Abstract
Background
Disability is associated with depression in older persons, yet the effect of disability burden on the likelihood of being depressed is uncertain.
Methods.
A total of 754 community-living persons, aged ≥70, underwent monthly assessments in four essential activities of daily living and assessments of depression (yes/no) every 18 months for up to 108 months. Within each 18-month person-interval, participants’ disability burden was operationalized as none or any, and according to severity (none, mild, or severe) and chronicity (none, nonchronic, or chronic) given the highest level of severity or chronicity experienced during a given 18-month interval, respectively. A variable combining severity and chronicity (none, nonchronic mild, nonchronic severe, chronic–mild, or chronic–severe) was also created. Using generalized estimating equations, we evaluated the association between each indicator of disability burden and subsequent depression.
Results
Participants who had any versus no disability during the previous 18 months were 65% more likely to experience subsequent depression (OR = 1.65; 95% confidence interval [CI] 1.34, 2.02). Quantifying severity (mild disability vs. none, OR = 1.43; 95% CI: 1.15, 1.79; severe disability vs. none, OR = 2.07; 95% CI 1.56, 2.74) and chronicity (nonchronic disability vs. none, OR = 1.44; 95% CI 1.13, 1.83; chronic disability vs. none, OR = 1.96; 95% CI 1.50, 2.55) indicated increasingly stronger associations with subsequent depression, with the highest likelihood of subsequent depression (OR = 2.42; 95% CI 1.78, 3.30) observed among participants with chronic–severe disability.
Conclusions
Quantifying the magnitude of disability burden, particularly on the basis of severity and chronicity, provides additional information regarding the likelihood of experiencing subsequent depression among older persons.
Key Words: Aging, Disability, Depression, Depressive symptoms, Prospective studies.
Depression and disability in activities of daily living (ADLs) are important clinical and public health problems in older persons. Both conditions are common and associated with substantial morbidity, increased use of health care services, and higher mortality risk (1–5). These conditions also are inextricably linked, with studies supporting each as a risk factor for the other; although, some research points to a stronger influence of disability on subsequent depression than that of depression on disability (6,7). These robust, and likely mutually reinforcing relationships, are grounded in theory. For example, stress theory asserts that disruption of body systems, ie, altered homeostasis, resulting from new disability or the ongoing psychological and physical stress of chronic disability, may lead to depression, and it also suggests that depressive symptoms, such as anhedonia, indirectly lead to disability through altered neural, hormonal, and immunologic functions (8,9).
Several prior studies have found that disability is associated with depression. However, it remains uncertain as to whether the likelihood of experiencing depression is similar regardless of disability burden. The burden of disability, both across and within older persons, is highly variable in terms of severity and chronicity (10,11). Yet, in prior studies, disability has primarily been defined as present or absent regardless of severity (6,12), and infrequent assessments of disability have precluded assessments of chronicity over time (6,13,14). Consequently, research is needed to broaden the understanding of the overall impact of disability burden on subsequent depression.
The objective of this prospective study was to determine whether, and to what extent, different indicators of disability burden are associated with the likelihood of experiencing depression in older persons. To achieve our objective, we used data from a unique cohort of older persons who had monthly assessments of disability for 9 years and up to six assessments of depression at 18-month intervals. We estimated the effect of disability burden, operationalized on the basis of severity and chronicity, on older persons’ likelihood of subsequent depression.
Methods
Sample
Participants were members of the Precipitating Events Project (PEP), a longitudinal study of 754 nondisabled, community-living persons aged 70 years or older (15). The assembly of the cohort has been described in detail elsewhere (15). Briefly, potential participants were identified from 3,157 age-eligible members of a health plan in New Haven, Connecticut. The primary inclusion criteria were English-speaking and requiring no personal assistance with four essential ADLs—bathing, dressing, transferring from a chair, and walking across a room. The participation rate was 75.2% (15). The Human Investigation Committees at Yale University and the University of Connecticut Health Center approved the study.
Data Collection
Comprehensive home-based assessments were completed at baseline and subsequently at 18-month intervals for up to 108 months. Monthly telephone interviews were also completed during this time. Deaths were ascertained by review of local obituaries and/or from an informant during a subsequent telephone interview. A total of 405 (53.7%) participants died after a median follow-up of 68 months, whereas 35 (4.6%) dropped out of the study after a median follow-up of 24 months. Data were otherwise available for approximately 98% of the 62,107 monthly telephone interviews.
During each of the comprehensive assessments, data were collected on several important clinical factors. Medical comorbidity was ascertained based on a count of up to nine self-reported, physician-diagnosed chronic medical conditions: hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, and cancer. Cognitive status was assessed by the Folstein Mini-Mental State Examination (MMSE [16]), where MMSE scores range from 0 to 30, with higher scores representing better cognitive status. Physical activity was assessed by the Physical Activity Scale for the Elderly (PASE), where PASE scores range from 0 to 400 (17). The use of antidepressant medication(s) was ascertained by review of all pill bottles or a medication list. If a list was unavailable, participants were asked to recall medications they had taken during the prior 2 weeks. All medications, but not the doses or dosing schedule, were recorded and antidepressant medications were subsequently coded based on the American Hospital Formulary system code 28.16.04. Trazodone and Amitriptyline were not coded as antidepressants because they are commonly used for other indications, including sleep and pain (18,19). The amount of missing data for the aforementioned variables was less than 1% in the baseline assessment and less than 5% in all subsequent assessments.
Assessment of depressive symptoms .—During each of the comprehensive assessments, the frequency of depressive symptoms in the previous week was assessed with the 11-item Center for Epidemiologic Studies-Depression (CES-D) scale (20). As reported previously (21–23), scores were transformed to be compatible with the 20-item scale (24), and participants scoring ≥20 were considered to have “clinically significant depressive symptoms” or “depression.” Data on depression were complete for 100% of the participants at baseline and 95%, 93%, 91%, 90%, 89%, and 88% of the nondecedents at 18, 36, 54, 72, 90, and 108 months, respectively.
Assessment and operationalization of disability .—Disability in the four essential ADL tasks was assessed during the monthly telephone interviews. Complete details regarding the monthly interviews, including formal tests of reliability and accuracy, have been previously described (25). Participants who needed help from another person or were unable to complete an ADL task were considered disabled in that ADL. Disability was then classified each month as none, mild, and severe (ie, disabled in 0, 1–2, or 3–4 ADLs, respectively [11]). The small amount of missing monthly data on disability was imputed using methods described previously (23). We then operationalized disability burden for each participant within each 18-month person-interval (eg, 0–18 months, 18–36 months, etc.) on the basis of severity and chronicity. First, a dichotomous 0/1 variable was created to indicate presence of no disability or any disability during each interval. Then, participants with any disability were coded as having either mild or severe disability burden according to the highest level of disability experienced during a given 18-month interval. A three-level categorical variable was subsequently created to indicate if participants had no, mild, or severe disability during each respective interval. For example, a participant who experienced both mild and severe disability between 18 and 36 months would be coded as having severe disability during that interval. Participants with any disability were also coded according to whether or not they experienced chronic disability in a given interval, where chronic disability was considered as experiencing at least 3 consecutive months of disability. A three-level categorical variable was then created to indicate if participants had no, nonchronic, or chronic disability during each respective interval. Finally, we created a five-level categorical variable using both the severity and chronicity data to indicate if participants had no, nonchronic mild, nonchronic severe, chronic–mild, or chronic–severe disability during each respective interval. We also operationalized each of these variables using only the 6 months immediately preceding the 18, 36, 54, 72, 90, and 108-month depression assessments.
Statistical Analysis
Because we were interested in the effect of disability burden on subsequent depression, depression as an outcome was derived from the 18, 36, 54, 72, 90, and 108-month face-to-face interviews. Consequently, our analytic sample included the 685 (90.8%) PEP participants who completed a depression assessment at any of these time points. These 685 participants contributed a total of 3,036 person-intervals of 18 months each over the study period. The baseline characteristics of the 685 participants in the analytic sample did not differ from those of the 69 participants who died (n = 48) before the 18-month follow-up assessment or those who had no depression data at any of the comprehensive assessments (n = 21), with the exception of age. The participants in the analytic sample were younger than those not included in the sample (p < .001).
We determined the baseline characteristics of the analytic sample using descriptive statistics. Within each 18-month interval, we used chi-square tests to evaluate the unadjusted association between any (vs. no) disability and depression at the end of that interval. These analyses were run separately for participants who did and did not have depression at the beginning of the respective interval. To evaluate this association across the entire study period, we first stratified the data according to person-intervals where participants were nondepressed (n = 2,517 person-intervals) or depressed (n = 519 person-intervals) at the beginning of each interval, respectively. Within these nondepressed and depressed groups, we used chi-square statistics to determine if the percentage of person-intervals ending in depression differed between participants who had any disability versus no disability. These analyses did not account for potential within-subject correlation over time. We used similar procedures to evaluate the association between disability severity (mild vs. no disability; severe vs. no disability), chronicity (nonchronic vs. no disability; chronic vs. no disability), and severity-chronicity (nonchronic mild; nonchronic severe; chronic mild; and chronic severe vs. no disability) and subsequent depression, respectively. Generalized estimating equations with the exchangeable correlation structure were then used to determine the longitudinal association between each indicator of disability burden and subsequent depression. For the multivariable models, the covariates included demographic characteristics, number of chronic conditions, MMSE score, physical activity score, and antidepressant use. Furthermore, because participants were still at risk of remaining depressed once they became depressed, we did not exclude participants from the analyses who were depressed at baseline (n = 86) or who developed depression during the study. Rather, the analyses included a variable that controlled for participants’ depression status at the beginning of each 18-month interval. Adjusted odds ratios specifying the association between the indicators of disability burden and subsequent depression were derived based on quasi-likelihood estimates and z-tests were used to evaluate statistical significance. Quasi-likelihood under the Independence Model Criterion statistics were used to evaluate model fit. These multivariable analyses were rerun using the indicators of disability burden as operationalized within the 6 months immediately prior to the depression assessment.
All statistical tests were two-tailed with p < .05 indicating significance, and all analyses were performed using SAS version 9.1.
Results
Table 1 provides the baseline characteristics of the analytic sample. Participants had an average age of 78 years, approximately two thirds were women, and most were white. Participants were generally healthy at baseline with an average of less than two chronic conditions and high MMSE and physical activity scores. About 10% of the participants were taking an antidepressant medication, and about 12% were depressed (ie, CES-D ≥ 20).
Table 1.
Baseline Characteristics of the Analytic Sample
| Characteristic | N = 685 | |
|---|---|---|
| Age, M (SD) | 78.2 (5.1) | |
| Women, n (%) | 445 (64.9) | |
| Whites, n (%) | 681 (89.8) | |
| Years of education, M (SD) | 12.0 (2.9) | |
| Number of chronic conditions, M (SD) | 1.8 (1.2) | |
| Cognitive status score, M (SD)* | 26.8 (2.4) | |
| Physical activity score, M (SD)† | 92.3 (57.8) | |
| Antidepressant medication use, n (%) | 73 (10.6) | |
| Depressed, n (%)‡ | 86 (12.6) |
*Assessed with the Mini-Mental State Examination.
†Assessed with the Physical Activity Scale for the Elderly.
‡Determined using the Center for Epidemiological Studies-Depression Scale where depressed is a score of ≥20.
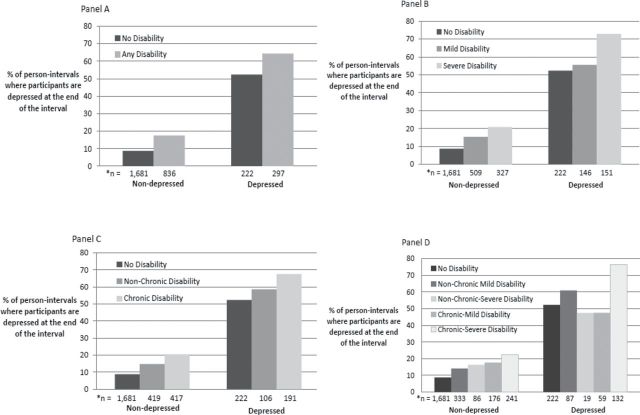
A total of 388 (51.3%) participants were disabled at some point during the 9-year study period. Between baseline and 18 months, 207 (30.3%) participants experienced disability. During the five subsequent intervals, 237 (35.0%), 279 (44.5%), 277 (49.6%), 264 (52.6%), and 250 (55.3%) participants experienced disability, respectively. Figure 1 illustrates the association between each indicator of disability burden and subsequent depression among all person-intervals across the 9-year study period, stratified according to whether or not participants were nondepressed (n = 2,517 person-intervals) or depressed (n = 519 person-intervals) at the beginning of each person-interval. Panel A indicates that within both nondepressed and depressed groups, the percentage of person-intervals where participants were depressed at the end of the interval was significantly higher among the person-intervals where participants experienced any disability compared with no disability (p < .001). Panels B and C show that within both nondepressed and depressed groups, the percentage of person-intervals where participants were depressed at the end of the interval increases with increasing severity (Panel B; p for trend <.001), and for those with nonchronic and chronic disability compared with no disability, respectively (Panel C; p for trend <.001). Finally, Panel D indicates that within the nondepressed group, the percentage of person-intervals where participants were depressed at the end of the interval increases with increasing disability burden (p for trend <.001). In the depressed group, the percentage of person-intervals where participants were depressed at the end of the interval increases with increasing disability burden (p for trend <.001), with the exception of person-intervals where participants experienced nonchronic severe disability and chronic mild disability.
Figure 1.
The association between indicators of disability burden and subsequent depression. Panels A, B, C, and D are stratified by person-intervals where participants were nondepressed (n = 2,517) or depressed (n = 517) at the beginning of each person-interval. Panel A: Percentage of person-intervals where participants experienced subsequent depression among those with any vs. no disability. Panel B: Percentage of person-intervals where participants experienced subsequent depression among those with no, mild, and severe disability. Panel C: Percentage of person-intervals where participants experienced subsequent depression among those with no, nonchronic, and chronic disability. Panel D: Percentage of person-intervals where participants experienced subsequent depression among those with no, nonchronic mild, nonchronic severe, chronic–mild, and chronic–severe disability.
*Number of person-intervals within each category where participants are nondepressed and depressed at the beginning of the interval, respectively.
Table 2 presents the results of the multivariable longitudinal models where disability burden was operationalized as any versus none and in terms of severity, chronicity, and severity-chronicity. On average, compared with participants who experienced no disability, participants with any disability were approximately 65% more likely to experience subsequent depression (OR = 1.65; 95% CI 1.34, 2.02). Operationalizing disability burden according to severity (mild disability vs. none OR = 1.43; 95% CI 1.15, 1.79; severe disability vs. none OR = 2.07; 95% CI 1.56, 2.74) and chronicity (nonchronic disability vs. none OR = 1.44; 95% CI 1.13, 1.83; chronic disability vs. none OR = 1.96; 95% CI 1.50, 2.55) revealed increasingly stronger associations with subsequent depression as disability burden increased. When severity and chronicity were considered jointly, there was little difference in the likelihood of subsequent depression for comparisons between no disability and nonchronic mild, nonchronic severe, and chronic mild disability, respectively, with odds ratios ranging from approximately 1.3–1.5. In contrast, compared with participants having no disability, the odds of experiencing depression were more than 2.4 times as high among those having chronic–severe disability. Findings were similar when these models were run while restricting each indicator of disability burden to the 6 months immediately preceding the depression assessment.
Table 2.
The Association Between Indicators of Disability Burden and Subsequent Depression Over 108 Months*,†
| Disability Burden | Odds Ratio | 95% Confidence Interval | p-Value | |||
|---|---|---|---|---|---|---|
| Any disability | ||||||
| None | 1.00 | — | — | |||
| Any | 1.65 | 1.34, 2.02 | <0.001 | |||
| Severity | ||||||
| None | 1.00 | — | ||||
| Mild | 1.43 | 1.15, 1.79 | 0.002 | |||
| Severe | 2.07 | 1.56, 2.74 | <0.001 | |||
| Chronicity | ||||||
| None | 1.00 | — | — | |||
| Nonchronic | 1.44 | 1.13, 1.83 | 0.004 | |||
| Chronic | 1.96 | 1.50, 2.55 | <0.001 | |||
| Severity–chronicity | ||||||
| None | 1.0 | — | — | |||
| Nonchronic mild | 1.47 | 1.14, 1.90 | 0.003 | |||
| Nonchronic severe | 1.31 | 0.78, 2.21 | 0.30 | |||
| Chronic mild | 1.43 | 1.02, 2.00 | 0.04 | |||
| Chronic severe | 2.42 | 1.78, 3.30 | <0.001 | |||
*Adjusted for age, sex, race, education, number of chronic conditions, cognitive status score, physical activity score, antidepressant medication use, and depression (CES-D score of ≥20) at the beginning of each 18-month interval.
†Quasi-likelihood under the independence model criterion statistics were 2,553.4; 2,552.4; 2,557.6; and 2,555.7 for the any, severity, chronicity, and severity-chronicity models, respectively, and indicate comparable fit across all models.
Discussion
In this longitudinal study, which included monthly assessments of disability and repeated assessments of depression, we evaluated the association between various indicators of disability burden and subsequent depression in older persons over a period of 9 years. We confirmed that disability is a salient risk factor for depression in older persons. More importantly, we found that quantifying the magnitude of older persons’ disability burden, particularly on the basis of severity and chronicity, offers additional information for estimating the likelihood of experiencing subsequent depression relative to the usual procedure of categorizing disability as simply absent or present.
Whereas disability in older persons had historically been conceptualized as a progressive condition (4), it is now widely accepted that disability in this population is highly dynamic and heterogenous (26). Despite this knowledge, wide time intervals (eg, 5 years) between disability assessments (6,14) or the evaluation of disability at only one time point (13,27,28) previously made it impossible to determine if the likelihood of being depressed increases with worsening severity of disability or differs between those with nonchronic versus chronic disability. This “snapshot” approach to assessing disability likely underestimates those with disability (4) and precludes assessment of chronicity. In contrast, the monthly assessments in this study optimized the likelihood of accurately ascertaining participants’ highest level of disability severity within each 18-month interval and enabled us to distinguish between those who experienced nonchronic versus chronic disability.
We found that severe disability and chronic disability each had a strong, independent association with subsequent depression. However, because study participants experienced nonchronic severe disability and chronic mild disability in only 3.5% and 7.7% of the total person-intervals, respectively, it is likely that these aforementioned associations were driven by participants who experienced chronic–severe disability. When the five-category disability burden variable was evaluated, the addition of chronicity in those with severe disability substantially increased the likelihood of depression but had no additive effect on the association between mild disability and depression. The absence of a significant association between nonchronic severe disability and subsequent depression is likely attributable to the small number of person-intervals where participants experienced nonchronic severe disability. Based on our findings, older persons with chronic–severe disability may be at particularly high risk of depression, highlighting the potential clinical importance of assessing disability burden on the basis of both severity and chronicity.
Older persons have been found to move into and out of depressed and nondepressed states over time (21,22). The repeated assessments of depression over six time intervals in this study likely enabled us to classify participants as depressed who may otherwise have been misclassified as nondepressed had only one follow-up assessment of depression occurred, as has been done previously (13,28). Furthermore, failure to include those with prior depression in the analyses, who are still at risk of being depressed, may consequently provide a biased effect of disability burden on subsequent depression and would likely underestimate the true effect of disability burden on depression. We found that regardless of the absence or presence of depression at the beginning of each person-interval, the percentage of participants who were depressed at the end of each 18-month interval was significantly higher among those who experienced any versus no disability during the respective interval. Similar results were observed as disability burden worsened based on severity, chronicity, and severity–chronicity. In multivariable analyses, disability was strongly associated with experiencing depression at the end of each interval, even after adjusting for the absence or presence of depression at the beginning of each person-interval. Consequently, our findings demonstrate that the relationship between disability burden and subsequent depression is not driven solely by whether or not participants had prior depression.
There are several limitations to this study that warrant comment. Had we known the prevalence of disability in the 18 months prior to baseline, the 30% increase in the prevalence of disability between baseline (where all participants were nondisabled) and 18 months would likely not have been as sharp. In addition, competing mortality may also have lowered the disability rate over time, thereby accounting for the increasingly smaller differences in the prevalence of disability from one interval to the next. We were unable to confirm clinical depression using the CES-D. However, the cutpoint of 20 or more on this instrument not only increases the likelihood of identifying older persons with major depression (29), but is also very useful for identifying subsyndromal depression, ie, depressive symptomatology that is clinically meaningful given its strong association with negative health outcomes (30,31). Using the cutpoint of 20 or more, nearly 13% of the sample in this study was depressed at baseline, a rate somewhat higher than that reported in other studies using a cutpoint of 20 or more on the CES-D (32,33). The difference may be explained by the higher mean age, more racially diverse population, or larger proportion of females in our sample relative to the samples in prior studies. The discrepancy may be further explained by prior studies’ exclusion of those with mobility disability at baseline (32) or exclusion of participants who died during the follow-up period from the analyses (33). We used an analytic approach to ensure that disability burden temporally preceded depression. However, because depression was only measured at 18-month intervals, it is possible that depression could have started earlier within any given interval, subsequently leading to disability. Although we adjusted for antidepressant use, information regarding the dose, dosing schedule, adherence, indication, and start of treatment was not available. Finally, because our study participants were members of a single health plan, initially nondisabled, and at least aged 70 years at baseline, the generalizability of our findings to other older adult populations may be questioned. However, the demographic characteristics of our study population, including years of education, closely mirror those of persons aged 70 years or older in New Haven County, Connecticut, which, in turn, are comparable to those in the United States as a whole, with the exception of race. New Haven County has more non-Hispanic whites in this age group than in the United States (91% vs. 84%). Furthermore, generalizability depends not only on the characteristics of the study population but also on its stability over time (34).
Our findings complement prior research evaluating the relationship between disability and depression. Furthermore, our findings emphasize that assessing either severity or chronicity of disability may be less useful in estimating risk of subsequent depression than may be a joint assessment of both types of disability burden. Future work is needed to identify the underlying physiological mechanisms that drive the relationship between disability and depression in older persons and to determine if these mechanisms differ according to burden of disability.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (grant numbers R37AG17560, R01AG022993, and K24AG021507 to TG and K01AG031324 to LB). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (grant number P30AG21342).
Acknowledgments
This paper was initially presented as a talk at the 2010 Annual Meeting of the American Geriatrics Society. We thank Denise Shepard, BSN, MBA, Andrea Benjamin, BSN, Paula Clark, RN, Martha Oravetz, RN, Shirley Hannan, RN, Barbara Foster, Alice Van Wie, BSW, Patricia Fugal, BS, and Amy Shelton, MPH for assistance with data collection; Wanda Carr and Geraldine Hawthorne for assistance with data entry and management; Evelyne Gahbauer, MD, MPH and Linda Leo-Summers, MPH who provided data management and programming; Peter Charpentier, MPH for development of the participant tracking system; and Joanne McGloin, MDiv, MBA for leadership and advice as the Project Director.
References
- 1. Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003. 58 249–265 [DOI] [PubMed] [Google Scholar]
- 2. Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004. 42 512–521 [DOI] [PubMed] [Google Scholar]
- 3. Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001. 161 2602–2607 [DOI] [PubMed] [Google Scholar]
- 4. Guralnik JM, Ferrucci L. Underestimation of disability occurrence in epidemiological studies of older people: is research on disability still alive?. J Am Geriatr Soc. 2002. 50 1599–1601 [DOI] [PubMed] [Google Scholar]
- 5. Sun W, Schooling CM, Chan WM, Ho KS, Lam TH. The association between depressive symptoms and mortality among Chinese elderly: a Hong Kong cohort study. J Gerontol A Biol Sci Med Sci. 2011. 66 459–466 [DOI] [PubMed] [Google Scholar]
- 6. Ormel J, Rijsdijk FV, Sullivan M, van Sonderen E, Kempen GI. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. J Gerontol B Psychol Sci Soc Sci. 2002. 57 P338–P347 [DOI] [PubMed] [Google Scholar]
- 7. Chen CM, Mullan J, Su YY, Griffiths D, Kreis IA, Chiu HC. The longitudinal relationship between depressive symptoms and disability for older adults: a population-based study. J Gerontol A Biol Sci Med Sci. 2012. doi:10.1093/gerona/gls074 [DOI] [PubMed] [Google Scholar]
- 8. Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981. 22 337–356 [PubMed] [Google Scholar]
- 9. Avison WR, Turner RJ. Stressful life events and depressive symptoms: disaggregating the effects of acute stressors and chronic strains. J Health Soc Behav. 1988. 29 253–264 [PubMed] [Google Scholar]
- 10. Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community-living older persons. J Gerontol A Biol Sci Med Sci. 2003. 58 70–75 [DOI] [PubMed] [Google Scholar]
- 11. Ferrucci L, Guralnik JM, Simonsick E, Salive ME, Corti C, Langlois J. Progressive versus catastrophic disability: a longitudinal view of the disablement process. J Gerontol A Biol Sci Med Sci. 1996. 51 M123–M130 [DOI] [PubMed] [Google Scholar]
- 12. Schoevers RA, Beekman AT, Deeg DJ, Geerlings MI, Jonker C, Van Tilburg W. Risk factors for depression in later life; results of a prospective community based study (AMSTEL). J Affect Disord. 2000. 59 127–137 [DOI] [PubMed] [Google Scholar]
- 13. Harris T, Cook DG, Victor C, DeWilde S, Beighton C. Onset and persistence of depression in older people–results from a 2-year community follow-up study. Age Ageing. 2006. 35 25–32 [DOI] [PubMed] [Google Scholar]
- 14. Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. J Aging Health. 2005. 17 263–292 [DOI] [PubMed] [Google Scholar]
- 15. Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001. 135 313–321 [DOI] [PubMed] [Google Scholar]
- 16. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975. 12 189–198 [DOI] [PubMed] [Google Scholar]
- 17. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993. 46 153–162 [DOI] [PubMed] [Google Scholar]
- 18. Mayers AG, Baldwin DS. Antidepressants and their effect on sleep. Hum Psychopharmacol. 2005. 20 533–559 [DOI] [PubMed] [Google Scholar]
- 19. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochr Database System Rev. 2007;(4):CD005454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977. 1(3):385–481 [Google Scholar]
- 21. Barry LC, Allore HG, Guo Z, Bruce ML, Gill TM. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psychiatry. 2008. 65 172–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barry LC, Abou JJ, Simen AA, Gill TM. Under-treatment of depression in older persons. J Affect Disord. 2012. 136 789–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barry LC, Murphy TE, Gill TM. Depressive symptoms and functional transitions over time in older persons. Am J Geriatr Psychiatry. 2011. 19 783–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993. 5 179–193 [DOI] [PubMed] [Google Scholar]
- 25. Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004. 291 1596–1602 [DOI] [PubMed] [Google Scholar]
- 26. Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005. 161 575–584 [DOI] [PubMed] [Google Scholar]
- 27. Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychol Aging. 1996. 11 572–581 [DOI] [PubMed] [Google Scholar]
- 28. Chang M, Phillips C, Coppin AK, et al. An association between incident disability and depressive symptoms over 3 years of follow-up among older women: the Women’s Health and Aging Study. Aging Clin Exp Res. 2009. 21 191–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med. 1997. 157 449–454 [PubMed] [Google Scholar]
- 30. Lyness JM, Heo M, Datto CJ, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006. 144 496–504 [DOI] [PubMed] [Google Scholar]
- 31. Lyness JM, King DA, Cox C, Yoediono Z, Caine ED. The importance of subsyndromal depression in older primary care patients: prevalence and associated functional disability. J Am Geriatr Soc. 1999. 47 647–652 [DOI] [PubMed] [Google Scholar]
- 32. Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. 1999. 89 1346–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998. 279 1720–1726 [DOI] [PubMed] [Google Scholar]
- 34. Szklo M. Population-based cohort studies. Epidemiol Rev. 1998. 20 81–90 [DOI] [PubMed] [Google Scholar]