Abstract
The New Vaccinations of Infants in Practice online survey in seven countries evaluated vaccination-related attitudes and concerns of parents of infants and health care providers (HCPs) who provide pediatric medical care. The survey showed that HCPs and parents were open to adding new vaccines to the immunization schedule, even if it requires co-administration with current vaccines or introduction of new office visits. Parental disease awareness campaigns would be helpful to achieve widespread acceptance of changes to vaccination schedules. In addition, HCPs would ideally provide disease education to parents to accompany recommendations for a new vaccine.
Electronic supplementary material
The online version of this article (doi:10.1007/s00431-012-1904-4) contains supplementary material, which is available to authorized users.
Keywords: Survey, Health care providers, Parents, Attitude, Infant, Immunization, Concomitant, Vaccinations, Vaccine, Meningococcal, Provider practices
Introduction
Over the last 20 years, a number of new childhood vaccines (including but not limited to pneumococcal conjugate vaccines, and meningococcal serogroup C and serogroups ACWY conjugate vaccines) have been introduced into national immunization schedules, and they continue to be incorporated into the routine infant vaccination programs in many countries. Such introduction of an additional vaccine in early infancy requires either (a) additional vaccination visits or (b) co-administration with other routine vaccines. Current vaccination practices typically involve co-administration of two or three vaccines concomitantly (depending on the country) for an infant visit. Adding yet another vaccine to the routine immunization schedule would likely increase this number to three or four injections per visit (depending on the country).
An increasingly crowded immunization calendar might lead health care providers (HCPs) and/or parents to balance the need to ensure that the child receives all necessary vaccines with their desires to minimize potential discomfort and/or distress for both child and parent. In addition, parental decisions on infant immunization may also be influenced by their knowledge of the infectious disease being prevented and the likelihood their child will become infected [2].
To comprehensively evaluate vaccination-related attitudes and concerns of parents of infants and the HCPs who provide their medical care, we conducted the New Vaccinations of Infants in Practice (New VIP) survey online in seven countries around the globe: Australia, Canada, France, Germany, Spain, Sweden, and the UK. In addition, we further sought relevant insights by using one vaccine in particular as an example. Since a vaccine against meningococcal serogroup B (MenB) is a likely candidate to be added to the routine infant immunization schedules in many countries, we chose this vaccine for the survey. We therefore used a profile of this vaccine as a practical example to further delineate factors influencing parental decisions on co-administering a new vaccine.
Method
The New VIP survey had two sections. One section involved parents who were highly involved with vaccination decisions of at least one infant between 0 to 23 months of age, and the other section involved HCPs who regularly administer vaccines to infants and children up to 2 years of age. The survey was conducted between 5 September and 1 November 2011.
For the purpose of this report, key findings from the seven countries were grouped together into a combined analysis. All respondents were recruited by email invitation from Ipsos Healthcare databases of HCPs and parents. All respondents worked outside the pharmaceutical, marketing/advertising, and market research industries. Participating HCPs and parents received an industry-standard honorarium to complete the survey. Both the parent and the HCP questionnaires were pretested in qualitative and/or quantitative pilot studies. Surveys were initially developed in English and subsequently translated by professional translators into native languages for non-English-speaking countries.
Parental and HCPs’ attitudes on fever associated with vaccinations and their attitudes toward using antipyretics to prevent or treat fevers were also assessed but are not included in this publication (results to be published separately).
Parent survey
The 20-min parent questionnaire was comprised of 47 closed-ended questions that were completed online. Based on answers to screening questions, parents went on to complete the main part of the questionnaire if they met the following criteria: (a) they were between 20 and 50 years of age, (b) there were two or more people in the household, (c) there was at least one child between 0 and 23 months of age (parents with multiple children responded with respect to their youngest child), (d) the parent was completely or closely involved in vaccine decision making for their youngest child, and (e) their child had received at least one vaccination for any disease or would be vaccinated in the future.
A total of 4,946 parents agreed to participate and underwent screening for survey eligibility. Country-specific quotas for parental age and geography were employed to match census data for each country and to remove potential convenience sample bias. Overall, 1,884 of 4,946 (38 %) parents who were initially screened failed to meet survey criteria and were excluded, and 602 (12 %) initially qualified but then abandoned the survey prior to completion. Of those 38 % who were excluded from the survey, the main reason for exclusion was that the parent had no child between 0 and 23 months of age (89 % of such terminations). Thus, a total 2,460 (50 %) parents completed the survey.
The main questionnaire (see online supplement) addressed several broad categories:
General beliefs toward childhood vaccinations overall and attitudes and perceptions of vaccine efficacy and safety
Attitudes toward co-administration of new infant vaccines, including preferences for maximum number of vaccine injections per office visit, factors influencing decision to vaccinate their child, and preferences for adding a new vaccine to infant vaccination schedule
Knowledge of and attitudes toward meningococcal disease (a disease for which many countries may soon adopt a new vaccine (against serogroup B) into many routine immunization schedules) as well as views and perspectives on such vaccination
Health care provider survey
The 30-min online survey involved a multi-section questionnaire. Country-specific quotas were employed for the type of practice (solo/group) and practice setting (private office/public health clinic) in order that the survey population in each country was generally reflective of the types of practitioners typically involved in pediatric vaccinations (i.e., pediatricians, general practitioners, and nurses, depending on the country). In addition, quotas for age, gender, and geography, based on publically available data, were used to remove potential convenience sample bias and make sure HCPs sampled were reflective of the individual countries.
A total of 1,939 HCPs initially agreed to participate in the survey and underwent screening for eligibility. To be eligible, HCPs (a) had to treat a minimum number of total patients per month (varying between ≥70 to ≥150 patients depending on specialty and country), (b) had to treat a minimum proportion of patients per month who were aged between 0 and 24 months (varying between 10 and 40 % depending on specialty and country), (c) had to recommend or discuss pediatric vaccines with parents, (d) had to spend a minimum proportion of their professional time in direct patient care (varying from 60 to 70 %, depending on country), (e) were in practice for at least 3 and no more than 35 years, and (f) were not involved in pediatric clinical trials nor employed in the vaccines industry. Additional eligibility criteria were based on the health care system of each individual country and included practice location (office or public clinic) and the practice setting (solo or group) where the HCP spends most of his/her time seeing patients.
Based on their responses to screening questions, 886 (46 %) HCPs failed to meet survey criteria and were excluded, and 328 (17 %) initially qualified but abandoned the survey before completion. Of the 46 % who were excluded, the top two main reasons for such exclusion were (1) that their primary practice location was not typical for their respective country and (2) that they saw too few patients between 0 and 24 months. Thus, a total of 725 (37 %) HCPs completed the survey.
The main part of the questionnaire for HCPs involved a total of 65 closed-ended questions. Specific questions (see online supplement) pertinent to this article addressed several broad themes:
General beliefs toward childhood vaccinations
Factors influencing HCPs’ decision to recommend a new infant vaccine to parents
Attitudes toward co-administration of infant vaccines and factors impacting their decision to administer multiple vaccines per visit
Weighting and statistical analysis
Where applicable, data represent the combined percentage of parents/HCPs selecting the top two (of six total) categories, specifically categories 5 and 6, based on a 6-point scale (ranging from 1 = extremely unlikely [strongly disagree, not a problem, or not important] to 6 = extremely likely [strongly agree, serious problem, or very important]).
To generalize survey results to the respective national populations, results for each country were postweighted (rim-weighting method [3]) using age and geography (based on census information) for parents, and gender, age, and geography within specialty (based on EphMRA or census information) for HCPs. The combined country data for each of HCPs and parents were then postweighted according to population statistics in each country to arrive at one “total” HCP and one “total” parent response for the seven countries, combined together. After applying both weights, the overall weighting efficiency was 88 % for parents and 87 % for HCPs.
The maximum margin of error for estimates of simple percentages at a 95 % confidence level for the combined analysis was ±1.98 % for a sample size of 2,460 parents and ±3.64 % for a sample size of 725 HCPs. McNemar’s test was used to determine the statistical significance of differences in proportions. All differences were considered significant at the p < 0.05 level.
A maximum differential technique was utilized to measure the relative preference or importance of multiple factors [9]. Respondents were presented with two of four factors at a time (total of six combinations) and asked to choose the more important factor. A Hierarchical Bayes estimation [8] was then used to compute individual-level weights for each item under the logit rule. For ease of interpretation, the results were converted to ratio-scaled probabilities ranging from 0 (representing least/worst) to 100 (representing optimal most/best). Thus, an item with a score of 70 is twice as preferred or important as an item with a score of 35.
Results
Demographic characteristics
Overall, 2,460 parents of infants and 725 pediatric HCPs responded to the survey. Table 1 summarizes the number of parents and the number and types of HCPs surveyed in each country, as well as the overall demographic characteristics. Percentages and numbers shown are weighted to reflect demographics for each country and for the population sizes of the seven-country total.
Table 1.
Number of parents and number and types of HCPs surveyed in each country
| Australia | Canada | France | Germany | Spain | Sweden | UK | Total | |
|---|---|---|---|---|---|---|---|---|
| Parents | 201 | 445 | 402 | 403 | 402 | 203 | 404 | 2,460 |
| Total HCPs | 105 | 100 | 100 | 100 | 100 | 80 | 140 | 725 |
| General practitioner | 90 | 20 | 20 | 20 | – | 38 | 70 | 258 |
| Pediatrician | – | 80 | 80 | 80 | 100 | 41 | – | 381 |
| Nurse | 15 | – | – | – | – | 1 | 70 | 86 |
Overall, HCPs had a close gender split (female, 55 %; male, 45 %), with a mean age of 48 years, practiced medicine for a mean of 17.1 years, spent 91 % of their professional time in direct patient care, were primarily in group rather than solo practice (63 vs. 37 %), spent most of their time in a private office setting (87 %), treated a mean of 467 patients per month (48 % between birth and 24 months), and virtually all (99 %) recommended vaccines according to the official national schedule
Overall, parents were predominately female (71 %) with a mean age of 34 years, had a mean of four people per household and two children <18 years. Approximately 62, 33, and 11 % of parents with the first, second, and third child, respectively, between ages 0–23 months; 56 and 44 % of parents were either entirely responsible or closely involved in vaccination decisions for their youngest child, and all parents reported that their child had received/planned to receive at least one vaccine (100 %)
Parent survey
General beliefs toward childhood vaccinations
A majority of parents (84 %) accepted the vaccines recommended in the national schedules, and most (76 %) accepted the vaccines to be administered according to the recommended immunization calendar (Fig. 1). Further, 67 % would be as willing to accept these vaccinations even if they had to pay for the vaccinations out of pocket.( Q19 p42, Q19a p43 ) Overall, 75 % of parents agreed (Fig. 2) that they trusted their HCP’s judgments about vaccine choices, and 70 % were confident in the safety of routinely recommended vaccines.( Q22 p55 ) Only 10 % of parents believed that their child received too many vaccines (needlesticks) at a given office visit,( Q23 p69 ) but 18 % of parents claimed that if a vaccine was not in the official schedule, it is not worth getting.
Fig. 1.
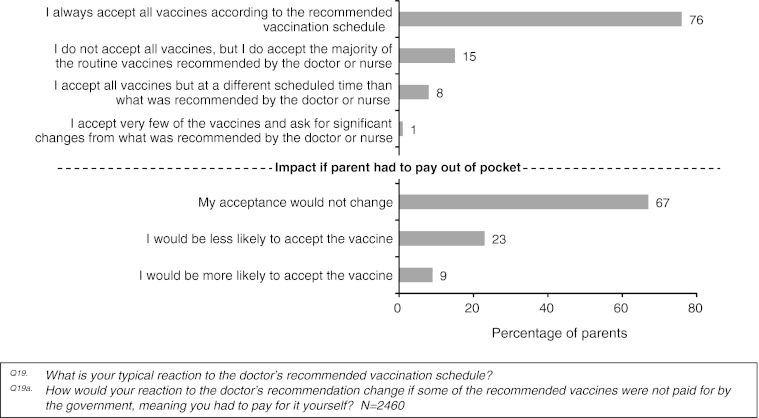
Typical reaction of parents to the doctor’s recommended vaccination schedule
Fig. 2.
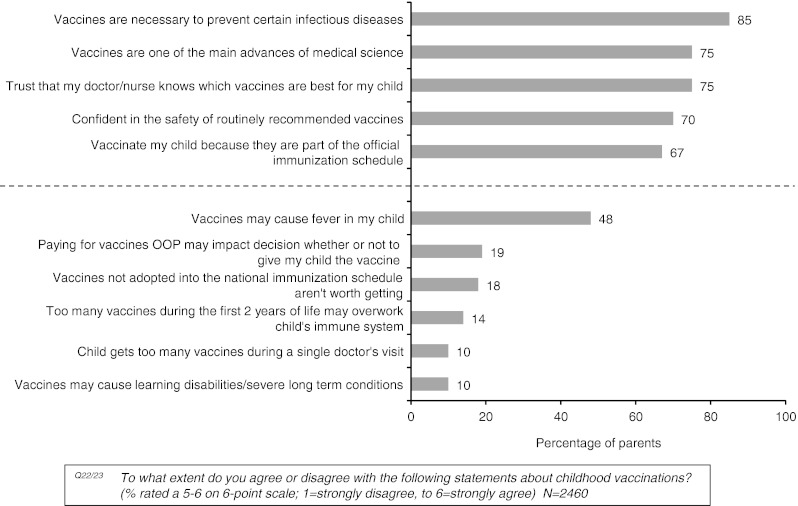
Summary of general parental beliefs regarding childhood vaccines (N = 2,460)
Attitudes toward co-administration of infant vaccines
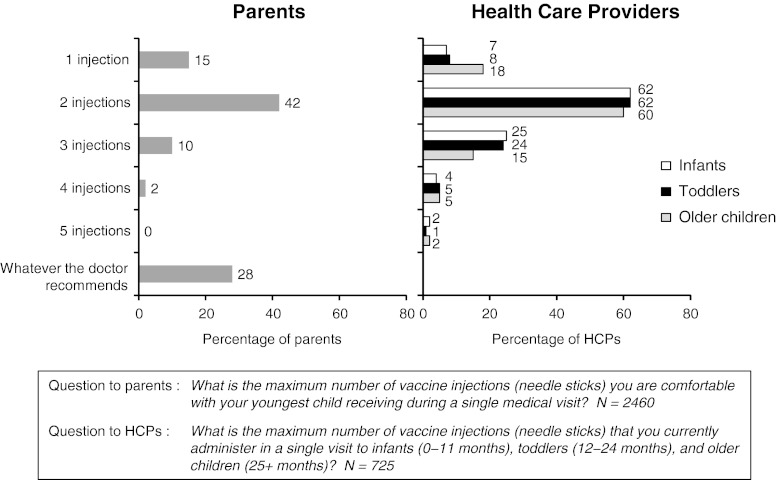
When asked what was the maximum number of vaccine injections they were comfortable with their child receiving during a single medical visit, about 28 % of parents indicated that they were comfortable with following their HCPs’ recommendations during a given office visit (Fig. 3), while 15 % were comfortable with only one injection and 42 % with two injections.
Fig. 3.
Maximum number of vaccine injections parents were comfortable with their child receiving during a single medical visit
The most notable reasons (top 3 ranking) influencing parents’ comfort level with the maximum number of injections per office visit for their child were (1) avoiding too much pain and discomfort (64 %) and (2) ensuring their child received all needed vaccines (61 %).( Q21 p45 ) However, 38 % were concerned about “overworking” their child’s immune system.
The example of a new MenB vaccine: parental knowledge about the disease and views on the vaccine
Before reviewing disease information, 55 % of parents agreed that invasive meningococcal disease could lead to death, 60 % to rapidly worsening symptoms, and 63 % to permanent or disabling effects.( Q27a p90 ) When asked at what age children are most at risk for contracting meningococcal disease, nearly equal proportions of parents either stated that they did not know (35 %) or (erroneously) thought 13 month- to 3-year olds were at greatest risk (30 %), while only 16 % correctly knew that 0–12-month olds are the age group at highest risk for contracting the disease.( Q26 p87 )
Overall, 61 % of parents were not sure whether their child may be at risk for types of meningitis not covered by routine vaccines, with 29 % believing their child could be at such risk.( Q30 p101 ) Moreover, fewer than 40 % of parents (900/2,460) knew whether their child had already received a meningococcal vaccine.( Q28 p100 )
After a brief exposure to disease information, the proportion of parents who stated that they would be highly likely to accept such vaccination of their child at 0–6 months of age against this disease if it was approved and recommended by their child’s HCP increased from 54 to 68 % after seeing this information.( Q42 p125 ) Exposure to disease information significantly augmented parental acceptance by increasing (1) the percentage of parents who would likely accept co-administration of this MenB vaccine with the currently recommended infant vaccines (31 to 37 %, respectively, p < 0.01) as well as (2) the percentage of parents who would schedule a separate office visit to receive the new vaccine by itself (37 to 41 %, respectively, p < 0.01).( Q39 p116; Q43a p128 ) At 89 % probability of importance, the primary factor influencing parental decisions about this vaccine for 0- to 6-month olds was the knowledge that children under 1 year of age are 8 (Sweden) to 25 (UK) times more likely (varying according to country) to get meningococcal disease than other age groups. In contrast, the fact there could be additional vaccinations at each medical visit had a 48 % probability of importance, the option to delay vaccination 27 %, and the potential for postvaccination fever 15 %.( Q47 )
HCP survey
General beliefs toward childhood vaccinations
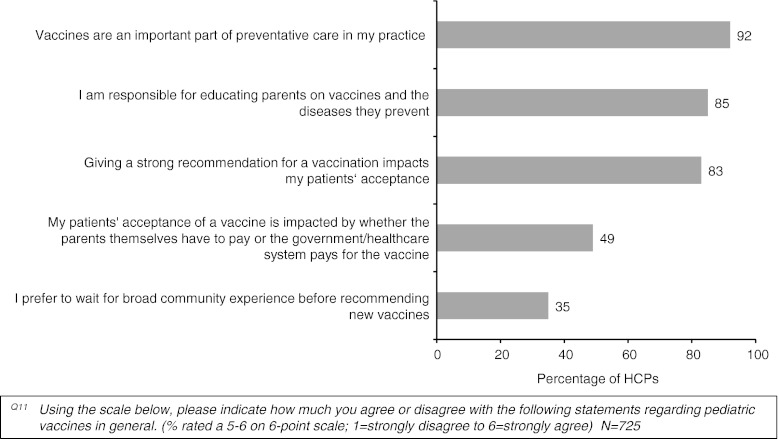
Overall, the vast majority of HCPs agreed that vaccines are an important part of preventive care and that HCPs play an important role in vaccine education and recommendation (Fig. 4).( Q11 p62 ) Furthermore, only 35 % of HCPs claimed that they would need to wait for broad community experience before recommending a new vaccine. The most important reasons among HCPs when making pediatric vaccine recommendations were the severity and/or lethality of the disease (84 %), and inclusion in the official schedule (65 %), while the incidence of the disease is much less of a factor according to the physicians’ expertise (39 %).( Q16 p84 )
Fig. 4.
Summary of general beliefs of HCPs with respect to pediatric vaccines
HCPs report that the most important reasons (top 3 ranking) that parents would give for choosing to not vaccinate their children were the beliefs that vaccines might be unsafe and may trigger serious long-term illnesses (80 %) and that vaccines might overload the immune system of children (53 %).( Q15 p76 ) Much less common were the beliefs that children might be getting too many vaccines, either at a given visit (18 %) or overall in the first 2 years of life (29 %).
Attitudes toward co-administration of new infant vaccines
HCPs were generally aligned with their respective official immunization schedules for infants (0–11 months) with respect to the maximum number of injections per visit. At the time of the survey, approximately 62 % were administering a maximum of two injections per visit for infants, and 25 % were administering up to three injections (which apparently depended upon immunization schedules and vaccine combinations available in that country) (Fig. 3).( Q5 p46 ) When asked which factors influenced their decision to administer multiple vaccines per visit, 83 % of HCPs said following the official immunization schedule was the main reason.( Q7 p52 ) Much less common and reported by only a minority of HCPs was the notion that one must vaccinate while the HCP has access to the patient (48 %) or a fear that the child may not return to the clinic (36 %).
The greatest concern or risk factor that HCPs considered when administering more than one vaccine during a single visit was their expectations of parental concern about their child’s pain and discomfort. Notably, this proportion of HCP responses was significantly greater than those who responded regarding their own concerns about their patients’ pain and discomfort (58 vs. 41 %).( Q8 p56 )
Discussion
Over the past two decades, the number of vaccinations for infants has more than doubled in most industrialized nations. With the development of additional vaccines and their potential implementation on the horizon, especially into increasingly crowded immunization schedules, additional vaccination visits or co-administration of multiple vaccines will be needed in order to accommodate such medical advances. In this context, it is helpful to confirm the attitudes toward new vaccinations among parents of young children, as well as among the HCPs who will recommend and/or administer these vaccines. Whereas other surveys have focussed on attitudes to vaccination at the national level, for example in Italy [1], Belgium [10], Germany [6], the Netherlands [5], and the USA [7], this New VIP survey represents the first comprehensive, multinational investigation of contemporary attitudes and preferences toward vaccination and its related issues.
The New VIP survey illustrates the interdependence among parents, HCPs, and decision-making bodies with respect to infant immunizations in general. Three quarters of parents accept all of the vaccines according to their country’s recommended immunization schedule (and a large majority cite it as a top reason to vaccinate), and a similar proportion of parents trust their doctors’ or nurses’ recommendations regarding vaccinations. Fortunately, for the remaining 25 % of parents whose education will be an important factor in achieving high rates of vaccine coverage, 85 % of HCPs recognize that they are responsible for educating parents on vaccines and the diseases they prevent, and they also recognize that their strong recommendation impacts parental acceptance of vaccination. A study in Italy [1] found that 82.7 % of pediatricians routinely educate parents about the recommended vaccinations for their children, while 95 % of German parents “regard their pediatrician as the most important source of information regarding immunization” [6], and US parents who hesitated to have their child vaccinated tended to follow the physician’s recommendation [7].
It is interesting then that HCPs rate the inclusion of a vaccine on the official schedule as only the second-highest-rated factor impacting their decision to recommend a new vaccine; the severity/lethality of the prevented disease was actually rated as the main factor by a wide margin. One might consider the decision process of the surveyed HCPs quite appropriate because it is, in fact, those diseases that are perhaps the most difficult to treat adequately that one should most attempt to prevent. In fact, physicians rated disease severity far higher than they did either the disease incidence or their need to have personal experience with the disease. Furthermore, a large majority of physicians did not feel that they needed to wait for broad community experience before they were ready to recommend new vaccines to their patients.
Governmental bodies and health care policy makers who formulate recommendations as part of national immunization programs, in turn, are reciprocally influenced by the guidance from the medical community, typically via specific expert advisory panels as well as by the likelihood that the general public will accept a potential new vaccine. Furthermore, such vaccination recommendations are typically accompanied by public funding, which is often justified by the knowledge that parents would be willing to pay for such vaccines themselves, if need be. Hence, it is comforting to see that a majority of parents would be equally accepting of a vaccine even if they had to pay out of pocket.
It is also notable that while parents tend to cite inclusion on the vaccination schedule as a key reason to vaccinate, the converse is apparently not true. Specifically, lack of inclusion of a vaccine on the immunization calendar was noted by only a small fraction of respondents to indicate that the vaccine would not be worth getting.
In the countries surveyed, infants typically received a PCV vaccine as well as vaccination against DTaP, IPV, HepB, and Hib in different combinations, typically resulting in two or three injections per infant visit. Parents and HCPs felt most comfortable with the number of injections per visit that corresponded to the current official recommendations and currently available vaccine combinations in their country. Our data are consistent with those from Belgium [10] and the Netherlands [5] where most parents do not want their child to receive more than two injections per visit, so if a new vaccine were then to be introduced into the schedule, it would most likely require either (a) concomitant administration with the existing vaccinations during these HCP visits or (b) additional office visits for vaccination. Based on the survey responses, parents seem to balance, relatively equally, two primary factors against each other: the wish to ensure that the child receives the necessary vaccinations vs. the desire to avoid too much discomfort at any given office visit.
This survey has revealed that any theoretical “overworking” of a child’s immune system resulting from too many vaccines at once is only a concern for 38 % of parents, and such a view among parents about this topic was even less of an issue than the HCPs’ perceptions of such parental concern. This contrasts with German parents, of whom only 21 % were worried about overloading their child’s immune system [8]. However, a majority of HCPs perceived the main reason for parents choosing not to vaccinate their child was the belief that the vaccines may be unsafe and could trigger serious long-term diseases, but over 91 % of German parents trust that recommended vaccines are safe [6]. Yet, HCPs are ideally positioned to understand the clinical data demonstrating vaccine safety and efficacy and to therefore provide reassurance and strong recommendations for a vaccine to the parents.
Finally, using the currently relevant example of an upcoming new vaccine, even while some parents may have been confused about which vaccines their children have already received, this survey revealed that even a brief, objective education of the parents on this vaccine-preventable disease could significantly increase their likelihood of adoption of a new vaccine. Furthermore, a nearly equal number of parents would be in favor of additional, separate office visits to accommodate the new vaccinations as would be the number of parents who would wish to keep the current number of office visits and administer the new vaccine concomitantly with those currently on the schedule.
It should be noted that this survey has a number of limitations. This questionnaire included realistic, but hypothetical, scenarios, and it is not possible to ascertain whether parents or HCPs would actually follow through with their stated intentions. As with any survey, our findings may be influenced by the recall bias and response bias of the surveyed individuals. This may result in a possible tendency of some survey participants to overstate their experience or interest in a desire to please the surveyor. Finally, our online survey involved parents and HCPs with internet access, implying a higher socioeconomic and educational level; this potential selection bias might impact the generalizability of our result to the whole population, although our data are consistent with those of an internet-based survey of German parents [6]. The survey of highly educated Dutch parents indicated that their unwillingness to accept new vaccines was due to lack of education about them [5].
In conclusion, these survey findings suggest that a population-wide effort to improve global awareness of a specific vaccine-preventable disease would be required for any successful vaccine initiative, and these data may be useful for public health officials and policy makers as they update existing infant immunization schedules to accommodate new vaccines. Notably, both HCPs and the public in general seem to be open to the introduction of new vaccinations (especially for those that help to protect against diseases with a high degree of severity or mortality) and their inclusion on the immunization calendar, even if it requires co-administration with current vaccines or introduction of new office visits. However, not only would public disease awareness campaigns be helpful to achieve widespread acceptance of changes to vaccination schedules, but also HCPs would ideally provide disease education to their patients’ parents to accompany their strong professional recommendations for a new vaccine.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 255 kb)
Acknowledgments
Novartis Vaccines and Diagnostics, Cambridge, MA, provided funding for this research and manuscript. One author (B. Sudovar) from Novartis, in close collaboration with Ipsos Healthcare (Plymouth Meeting, PA), and the other authors developed both HCP and parent online questionnaires. Ipsos Healthcare subsequently conducted the surveys and tabulated the results. The authors were involved in all stages of the research, including data analysis/interpretation, and contributed to the drafting and/or revising of the publication for important intellectual content. The final version was approved for publication by all authors. The authors thank Jan S. Redfern, PhD, Redfern Strategic Medical Communications, Inc., Goshen, NY, USA, for writing assistance and Keith Veitch (Novartis Vaccines and Diagnostics) for editorial support. The manuscript was prepared according to the International Society of Medical Publication Professionals’ Good Publication Practice for Communicating Company-Sponsored Medical Research—the GPP2 Guidelines [4].
References
- 1.Anastasi D, Di Giuseppe G, Marinelli P, Angelillo IF. Paediatricians knowledge, attitude, and practices regarding immunizations for infants in Italy. BMC Publ Health. 2009;9:463. doi: 10.1186/1471-2458-9-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bedford H, Lansley M. More vaccines for children? Parents’ views. Vaccine. 2007;25:7818–23. doi: 10.1016/j.vaccine.2007.08.057. [DOI] [PubMed] [Google Scholar]
- 3.Deming WE, Stephan FF. On a least squares adjustment of a sampled frequency table when the expected marginal totals are known. Ann Math Stat. 1940;11:427–444. doi: 10.1214/aoms/1177731829. [DOI] [Google Scholar]
- 4.Graf C, Battisti WP, Bridges D, Bruce-Winkler V, Conaty JM, Ellison JM, Field EA, Gurr JA, Marx M-E, Patel M, Sanes-Miller C, Yarker YE. Research methods & reporting. Good publication practice for communicating company sponsored medical research: the GPP2 guidelines. BMJ. 2009;339:b4330. doi: 10.1136/bmj.b4330. [DOI] [PubMed] [Google Scholar]
- 5.Hak E, Schönbeck Y, De Melker H, Van Essen GA, Sanders EAM. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine. 2005;23:3103–3107. doi: 10.1016/j.vaccine.2005.01.074. [DOI] [PubMed] [Google Scholar]
- 6.Heininger U. An internet-based survey on parental attitudes towards immunization. Vaccine. 2006;24:6351–6355. doi: 10.1016/j.vaccine.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 7.McCauley MM, Kennedy A, Basket M, Sheedy K. Exploring the choice to refuse of delay vaccines: a national survey of parents of 6- through 23-month-olds. Acad Pediatrics. 2012;12:375–383. doi: 10.1016/j.acap.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Orme B (2000) Hierarchical Bayes: why all the attention? Sawtooth Software, Sequim, WA, www.sawtoothsoftware.com/download/techpap/hbwhy.pdf. Accessed 29 May, 2012
- 9.Sawtooth Software, Inc. (2007) Sawtooth Software technical paper series: the MaxDiff/Web V6.0 technical paper. www.sawtoothsoftware.com/download/techpap/maxdifftech.pdf. Accessed Jan 3, 2012.
- 10.Theeten H, Hens N, Aerts M, Vandermeulen C, Roelants M, Hoppenbrouwers K, Van Damme P, Beutels P. Common attitudes about concomitant vaccine injections for infants and adolescents in Flanders. Belgium Vaccine. 2009;27:1964–1969. doi: 10.1016/j.vaccine.2009.01.096. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 255 kb)