(2):119–27. doi: 10.1080/01421590701310897. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed I, Banu H, Al-Fageer R, Al-Suwaidi R. Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care. 2009;24(3):e1–e7. doi: 10.1016/j.jcrc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Warriner D, Banham L. Shadowing the junior doctor. Student BMJ. 2007;15:427–70. [Google Scholar]
- 5.Prince KJ, Boshuizen HP, Van der Vleuten CP, Scherpbier AJ. Students’ opinions about their preparation for clinical practice. Med Educ. 2005;39(7):704–12. doi: 10.1111/j.1365-2929.2005.02207.x. [DOI] [PubMed] [Google Scholar]
- 6.Bogg J, Gibbs T, Bundred P. Training, job demands and mental health of pre-registration house officers. Med Educ. 2001;35(6):590–5. doi: 10.1046/j.1365-2923.2001.00951.x. [DOI] [PubMed] [Google Scholar]
- 7.Wall D, Bolshaw A, Carolan J. From undergraduate medical education to pre-registration house office year: how prepared are students? Med Teach. 2006;28(5):435–9. doi: 10.1080/01421590600625171. [DOI] [PubMed] [Google Scholar]
- 8.General Medical Council. Tomorrows Doctors: outcomes and standards for undergraduate medical education. London: General Medical Council; 2009. [Google Scholar]
- 9.Duns G, Weiland T, Crotty B, Jolly B, Cuddihy H, Dent A. Self-rated preparedness of Australian prevocational hospital doctors for emergencies. Emerg Med Australas. 2008;20(2):144–88. doi: 10.1111/j.1742-6723.2008.01062.x. [DOI] [PubMed] [Google Scholar]
- 10.Petersson BH, Agergaard M, Risør T. [The newly graduated doctor. Is he or she sufficiently prepared to fulfil a doctor’s responsibilities?]Ugeskr Laeger. 2006;168(18):1756–9. Danish. [PubMed] [Google Scholar]
- 11.Haffling AC, Håkansson A. Patients consulting with students in general practice: Survey of patients satisfaction and their role in teaching. Med Teach. 2008;30:622–9. doi: 10.1080/01421590802043827. [DOI] [PubMed] [Google Scholar]
- 12.O’ Sullivan AJ, Toohey SM. Assessment of professionalism in undergraduate medical students. Med Teach. 2008;30(3):280–6. doi: 10.1080/01421590701758640. [DOI] [PubMed] [Google Scholar]
- 13.The Audit Commission. A Spoonful of sugar: medicines management in NHS hospitals. London: The Audit Commission; 2001. [Google Scholar]
- 14.Han WH, Maxwell SR. Are medical students adequately trained to prescribe at the point of graduation? Views of first year foundation doctors. Scot Med J. 2006;51(4):27–32. doi: 10.1258/RSMSMJ.51.4.27. [DOI] [PubMed] [Google Scholar]
- 15.Illing J, Peile E, Morrison J, Morrow G, Davies C, Donaldson M, et al. How prepared are medical graduates to begin practice? A comparison of three diverse UK medical schools Final summary and conclusions for the GMC Education Committee. London: General Medical Council; 2008. Available from: http://www.gmc-uk.org/FINAL_How_prepared_are_medical_graduates_to_begin_practice_September_08.pdf_29697834.pdf Last accessed March 2012.
- 16.Kilminster SM, Jolly BC. Effective supervision in clinical practice settings: a literature review. Med Educ. 2000;34(10):827–40. doi: 10.1046/j.1365-2923.2000.00758.x. [DOI] [PubMed] [Google Scholar]
- 17.Mattern WD, Weinholtz D, Freidman CP. The attending physician as teacher. N Engl J Med. 1983;308(19):1129–32. doi: 10.1056/NEJM198305123081904. [DOI] [PubMed] [Google Scholar]
- 18.Calman KC, Donaldson M. The pre-registration house officer year: a critical incident study. Med Educ. 1991;25(1):51–9. doi: 10.1111/j.1365-2923.1991.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 19.Davies BW, Campbell WB. Inguinal hernia repair: see one do one teach one? Ann R Coll Surg Engl. 1995;77(6 Suppl):299–301. [PubMed] [Google Scholar]
- 20.Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. BMJ. 2004;329(7469):770–3. doi: 10.1136/bmj.329.7469.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akehurst JC. Electronic monitoring of clinical experience during undergraduate training in diagnostic radiology. Br J Radiol. 1999;72(853):76–9. doi: 10.1259/bjr.72.853.10341693. [DOI] [PubMed] [Google Scholar]
- 22.Watters DA, Green AJ, Van Rij A. Requirements for trainee logbooks. ANZ J Surg. 2006;76(3):181–4. doi: 10.1111/j.1445-2197.2006.03663.x. [DOI] [PubMed] [Google Scholar]
- 23.Shields R, Macleod DA, Porter RW. Structured learning is now being used Letter. BMJ. 1997;315(7100):124–5. doi: 10.1136/bmj.315.7100.125. [DOI] [PMC free article] [PubMed] [Google Scholar]


