Abstract
Purpose
Surgical management of superior oblique palsy (SOP) is challenging because of combined vertical, horizontal, and torsional misalignment. Our purpose is to report the surgical results of subjects with large primary position hypertropias (≥20 PD) due to unilateral SOP.
Methods
Retrospective review of the records of patients with large hypertropias (>20 PD) secondary to clinically diagnosed SOP. Criteria for success included (1) correction of the anomalous head posture, (2) primary position alignment between orthotropic and 6 PD of undercorrection, and (3) no reoperation required for residual deviations in any direction of gaze.
Results
Forty-five subjects met inclusion criteria. Mean preoperative alignment in primary gaze was 26.5 +/− 6.5 PD compared to 3.0 +/− 4.4 PD postoperatively (p value = <0.001). Twenty-three (51%) cases met our criteria for success with one operation. Of the subjects who had single muscle surgery, 14% had a successful outcome, with a mean 67% (17.3 PD) reduction in hypertropia. Of subjects who underwent simultaneous multiple muscle surgery, 58% met the criteria for a successful result, with a mean 92% (24.6 PD) reduction in primary gaze hypertropia. Success was the highest in subjects who underwent ipsilateral inferior oblique combined with contralateral inferior rectus recessions with (60% success) or without (65% success) a Harada-Ito procedure.
Conclusions
Undercorrections are frequent following surgery for unilateral SOP with preoperative deviations ≥20 PD in primary position, especially after single muscle surgery. Simultaneous multiple muscle surgery rarely results in overcorrection and is recommended in SOP patients with >20 PD of hypertropia in primary position.
Introduction
Surgical management of superior oblique palsy (SOP) is aimeds at achieving fusion and eliminating any anomalous head posture. Although some patients with SOP spontaneously recover, most patients with torticollis or diplopia require treatment.1 Treatment for SOP commonly consists of surgical intervention since lateral incomitance often limits prism use, and botulinum toxin studies have not been encouraging for long-term improvement.2 Vertical diplopia, torsional diplopia, or significant torticollis are all indications for surgery. A number of operative techniques have been recommended for the treatment of SOP including weakening the ipsilateral inferior oblique,3–7 contralateral inferior rectus recession,8 ipsilateral superior rectus recession,9 and superior oblique tuck, isolated or in combination.10–14 The most optimal surgical option has not been well-defined in previous studies, especially for the subset of patients with large primary gaze deviations.
A number of studies have reported the efficacy of different surgical procedures,3–7,10–12 and there have many reports comparing the success of two or more surgical techniques.8–9,14–18 However, the majority of subjects in these studies had hypertropias less than 20 prism diopters (PD) in primary gaze. Those who reported on subsets with large hypertropias have a small number of subjects who underwent only one type of procedure. In these studies, undercorrections are common in patients with more than 20 PD of deviation in primary position.7,9,12,14,17 The literature, however, is not clear if patients with SOP with primary gaze deviations greater than 20 PD should have one or two muscles operated on simultaneously. In this study, we present cases with large-angle hypertropias of at least 20 PD treated by different surgical procedures and compare the postoperative results.
Methods
This study was approved by the University of California, Los Angeles Institutional Review Board and conformed to the requirements of the United States Health Insurance Portability and Accountability act and the tenets of the Declaration of Helsinki. The records of patients with SOP who underwent surgery over a 25-year period treated by a single surgeon (ALR) at the Jules Stein Eye Institute were identified. Patients who were amblyopic, had bilateral SOP, or had a previous surgical procedure were excluded. The minimum post-operative follow-up required for inclusion in the study was six months.
The following demographic information was obtained for the subjects’ records: age, gender, etiology, and the affected eye. The ophthalmologic examination performed, according to limits of ability to cooperate, included visual acuity, ductions, versions, ocular alignment according to alternate occlusion test with prism in near and far fixation in all cardinal gazes, and Beilschowsky’s head-tilt test. In general, visual acuity was assessed using projected age-appropriate optotypes. Near stereopsis was assessed using the Titmus test using the proper refractive correction. Ocular alignment was assessed using cover/uncover and alternate prism cover testing at distance (20 feet) in the cardinal gaze positions. Motor alignment at near was assessed at 14 inches. All motor evaluations were done using spectacle correction. Torticollis was assessed in the patient’s habitual head position in degrees. Subjective excyclotropia was detected by double Maddox rod test.19 A cycloplegic refraction, slit lamp evaluation of the anterior segment, and direct or indirect examination of the posterior segment were performed in all cases. SOP was diagnosed on the basis of history and examination findings based on analysis of versions, ocular alignment in diagnostic gaze positions, head tilt test, and subjective torsion. Ocular versions were graded from −4 (inability to move the eye past midline) to +4 (maximum observable overaction) with 0 being normal movement.20
The operative reports and surgeon’s notes were reviewed. All the procedures for each case were recorded and included the type and number of operated muscles and the amount of surgery performed. Surgical procedures included:
Inferior oblique recession
Superior oblique tuck
Inferior oblique recession and ipsilateral superior rectus recession
Inferior oblique recession and contralateral inferior rectus recession
Inferior oblique recession and contralateral inferior rectus recession with Harada-Ito procedure
Superior oblique tuck and contralateral inferior rectus recession
Superior oblique tuck and inferior oblique recession
Superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession
Superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession
Inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
The operative technique by this surgeon for both the superior oblique tuck and Harada-Ito procedure have been described elsewhere.12,21 The decision to use different surgical approaches were based upon the amount and directionality of lateral incomitance, the amount of excyclotorsion, and the amount of deviation in primary, up- and down-gaze.
Postoperative examinations were performed routinely between one day and one week, and then at one month and six month intervals. Both the preoperative and postoperative evaluations were done by the operating surgeon. At each postoperative visit a complete evaluation of ocular alignment, head posture, ocular torsion and complications were noted.
Statistical Analysis
Criteria for surgical success included correction of head posture and a primary position alignment between orthotropia and 6 PD of undercorrection. Patients who required reoperation for a residual deviation in any field of gaze despite being aligned between orthotropia and 6PD of undercorrection in primary gaze were not considered surgical successes. Statistical analysis was performed using JMP version 9.0.0 (Cary, NC) and Microsoft Excel. To compare means between two groups, a paired, one-tailed Student’s t test was used. To compare pre-operative characteristics such as age and primary position deviation amongst the various surgical groups, a Wilcoxon ranksum test was performed. A p-value of less than 0.05 was considered statistically significant.
Results
Forty-five patients underwent surgery for a primary gaze hypertropia of at least 20 PD due to unilateral SOP. Table 1 lists frequency of each procedure performed, the etiology of SOP, and the mean age for all patients as well as for each procedure subgroup. There was no difference in age or preoperative alignment amongst treatment groups (p<0.05 for both comparisons). An anomalous head posture was noted in 44 (98%) of patients. Of these, 32 (72%) had contralateral head tilt and 2 (4%) had ipsilateral head tilt, 2 (4%) had a chin depression, 1 (2%) had an ipsilateral head turn, and 6 (13%) had a combination of head tilt and turn. The mean postoperative follow-up period was 16 months (range 6 months to 16 years).
TABLE 1.
Patient Data: Number (Frequency) of Type of Vertical Muscle Surgery, Age, and Etiology in 45 Unilateral Superior Oblique Palsy Cases
| Procedure | Number (%) | Age (Years) Mean (Range) |
Etiology Congenital/Acquired |
|---|---|---|---|
| All Patients | 45 | 33.7 (7–87) | 21/24 |
| SO tuck | 3 (7) | 36.0 (9–87) | 1/2 |
| IO Recession | 4 (9) | 28.3 (12–44) | 2/2 |
| IO Recession/SR Recession | 8 (18) | 44.3 (31–69) | 4/4 |
| IO Recession/IR Recession | 20 (44) | 33.9 (7–61) | 8/12 |
| IO Recession/IR Recession/Harado Ito | 5 (11) | 49.0 (41–64) | 3/2 |
| Other multiple muscle combination* | 5 (11) | 34.2 (7–51) | 3/2 |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
Seven (16%) of the cases were one-muscle surgeries, twenty-nine (64%) of the cases were two-muscle surgeries, and nine (20%) were three-muscle surgeries. The “other multiple muscle” surgery group was composed of two two-muscle surgeries (a superior oblique tuck and inferior oblique recession combination and a superior oblique tuck and contralateral inferior rectus recession combination) as well as three three-muscle surgeries (a superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession combination; a superior oblique tuck, inferior oblique recession and superior rectus recession combination; and a inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession combination). The preoperative largest angle of deviation for the majority of patients was in primary position, contralateral gaze, and down gaze (Table 3). Seven (16%) of the patients had equally large deviations in primary position, contralateral gaze, and up gaze, all of whom had inferior oblique and superior rectus recessions (with one patient having an additional superior oblique tuck). Only 2 (4%) patients had comitant strabismus, and both underwent inferior oblique and contralateral inferior rectus recessions. Of note, all seven patients who underwent single muscle surgery had a large amount of incomitance (range: 22–45 PD).
TABLE 3.
Gaze Deviation Patterns According to First Procedure Performed
| Frequency of Procedure (Number of Successes) | |||||
|---|---|---|---|---|---|
| Largest Gaze Deviation | SO Tuck | IO Recession | IO/SR Recessions |
IO/IR Recessions +/− Harado Ito |
Other Multiple Muscle Comb |
| Primary Gaze (n=3) | 0 | 0 | 1 (1) | 1 (1) | 1(0) |
| Primary and Contralateral Gaze (n=10) | 0 | 0 | 1 (0) | 8 (7) | 1 (0) |
| Primary, Contralateral and Down Gaze (n =23) | 3(1) | 4(0) | 0 | 14 (8) | 2 (1) |
| Primary, Contralateral and Up Gaze (n=7) | 0 | 0 | 6 (3) | 0 | 1(1) |
| Equal in All Gazes | 0 | 0 | 0 | 2(2) | 0 |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
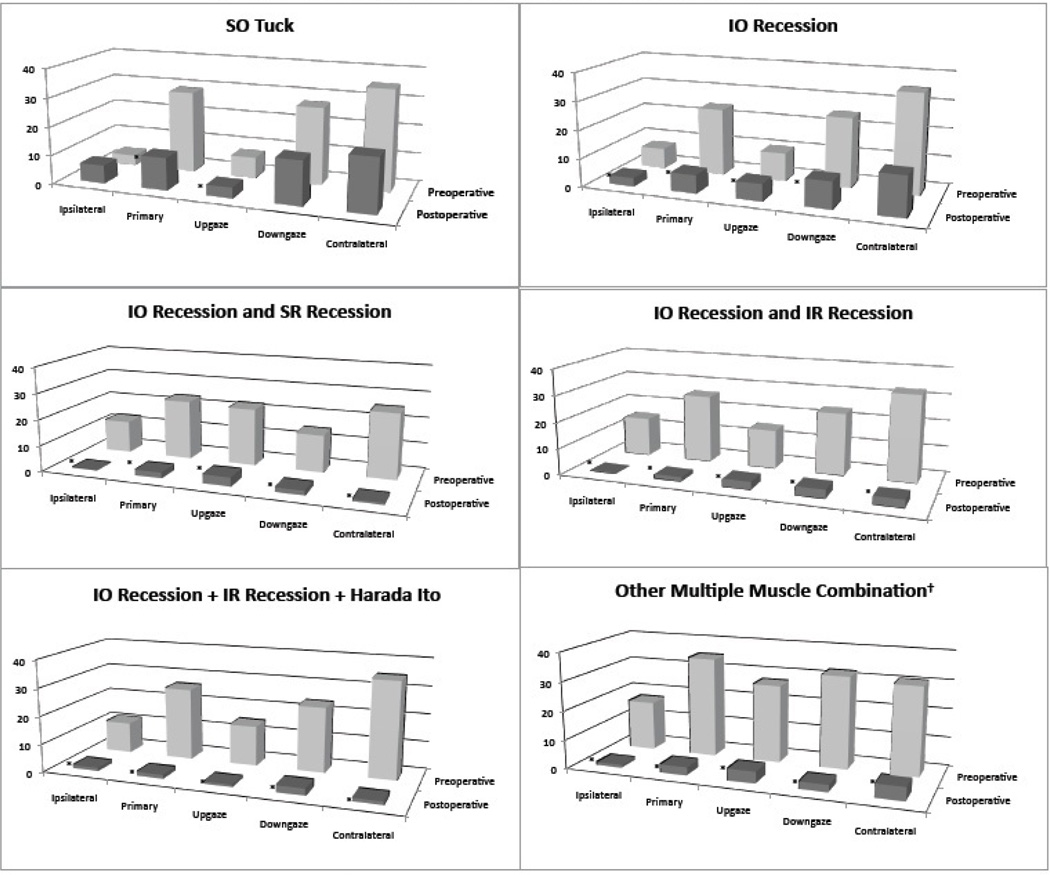
The preoperative vertical deviation in primary gaze and postoperative vertical deviation in primary gaze for each of the six different operations are shown in Figure 1. The mean angle of preoperative vertical deviation in primary gaze was 26.5 +/− 6.5 PD (range 20–42 PD) and the mean angle of postoperative vertical deviation, measured at the patient’s last postoperative appointment prior to either discharge or further treatment was 3.0 +/− 4.4 PD (range 0 to 22 PD). These findings are presented according to the procedure done for the first surgery in Table 2.
FIGURE 1. Preoperative and Postoperative Deviations (PDS).
* Indicates statistically signficant reduction in primary gaze deviation
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
† Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession, inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
TABLE 2.
Patient Data: Mean Primary Gaze Preoperative and Postoperative Deviation According to First Procedure Performed
| Procedure |
Preoperative Deviation (PDs) Mean (Range) |
Postoperative Deviation (PDs) Mean (Range) |
p-value |
|---|---|---|---|
| All Patients | 26.5 (20–45) | 3.0 (0–22) | <0.001 |
| SO tuck (n=3) | 28.6 (26–30) | 11.3 (0–22) | 0.002 |
| IO Recession (n=4) | 23.8 (20–30) | 6.5 (0–14) | 0.02 |
| IO Recession/SR Recession (n=8) | 23.5 (20–30) | 2.5 (0–6) | <0.001 |
| IO Recession/IR Recession (n=20) | 25.9 (20–45) | 1.6 (0–8) | <0.001 |
| IO Recession/IR Recession/Harado Ito (n=5) | 26.4 (20–35) | 1.8 (0–8) | <0.001 |
| Other multiple muscle combination*(n=5) | 35.0 (25–45) | 3.2 (2–5) | 0.005 |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
The number of surgeries required to achieve surgical success, according to the first surgery performed, are summarized in Table 4. One of the two patients who had an inferior oblique recession as their only operation had a late undercorrection for which a second operation was planned but not done after the patient was lost to follow-up. Additionally, one of the four patients who underwent an inferior oblique and inferior rectus recession plus Harada-Ito procedure as their only operation was overcorrected by 3 PD. Although both of these patients underwent only one surgery, neither was considered surgical successes by our definition. Twenty-five (56%) patients achieved primary gaze alignment between orthotropia and 6PD of undercorrection at last follow-up. Two of these patients required reoperation for a residual deviation in downgaze (n=1) and contralateral gaze (n=1), and were not considered a surgical success by our criteria. Twenty-three (51%) of cases met our criteria for surgical success with one operation. Of these, 22 (96%) were in patients who had two or more muscles operated on (Table 5).
TABLE 4.
Number of Surgeries Performed According to First Procedure Performed
| Number Of Cases (% of Total Cases For Each Procedure) | ||||
|---|---|---|---|---|
| Procedure at First Surgery | 1 Surgery | 2 Surgeries | 3 Surgeries | 4 Surgeries |
| SO Tuck (n=3) | 1 (33) | 2(66) | 0 | 0 |
| IO Recession (n=4) | 2 (50) | 1(25) | 1(25) | 0 |
| IO Recession/SR Recession (n=8) | 4 (50) | 2(25) | 1(12) | 1(12) |
| IO Recession/IR Recession (n=20) | 14 (75) | 5(25) | 1(5) | 0 |
| IO Recession/IR Recession/Harado Ito (n=5) | 4 (80) | 1(20) | 0 | 0 |
| Other multiple muscle combination*(n=5) | 2 (40) | 2(40) | 1(20) | 0 |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
TABLE 5.
Overall Success† with one Surgery According to Procedure Performed
| Procedure | Number (%) of Successful Results |
|---|---|
| SO Tuck (n=3) | 1(33%) |
| IO Recession (n=4) | 0 |
| IO Recession/SR Recession (n=8) | 4 (38%) |
| IO Recession/IR Recession (n=20) | 13 (65%) |
| IO Recession/IR Recession/Harado Ito (n=5) | 3 (60%) |
| Other multiple muscle combination (n=5) | 2 (40%) |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
Success criteria included (1) correction of the anomalous head posture, (2) primary position alignment between orthotropic and 6 PD of undercorrection, and (3) no reoperation required for residual deviations in any direction of gaze.
The highest success rate with one surgery belonged to the groups that had the combination of inferior oblique recession and contralateral inferior rectus recession (65%) and those who had this combination in addition to the Harada-Ito procedure (60%). Of the patients who required further treatment, 13 (72%) achieved success after a second surgery. No patients were overcorrected in the immediate postoperative period, which we defined as the first follow-up visit, usually the next day after surgery. Forty (89%) patients were aligned between orthotropia and 6 PD of undercorrection within this immediate postoperative period—“immediate success.” Five patients were undercorrected (mean 13.2 +/− 5.4 PD) in the immediate postoperative period. Of these, one was undercorrected by 8PD after an inferior oblique and inferior rectus recession and required no further treatment up to 26 months of follow-up. The other four were undercorrected by 10 to 22 PD after either inferior oblique recession or superior oblique tuck and required one to three more surgeries to achieve successful results. Between the first postoperative visit (within one week) and last follow up visit prior to further surgery (2 months to 16 years), 14 (31%) of the 40 patients with immediate success developed deviations >6 PD. Four patients were undercorrected (mean 14.6 +/− 6.7 PD) and 10 patients were overcorrected (mean 18.3 +/− 6.2 PD). These primary gaze deviation outcomes are presented for each procedure performed in Table 6.
TABLE 6.
Postoperative Primary Gaze Hypertropia Outcomes According to First Procedure Performed
| Number Of Cases (% of Total Cases For Each Procedure) | |||||
|---|---|---|---|---|---|
| Procedure | Immediate Undercorrection |
Late Undercorrection |
Late Overcorrection |
Immediate Success |
Late Success |
| SO Tuck (n=3) | 2(66) | 0 | 0 | 1(33) | 1(33) |
| IO Recession (n=4) | 2(50) | 1 (25) | 0 | 2(50) | 1(25) |
| IO Recession/SR Recession (n=8) | 0 | 0 | 4 (50) | 8 (100) | 4(50) |
| IO Recession/IR Recession (n=20) | 1(5) | 2(10) | 3(15) | 19(95) | 14(70) |
| IO Recession/IR Recession/Harado Ito (n=5) | 0 | 0 | 1 | 4(80) | 3(60) |
| Other multiple muscle combination (n=5) | 0 | 1(20) | 2(40) | 4(80) | 2(40) |
SO= superior oblique, IO= inferior oblique, SR= superior rectus, IR= inferior rectus
Multiple muscle combinations included superior oblique tuck and contralateral inferior rectus recession; superior oblique tuck and inferior oblique recession; superior oblique tuck, contralateral inferior rectus recession, and ipsilateral superior rectus recession; superior oblique tuck, inferior oblique recession and ipsilateral superior rectus recession; inferior oblique recession, ipsilateral superior rectus recession and contralateral inferior rectus recession.
The lowest success rates belonged to the single muscle surgeries. Of the subjects who had single muscle surgery, 14% had a successful outcome, with a mean 67% (17.3 PD) reduction in hypertropia. Of subjects who underwent simultaneous multiple muscle surgery, 58% met the criteria for a successful result, with a mean 92% (24.6 PD) reduction in primary gaze hypertropia.
Similar results were seen in down gaze as well. Average postoperative hypertropia in down gaze for the inferior oblique recession group and the superior oblique tuck group were 9.5 PD and 15.3 PD, respectively. All other surgery groups had average postoperative deviations of less than 6PD in down gaze. Of the 25 patients who had successful outcomes in primary gaze with one surgery, 13 were orthotropic in down gaze, and an additional 10 were within 6 prism diopters of orthotropia in down gaze.
All patients had resolution of their abnormal head position after one surgery. Preoperative torsion was recorded in 41 patients and was on average 8.4 +/− 3.8 degrees. Twenty-five (56%) of the subjects had horizontal deviations in primary gaze as well. Twenty (80%) had deviations less than 15 PD. Of the 25, 18 (72%) were exotropias, and 7 (38%) were esotropias. Of the 18 exotropias, 12 (67%), and, of the 7 esotropias, 3 (42%) resolved with vertical muscle surgery only. All of these patients had horizontal deviations less than 15 PD. Of the five patients who had horizontal deviations greater than 15 PD, three underwent horizontal muscle surgery for exotropia and two for esotropia. All three patients with exotropias were undercorrected in both vertical and horizontal deviation postoperatively, one of the two patients with esotropia was overcorrected, and one was orthotroptic in both vertical and horizontal gaze. Of the 25 patients with any horizontal deviation, 13 (52%) had successful results after one vertical muscle surgery; however, in the five patients with horizontal deviations greater than 15 PD who underwent horizontal muscle surgery only one (20%) was successful in both vertical and horizontal gaze with one surgery.
Discussion
SOP is the most common cause of vertical strabismus22 and the majority of patients will require surgical treatment. In a number of studies, single muscle surgery has been proven inadequate for the few patients within the series who had large hypertropias in primary gaze. Morad et al concluded that the standard ungraded 10mm inferior oblique recession as the primary weakening procedure was effective and safe, but the only two patients in their study that had hypertropias of greater than 20 PD remained undercorrected and symptomatic after inferior oblique recession alone.8 In a series of patients undergoing superior oblique tuck, Bhola et al found that all patients requiring reoperation had preoperative hypertropias greater than 15 PD in primary gaze.12 They concluded that isolated superior oblique tucking may not be sufficient to correct hypertropias greater 15 PD, and such cases should undergo additional muscle surgery. We found that isolated inferior oblique recession and isolated superior oblique tuck are not effective for primary gaze deviations greater than 20 PD. Of the 7 patients in our series who underwent a single oblique muscle surgery, only one had a successful outcome. Additionally, patients who underwent superior oblique tuck or inferior oblique recession had worse residual hypertropias in down gaze.
There are multiple techniques for weakening the inferior oblique muscle. Favardin and Nazarpoor reported 8 patients with hypertropia larger than 20 PD.7 Seven of those patients were aligned within 6 PD of orthotropia postoperatively and no patient was overcorrected with anterior transposition of the inferior oblique muscle. In our study isolated inferior oblique recession resulted in undercorrection in 75% of cases. It is likely that a stronger weakening effect and an associated antielevation mechanism result in more vertical correction in patients undergoing anterior transposition of the inferior oblique muscle in the above-mentioned study.
It has been recommended that patients with large vertical deviations in primary gaze be managed with combination of oblique and vertical rectus muscle surgery.23–25 In a study by Caca et al, 10 of 48 unilateral, congenital SOP cases had primary gaze hypertropias greater than 20PD. After a myectomy and concomitant inferior oblique disinsertion-recession in combination with an ipsilateral SR recession, 5 patients achieved results defined as “excellent” (0 to 3 PD), two achieved “good” results (4 to 7PD), and 3 had “poor” results (> 7PD) requiring reoperation.9 In a series of 12 patients with unilateral SOP by Saunders and colleagues, 9 subjects had preoperative hyperdeviations above 20 PD.14 They found that ipsilateral inferior oblique myectomy and superior oblique tuck was effective in their patients, all of who achieved fusion in practical fields of gaze. Hatz et al performed inferior oblique anteriorization and recession in combination with contralateral inferior rectus recession on patients with 20 PD.17 Of these patients, 17% were reported to have remaining hyperdeviations greater than 5 prism diopters. While postoperative deviations and reoperation rates were reported in all three studies, none defined success criteria and reported success rates. Furthermore, all of these results from the aforementioned studies are from case reviews in which a small subset of the patients who presented with large hypertropias underwent a combination of oblique muscle and vertical rectus muscle surgery.
In our study, patients who underwent multiple muscle surgeries on average had a greater reduction in hypertropia and a smaller reoperation rate than the single muscle surgery group. It is likely that single muscle surgery was chosen on those patients with a large amount of incomitance because of a concern for overcorrection in ipsilateral gaze. However, of the patients who had multiple muscle surgery, none required reoperation for overcorrection in ipsilateral gaze. Among the patients who underwent multiple muscle surgery, those that had inferior oblique and inferior rectus recessions, with or without a Harada-Ito procedure, were most likely to have successful outcomes. Unfortunately, postoperative torsion was not recorded for all patients, and it is unclear if those who underwent the Harada-Ito procedure had better improvement of torsional diplopia.
Helveston et al reported finding a horizontal deviation in 36% of superior oblique palsies, of which 68% resolved with vertical muscle surgery alone.26 Of the unilateral cases, 75% had exotropias, which they found were almost twice as likely to resolve post-operatively without horizontal rectus muscle surgery. In our patients, we found a much larger prevalence of horizontal deviations. Over half of our patients had horizontal strabismus. Similar to Helveston and colleagues, we found the majority (72%) of these to be exotropias, which resolved postoperatively more often than the esotropias (67% vs. 42%). Horizontal muscle surgery was only required in 5 of our subjects whose preoperative horizontal deviations exceeded 15 PD. In our series, the reoperation rate was higher in patients who required simultaneous horizontal muscle surgery than those who did not. The reoperations were more common in exotropic than esotropic patients (100% vs. 50%). Therefore, while horizontal deviations are more likely to be present in SOP patients who present with large hypertropias, mild to moderate horizontal deviations should not be a definite indication for horizontal muscle surgery. A higher threshold for horizontal muscle surgery should be used since most have a tendency to resolve with any vertical muscle procedure, and patients who undergo horizontal muscle surgery tend to require more surgery because of undercorrection or overcorrection of vertical and horizontal deviation.
The results of this study should be understood within the context of its limitations. First, this was a retrospective study, in which the surgical procedure may not have been completely standardized over time. The retrospective nature of the study precludes definitive conclusions regarding indications for various surgical procedures, given that it is subject to inherent selection and follow-up bias. Finally, missing data regarding post-operative torsion in many patients precludes careful analysis of the various surgical techniques’ ability to address torsional deviations.
Unilateral SOP patients with large deviations in primary gaze are challenging to treat. The most improvement in primary gaze hypertropia was achieved with multiple muscle surgery rather than single muscle surgery. Patients undergoing multiple muscle surgeries were more likely to achieve results between orthotropia and 6PD of undercorrection and less likely to require reoperation. Furthermore, SOP patients with large hypertropias are more likely to have horizontal deviations as well, and up to 15PD of horizontal strabismus is likely to resolve with vertical muscle surgery alone. Of the different multiple muscle combinations studied here, inferior oblique recession with contralateral rectus recessions resulted in lowest reoperation rate.
Footnotes
None of the authors have a financial or proprietary interest in any material or method mentioned.
Presented at the annual meeting of the Association of Research in Vision and Ophthalmology, 2012, Fort Lauderdale, FL
This study was conducted at the Jules Stein Eye Institute and Department of Ophthalmology, David Geffen School of Medicine at UCLA, Los Angeles, California
References
- 1.Parks MM. Isolated cyclovertical muscle palsy. AMA Arch Ophthalmol. 1958;60:1027–1035. doi: 10.1001/archopht.1958.00940081047008. [DOI] [PubMed] [Google Scholar]
- 2.Garnham L, Lawson JM, O’Neil D, et al. Botulinum toxin in fourth nerve palsies. Aust NZ J Ophthalmology. 1997;25:31–35. doi: 10.1111/j.1442-9071.1997.tb01272.x. [DOI] [PubMed] [Google Scholar]
- 3.Toosi SH, Von Noorden GK. Effect of isolated inferior oblique muscle myectomy in the management of superior oblique muscle palsy. Am J. Ophthalmol. 1979;88:602–608. doi: 10.1016/0002-9394(79)90522-1. [DOI] [PubMed] [Google Scholar]
- 4.Jones TW, Lee DA, Dryer JA. Inferior oblique surgery: Experience at the Mayo Clinic from 1960 to 1981. Arch Ophthalmol. 1984;102:714–716. doi: 10.1001/archopht.1984.01040030570020. [DOI] [PubMed] [Google Scholar]
- 5.Mulvihill A, Murphy M, Lee JP. Disinsertion of the inferior oblique muscle for treatment of superior oblique paresis. J Pediatr Ophthalmol Strabismus. 2000;37:279–282. [PubMed] [Google Scholar]
- 6.Duranoglu Y. Effectiveness of disinsertion-resection and tucking of the inferior oblique muscle in patients with unilateral long-standing superior oblique muscle palsy. J Pediatr Ophthalmol Strabismus. 2007;44:283–287. doi: 10.3928/01913913-20070901-02. [DOI] [PubMed] [Google Scholar]
- 7.Farvardin M, Nazarpoor S. Anterior transposition of the inferior oblique muscle for treatment of superior oblique palsy. J Pediatr Ophthalmol Strabismus. 2002;39:100–104. doi: 10.3928/0191-3913-20020301-10. [DOI] [PubMed] [Google Scholar]
- 8.Morad Y, Weinstock VM, Kraft SP. Outcome of inferior oblique recession with or without vertical rectus recession for unilateral superior oblique palsy. Binocul Vis Strabismus Q. 2001;18:1:23–28. [PubMed] [Google Scholar]
- 9.Caca I, Sahin A, Cingu A, et al. Residual symptoms after surgery for unilateral congenital superior oblique palsy. J AAPOS. doi: 10.3928/01913913-20110628-01. Epub ahead of print July 6, 2011. [DOI] [PubMed] [Google Scholar]
- 10.Wheeler J. Advancement of the superior oblique and inferior oblique muscles. Trans Am Ophthalmol Soc. 1934;32:237–244.1. [PMC free article] [PubMed] [Google Scholar]
- 11.Durnian JM, Marsh IB. Superior Oblique Tuck: It’s success as a muscle treatment for selected cases of superior oblique palsy. Strabismus. 2011;19:133–137. doi: 10.3109/09273972.2011.620058. [DOI] [PubMed] [Google Scholar]
- 12.Bhola R, Velez FG, Rosenbaum AL. Isolated superior oblique tucking: an effective procedure for superior oblique palsy with profound superior oblique underaction. J AAPOS. 2004;9:243–249. doi: 10.1016/j.jaapos.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Morris RJ, Scott WE, Keech RV. Superior oblique tuck surgery in the management of superior oblique palsy. J Pediatr Ophthalmol Strabismus. 1999;29:337–346. doi: 10.3928/0191-3913-19921101-04. [DOI] [PubMed] [Google Scholar]
- 14.Saunders RA. Treatment of superior oblique palsy with superior oblique tendon tuck and inferior oblique muscle myectomy. Ophthalmology. 1986;93:1023–1027. doi: 10.1016/s0161-6420(86)33627-3. [DOI] [PubMed] [Google Scholar]
- 15.Graf M, Lorez B, Eckstein A, et al. Superior oblique tucking with versus without additional inferior oblique recession for acquired trochlear nerve palsy. Graefs Arch Clin Exp Ophthalmol. 2010;248:223–229. doi: 10.1007/s00417-009-1188-1. [DOI] [PubMed] [Google Scholar]
- 16.Davis AR, Dawson E, Lee JP. Residual symptomatic superior oblique palsy. Strabismus. 2007;15:69–77. doi: 10.1080/09273970701404993. [DOI] [PubMed] [Google Scholar]
- 17.Hatz KB, Brodsky MC, Killer HE. When is isolated inferior oblique muscle surgery appropriate treatment for superior oblique palsy. Eur J of Ophthalmol. 2008;26:10–16. doi: 10.1177/112067210601600103. [DOI] [PubMed] [Google Scholar]
- 18.Simons BD, Saunders MD, Siatkoski MD, et al. Outcome of surgical management of superior oblique palsy: a study of 123 cases. Binocul Vis Strabismus Q. 1998;13:273–282. [PubMed] [Google Scholar]
- 19.Phillips PH, Hunter DG. Evaluation of ocular torsion and principles of management. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management. WB Saunders; 1999. pp. 52–72. [Google Scholar]
- 20.Mehta A. Chief complaint, history, and physical examination. In: Rosenbaum AL, Santiago P, editors. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia, PA: WB Saunders Co; 1999. pp. 3–21. [Google Scholar]
- 21.Nishimura JK, Rosenbaum AL. The long-term torsion effect of the adjustable Harada-Ito procedure. J AAPOS. 2002;6:141–144. doi: 10.1067/mpa.2002.123429. [DOI] [PubMed] [Google Scholar]
- 22.Plager DA. Superior oblique palsy and superior oblique myokymia. In: Rosenbaum AL, Santiago P, editors. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia, PA: WB Saunders Co; 1999. pp. 219–229. [Google Scholar]
- 23.Knapp P. Classification and treatment of superior oblique palsy. Am Orthoptic Journal. 1974;24:18. [PubMed] [Google Scholar]
- 24.Jampolsky A. Symposium on Strabismus; Transactions of the New Orleans Academy of Ophthalmology. St. Louis: CV Mosby; 1971. Vertical strabismus surgery; pp. 382–384. [Google Scholar]
- 25.Souza-Dias C. The surgical treatment of unilateral superior oblique palsy. Am Orthoptic Journal. 1992;42:16. [Google Scholar]
- 26.Helveston EM, Mora JS, Lipsky SN, et al. Surgical treatment of superior oblique palsy. Trans Am Ophthalmol Soc. 1996;94:315–334. [PMC free article] [PubMed] [Google Scholar]