Abstract
Study objective
Genital herpes (HSV) is exceedingly common in the United States and women are disproportionally affected. This study aims to describe young women’s beliefs about HSV and examine the correlates of those beliefs.
Design
A 40 item Herpes Representation measure (HSV- RoSTD) and a demographic questionnaire were administered to a convenience sample of young women. Data analysis included descriptive statistics, t-tests and Pearson’s correlations.
Setting
Four women’s health clinics and one large state university.
Participants
302 women aged 18–24.
Interventions
None.
Main outcome measures
Four dimensions of HSV representations (cause, identity, future perspective and psychosocial consequences), age and STD testing history.
Results
Nearly all (98%) believed that HSV would result in genital sores and 68% believed they could tell if their sexual partner had HSV. Most (89%) understood the longevity of HSV, however 30% believed that they could take a pill to get rid of the infection, and 15% indicated that it was likely they would die from HSV. Negative beliefs about the psychosocial impact of HSV were common as 95% indicated they would be depressed and 90% indicated concern about sex and partner notification. Those who were younger and those who had never been tested for STDs believed a genital herpes infection is highly symptomatic. Finally, negative beliefs about the psychosocial consequences of HSV were associated with beliefs about HSV being symptomatic, having a negative impact on future health, and being associated with sexual risk behaviors.
Conclusions
Young women have misconceptions about HSV, particularly regarding the symptomatology and the role of HSV medication. Noteworthy concerns about the negative psychosocial consequences of an HSV diagnosis were also raised, all of which have implications for young women’s sexual health.
Keywords: Health Beliefs, Women’s Health, Herpes Simplex Virus
INTRODUCTION
Genital herpes is a common sexually transmitted disease (STD) caused by the herpes simplex virus (HSV). There are two types of HSV – type one (HSV-1) and type two (HSV-2). While both types may be spread via oral-genital or genital-genital contact, HSV-2 is more likely to cause recurrent genital herpes outbreaks.1 In the United States, 16.2% of the population aged 14–49 has genital HSV-2. This infection is twice as common in women than men; one in five women are infected compared to one in nine men.1 Young women are particularly vulnerable to genital herpes2–4 as the prevalence increases from 1.6% among adolescents to 10.6% among young adults.3 The annual health care costs due to genital herpes are estimated at over 1 billion dollars.5
A significant factor likely contributing to the high prevalence of HSV is that most people with genital herpes do not realize they are infected.1 Although classic symptoms of HSV include genital blisters or ulcers, most people who are infected have vague symptoms, such as genital itching, or no symptoms at all.1, 2 particularly vulnerable to genital herpes infections increase the risk of acquiring and transmitting Human Immunodeficiency Virus (HIV).1
Genital herpes is highly stigmatized. People perceive genital herpes as the second most likely STD, after HIV, to damage someone’s reputation and to be viewed as a sign of weak moral character.6 Subsequently, an HSV diagnosis often results in negative psychological consequences and women are affected to a greater extent by these stigma related consequences than men.7, 8 Genital herpes diagnosis also impacts relationships. People may choose to maintain current relationships or avoid future sexual situations/relationships solely to avoid the need for further disclosure.7 The frequency of outbreaks can also influence psychological adjustment. People experiencing more frequent outbreaks are more likely to be embarrassed and upset about their diagnosis, worry about next outbreak, and have more difficulty adjusting to life after diagnosis.9
Although limited in breadth and depth, the available evidence suggests that people lack knowledge about various aspects of HSV. For example, in an analysis of HSV-related questions drawn from chat room transcripts, questions centered on transmission risks and symptoms, antiviral medications and disclosure of HSV diagnosis to sexual partners.10 Another study found that even though many participants correctly answered questions about genital herpes and transmission, most participants lacked confidence in the accuracy of their responses and felt poorly informed about HSV overall.11 Finally, in an investigation of women who were at high-risk for HSV (yet did not perceive themselves to be at high-risk) it was reported that their knowledge of HSV was high, yet the specific items assessing HSV knowledge were not reported.12
The current literature regarding women’s beliefs about genital herpes is limited and is heavily focused on the psychosocial consequences of HSV among those already diagnosed. Little is known about the broader HSV beliefs held by women in the general population. Given the high prevalence of HSV, particularly among young women, a comprehensive examination of young women’s beliefs about HSV is needed.
One way to examine HSV beliefs is with the use of the Common Sense Model (CSM). The CSM13, 14 is a theoretical framework that suggests beliefs about an illness guides health behavior related to that illness. Beliefs about an illness are formed through personal experience as well as from broader sociocultural beliefs and systems. According to the model, illness beliefs (i.e., illness representations) are organized into five dimensions (Identity, Consequences, Control, Chronicity, and Cause). The CSM has been used to describe beliefs about a wide number of illnesses16 including women’s beliefs about human papillomavirus.17 Although the CSM does not describe relationships among the representational dimensions, significant positive correlations have been found between beliefs about consequences, symptomatology (identity), and chronicity.16 In these studies, the more strongly persons believed that the consequences of an illness were severe, the more strongly they believed that the illness was chronic and the more likely they were to report symptoms of the illness.
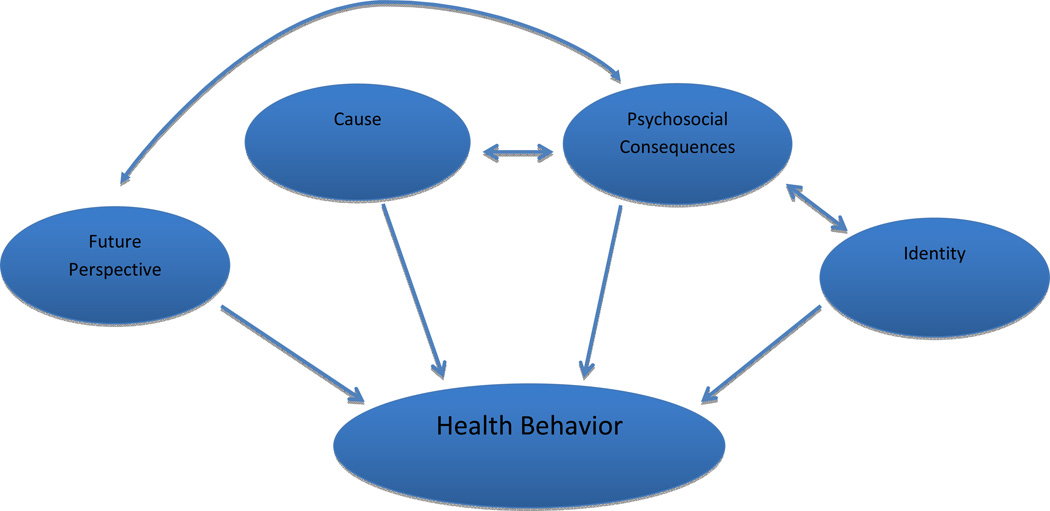
For STDs, previous research by the first author found that women’s representations about STDs consist of four dimensions: Future Perspective, Cause, Psychosocial Consequences, and Identity.15 The Future Perspective dimension includes beliefs about the future health implications of an STD diagnosis. The Cause dimension includes beliefs about behaviors associated with STD acquisition. The Psychosocial Consequence dimension includes beliefs about the impact of an STD diagnosis on mental health and intimate relationships, and the Identity dimension includes beliefs about the symptoms associated with an STD. Figure 1 illustrates the model of STD beliefs and their theoretical relationships to each other and to health behavior. According to this model, for example, if a woman is at risk for HSV and has no symptoms, and she believes that HSV is a symptomatic illness, she may not seek testing (a health behavior). Also, if she believes the psychosocial consequences of HSV are severe, she may have very negative beliefs about her future health if infected with HSV. Whether these hypothesized relationships exist among STD beliefs has not been previously examined.
Figure 1.
Dimensions of STD Representations
Based on the model of STD beliefs, the specific aims of this study were:
To describe young women’s representations about herpes simplex virus (HSV).
To examine whether HSV representations differ based on age and history of STD testing.
To examine the relationship between women’s beliefs about the psychosocial consequences of HSV and their beliefs about symptoms, future perspective and cause.
MATERIALS AND METHODS
Design
This investigation employed a cross-sectional survey design and was part of a larger study examining women’s beliefs about various STDs.15 Only the HSV beliefs will be described.
Participants
Women aged 18–24 with the ability to read and write English were eligible to participate. Human subject approval was obtained.
Instruments
Participants completed two instruments: a demographic and health information questionnaire and the HSV Representations of Sexually Transmitted Diseases (HSV - RoSTD).
Demographic and health information
This questionnaire assessed demographic characteristics and STD related history.
HSV Representations of Sexually Transmitted Diseases (HSV - RoSTD)
This theoretically derived self-report instrument measured women’s representations about HSV. The HSV - RoSTD had a total of 40 items divided among four subscales: Future Perspective, Cause, Psychosocial Consequences, and Identity. Details about the scale development and psychometric testing can be found in a previous publication15. The sample and data used in this study were derived from the original investigation
The Future Perspective subscale includes 14 items to measure beliefs about the future health implications associated with HSV. Participants respond to each item on a four-point Likert scale anchored with, Not Likely (1) to Very Likely (4). Higher scores indicate stronger beliefs about the negative impact of an HSV diagnosis on the future. Five items within this subscale are reverse coded. Measures of internal consistency were Cronbach’s alpha (α = .72) and composite reliability (.86). Two week test-retest reliability was r = .84.
The Cause subscale includes seven items that measure beliefs about the likelihood of HSV transmission associated with various sexual risk behaviors. Participants respond to each item on a four-point Likert scale anchored with Low (1) to High (4). Higher scores indicate greater recognition of the sexual risk behaviors associated with HSV transmission. Measures of internal consistency were Cronbach’s alpha (α = .76) and composite reliability (.85). Two week test-retest reliability was r = .69.
The Psychosocial Consequences subscale has 12 items and measures beliefs about the psychosocial impact of an HSV diagnosis on intimate relationships and personal mental health. Participants respond to each item on a four-point Likert scale anchored with Not Likely (1) to Very Likely (4). Higher scores indicate stronger beliefs about the negative psychosocial impact of an HSV diagnosis. Measures of internal consistency were Cronbach’s alpha (α = .82) and composite reliability (.91). Two week test-retest reliability was r = .84.
The Identity subscale has 7 items that measure beliefs about physical symptoms associated with an HSV diagnosis. Participants respond to each item on a four-point Likert scale anchored with Not Likely (1) to Very Likely (4). Higher scores endorse the presence of more physical symptoms associated with HSV. Measures of internal consistency were Cronbach’s alpha (α = .53) and composite reliability (.69). Two week test-retest reliability was r = .75.
Procedure
Recruitment occurred from two different settings: a university classroom at a large public midwestern university and four women’s health clinics. Participants from the women’s health clinics were recruited following appointments at two urban-based family planning clinics, one urban public health department or a university-based women’s health clinic. Detailed study procedures have been previously published.15
All participants received a survey packet containing the study measures. Classroom participants completed the surveys outside of class and return the completed surveys the next class session. Clinic participants completed the survey packet in private locations at the clinics and returned them to the researcher at the clinics. All participants received $5 for their participation.
Response rates were estimated due to procedures to protect participant anonymity. The classroom participant response rate was estimated to be 50%, as 85% of the 280 students enrolled in the course were women (n = 238), 85% of the 238 females (n = 202) typically attended class and 101 surveys were returned 101/202 = 50%. The clinic staff did not record the number of women who were approached/declined to participate. However, all of the women who met with the clinic-based researcher about the study agreed to participate (100%).
Data analysis
Data were analyzed using SPSS (version 19). Descriptive statistics were used to examine women HSV representations. Independent sample t-tests were used to examine whether differences existed in HSV representations based on age and STD testing history. Pearson’s correlations were used to examine the relationship between the representational dimensions.
RESULTS
Description of Sample
The mean age of the participants (n = 302) was 20.3 (SD = 1.8). Two-thirds (n = 201, 66.7%) were recruited from clinic locations and the other one-third (n = 101, 33.4%) were recruited from a university class. Half (49.7%) reported being in a “serious” romantic relationship. Most of the participants were Caucasian (n = 236, 78.1%) and not Hispanic (n = 270, 89.4%), while 18% (n = 55) were racial/ethnic minorities. Ninety-three percent were educated beyond high school. A majority (62.3%) reported having received STD testing at some point. Some of the participants (12.6%) reported having a history of an STD diagnosis. The prevalence of self-reported STD diagnoses were: HPV (n = 23, 7.6%), Chlamydia (n = 13, 4.3%), Trichomoniasis (n = 4, 1.3%), Syphilis (n = 1, 0.3%), HSV (n = 2, 0.7%).
Specific Aim 1: To describe young women’s representations about herpes simplex virus (HSV).
Future perspective
The mean score for the Future Perspective subscale was 2.96 (0.44), which indicates that participants believed that an HSV diagnosis would have a negative impact on their future health (Table 1). Overall, the women did recognize the chronicity of HSV as 89% indicated that an HSV infection was likely (13%, n = 39) or very likely (76%, n = 228) to last their entire lives. However, conversely, 17% of the sample believed that it was likely (10%, n = 30) or very likely (6.7%, n = 20) that an HSV infection could be cured. Misconceptions about treatment options were also apparent as 30% believed that it was likely (20.1%, n = 60) or very likely (9.7%, n = 29) that they could take a pill to get rid of an HSV infection. Further, even with treatment options available to help manage the symptoms of an HSV infection, 34% believed that it was likely (14.7%, n = 44) or very likely (19%, n = 57) that there would be nothing they could do about an HSV infection if they were diagnosed. Finally, although a genital HSV infection does not result in death, 15% inaccurately believed that death was likely (9.4%, n = 28) or very likely (5.4%, n = 16).
Table 1.
HSV Representations: Future Perspective Dimension
| Not likely n (%) |
Somewhat likely n (%) |
Likely n (%) |
Very likely n (%) |
|
|---|---|---|---|---|
| Having HSV means I would always have to take medication | 17 (5.7) | 31 (10.4) | 52 (17.4) | 199 (66.6) |
| I could die from HSV | 171 (57.6) | 82 (27.6) | 28 (9.4) | 16 (5.4) |
| Having HSV would mean that I would always need medical treatment | 18 (6.0) | 44 (14.7) | 90 (30.0) | 148 (49.3) |
| Having HSV means that I will have to tell future sexual partners | 13 (4.3) | 12 (4.0) | 33 (11.0) | 241 (80.6) |
| If I had HSV and it was treated, it could come back | 2 (0.70) | 15 (5.0) | 55 (18.3) | 228 (76.0) |
| If I had HSV, it would last my entire life | 15 (5.0) | 18 (6.0) | 39 (13.0) | 228 (76.0) |
| HSV will last a long time | 9 (3.0) | 13 (4.3) | 38 (12.6) | 241 (80.1) |
| If I had HSV, there would be nothing I could do about it | 147 (49.0) | 52 (17.3) | 44 (14.7) | 57 (19.0) |
| If I had HSV, there would be very little I could do about it | 58 (19.3) | 70 (23.3) | 79 (26.3) | 93 (31.0) |
| HSV comes and goes very quickly | 180 (60.4) | 42 (14.1) | 33 (11.1) | 43 (14.4) |
| If I had HSV, it could be cured | 197 (65.4) | 54 (17.9) | 30 (10.0) | 20 (6.6) |
| If I had HSV, I could take a pill to get rid of the infection | 150 (50.2) | 60 (20.1) | 60 (20.1) | 29 (9.7) |
| If I had HSV, there would be a lot I could do to control the infection | 40 (13.4) | 78 (26.1) | 85 (28.4) | 96 (32.1) |
| If I had HSV, I could take a pill to help control the infection | 24 (8.0) | 34 (11.4) | 95 (31.8) | 146 (48.8) |
Score range 1–4, higher subscores suggest stronger beliefs about the negative impact of the HSV diagnosis on the future. Overall Subscale Mean = 2.96, SD = 0.44.
Cause
The mean score for the Cause subscale was 3.45 (0.47), which indicates that young women recognized the sexual risk behaviors that are associated with HSV transmission (Table 2). The sexual behaviors that most women perceived as very likely to transmit HSV were: vaginal sex without a condom with someone who has HSV (82.5%, n = 249), oral sex without a condom with a person who has HSV (77.3%, n = 232) and having several sexual partners (69.8%, n = 210). Behaviors seen by fewer people as very likely to transmit HSV were: having sex with someone whose sexual history is unknown (54.2%, n = 162), a one-night stand (48%, n = 144), vaginal sex without a condom with a new partner (44.7%, n = 134) and sexual contact with another woman (41.5%, n = 125).
Table 2.
HSV Representations: Cause Dimension
| What is your chance of getting HSV: | Low n (%) |
Somewhat Low n (%) |
Somewhat High n (%) |
High n (%) |
|---|---|---|---|---|
| When you have vaginal sex without a condom with someone who has HSV? | 1 (0.3) | 15 (5.0) | 37 (12.3) | 249 (82.5) |
| When you have several sexual partners? | 2 (0.7) | 21 (7.0) | 68 (22.6) | 210 (69.8) |
| When you have oral sex without a condom with a person who has HSV? | 8 (2.7) | 6 (2.0) | 54 (18.0) | 232 (77.3) |
| When you have vaginal sex without a condom with a new partner? | 10 (3.3) | 47 (15.7) | 109 (36.3) | 134 (44.7) |
| When you have a one-night stand? | 7 (2.3) | 42 (14.0) | 107 (35.7) | 144 (48.0) |
| When you have sex with someone and you don’t know about his or her sexual past? | 5 (1.7) | 36 (12.0) | 96 (32.1) | 162 (54.2) |
| Through sexual contact with another woman? | 12 (4.0) | 41 (13.6) | 123 (40.9) | 125 (41.5) |
Score range 1–4, higher subscores indicate greater recognition of the sexual risk behaviors associated with HSV transmission. Overall Subscale Mean = 3.45, SD = 0.47.
Psychosocial consequences
The mean score for the Psychosocial Consequence subscale was 3.60 (0.43), which indicates that young women believed an HSV diagnosis would have a negative impact on their mental health and intimate relationships (Table 3). The notion that HSV is a stigmatizing disease was reflected in the women’s responses as 95% believed that it was likely (22%, n = 33) or very likely (84%, n = 252) that they would feel ashamed or embarrassed following an HSV diagnosis and 90% believed that it was likely (13.4%, n = 40) or very likely (76.6%, n = 229) that they would feel depressed after an HSV diagnosis.
Table 3.
HSV Representations: Psychosocial Consequence Dimension
| Not likely n (%) |
Somewhat likely n (%) |
Likely n (%) |
Very likely n (%) |
|
|---|---|---|---|---|
| Having HSV would negatively affect the way my sexual partner sees me | 1 (0.3) | 7 (2.3) | 34 (11.3) | 258 (86.0) |
| Having HSV would cause my sexual partner to not want to be with me anymore | 20 (6.7) | 35 (11.7) | 66 (22.1) | 178 (59.5) |
| Having HSV would make me feel ashamed or embarrassed | 6 (2.0) | 9 (3.0) | 33 (11.0) | 252 (84.0) |
| Having HSV would cause me to stop having sex | 24 (8.0) | 48 (16.0) | 76 (25.3) | 152 (50.7) |
| Having HSV would cause me to stop trusting my sexual partners | 8 (2.7) | 21 (7.0) | 54 (17.9) | 218 (72.4) |
| Having HSV would cause my sexual partner to stop trusting me | 6 (2.0) | 33 (11.0) | 51 (16.9) | 211 (70.1) |
| Having HSV means I would always have to use a condom when I have sex | 4 (1.3) | 11 (3.7) | 22 (7.4) | 261 (87.6) |
| Having HSV would make me feel depressed | 8 (2.7) | 22 (7.4) | 40 (13.4) | 229 (76.6) |
| If I had HSV, I would worry about telling a new sexual partner that I had HSV | 17 (5.7) | 13 (4.3) | 32 (10.7) | 237 (79.3) |
| Having HSV would run my sex life | 19 (6.3) | 28 (9.3) | 80 (26.6) | 174 (57.8) |
| If I told someone that I had HSV they would not want to have sex with me | 5 (1.7) | 9 (3.0) | 49 (16.3) | 238 (79.1) |
| If I had HSV I would worry about having to tell my current sexual partner | 7 (2.3) | 7 (2.3) | 37 (12.3) | 249 (83.0) |
Score range 1–4, higher subscores suggest stronger beliefs about the negative impact of the HSV diagnosis on mental health and intimate relationships. Overall Subscale Mean = 3.60, SD = 0.43.
Concerns about intimate partners were also common
Nearly all of the women believed that an HSV diagnosis would be likely (11.3%, n = 34) or very likely (86%, n = 258) to negatively affect the way they are viewed by their sexual partners. To the extent that 82% believed that it was likely (22.1%, n = 66) or very likely (59.5%, n = 178) that an HSV diagnosis would cause their sexual partners to end the relationship. Further, 90% believed that an HSV diagnosis was likely (17.9%, n = 54) or very likely (72.4%, n = 218) to cause them to stop trusting their sexual partner.
The women also commonly reported that an HSV diagnosis would impact their sexual behavior. Specifically, 84% believed that an HSV diagnosis would be likely (26.6%, n = 80) or very likely (57.8%, n = 174) to ruin their sex life and 75% indicated that an HSV diagnosis was likely (25.3%, n = 76) or very likely (50.7%, n = 152) to cause them to stop having sex. Finally, partner notification following an HSV diagnosis was also a major concern. Nearly all women, 95%, believed that they would be likely (12.3%, n = 37) or very likely (83%, n = 249) to worry about telling their current sexual partner about an HSV diagnosis and 90% of women indicated that they would be likely (10.7%, n = 32) or very likely (79.3%, n = 237) to worry about telling future sexual partners about an HSV diagnosis.
Identity
The mean score for the Identity subscale was 2.69 (0.51), indicating that the women believed that symptoms of an HSV infection were likely (Table 4). Nearly all (96%) believed that they would be likely (9.3%, n = 28) or very likely (86.7%, n = 261) to have genital sores if they had HSV. The majority (68%) also believed that they would be likely (31.2%, n = 94) or very likely (36.5%, n = 110) to be able to tell if their sexual partner had HSV.
Table 4.
HSV Representations: Identity Dimension
| Not likely n (%) |
Somewhat likely n (%) |
Likely n (%) |
Very likely n (%) |
|
|---|---|---|---|---|
| Having HSV will affect my appearance | 89 (29.6) | 51 (16.9) | 74 (24.6) | 87 (28.9) |
| If I had HSV, I would have physical symptoms | 9 (3.0) | 40 (13.3) | 83 (27.6) | 169 (56.1) |
| If I had HSV, I would have genital sores | 2 (0.7) | 10 (3.3) | 28 (9.3) | 261 (86.7) |
| If I had HSV, I would feel sick | 143 (47.8) | 99 (33.1) | 31 (10.4) | 26 (8.7) |
| If I had HSV, I would having burning when I urinate | 93 (31.2) | 76 (25.5) | 70 (23.5) | 59 (19.8) |
| If I had HSV, I would have genital discharge | 116 (39.2) | 87 (29.4) | 54 (18.2) | 39 (13.2) |
| I could tell if my partner had HSV | 51 (16.9) | 46 (15.3) | 94 (31.2) | 110 (36.5) |
Score range 1–4, higher subscores suggest the endorsement of more physical symptoms associated with the HSV. Overall Subscale Mean = 2.69, SD = 0.51.
Specific Aim 2: To examine whether HSV representations differ based on age and history of STD testing.
A t-test was conducted to determine whether differences existed in the HSV RoSTD subscales scores based on age (Table 5). A significant difference was found only for the Identity subscale. Women who were younger (18–20 years) (t = −4.63, df = 295.92, p <.01) were more likely to believe that an HSV infection causes more symptoms when compared to those who were older (21–24 years). A similar analysis was completed to determine whether differences existed in the HSV RoSTD subscale scores based on history of STD testing (Table 6). Again, only the Identity subscale was significant. Those who had never received STD testing had higher scores on the Identity subscale (i.e., reported more symptoms related to HSV) compared to those who had been tested (t = −3.68; df = 286, p < .01).
Table 5.
T-Tests for HSV RoSTD subscales by Age
| Dimension | Age | n | M | SD | t | df | p |
|---|---|---|---|---|---|---|---|
| Futureb | 18–20 | 168 | 2.96 | 0.48 | −.05 | 296.85 | 0.96 |
| 21–24 | 132 | 2.96 | 0.36 | ||||
| Cause | 18–20 | 169 | 3.48 | 0.48 | 1.08 | 299 | 0.28 |
| 21–24 | 132 | 3.42 | 0.46 | ||||
| Psychosocial | 18–20 | 169 | 3.63 | 0.41 | 1.38 | 299 | 0.17 |
| 21–24 | 132 | 3.56 | 0.44 | ||||
| Identityb | 18–20 | 168 | 2.80 | 0.52 | −4.6 | 295.92 | 0.00a |
| 21–24 | 132 | 2.54 | 0.45 |
Note:
= Significant t-test at p ≤ 0.05.
= Significant Levene’s Test for Equality of Variance, t-test results for unequal variances reported.
Table 6.
T-Tests for HSV RoSTD subscales by STD Testing History
| Dimension | STD testing history |
n | M | SD | t | df | p |
|---|---|---|---|---|---|---|---|
| Futureb | Yes | 187 | 3.01 | 0.36 | 1.66 | 148.56 | 0.10 |
| No | 101 | 2.91 | 0.55 | ||||
| Cause | Yes | 188 | 3.44 | 0.47 | −.58 | 287 | 0.56 |
| No | 101 | 3.47 | 0.49 | ||||
| Psychosocial | Yes | 188 | 3.59 | 0.43 | −.36 | 287 | 0.72 |
| No | 101 | 3.61 | 0.43 | ||||
| Identity | Yes | 187 | 2.60 | 0.50 | −3.7 | 286 | 0.00a |
| No | 101 | 2.83 | 0.53 |
Note:
= Significant t-test at p ≤ 0.05.
= Significant Levene’s Test for Equality of Variance, t-test results for unequal variances reported.
Specific Aim 3: To examine the relationship between women’s beliefs about the psychosocial consequences of HSV and their beliefs about symptoms, future perspective and cause.
Pearson’s correlations were conducted to examine the relationship between the Psychosocial Consequence subscale and Identity, Future Perspective, and Cause subscales. Significant positive correlations were found between the Psychosocial Consequence subscale and Identity (r = .31, p < 0.01) Future Perspective (r = .35, p < 0.01), and Cause (r = .14, p = 01). Negative beliefs about the psychosocial consequences of HSV were associated with beliefs about HSV being symptomatic, having a negative impact on future health, and being associated with sexual risk behaviors.
DISCUSSION
This study provides insight into young women’s beliefs about HSV. Although HSV affects 20.9% of women in the United States1, only 0.7% (n = 2) of our sample indicated that they had been diagnosed with HSV. Similar self-reported HSV prevalence has been found in another sample of young adults.18 The fact that most of the women in this study did not self-report HSV is a strength of this study as it provides unique insight into the HSV beliefs of those in a high-risk group (based on age and sex).3 However, given the known prevalence rates of HSV among women, it is likely that some participants were unaware they were infected with HSV.
Future Perspective
A number of misconceptions about the chronicity of HSV were identified. We found that 15% of women inaccurately believed they could die from an HSV infection. Further, some believed that HSV could be cured, that a pill could get rid of the infection, and that there would be very little they could do to control a HSV infection. These findings suggest that this population needs additional education about health implications of HSV as well as the role of antiviral therapies in managing an HSV infection. We identified a significant correlation between beliefs about the negative impact of an HSV diagnosis on health and the severity of the negative psychosocial consequences of a diagnosis. It is not surprising that those who believe an HSV diagnosis is likely to have a more negative impact on their health (such as death or limited control over management) were more likely to perceive a more severe impact on their mental health and intimate relationships. Improving the accuracy of women’s understanding of the long-term health implications and controllability of HSV may help reduce the perceived negative psychosocial consequences.
Cause
In general the young women understood the sexual risk behaviors associated with HSV transmission. However, the behavior that the fewest women indicated as likely for transmission of HSV was sexual contact with another woman. This suggests that women may not understand the risks involved in female-to-female sexual contact, which occurs in approximately 9.4% of young women (18–29 years of age), regardless of sexual orientation.19 Additionally, the behaviors rated by the majority as the most likely to transmit HSV were the sexual behaviors with persons already known to be infected with HSV. Although these beliefs are completely accurate, these findings may suggest that women underestimate the actual prevalence rates of HSV, particularly given the high rate of people with undiagnosed HSV.1 Further, we identified that less than half of the women believed that a one night stand and sex with a new partner were very likely modes of transmission. This is concerning given the high HSV prevalence and the lower levels of disclosure of an HSV diagnosis with unsteady sexual partners.20, 21 Women at high-risk for HSV underestimate their risk.12 Additional research is needed to examine the relationship between perceived and actual HSV prevalence.
Psychosocial Consequences
The women had very negative beliefs about the impact of an HSV diagnosis on their mental health and intimate relationships. Nearly all women believed they would be likely to experience depression, embarrassment and anxiety following an HSV diagnosis. A likely reason for the strong beliefs about the negative psychosocial consequences is the significant stigma associated with HSV and other STDs.8 A number of studies corroborate the serious psychological impact of an HSV diagnosis.10, 22, 23 Given the relationship between daily distress, HSV shedding and frequency of outbreaks,24 interventions that address psychological implications of a new HSV diagnosis are warranted. Further, there is a need for interventions aimed toward the general population to reduce the stigma associated with STDs overall.
Concerns about the impact of an HSV diagnosis in several areas of intimate relationships were also noted. First, women believed that an HSV diagnosis would negatively affect relationships including violating trust within a relationship and concern about the ability to maintain a relationship after a diagnosis. Second, women commonly had beliefs about the negative impact of an HSV diagnosis on their sex life including their sex life being ruined, the need for long-term abstinence and no longer being viewed as sexually desirable. Third, women would be concerned about notifying both current and future sexual partners about an HSV diagnosis. Intimate relationships following an HSV diagnosis are of high concern among young women. Self-management interventions for those diagnosed with HSV should be inclusive of counseling to manage the complex relational and sexual implications. This may include validating that sexual self-worth is not dependent on absence of disease and that fulfilling sexual relationships are possible even after an HSV diagnosis.25 This should be balanced with education about how to reduce risk of transmission to partners and support for partner notification. The importance of partner notification cannot be overlooked as disclosure to partners may result in a decreased risk of HSV transmission.26
Finally, previous research has found that an HSV diagnosis was unrelated to the adoption of safer sex practices.27 Although our sample commonly indicated they would be likely to stop having sex after an HSV diagnosis, the reality is that long-term abstinence is unlikely and unwarranted. Diagnosis alone is not enough to motivate safer sex practices.27 This provides further support of the need for counseling specific to sexual activity following an HSV diagnosis.
Identity
The women commonly believed that HSV is symptomatic; 96% believed it results in genital sores and 68% believed they could tell if their partner had HSV. However, the majority of HSV infections are asymptomatic or have symptoms other than pronounced genital sores and that transmission can occur in the absence of symptoms.1 We also identified that women who had never been tested for STDs were more likely to believe that HSV would be symptomatic. This does raise concern about the potential for missed screening opportunities as young women may rely upon presence of symptoms to be an impetus for STD testing. A lack of knowledge of asymptomatic infections is a barrier to STD testing,28 conversely the presence of symptoms is a predictor of HSV testing intent.29 Thus education about symptomatic and asymptomatic infections is necessary to ensure that those at-risk are screened. HSV testing is currently recommended only for those who are symptomatic.30 In the absence of screening recommendations for those who are asymptomatic, we believe that testing should be left to the discretion of health care provider who can counsel women who may be at-risk to receive testing.
We identified a significant positive correlation between beliefs about the presence of symptoms and the negative psychosocial consequences of HSV. Given this correlation, educating women about the actual symptomatology of an HSV infection (which often has minimal symptoms or symptoms that decrease over time1) may help reduce the extent of their negative psychosocial concerns. Further, because there is evidence that people with recurrent symptomatic HSV infections are more likely to have consistent anxiety,24,31 controlling physical symptoms with the use of antiviral medication may also help reduce the negative psychosocial impact of an HSV diagnosis. Although future research is needed to examine this relationship, the benefits of suppressive therapy may not only reduce HSV transmission1 but may also positively impact psychosocial adjustment following an HSV diagnosis.32
Future Research
Our findings give direction for two additional areas of future research not previously mentioned. First, since illness representations are in part formed through personal experience, future research should also examine whether differences in representations exist based on personal experience with HSV (i.e., personal, family or acquaintance). Second, the HSV RoSTD comprehensively examines women’s beliefs about HSV along four dimensions and creates an excellent foundation for developing patient-centered interventions to address beliefs. However, it is important to note that identifying additional knowledge based beliefs about HSV held by women such as prevalence, detailed HSV pathophysiology (e.g., incubation periods) and even understanding of the term “virus” may also be important for guiding interventions aimed to improve general knowledge of HSV and/or improve management of those infected.
Limitations
These findings must be interpreted within the limitations of this study. First, the sample was well-educated and relatively racially homogenous which limits the ability to generalize the findings. Further, the cross-sectional design precludes determination of causal relationships.
Conclusions
Even among young women who were well-educated, a number of HSV misconceptions were identified. These misconceptions indicate a clear need for improved public education about this exceedingly common infection. Not only will education better inform the general public and reduce misconceptions, but open communication may also reduce HSV- related stigma and perhaps allow for a better understanding and more open dialogue about HSV among those affected and their partners, friends and family. Health care providers should be cognizant of the common HSV misconceptions among women with particular emphasis on symptomatology as it seems to be associated with not only STD testing behavior but also appears to be related to psychosocial stress. Further, women have serious concerns about the psychosocial implications of an HSV infection. Interventions that comprehensively address these psychosocial concerns including psychological well-being and intimate relationships are needed. The development of novel peer support interventions aimed to address these psychosocial concerns is also an area worthy of attention. In the absence of comprehensive HSV management guidelines, understanding women’s beliefs about HSV gives insight into direction for both clinical care and guideline development.
Acknowledgements
This research was financially supported in part by the National Institute of Nursing Research grants F31NR009580 and T32NR007102, the Midwest Nursing Research Society, and the University of Wisconsin-Madison, School of Nursing.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Heather Rhea Royer, Assistant Professor, University of Wisconsin-Milwaukee, College of Nursing, PO Box 413, 1921 E. Hartford Avenue, Milwaukee, Wisconsin, United States of America 53211, hrroyer@uwm.edu, 1-414-229-2597 (Office), 1-414-299-3989 (Fax).
Elizabeth C. Falk, Nurse Practitioner, University Health and Counseling Services, University of Wisconsin-Whitewater Whitewater, Wisconsin, United States of America.
Susan M. Heidrich, Helen Denne Schulte Emeritus Professor at the University of Wisconsin-Madison School of Nursing, Madison, Wisconsin, United States of America; Nurse Scientist at the Wm.S. Middleton Memorial Veterans Administration Hospital, Madison, Wisconsin, United States of America.
References
- 1.Centers for Disease Control and Prevention. Genital Herpes - CDC Fact Sheet. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [cited 2011 April 26]. updated July 13, 2010 Available from: http://www.cdc.gov/std/herpes/stdfact-herpes.htm. [Google Scholar]
- 2.Auslander BA, Biro FM, Rosenthal SL. Genital herpes in adolescents. Seminars in Pediatric Infectious Diseases. 2005;16(1):24–30. doi: 10.1053/j.spid.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Batalden K, Bria C, Biro FM. Genital herpes and the teen female. J Pediatr Adolesc Gynecol. 2007;20(6):319–321. doi: 10.1016/j.jpag.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Stanberry LR, Rosenthal SL, Mills L, Succup PA, Biro FM, Morrow RA, et al. Longitudinal risk of herpes simplex virus (HSV) type 1, HSV type 2, and cytomegalovirus infections among young adolescent girls. Clin Infect Dis. 2004;39:1433–1438. doi: 10.1086/425307. [DOI] [PubMed] [Google Scholar]
- 5.Szucs T, Berger K, Fisman D, Harbarth S. The estimated economic burden of genital herpes in the United States. An analysis using two costing approaches. BMC Infect Dis [Internet] 2001;1(1):5. doi: 10.1186/1471-2334-1-5. Available from: http://www.biomedcentral.com/content/pdf/1471-2334-1-5.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neal TMS, Lichtenstein B, Brodsky SL. Clinical implications of stigma in HIV/AIDS and other sexually transmitted infections. Int J STD AIDS. 2010;21:158–160. doi: 10.1258/ijsa.2008.008445. [DOI] [PubMed] [Google Scholar]
- 7.Merin A, Pachankis JE. The psychological impact of genital herpes stigma. J Health Psychol. 2011;16(1):80–90. doi: 10.1177/1359105310367528. [DOI] [PubMed] [Google Scholar]
- 8.Hood JE, Friedman AL. Unveiling the hidden epidemic: a review of stigma associated with sexually transmitted infections. Sex Health. 2011;8:159–170. doi: 10.1071/SH10070. [DOI] [PubMed] [Google Scholar]
- 9.Romanowski B, Zdanowicz YM, Owens ST. In search of optimal genital herpes management and standard of care (INSIGHTS): doctors' and patients' perceptions of genital herpes. Sex Transm Infect. 2008;84(1):51–56. doi: 10.1136/sti.2007.027631. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert LK, Omisore F. Common questions about herpes: analysis of chat-room transcripts. Herpes. 2009;15(3):57–61. [PubMed] [Google Scholar]
- 11.Rana RK, Pimenta JM, Rosenberg DM, Tyring SK, Paavonen J, Cook SF, et al. Demographic, behavioral, and knowledge factors associated with herpes simplex virus type 2 infection among men whose current female partner has genital herpes. Sex Transm Dis. 2005;32(5):308–313. doi: 10.1097/01.olq.0000162363.82005.fe. [DOI] [PubMed] [Google Scholar]
- 12.Roth AM, Dodge BM, Pol BVD, Reece M, Zimet GD. Low acceptance of HSV-2 testing among high-risk women. Int J STD AIDS. 2011;22:329–331. doi: 10.1258/ijsa.2010.010399. [DOI] [PubMed] [Google Scholar]
- 13.Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to medical psychology. Oxford, UK: Pergamon Press; 1980. pp. 7–30. [Google Scholar]
- 14.Leventhal H, Nerenz DR, Steele DJ. Illness representation and coping with health threats. In: Baum A, Taylor SE, Singer JE, editors. Handbook of psychology and health: Social psychological aspects of health. Vol. 4. Hillsdale, NJ: Erlbaum; 1984. pp. 219–252. [Google Scholar]
- 15.Royer HR, Heidrich SM, Brown RL. Young women's representations of sexually transmitted diseases (RoSTD): A psychometric study. Res Nursing Health. 2012;35:15–29. doi: 10.1002/nur.21452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. 2003;18(2):141–184. [Google Scholar]
- 17.Royer HR, Falk EC. Young women's beliefs regarding human papillomavirus. J Obstet Gynecol Neonatal Nurs. 2012;41(1):92–102. doi: 10.1111/j.1552-6909.2011.01309.x. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert LK, Levandowski BA, Roberts CM. Characteristics associated with genital herpes testing among young adults: assessing factors from two national data sets. J Am Coll Health. 2011;59(3):143–150. doi: 10.1080/07448481.2010.497522. [DOI] [PubMed] [Google Scholar]
- 19.Xu F, Sternberg MR, Markowitz LE. Women who have sex with women in the United States: prevalence, sexual behavior and prevalence of herpes simplex virus type 2 infection-results from national health and nutrition examination survey 2001–2006. Sex Transm Dis. 2010;37(7):407–413. doi: 10.1097/OLQ.0b013e3181db2e18. [DOI] [PubMed] [Google Scholar]
- 20.Bickford J, Barton SE, Mandalia S. Chronic genital herpes and disclosure…the influence of stigma. Int J STD AIDS. 2007;18:589–592. doi: 10.1258/095646207781568484. [DOI] [PubMed] [Google Scholar]
- 21.Green J, Ferrier S, Kocsis A, Shadrick J, Ukoumunne OC, Murphy S, et al. Determinants of disclosure of genital herpes to partners. Sex Transm Infect. 2003;79:42–44. doi: 10.1136/sti.79.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamill M, Goldmeier D. Patients support innovative models of care in recurrent genital herpes clinics: results from a patient satisfaction study. Int J STD AIDS. 2005;16(9):615–617. doi: 10.1258/0956462054944499. [DOI] [PubMed] [Google Scholar]
- 23.Mark H, Gilbert L, Nanda J. Psychosocial well-being and quality of life among women newly diagnosed with genital herpes. J Obstet Gynecol Neonatal Nurs. 2009;38(3):320–326. doi: 10.1111/j.1552-6909.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- 24.Strachan E, Saracino M, Selke S, Magaret A, Buchwald D, Wald A. The effects of daily distress and personality on genital HSV shedding and lesions in a randomized, double-blind, placebo-controlled, crossover trial of acyclovir in HSV-2 seropositive women. Brain Behav Immun. 2011;25(7):1475–1481. doi: 10.1016/j.bbi.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newton DC, McCabe MP. Sexually transmitted infections: impact on individuals and their relationships. J Health Psychol. 2008;13(7):864–869. doi: 10.1177/1359105308095058. [DOI] [PubMed] [Google Scholar]
- 26.Wald A, Krantz E, Selke S, Lairson E, Morrow RA, Zeh J. Knowledge of partners' genital herpes protects against herpes simplex virus type 2 acquisition. J Infect Dis. 2006;194(1):42–52. doi: 10.1086/504717. [DOI] [PubMed] [Google Scholar]
- 27.Crosby RA, Head S, DiClemente RJ, Meyerson B, Troutman A. Do protective behaviors follow the experience of testing positive for herpes simplex type 2? Sex Transm Dis. 2008;35(9):787–790. doi: 10.1097/OLQ.0b013e318177a068. [DOI] [PubMed] [Google Scholar]
- 28.Myers JL. Why do young women get tested for sexually transmitted infections? Evidence from the national longitudinal study of adolescent health. J Womens Health (Larchmont) 2011;20(8):1225–1231. doi: 10.1089/jwh.2010.2544. [DOI] [PubMed] [Google Scholar]
- 29.Kelly NC, Zimet GD, Aalsma MC, Bernstein DI, Fortenberry JD, Rosenthal SL. Intent to accept and acceptance of herpes testing in adolescents and young adults. Sex Transm Infect. 2009;85(4):296–299. doi: 10.1136/sti.2008.032847. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Genital Herpes Screening – Frequently asked qusetions. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [cited 2012 October 24]. updated August 30, 2011 Available from: http://www.cdc.gov/std/herpes/screening.htm. [Google Scholar]
- 31.Carney O, Ross E, Bunker C, Ikkos G, Mindel A. A prospective study of the psychological impact on patients with a first episode of genital herpes. Genitourinary Medicine. 1994;70:40–45. doi: 10.1136/sti.70.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel R, Tyring S, Strand A, Price MJ, Grant DM. Impact of suppressive antiviral therapy on the health related quality of life of patients with recurrent genital herpes infection. Sex Transm Infect. 1999;75(6):398–402. doi: 10.1136/sti.75.6.398. [DOI] [PMC free article] [PubMed] [Google Scholar]