The second-generation 320–detector row CT scanner provided excellent image quality over a wide range of body sizes and heart rates at lower radiation doses compared with a previous-generation CT scanner.
Abstract
Purpose:
To (a) use a new second-generation wide-volume 320–detector row computed tomographic (CT) scanner to explore optimization of radiation exposure in coronary CT angiography in an unselected and consecutive cohort of patients referred for clinical purposes and (b) compare estimated radiation exposure and image quality with that from a cohort of similar patients who underwent imaging with a previous first-generation CT system.
Materials and Methods:
The study was approved by the institutional review board, and all subjects provided written consent. Coronary CT angiography was performed in 107 consecutive patients with a new second-generation 320–detector row unit. Estimated radiation exposure and image quality were compared with those from 100 consecutive patients who underwent imaging with a previous first-generation scanner. Effective radiation dose was estimated by multiplying the dose-length product by an effective dose conversion factor of 0.014 mSv/mGy ⋅ cm and reported with size-specific dose estimates (SSDEs). Image quality was evaluated by two independent readers.
Results:
The mean age of the 107 patients was 55.4 years ± 12.0 (standard deviation); 57 patients (53.3%) were men. The median body mass index was 27.3 kg/m2 (range, 18.1–47.2 kg/m2); however, 71 patients (66.4%) were overweight, obese, or morbidly obese. A tube potential of 100 kV was used in 97 patients (90.6%), single-volume acquisition was used in 104 (97.2%), and prospective electrocardiographic gating was used in 106 (99.1%). The mean heart rate was 57.1 beats per minute ± 11.2 (range, 34–96 beats per minute), which enabled single-heartbeat scans in 100 patients (93.4%). The median radiation dose was 0.93 mSv (interquartile range [IQR], 0.58–1.74 mSv) with the second-generation unit and 2.67 mSv (IQR, 1.68–4.00 mSv) with the first-generation unit (P < .0001). The median SSDE was 6.0 mGy (IQR, 4.1–10.0 mGy) with the second-generation unit and 13.2 mGy (IQR, 10.2–18.6 mGy) with the first-generation unit (P < .0001). Overall, the radiation dose was less than 0.5 mSv for 23 of the 107 CT angiography examinations (21.5%), less than 1 mSv for 58 (54.2%), and less than 4 mSv for 103 (96.3%). All studies were of diagnostic quality, with most having excellent image quality. Three of four image quality indexes were significantly better with the second-generation unit compared with the first-generation unit.
Conclusion:
The combination of a gantry rotation time of 275 msec, wide volume coverage, iterative reconstruction, automated exposure control, and larger x-ray power generator of the second-generation CT scanner provides excellent image quality over a wide range of body sizes and heart rates at low radiation doses.
© RSNA, 2013
Supplemental material: http://radiology.rsna.org/lookup/suppl/doi:10.1148/radiol.13122621/-/DC1
Introduction
Coronary computed tomographic (CT) angiography is a robust and established noninvasive imaging tool (1,2), with high sensitivity and high negative predictive value (3,4). The high negative predictive value is particularly effective and safe for the exclusion of significant coronary artery disease in patients presenting to the emergency department with acute chest pain (5–7). However, the clinical benefit of coronary CT angiography has been tempered by concerns of future malignancy induced by the radiation exposure (8,9). Technologic advances and practice patterns have evolved to not only reduce radiation exposure but also to optimize and improve image acquisition (10).
Wide-volume scanners with 320 detector rows and up to 16 cm of cranial-caudal coverage enable whole-heart coverage at one acquisition time point (within one heartbeat or volume), which eliminates “stair-step” or misalignment artifacts (11–13) but also permits uniform attenuation when evaluating the coronary arteries, when analyzing myocardial perfusion defects (14,15), or when measuring contrast attenuation gradients across atherosclerotic lesions (16). Radiation doses are lower with wide-area detector scanners owing to shorter scanning times and reduction of redundant radiation from either overlapping of sequential axial scans or helical oversampling (13). In addition, total iodinated contrast material volume can be decreased to as low as 40 mL at 5 mL/sec in patients with normal cardiac output (17).
We hypothesized that the combination of a faster gantry rotation, wide volume coverage, iterative reconstruction, automated exposure control, and larger power generator can be used to perform diagnostic-quality coronary CT examinations with low radiation exposure. The specific aims of this study were to (a) use a new second-generation wide-volume 320–detector row CT scanner to explore optimization of radiation exposure in coronary CT angiography in an unselected and consecutive cohort of patients referred for clinical purposes and (b) compare estimated radiation exposure and image quality with those from a cohort of similar patients who underwent imaging with the previous first-generation CT system.
Materials and Methods
Study Design
This prospective study was performed at a single referral center and is registered at ClinicalTrials.gov (registration no. NCT01621594). The institutional review board approved the study, and all patients provided written consent. A separate cohort of consecutive patients who underwent imaging with a previous first-generation 320–detector row CT scanner were retrospectively analyzed to serve as a historical control group (National Institutes of Health Intramural Protocol 11-H-N043).
Study Cohort
Inclusion criteria for this study consisted of patients at least 18 years old who were clinically referred for contrast material–enhanced coronary CT angiography. Patients were excluded if they were pregnant or if their estimated glomerular filtration rate was less than 30 mL/min/1.73 m2 body surface area (18); however, no patients met either exclusion criterion. All patients were consecutive and prospectively enrolled during a 12-week period from July to October 2012 regardless of body size, heart rate, heart rhythm, previous cardiovascular history, or clinical indication. The retrospective historical control group consisted of consecutive patients who underwent coronary CT angiography with a previous first-generation 320–detector row CT system from January to April 2010.
CT Parameters
Patients underwent axial imaging with a second-generation, 320 × 0.5-mm detector row CT unit (Aquilion ONE ViSION Edition; Toshiba Medical Systems, Otawara, Japan) with a gantry rotation time of 275 msec. Images were reconstructed with a 512 × 512 matrix, 0.5-mm-thick sections, and 0.25-mm increments by using kernel FC03, iterative reconstruction AIDR3D (Toshiba Medical Systems) standard, and asymmetric cone beam reconstruction (19). Tube potential and tube current were determined with use of automatic exposure control (SUREExposure3D, Toshiba Medical Systems) on the basis of the x-ray attenuation on anterior-posterior and lateral scout images and the reconstruction kernel (20). Iopamidol (Isovue 370, Bracco Diagnostics, Princeton, NJ; 370 mg of iodine per milliliter) was injected via an antecubital vein at 5 mL/sec by using a triphasic protocol of, in general, 49 mL of contrast material followed by 20 mL of a 30% contrast material–70% saline mixture and 50 mL of saline. Breath-hold contrast-enhanced images were triggered within 1 second of a threshold of 400 HU monitored by using bolus tracking within the descending aorta. Bolus-tracking images were initiated 16 seconds after the start of contrast material administration. The diastolic exposure widow of the prospectively electrocardiographically (ECG) triggered scan was automatically determined by the scanner based on the heart rate during a breath-hold exercise just before contrast material administration. The heart rhythm was continuously monitored by the scanner, and, in the event of an arrhythmia during an ECG-gated scan, the exposure window was automatically widened to include the next beat to provide more available reconstruction phases at the expense of increased radiation exposure. Patients received metoprolol orally (maximum, 100 mg) and/or intravenously (maximum, 30 mg) at the discretion of the attending cardiovascular imager. Patients also received 0.4 mg of sublingual nitroglycerin for coronary vasodilation.
The CT parameters from the retrospective portion of the study were similar (Appendix E1 [online]).
Estimation of Radiation Dose
Effective radiation doses were estimated by multiplying the dose-length product reported by the scanner by a conversion factor of 0.014 mSv/mGy ⋅ cm according to standard methodology outlined in the most recent guidelines (10,21). The volumetric CT dose index (CTDIvol) was recorded for each study as reported by the scanner based on a 32-cm phantom. Because effective radiation dose is estimated from a standard-size reference adult, this value does not accurately describe an individual’s dose owing to differences in sex, body size, and age. Therefore, to help account for differences in patient size, the size-specific dose estimate (SSDE) was calculated on the basis of the individual effective patient diameter (or body size) as measured from the scout images (22).
Analysis of Image Quality
Two experienced cardiovascular imaging physicians (M.Y.C. and S.M.S., with 8 and 4 years of experience, respectively) evaluated image quality independently and in a blinded fashion by using a four-point scale over four individual categories (coronary motion artifact, image noise, contrast material enhancement, and fine detail), where 4 = excellent, no significant artifact; 3 = good, mild artifact; 2 = acceptable, moderate artifact present but images are still interpretable; and 1 = unevaluable, with severe artifacts rendering diagnostic interpretation not possible. The evaluation of coronary motion artifact focused on apparent blurring of the coronary artery contours. Image noise was evaluated on the basis of the visual appearance of image speckle or graininess. The assessment of contrast material enhancement involved evaluation of the subjective attenuation differences between the coronary artery and adjacent myocardium or epicardial fat. Fine detail was represented by visualization of small structures such as coronary arteries smaller than 1.5 mm in diameter or coronary plaque characterization. The reported image quality score is the mean between the two readers.
Statistical Analysis
Statistical analyses were performed with software (MedCalc 12.0; MedCalc Software, Mariakerke, Belgium). Data are presented as means ± standard deviations or as medians and interquartile ranges (IQRs). The Kolmogorov-Smirnov test was used to test whether data were normally distributed. The McNemar test was used to assess differences between paired proportions. The χ2 test was used to evaluate proportions of categoric data. The Student t test was used to compare continuous variables, and the Mann-Whitney U test was used to compare nonparametric variables. Interobserver agreement between the two readers with regard to subjective image quality assessment was evaluated with the Cohen κ test by using the following scale: κ values of less than 0.20 were indicative of poor agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, excellent agreement.
Results
Study Population
In total, 107 consecutive clinical coronary CT angiography examinations were evaluated with the new second-generation scanner. Table 1 describes the clinical characteristics of the 107 patients in this study. The mean patient age (±standard deviation) was 55.4 years ± 12.0 (range, 27–82 years); 57 of the 107 patients (53.3%) were men. In most cases (97 of 107 patients, 90.6%), the clinical indication for coronary CT angiography was the detection of coronary artery disease. However, a wide range of other indications, such as congenital heart disease (including evaluation of anomalous coronary arteries), coronary mass, graft patency following coronary artery bypass surgery, combined cardiac function and coronary artery assessment, and combined aorta and coronary artery evaluation, were also included.
Table 1.
Baseline Demographics
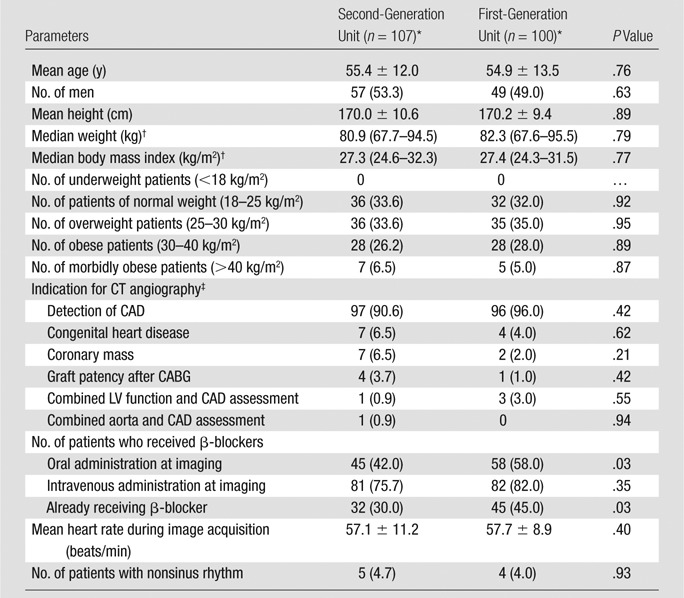
Except where indicated, numbers in parentheses are percentages. Percentages may not add to 100% owing to multiple categoric classifications.
Numbers in parentheses are IQRs.
CABG = coronary artery bypass graft, CAD = coronary artery disease, LV = left ventricle.
Overall, 71 of the 107 patients (66.4%) were overweight (36 patients, 33.6%), obese (28 of 107 patients, 26.2%), or morbidly obese (seven of 107 patients, 6.5%) (Fig E1 [online]). The median body mass index was 27.3 kg/m2 (range, 18.1–47.2 kg/m2).
At baseline, 32 of the 107 patients (30.0%) were taking a β-blocker. Additional β-blockers were administered orally in 45 patients (42.0%) and intravenously in 81 (75.7%). The mean heart rate during image acquisition was 57.1 beats per minute ± 11.2. Figure E2 (online) displays the distribution of heart rates. The heart rate during the CT acquisition was 75 beats per minute or lower in 102 of the 107 patients (95.3%) and less than 65 beats per minute in 84 (78.5%).
Retrospective Study Population
Overall, 100 consecutive clinical coronary CT angiography examinations performed with a previous first-generation 320–detector row CT scanner were retrospectively examined to serve as a comparison. The clinical characteristics of this cohort were similar to those of the prospective group who underwent imaging with the new-generation scanner and are displayed in Table 1.
CT Parameters
A tube potential of 100 kV was used in 97 of the 107 patients (90.6%) for coronary CT acquisition despite the large number of patients in the obese and morbidly obese categories. Table 2 summarizes the CT parameters.
Table 2.
Coronary CT Angiography Parameters
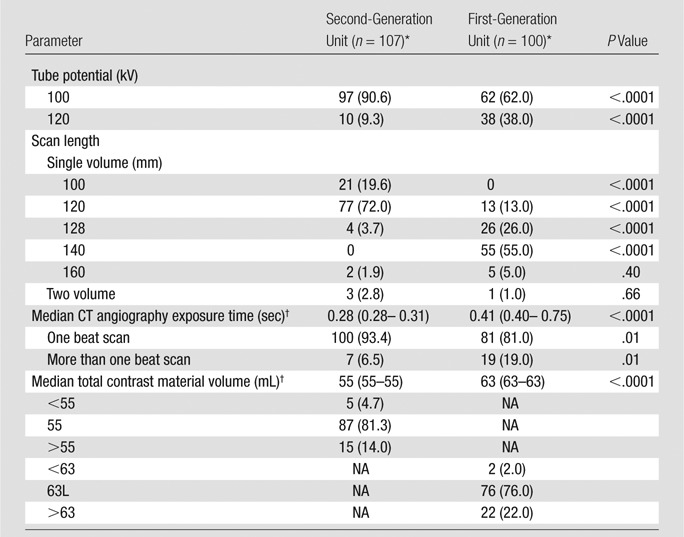
Except where indicated, data are numbers of patients, with percentages in parentheses. NA = not applicable.
Numbers in parentheses are IQRs.
Overall, 104 of the 107 patients (97.2%) underwent CT with use of a single-volume acquisition. In most cases (102 of 107 patients, 95.3%), hearts could be imaged within a 128-mm scan range. Two patients required 160-mm z-coverage to image the thoracic aorta in addition to the heart. A two-volume scan was needed to image more than 160-mm z-coverage in three patients for the evaluation of bypass grafts.
Prospective ECG gating was used in most patients (106 of 107 patients, 99.1%). Dose-modulated ECG gating was used to image the one patient who required combined valve and coronary artery assessment. Most CT angiography acquisitions (100 of 107 patients, 93.4%) were performed within one heartbeat because the heart rate was less than 75 beats per minute. Scanning in more than one heartbeat was necessary for heart rates faster than 75 beats per minute (n = 5) to improve temporal resolution through data segmentation, arrhythmia (n = 2), or for two-volume scanning for bypass graft evaluation (n = 3). The median total CT angiography exposure time was 0.28 second (IQR, 0.28–0.31 seconds).
Radiation Dose
The median dose-length product for all 107 scans was 66.8 mGy ⋅ cm (IQR, 41.1–124.9 mGy ⋅ cm), corresponding to an estimated effective dose of 0.93 mSv (IQR, 0.58–1.74 mSv). The radiation dose data are summarized in Table 3. When including all 107 patients, the estimated median effective dose was 0.93 mSv; however, when the six examinations that involved scanning more than the native coronary arteries were excluded (bypass graft, n = 4; combined aorta and coronary, n = 1; combined left ventricular assessment and coronary, n = 1), the median dose-length product was 62.7 mGy ⋅ cm (IQR, 40.5–118.4 mGy ⋅ cm), which represented an estimated effective dose of 0.88 mSv (IQR, 0.57–1.66 mSv).
Table 3.
Summary of Radiation Dose Data
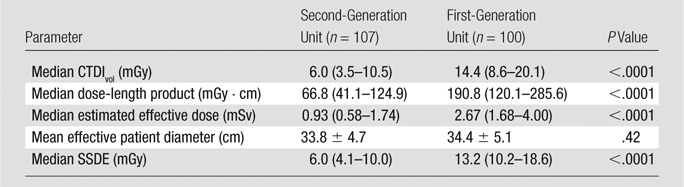
Note.—Numbers in parentheses are IQRs.
Overall, the radiation dose was less than 0.5 mSv in 23 of the 107 patients (21.5%), less than 1 mSv in 58 (54.2%), and less than 4 mSv in 103 (96.3%) (Fig E3 [online]). The median CTDIvol was 6.0 mGy (IQR, 3.5–10.5 mGy), and the mean effective patient diameter was 33.8 cm ± 4.7, yielding a median SSDE of 6.0 mGy (IQR, 4.1–10.0 mGy).
The overall radiation dose from the new second-generation 320–detector row CT system was significantly lower than that of the previous first-generation system, as displayed in Table 3. The median estimated effective dose with the second-generation system was reduced by 65% when compared with that with the first-generation system (0.93 mSv vs 2.67 mSv, respectively; P < .0001), with no significant differences in effective patient diameter (P = .42) or baseline demographics (Table 1). In addition, the median SSDE was significantly reduced by 55% (6.0 mGy vs 13.2 mGy, respectively; P < .0001).
Image Quality
The interobserver agreement between the two readers was excellent (κ = 0.81). The image quality score among the two readers was identical in 89.7% of cases (743 of 828 cases), and all discrepancies were by one point. All 107 coronary CT examinations were of diagnostic quality. Most studies had excellent image quality (score, 4) among all the categories, which included coronary motion, image noise, contrast material enhancement, and fine detail (Table 4). The mean image quality score ranged from 3.63 ± 0.49 to 3.84 ± 0.42 on a scale of 1 to 4. Specific case examples were selected to show image quality, particularly in more difficult cases (Figs 1–3 and E4–E6 [online]).
Table 4.
Summary of Image Quality Scores
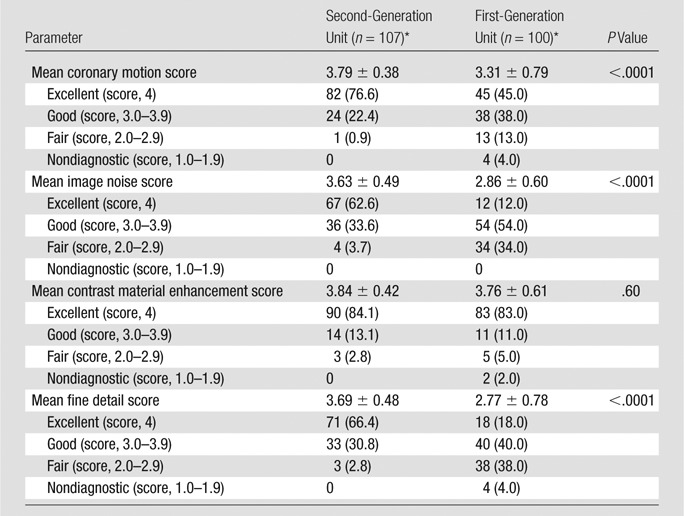
Except where indicated, data are numbers of patients, with percentages in parentheses. Image quality scores are the mean result from two independent readers who evaluated images in a blinded fashion.
Figure 1a:
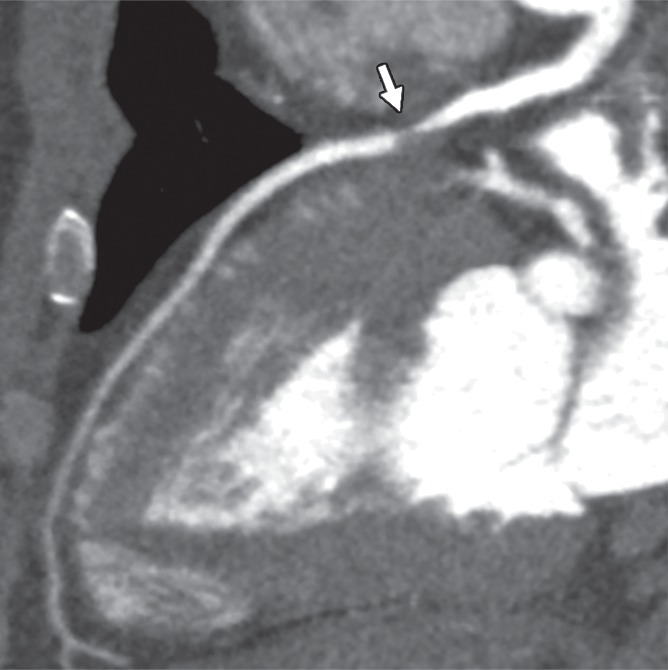
Obstructive noncalcified stenosis (arrow) of proximal left anterior descending artery in 42-year-old overweight man with atypical chest pain and a heart rate of 70 beats per minute (height, 175 cm; weight,100 kg; body mass index, 32.7 kg/m2; effective diameter, 35.4 cm). Two-heartbeat acquisition was selected because this case was early in our experience with prototype scanner. (a, b) Quality of image reconstructed from data obtained with only one heartbeat (a) is nearly indistinguishable from that of image reconstructed with data segmented between two heartbeats (b). (c) Three-dimensional surface rendering of heart and coronary arteries. Estimated effective radiation dose for two-heartbeat scan was 4.0 mSv (dose-length product, 284.5 mGy ⋅ cm; CTDIvol, 28.4 mGy; SSDE, 28.4 mGy). However, radiation dose could have been halved if only a single-heartbeat acquisition was selected. On the basis of similar initial experience, a prospectively acquired single-heartbeat scan can be obtained for heart rates slower than approximately 75 beats per minute.
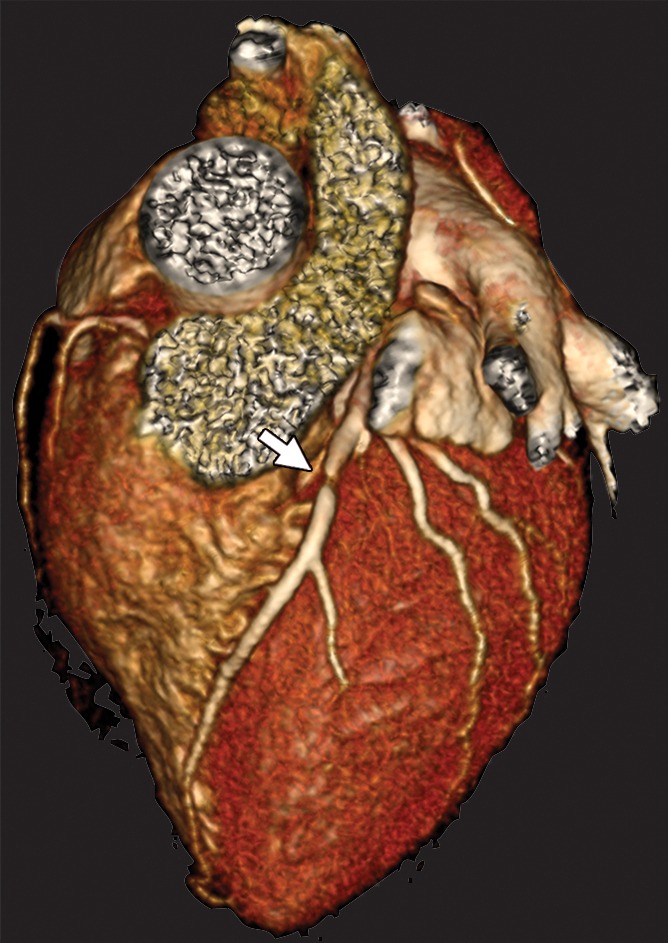
Figure 3a:
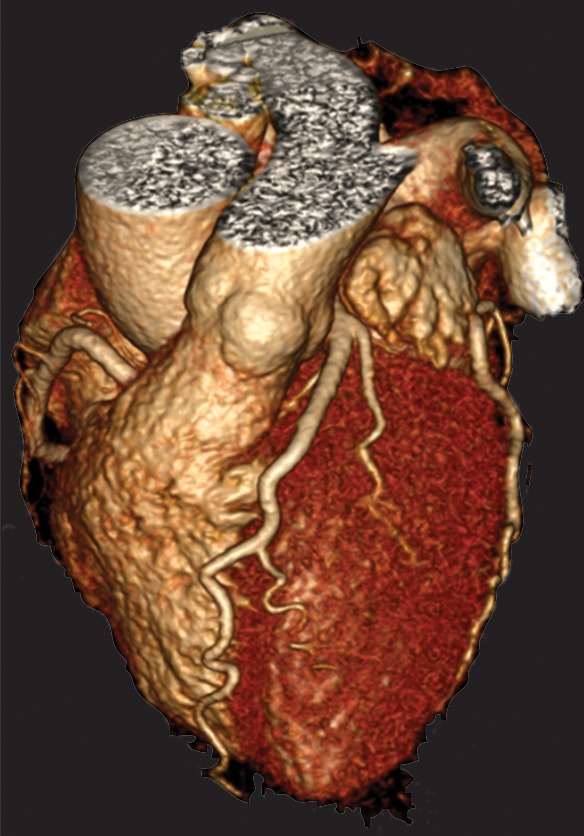
(a) Three-dimensional surface rendering and (b) normal coronary CT angiogram in obese woman (height, 162.6 cm; weight, 94.8 kg; body mass index, 35.9 kg/m2; effective patient diameter, 34.1 cm) imaged at 100-kV tube potential. The more powerful x-ray generator with automated exposure control combined to select a tube potential of 100 kV despite guidelines suggesting 120-kV imaging for patients with a body mass index greater than 30 kg/m2. A tube potential of 100 kV is theoretically better suited for attenuation characteristics of iodinated contrast media and lowers radiation dose compared with 120-kV settings. Estimated effective radiation dose was 0.7 mSv (dose-length product, 48.9 mGy ⋅ cm; CTDIvol, 4.1 mGy; SSDE, 4.3 mGy).
Figure 1b:
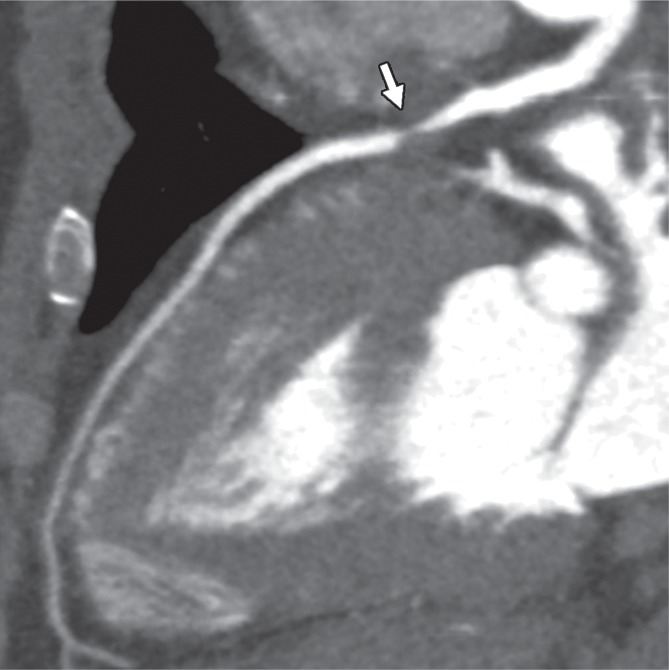
Obstructive noncalcified stenosis (arrow) of proximal left anterior descending artery in 42-year-old overweight man with atypical chest pain and a heart rate of 70 beats per minute (height, 175 cm; weight,100 kg; body mass index, 32.7 kg/m2; effective diameter, 35.4 cm). Two-heartbeat acquisition was selected because this case was early in our experience with prototype scanner. (a, b) Quality of image reconstructed from data obtained with only one heartbeat (a) is nearly indistinguishable from that of image reconstructed with data segmented between two heartbeats (b). (c) Three-dimensional surface rendering of heart and coronary arteries. Estimated effective radiation dose for two-heartbeat scan was 4.0 mSv (dose-length product, 284.5 mGy ⋅ cm; CTDIvol, 28.4 mGy; SSDE, 28.4 mGy). However, radiation dose could have been halved if only a single-heartbeat acquisition was selected. On the basis of similar initial experience, a prospectively acquired single-heartbeat scan can be obtained for heart rates slower than approximately 75 beats per minute.
Figure 1c:
Obstructive noncalcified stenosis (arrow) of proximal left anterior descending artery in 42-year-old overweight man with atypical chest pain and a heart rate of 70 beats per minute (height, 175 cm; weight,100 kg; body mass index, 32.7 kg/m2; effective diameter, 35.4 cm). Two-heartbeat acquisition was selected because this case was early in our experience with prototype scanner. (a, b) Quality of image reconstructed from data obtained with only one heartbeat (a) is nearly indistinguishable from that of image reconstructed with data segmented between two heartbeats (b). (c) Three-dimensional surface rendering of heart and coronary arteries. Estimated effective radiation dose for two-heartbeat scan was 4.0 mSv (dose-length product, 284.5 mGy ⋅ cm; CTDIvol, 28.4 mGy; SSDE, 28.4 mGy). However, radiation dose could have been halved if only a single-heartbeat acquisition was selected. On the basis of similar initial experience, a prospectively acquired single-heartbeat scan can be obtained for heart rates slower than approximately 75 beats per minute.
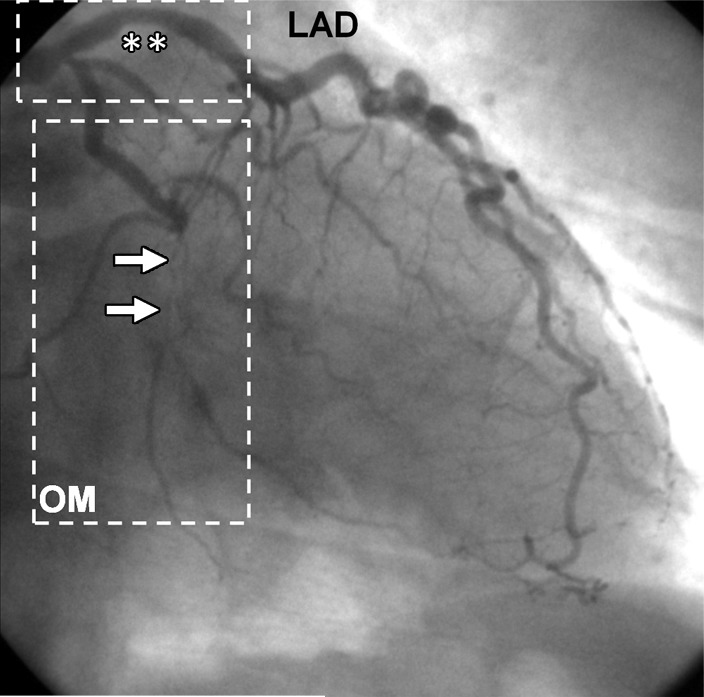
Figure 2a:

(a) Obstructive coronary CT angiogram of proximal portion of obtuse marginal (OM, arrows) and (b) corresponding invasive angiogram in 67-year-old man (height, 67.7 cm; weight, 176 kg; body mass index, 29.5 kg/m2; effective diameter, 31.3 cm; heart rate, 44 beats per minute). Nonobstructive mixed calcified and noncalcified coronary artery disease (*) of proximal left anterior descending coronary artery (LAD) is present on both (c) coronary CT angiogram and (b) invasive angiogram. Estimated effective radiation dose was 0.90 mSv (dose-length product, 64.1 mGy ⋅ cm; CTDIvol, 5.3 mGy; SSDE, 6.16 mGy).
Figure 2b:
(a) Obstructive coronary CT angiogram of proximal portion of obtuse marginal (OM, arrows) and (b) corresponding invasive angiogram in 67-year-old man (height, 67.7 cm; weight, 176 kg; body mass index, 29.5 kg/m2; effective diameter, 31.3 cm; heart rate, 44 beats per minute). Nonobstructive mixed calcified and noncalcified coronary artery disease (*) of proximal left anterior descending coronary artery (LAD) is present on both (c) coronary CT angiogram and (b) invasive angiogram. Estimated effective radiation dose was 0.90 mSv (dose-length product, 64.1 mGy ⋅ cm; CTDIvol, 5.3 mGy; SSDE, 6.16 mGy).
Figure 2c:
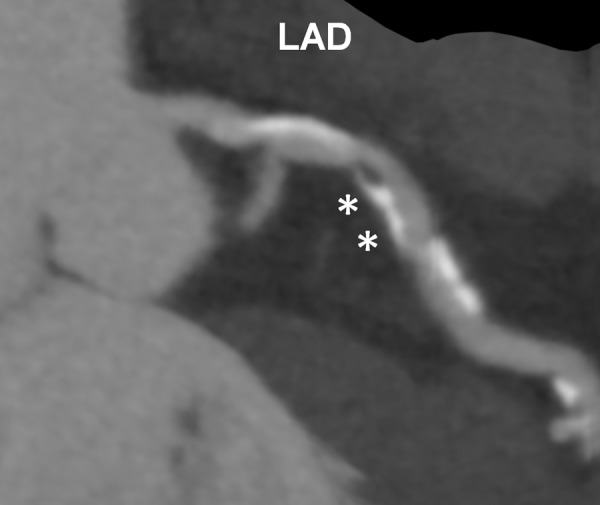
(a) Obstructive coronary CT angiogram of proximal portion of obtuse marginal (OM, arrows) and (b) corresponding invasive angiogram in 67-year-old man (height, 67.7 cm; weight, 176 kg; body mass index, 29.5 kg/m2; effective diameter, 31.3 cm; heart rate, 44 beats per minute). Nonobstructive mixed calcified and noncalcified coronary artery disease (*) of proximal left anterior descending coronary artery (LAD) is present on both (c) coronary CT angiogram and (b) invasive angiogram. Estimated effective radiation dose was 0.90 mSv (dose-length product, 64.1 mGy ⋅ cm; CTDIvol, 5.3 mGy; SSDE, 6.16 mGy).
Figure 3b:
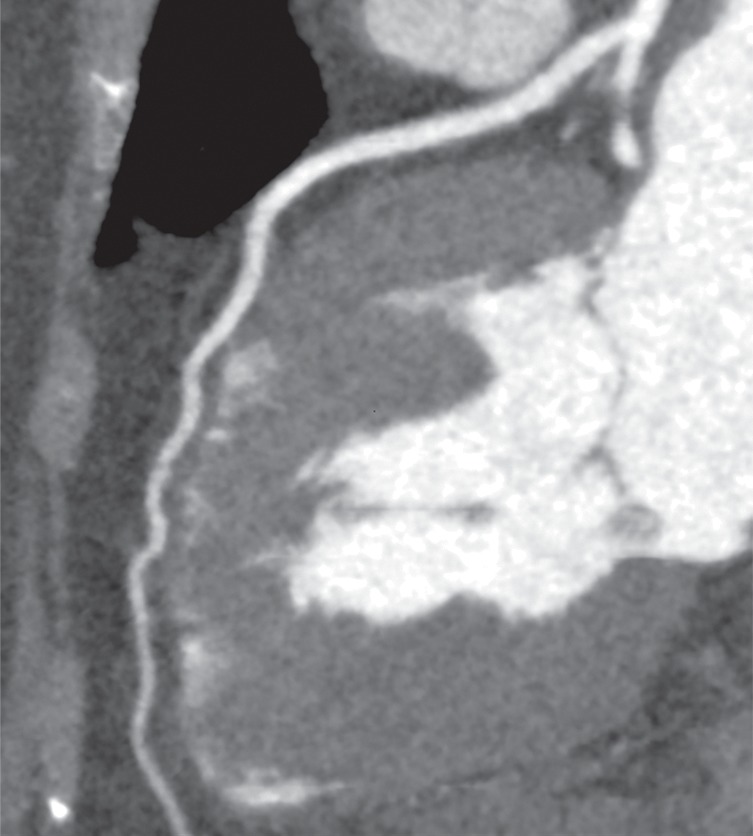
(a) Three-dimensional surface rendering and (b) normal coronary CT angiogram in obese woman (height, 162.6 cm; weight, 94.8 kg; body mass index, 35.9 kg/m2; effective patient diameter, 34.1 cm) imaged at 100-kV tube potential. The more powerful x-ray generator with automated exposure control combined to select a tube potential of 100 kV despite guidelines suggesting 120-kV imaging for patients with a body mass index greater than 30 kg/m2. A tube potential of 100 kV is theoretically better suited for attenuation characteristics of iodinated contrast media and lowers radiation dose compared with 120-kV settings. Estimated effective radiation dose was 0.7 mSv (dose-length product, 48.9 mGy ⋅ cm; CTDIvol, 4.1 mGy; SSDE, 4.3 mGy).
The image quality scores for coronary motion, image noise, and fine detail with the second-generation 320–detector row CT scanner were significantly higher than those with the first-generation system (P < .0001 for all, Table 4); however, the scores for contrast material enhancement were not significantly different (P = .60). The ability to select the best cardiac phase with minimal coronary motion artifact reduced some motion-related artifacts (Fig E7 [online]).
Discussion
The new second-generation 320–detector row CT scanner provided excellent image quality over a wide range of body sizes and heart rates at lower radiation doses than the previous first-generation CT scanner. This study represents the initial coronary angiography experience obtained with a prototype 320–detector row CT system that has recently received approval by the U.S. Food and Drug Administration. The experience represents a series of 107 consecutive and unselected patients. Image quality was high, and the associated radiation exposure was lower than that with a previous first-generation volume CT scanner. All scans were of diagnostic quality despite a wide range of patient sizes (66.4% of patients were overweight, obese, or morbidly obese) and a wide range of heart rates (34–95 beats per minute).
The median estimated radiation exposure was 0.93 mSv, and this represents at least a 75% reduction compared with previous reports from the first-generation 320–detector row CT scanner (11,12,23,24). This level of dose exposure was achieved by means of a combination of judicious use of β-blockers to help slow the resting heart rate and carefully controlling cranial-caudal scan range. Previous studies have demonstrated that lowering the heart rate with β-blockers is not only safe (25,26) but also reduces radiation exposure (27) and improves diagnostic image quality (28). In addition, tailoring the field of view of the examination to the clinical indication conforms to the “as low as reasonably achievable,” or ALARA, principal. Radiation dose is directly related to the craniocaudal scan range (24,27), a factor that the physician and technologist must control. Most of the scans were obtained with prospective ECG gating, which not only reduces radiation exposure by approximately 69%–83% over retrospective gating but also preserves image quality (29,30). No scans required fixed tube current retrospective gating. Only one of the 107 examinations was performed with dose modulation and complete cardiac cycle scanning to assess both cardiac function and coronary arteries.
The faster gantry rotation time of 275 msec combined with up to 16-cm z-axis volume coverage per rotation combined to enable single-heartbeat acquisitions in patients with heart rates of up to at least 75 beats per minute, which covered 95.3% of the patients in this study (102 of 107 patients). The previous first-generation wide-volume scanner had a gantry rotation time of 350 msec, which enabled single-heartbeat scanning with heart rates of up to approximately 65 beats per minute (13,23). The improvement in temporal resolution of the second-generation scanner reduced radiation exposure by permitting single-heartbeat acquisitions in a larger proportion of patients. The additional 17% of patients with heart rates between 65 and 75 beats per minute (18 of 107 patients) meant that we were able to use single-heartbeat scans in 95.3% of subjects in this study (102 of 107 patients). Previously, with the first-generation scanner, we would only have tried single-heartbeat scanning in 78.5% of these same patients (84 of the 107 patients). Overall, a significantly higher number of patients can undergo single-heartbeat scanning with the new-generation scanner (P < .0001, McNemar test).
CT filtered back projection reconstruction requires image data from 180° plus half of the fan beam angle. A 320–detector row wide-area detector CT scanner requires one complete gantry rotation (360° or 275 msec) for image reconstruction to correct for cone beam artifacts due to extreme angles between the x-ray source and detectors (19). However, the temporal resolution from this cone beam correction is approximately 140 msec for a single-volume acquisition. Therefore, the scanner acquires an acquisition window wider than the minimum needed for image reconstruction. This scan duration can be used to an advantage by enabling reconstruction of images across different cardiac phases. The ability to select the best cardiac phase with minimal coronary motion artifact can reduce some motion-related artifacts. In comparison, scan modes such as prospective gating with no ECG padding or ECG-triggered high-pitch helical acquisitions only provide one time point without the ability to select a slightly different phase of the cardiac cycle (31). For patients with heart rates faster than 75 beats per minute, multisegmented volume acquisition can be used for faster temporal resolution. Temporal resolution improves as a factor of the number of heartbeats (ie, 70-msec resolution for two-beat acquisition).
A tube potential of 100 kV could be used in most cases (97 of 107 patients, 90.6%) owing to the availability of a larger x-ray generator that can produce up to 900 mA. Imaging at 100 kV rather than 120 kV reduces radiation exposure by 31% while maintaining image quality (32). Current guidelines suggest that 100-kV imaging should be considered for patients with a body mass index of less than 30 kg/m2 (10). Although most patients in this study were overweight, obese, or morbidly obese (71 of 107 patients, 66.4%), most of those patients (61 of 71 patients, 86%) underwent imaging at 100 kV and all had diagnostic image quality. Thus, the guidelines may need to be revised to account for CT scanners equipped with iterative reconstruction and x-ray generators sufficient to deliver a high enough tube current.
Third-generation iterative reconstruction (AIDR3D), which works in both raw and image space, in combination with automated exposure control worked synergistically to help reduce radiation exposure and maintain image quality. Iterative reconstruction methods decrease image noise, which allows for reductions in tube current while preserving overall image quality (33,34). Automated exposure control software has provided approximately 30% dose reductions for cardiovascular CT while preserving image quality (35).
Although this initial experience with a new-generation scanner highlighted the ability to consistently perform coronary CT angiography in a consecutive series of 107 unselected patients, this study does have limitations. It will take additional time to acquire systematic comparisons with invasive coronary angiography. However, previous studies with the first-generation 320–detector row scanners have demonstrated high diagnostic accuracy (11,36,37). Most patients were given β-blockers to help lower the resting heart rate and, therefore, heart rate limits were not fully evaluated. Current guidelines support the use of β-blockers to reduce heart rate to improve image quality and reduce radiation exposure (10,25,38). Patients in this study were not randomized. Image quality or radiation doses were not compared with results from the previous first-generation scanner in the same patients. However, it is not practical to expose patients to sequential examinations with two radiation and contrast material exposures.
In conclusion, the combination of a gantry rotation time of 275 msec, 16-cm cranial-caudal wide volume coverage, iterative reconstruction, automated exposure control, and a larger x-ray power generator in the new second-generation 320–detector row CT scanner provided excellent image quality over a wide range of body sizes and heart rates at lower radiation doses compared with previous-generation CT scanners. This technology could further facilitate CT stress perfusion (14,15), contrast attnenuation gradients across atherosclerotic lesions (16), and noninvasive fractional flow reserve computed from coronary CT angiography (39).
Advances in Knowledge.
• Use of a 320–detector row CT scanner with 16-cm-wide volume coverage enabled 97.2% of coronary CT angiography examinations (104 of 107 examinations) to be performed with a single volume, whereas two-volume scans were used for bypass grafts and combined coronary and thoracic aorta evaluations.
• The gantry rotation time for a new second-generation scanner is faster than that of the previous first-generation scanner (275 vs 350 msec), which contributed to the performance of single-heartbeat coronary CT angiography in 100 of 107 patients (93.4%), including those with heart rates of up to approximately 75 beats per minute.
• A more powerful x-ray generator and automated exposure control combined to select a tube potential of 100 kV in 97 of 107 patients (90.6%)—a tube potential that is theoretically better suited for the attenuation characteristics of iodinated contrast media and lowers radiation dose compared with 120-kV settings.
• Iterative image reconstruction of three-dimensional volume scans was done within a normal clinical work flow (up to 50 images per second) and helped maintain excellent image quality in most subjects.
• Overall, these technical advances combined with individually optimized scan ranges resulted in a median radiation dose of 0.93 mSv; the radiation dose was less than 1 mSv in 54.2% of the CT angiography examinations (58 of 107 patients) and less than 4 mSv in 96.3% (103 of 107 patients).
Implications for Patient Care.
• Radiation exposure during diagnostic imaging is a substantial public concern.
• Minimizing radiation exposure while maintaining diagnostic-quality scans is clearly feasible with this new second-generation 320–detector row CT scanner.
• The low dose achieved during CT angiography could be used to minimize overall radiation dose to the patient or to enable additional types of imaging (eg, perfusion imaging) within reasonable radiation doses.
Disclosures of Conflicts of Interest: M.Y.C. No potential conflicts of interest to disclose. S.M.S. No potential conflicts of interest to disclose. A.E.A. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: has a research agreement with Toshiba.
Supplementary Material
Acknowledgments
The authors thank Jeffrey Hall, DipRad, John Schuzer, RT, and Chloe Steveson, MMRS, for their expertise in developing and implementing scanning protocols. In addition, the authors thank Richard Mather, PhD, for his technical knowledge and assistance. The prototype CT scanner was provided to the National Institutes of Health through a research agreement with Toshiba Medical Systems.
Received November 25, 2012; revision requested December 5; revision received December 21; accepted December 27; final version accepted December 28.
Funding: This research was supported by the National Institutes of Health (grant HL006138-02).
Abbreviations:
- CTDIvol
- volumetric CT dose index
- ECG
- electrocardiography
- IQR
- interquartile range
- SSDE
- size-specific dose estimate
References
- 1.Bluemke DA, Achenbach S, Budoff M, et al. Noninvasive coronary artery imaging: magnetic resonance angiography and multidetector computed tomography angiography—a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention, and the Councils on Clinical Cardiology and Cardiovascular Disease in the Young. Circulation 2008;118(5):586–606 [DOI] [PubMed] [Google Scholar]
- 2.American College of Cardiology Foundation Task Force on Expert Consensus Documents. Mark DB, Berman DS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 2010;121(22):2509–2543 [DOI] [PubMed] [Google Scholar]
- 3.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52(21):1724–1732 [DOI] [PubMed] [Google Scholar]
- 4.Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359(22):2324–2336 [DOI] [PubMed] [Google Scholar]
- 5.Goldstein JA, Chinnaiyan KM, Abidov A, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011;58(14):1414–1422 [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann U, Truong QA, Schoenfeld DA, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012;367(4):299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 2012;366(15):1393–1403 [DOI] [PubMed] [Google Scholar]
- 8.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007;357(22):2277–2284 [DOI] [PubMed] [Google Scholar]
- 9.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 2007;298(3):317–323 [DOI] [PubMed] [Google Scholar]
- 10.Halliburton SS, Abbara S, Chen MY, et al. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr 2011;5(4):198–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 2009;120(10):867–875 [DOI] [PubMed] [Google Scholar]
- 12.Rybicki FJ, Otero HJ, Steigner ML, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 2008;24(5):535–546 [DOI] [PubMed] [Google Scholar]
- 13.Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep 2010;12(1):68–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George RT, Arbab-Zadeh A, Miller JM, et al. Computed tomography myocardial perfusion imaging with 320-row detector computed tomography accurately detects myocardial ischemia in patients with obstructive coronary artery disease. Circ Cardiovasc Imaging 2012;5(3):333–340 [DOI] [PubMed] [Google Scholar]
- 15.George RT, Arbab-Zadeh A, Cerci RJ, et al. Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320-MDCT: the CT angiography and perfusion methods of the CORE320 multicenter multinational diagnostic study. AJR Am J Roentgenol 2011;197(4):829–837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steigner ML, Mitsouras D, Whitmore AG, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging 2010;3(2):179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hein PA, May J, Rogalla P, Butler C, Hamm B, Lembcke A. Feasibility of contrast material volume reduction in coronary artery imaging using 320-slice volume CT. Eur Radiol 2010;20(6):1337–1343 [DOI] [PubMed] [Google Scholar]
- 18.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function: measured and estimated glomerular filtration rate. N Engl J Med 2006;354(23):2473–2483 [DOI] [PubMed] [Google Scholar]
- 19.Bedayat A, Rybicki FJ, Kumamaru K, et al. Reduced exposure using asymmetric cone beam processing for wide area detector cardiac CT. Int J Cardiovasc Imaging 2012;28(2):381–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van der Molen AJ, Joemai RM, Geleijns J. Performance of longitudinal and volumetric tube current modulation in a 64-slice CT with different choices of acquisition and reconstruction parameters. Phys Med 2012;28(4):319–326 [DOI] [PubMed] [Google Scholar]
- 21.Bongartz G, Golding S, Jurik A, et al. European guidelines for multislice computed tomography: appendix C. Funded by the European Commission contract number FIGM-CT2000-20078-CT-TIP. Luxembourg: European Commission, March 2004 [Google Scholar]
- 22.Boone J, Strauss K, Cody D, et al. Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. Report of American Association of Physicists in Medicine (AAPM) Task Group 204. College Park, Md: American Association of Physicists in Medicine, 2011 [Google Scholar]
- 23.Hoe J, Toh KH. First experience with 320-row multidetector CT coronary angiography scanning with prospective electrocardiogram gating to reduce radiation dose. J Cardiovasc Comput Tomogr 2009;3(4):257–261 [DOI] [PubMed] [Google Scholar]
- 24.Khan A, Nasir K, Khosa F, Saghir A, Sarwar S, Clouse ME. Prospective gating with 320-MDCT angiography: effect of volume scan length on radiation dose. AJR Am J Roentgenol 2011;196(2):407–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahabadi AA, Achenbach S, Burgstahler C, et al. Safety, efficacy, and indications of β-adrenergic receptor blockade to reduce heart rate prior to coronary CT angiography. Radiology 2010;257(3):614–623 [DOI] [PubMed] [Google Scholar]
- 26.Roberts WT, Wright AR, Timmis JB, Timmis AD. Safety and efficacy of a rate control protocol for cardiac CT. Br J Radiol 2009;82(976):267–271 [DOI] [PubMed] [Google Scholar]
- 27.Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA 2009;301(5):500–507 [DOI] [PubMed] [Google Scholar]
- 28.Dewey M, Vavere AL, Arbab-Zadeh A, et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am J Roentgenol 2010;194(1):93–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hausleiter J, Meyer TS, Martuscelli E, et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging 2012;5(5):484–493 [DOI] [PubMed] [Google Scholar]
- 30.Earls JP, Berman EL, Urban BA, et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology 2008;246(3):742–753 [DOI] [PubMed] [Google Scholar]
- 31.Achenbach S, Marwan M, Schepis T, et al. High-pitch spiral acquisition: a new scan mode for coronary CT angiography. J Cardiovasc Comput Tomogr 2009;3(2):117–121 [DOI] [PubMed] [Google Scholar]
- 32.Hausleiter J, Martinoff S, Hadamitzky M, et al. Image quality and radiation exposure with a low tube voltage protocol for coronary CT angiography results of the PROTECTION II Trial. JACC Cardiovasc Imaging 2010;3(11):1113–1123 [DOI] [PubMed] [Google Scholar]
- 33.Beister M, Kolditz D, Kalender WA. Iterative reconstruction methods in x-ray CT. Phys Med 2012;28(2):94–108 [DOI] [PubMed] [Google Scholar]
- 34.Leipsic J, Labounty TM, Heilbron B, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol 2010;195(3):655–660 [DOI] [PubMed] [Google Scholar]
- 35.Ghoshhajra BB, Engel LC, Károlyi M, et al. Cardiac computed tomography angiography with automatic tube potential selection: effects on radiation dose and image quality. J Thorac Imaging 2013;28(1):40–48 [DOI] [PubMed] [Google Scholar]
- 36.Nasis A, Leung MC, Antonis PR, et al. Diagnostic accuracy of noninvasive coronary angiography with 320-detector row computed tomography. Am J Cardiol 2010;106(10):1429–1435 [DOI] [PubMed] [Google Scholar]
- 37.Sun G, Li M, Jiang XS, et al. 320-detector row CT coronary angiography: effects of heart rate and heart rate variability on image quality, diagnostic accuracy and radiation exposure. Br J Radiol 2012;85(1016):e388–e394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abbara S, Arbab-Zadeh A, Callister TQ, et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009;3(3):190–204 [DOI] [PubMed] [Google Scholar]
- 39.Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308(12):1237–1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


