Abstract
Atelectasis is a significant risk factor for the development of pneumonia, especially in pediatric populations that are more prone to alveolar collapse or those who may have weakened muscular tone. The Metaneb® System is a pneumatic, non-invasive physiotherapy technique that delivers chest high frequency oscillations (CHFO). CHFO has been shown to enhance mucociliary clearance of secretions and help resolve patchy atelectasis. This report describes the case of a 17 year old female who developed significant left sided atelectasis after extubation and was effectively managed with complete resolution of her atelectasis with the Metaneb System, obviating the need for reintubation.
Keywords: Chest high frequency oscillations, atelectasis
Introduction
Atelectasis, defined as airway collapse, resulting in non-aeration of affected lung regions is common place in critically ill patients, and is a well known risk factor for the development of pneumonia.1 There are several chest physiotherapy techniques (CPT) that have been devised for reduction of atelectasis in non-ventilated patients; however none have been deemed the standard of care for the management of this condition.2 The Intermittent Percussive Ventilation (IPV®) device, developed by Dr. Forest M. Bird in the late1980’s, is a ventilatory treatment technique that delivers small bursts of gas flow into the lung at high rates. This causes airway pressures to oscillate at very small tidal volumes, and the airway walls vibrate in unison with these oscillations.3 During the delivery of these small tidal volumes, it is theorized that collapsed airways are opened and intrabronchial secretions are mobilized.4 The Metaneb® System (Hill-Rom, Inc. Batesville, Indiana), which was FDA approved in to be used in the hospital setting , is similar to the IPV® device and uses similar engineering to provide the unique gas flow characteristics of IPV®, called chest high frequency oscillations (CHFO) (Figure 1). CHFO is described as a pneumatic form of chest physiotherapy that enhances mucociliary clearance and may resolve patchy atelectasis.5–7 The circuit interface used with the Metaneb® device is seen in Figure 2. The circuit consists of a patient mouthpiece, nebulizer, venturi, and accessory tubing. The Metaneb® can be adjusted to deliver various levels of high frequency rates, pressure limits, and has the capability to supply various levels of resistance on exhalation.
Figure 1.
Continuous high frequency oscillations are delivered during both inspiration and expiration (With permission from Hill Rom®)
Figure 2.
Patient interface between the patient and Metaneb® (With permission from Hill Rom®)
We report a case of a 17 year old female with > 80% dermatologic involvement of toxic epidermal necrolysis and Pseudomonas pneumonia who developed worsening atelectasis after extubation, and who was effectively managed with a Metaneb® device obviating the need for reintubation. This study was reviewed and approved by our Institutional Review Board.
Case Report
A 17 year old female with no prior medical history, reported to a referring institution complaining of a sudden onset of headaches. Upon evaluation, she was found to have a right basal ganglia intracerebral hemorrhage with mass effect and midline shift with an associated left-sided hemiparesis. No neurosurgical intervention was undertaken, but she was started on a regimen of phenytoin for seizure prophylaxis, which was then changed to levetiracetam. Despite having discontinued the phenytoin, she developed a diffuse rash, fevers, and generalized severe pain. Biopsy of the rash was taken by the Dermatology consultants revealed Toxic Epidermal Necrolysis (TEN).
The patient was transferred to our burn intensive care unit with large surface area involvement (>80% total body surface area) of her wounds and significant pain experienced with wound care. On hospital day (HD) 2 on our unit, the decision was made by the surgical team to electively intubate her for pain management and adequate wound care. On HD 3, the patient was taken to the operating room for extensive debridement and xenografting of her wounds. The patient tolerated the procedure well, and continued to be intubated for her extensive wound care. On HD 8, the patient became febrile with an elevated white blood cell count and left sided pulmonary infiltrate on chest x-ray (CXR). She was pan-cultured and respiratory cultures grew Pseudomonas, for which she was started on intravenous antibiotics.
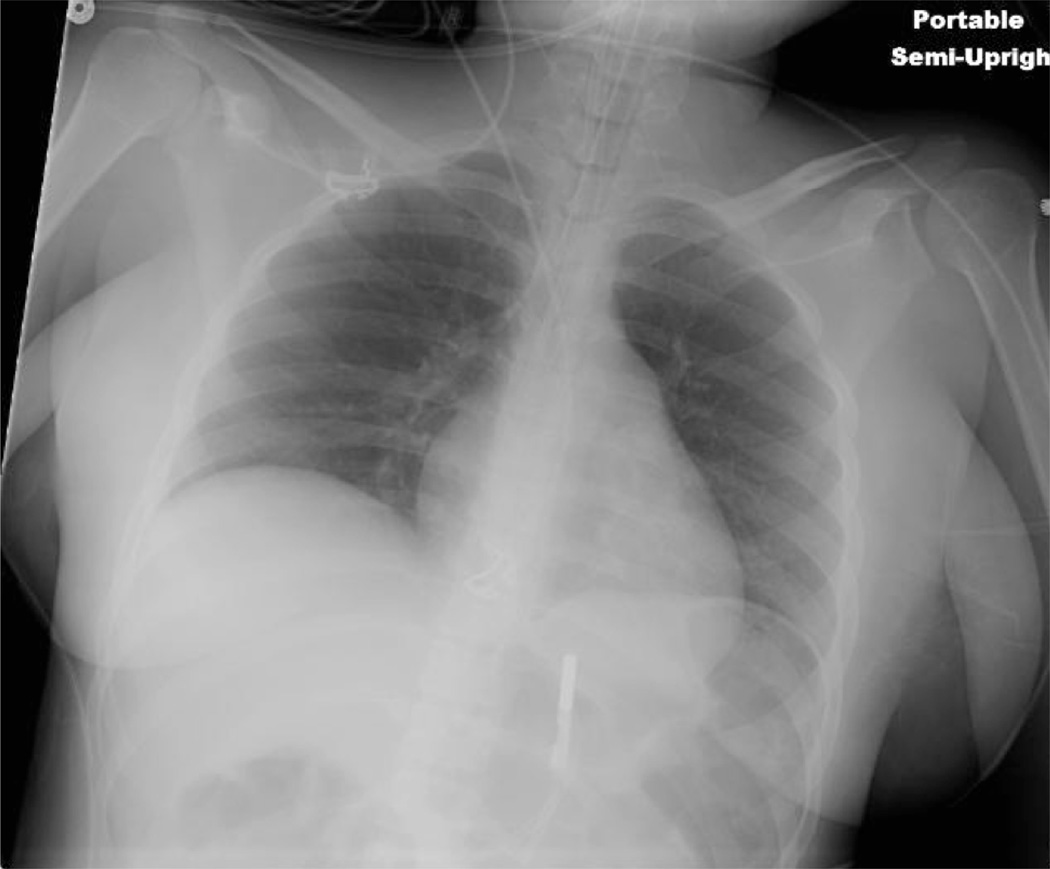
The patient continued to improve with normalization of her CXR and laboratory values and the decision was made to extubate her on HD 17 (See Figure 3). The patient tolerated the procedure well, however within 24 hours was noted to have an elevated white count, worsening physical exam with rhonchorous breath sounds on the left; greater than the right, which correlated with radiologic findings. During this time, the patient maintained adequate oxygenation, but had problems expectorating secretions because of an inability to cough effectively, due both to generalized weakness as well as her recently developed hemiparesis. Despite nebulized albuterol treatments and high flow oxygen therapy, her left sided atelectasis continued to worsen (See Figure 4).
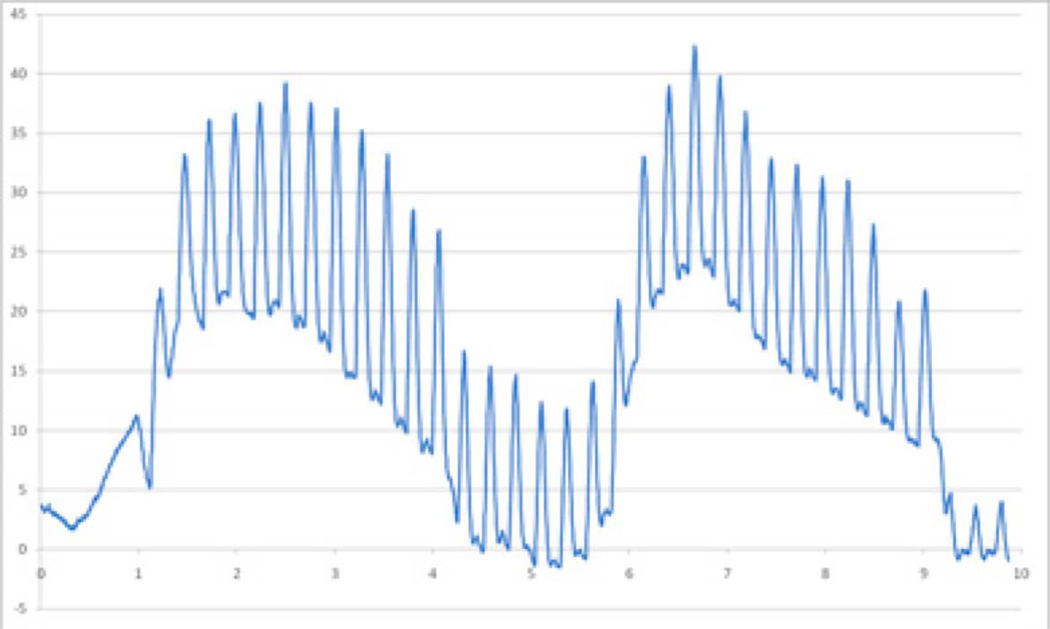
Figure 3.
CXR on HD 17
Figure 4.
CXR on HD 19 showing worsening left-sided atelectasis
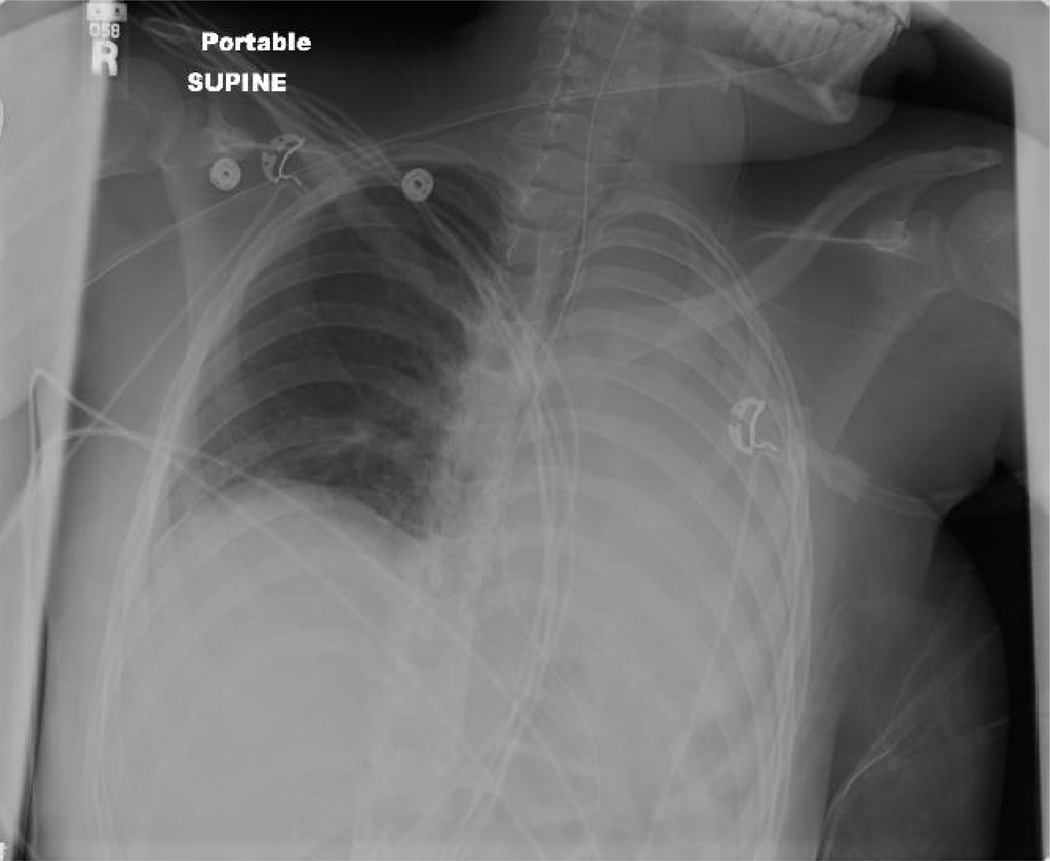
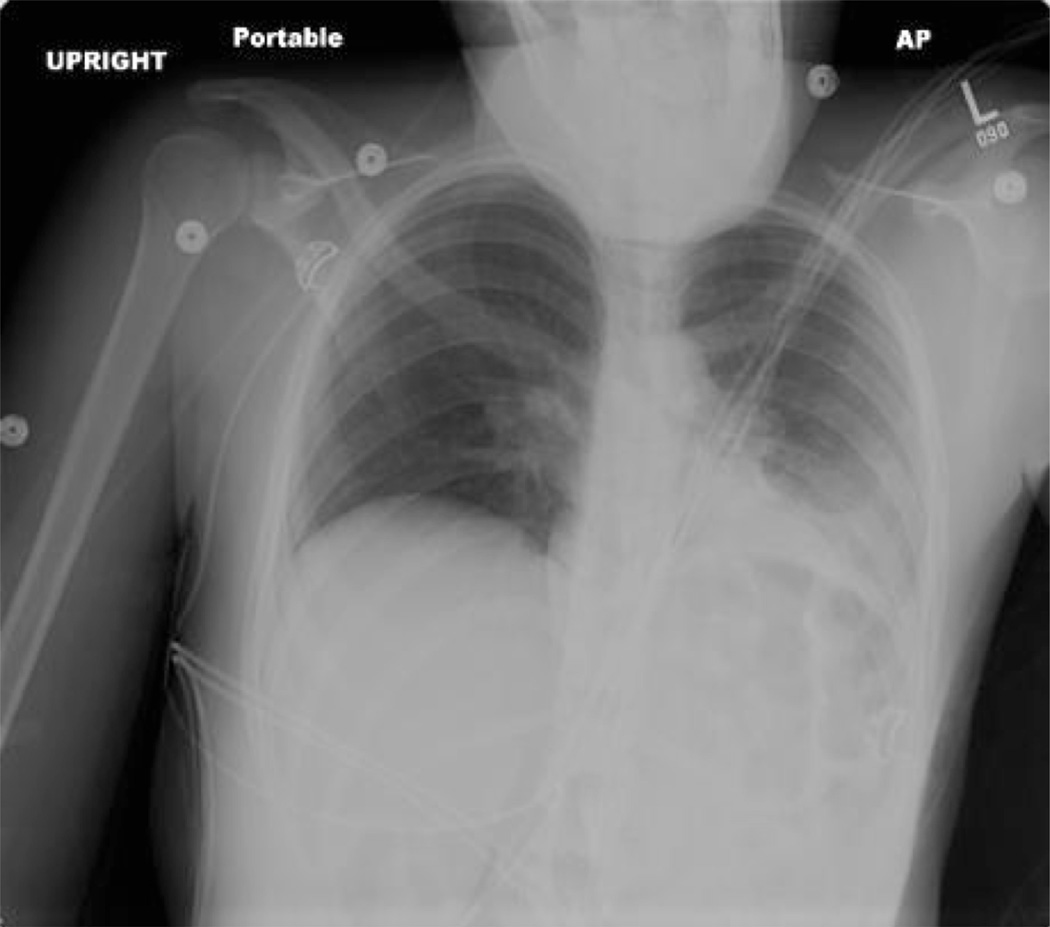
The decision was made to start her on breathing treatments using the Metaneb® device with aerosolized normal saline. Treament with the Metaneb® device was given every two to three hours for approximately ten minutes per treatment. Within four hours of starting the every 2 hour therapy, her atelectasis had partially improved (See Figure 5), and had completely resolved by HD 21 (See Figure 6), with normalization of her white count. During this episode of atelectasis, the patient was still on intravenous antibiotics that had been started for her previously diagnosed pneumonia. The patient remained on antibiotics for a total of 14 days. The patient continued to do well, had improved physical exam findings and was discharged to home on HD 25 with no further infectious or respiratory complications.
Figure 5.
CXR just four hours after the initiation of CHFO treatment
Figure 6.
CXR appearance on HD 21, two days after starting CHFO
Discussion
Atelectasis is a significant risk factor for the development of pneumonia, especially in patients that are more prone to alveolar collapse, such as pediatric populations or those who may have weakened muscular tone.1–2,8 CHFO, via the Metaneb® device, is an effective CPT modality for the management of atelectasis in non-ventilated patients, as shown in the case of this patient with left sided hemiparesis. After just eight hours of initiating Metaneb® system treatments, this patient had significant improvement in both radiologic and physical exam findings. If the patient had required re-intubation because of worsening atelectasis and pneumonia, her hospital stay could have been significantly extended, while placing her at risk for increased morbidity and/or mortality.
The Metaneb® device maintains high frequency oscillatory percussive breaths during inspiration and expiration to form a pressure gradient in small airways where secretions may be trapped. The Metaneb® device employs a fixed orifice venturi to deliver the high frequency percussive breaths whereas the IPV® device manufactured by Percussionaire® uses a sliding venturi system. In theory, both venturi systems are designed and engineered to provide high frequency percussions during both inspiration and exhalation which results in a pressure gradient. It is theorized that the pressure gradient that is created by these unique systems accelerates expiratory airflow allowing any secretions in the small airways to move up and into the larger airways, making it easier for patients to expectorate the secretions or to be suctioned via an artificial airway.7 At the same time, hyperinflation during the treatment with this device may help the patient to breath deep and cough effectively. Improvement in atelectasis in patients treated with IPV® or the Metaneb® System may be due to the increased efficiency of ventilation into the lungs via the high frequency oscillatory percussive breaths. In patients with bronchiectasis, short term IPV® has been shown to be as effective as chest physiotherapy with less discomfort for the patients receiving the therapy.9–10 Further studies need to be done to better understand how the Metaneb® system and IPV® treatments can be used to improve ventilation and mucous clearance in non-intubated patients.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
None of the authors in this study have any financial interests in the Hill Rom company.
References
- 1.Peroni DG, Boner AL. Atelectasis: mechanisms, diagnosis and management. Paediatr Respir Rev. 2000;1(3):274–278. doi: 10.1053/prrv.2000.0059. [DOI] [PubMed] [Google Scholar]
- 2.Deakins K, Chatburn RL. A comparison of intrapulmonary percussive ventilation and conventional chest physiotherapy for the treatment of atelectasis in the pediatric patient. Respir Care. 2002;47(10):1162–1167. [PubMed] [Google Scholar]
- 3.Salim A, Martin M. High-frequency percussive ventilation. Crit Care Med. 2005;33([Supp.]):S241–S245. doi: 10.1097/01.ccm.0000155921.32083.ce. [DOI] [PubMed] [Google Scholar]
- 4.Vargas F, Hilbert G. Intrapulmonary percussive ventilation and noninvasive positive pressure ventilation in patients with chronic obstructive pulmonary disease: “strength through unity?”. Crit Care Med. 2006;34(12):3043–3045. doi: 10.1097/01.CCM.0000248523.61864.D5. [DOI] [PubMed] [Google Scholar]
- 5.Scherer TA, Barandun J, Martinez E, Wanner A, Rubin EM. Effect of high-frequency oral airway and chest wall oscillation and conventional chest physical therapy on expectoration in patients with stable cystic fibrosis. Chest. 1998;113:1019–1027. doi: 10.1378/chest.113.4.1019. [DOI] [PubMed] [Google Scholar]
- 6.Kempainen RR, Williams CB, Hazelwood A, Rubin BK, Milla CE. Comparison of high-frequency chest wall oscillation with differing waveforms for airway clearance in cystic fibrosis. Chest. 2007;132:1227–1232. doi: 10.1378/chest.07-1078. [DOI] [PubMed] [Google Scholar]
- 7.Chatburn RL. High-frequency assisted airway clearance. Respir Care. 2007;52(9):1224–1235. [PubMed] [Google Scholar]
- 8.Toussaint M, De Win H, Steens M, Soudon P. Effect of intrapulmonary percussive ventilation on mucus clearance in duchenne muscular dystrophy patients: a preliminary report. Resp Care. 2003;48(10):940–947. [PubMed] [Google Scholar]
- 9.Yen Ha TK, Bui TD, Badin P, Toussaint M, Nguyen AT. Atelectatic children treated with intrapulmonary percussive ventilation via a face mask: clinical trial and literature review. Pediatr Int. 2007;49(4):502–507. doi: 10.1111/j.1442-200X.2007.02385.x. [DOI] [PubMed] [Google Scholar]
- 10.Paneroni M, Clini E, Simonelli C, Bianchi L, Degli Antoni F, Vitacca M. Safety and efficacy of short-term intrapulmonary percussive ventilation in patients with bronchiectasis. Respir Care. 2011;56(7):984–988. doi: 10.4187/respcare.01098. [DOI] [PubMed] [Google Scholar]