Abstract
Background
Research on resilience in the aftermath of potentially traumatic life events is still evolving. For decades researchers have documented resilience in children exposed to corrosive early environments, such as poverty or chronic maltreatment. Relatively more recently the study of resilience has migrated to the investigation of isolated and potentially traumatic life events (PTE) in adults.
Methods
In this article we first consider some of the key differences in the conceptualization of resilience following chronic adversity versus resilience following single-incident traumas, and then describe some of the misunderstandings that have developed about these constructs. To organize our discussion we introduce the terms emergent resilience and minimal-impact resilience to represent trajectories positive adjustment in these two domains, respectively.
Results
We focused in particular on minimal-impact resilience, and reviewed recent advances in statistical modeling of latent trajectories that have informed the most recent research on minimal-impact resilience in both children and adults and the variables that predict it, including demographic variables, exposure, past and current stressors, resources, personality, positive emotion, coping and appraisal, and flexibility in coping and emotion regulation.
Conclusions
The research on minimal impact resilience is nascent. Further research is warranted with implications for a multiple levels of analysis approach to elucidate the processes that may mitigate or modify the impact of a PTE at different developmental stages.
Keywords: emergent resilience, minimal-impact resilience, traumatic events, latent growth mixture modeling (LGMM)
Bad things can and do happen. As much as we might wish it otherwise, acute and highly aversive events such as natural disaster, serious injury, and the death of loved ones have plagued humans at every stage of the life cycle. While these events are usually intensely distressing for both children and adults, it has become abundantly clear that over the longer term not everyone reacts in the same way (Bonanno, 2004; Bonanno, Westphal, & Mancini, 2011). Indeed, although in common parlance such events are referred to as “traumatic”, in actuality because of the wide range in outcomes they evoke, these events are more appropriately described as “potentially traumatic events” or PTEs (Norris, 1992; Bonanno, 2004).
In this paper, we review the growing body of research on resilience to isolated PTEs and the factors that predict it. We begin by considering how resilience to PTEs might be defined, and pay special attention to some of the misunderstandings that have surrounded the construct. In part, we attribute these definitional misunderstandings to the fact that the psychological study of resilience was originally advanced in the literature on chronic adversity in children, and then only later migrated to the adult literature on single-incident trauma. Because single-incident trauma is phenomenologically distinct from chronic adversity, however, the study of resilience in the context of a PTE necessitated a degree of conceptual readjustment (Bonanno, 2004, 2005, 2012; Bonanno & Mancini, 2008; Masten & Narayan, 2012). We review the nuances of these adjustments in some detail and discuss some of the misunderstandings they have generated. To organize our discussion and to extend and integrate previous work on divergent pathways of adjustment (e.g., Bonanno, 2004; Masten & Narayan, 2012), we introduce the terms emergent resilience and minimal-impact resilience to represent trajectories of positive adjustment in the context of chronic adversity and single-incident trauma, respectively. We then describe the some of the recent statistical advances in latent trajectory modeling and briefly review each of the prototypical trajectories identified in response to isolated PTEs. Because emergent resilience has been well studied in the developmental literature, we devote the remainder of the paper to reviewing the relatively new research on minimal-impact resilience and the factors that predict it.
Developmental Origins and Conceptual Migration
The term “resilience” has been in broad use for centuries, and over time has taken on a diverse assortment of meanings. It is only in the past several decades, however, that resilience has gained currency as a psychological construct. The term first began to appear in the 1970s in the developmental literature on chronic adversity (Garmezy, 1972; Kagan, 1976; Kagan & Klein, 1973; Rutter, 1979). Much of the research on human development at the time was focused on the etiology of psychopathology. The focus began to shift however as a result of pioneering research by developmental psychologists, psychiatrists and other mental health professionals documenting the large numbers of children who, despite growing up in highly aversive circumstance, nonetheless emerged as functional and capable individuals (Garmezy, 1991; Murphy & Moriarty, 1976; Rutter, 1979; Werner, 1995). The term resilience was in fact defined in earlier work as a relatively positive psychological outcome in spite of exposure to severe risk experiences (Rutter, 2006). This research effectively broadened the corpus of developmental theory to encompass positive adaptation and adjustment. A growing literature on resilience using a life course perspective then focused on understanding positive developmental outcomes as well as the ability of individuals who had suffered from setbacks and multiple adversities in adolescence to show evidence of competent functioning across multiple domains in adulthood, including social relationships, job performance, and marriage (Gralinski-Bakker, Hauser et al., 2004; Sampson & Laub, 1992; DiRago & Vaillant, 2007; Vaillant & Davis, 2000).
The evolution of developmental research on resilience has been summarized in four broad phases (Masten 2011; Rutter, 2000). To review briefly, in its earliest phases this work focused on the measurement and definition of resilience, with particular interest on attempting to understand the factors that were associated with positive outcomes in those exposed to adverse conditions. Identification of the differences between those who did well and those who did not was paramount. A considerable bulk of the research indicated that there were in fact great consistencies across resources, individual qualities and relationships as predictors of resilient outcomes. The exploration then expanded in a second phase of the research that moved beyond the mere identification of resilience factors and toward elucidating and understanding the specific processes that led to resilience. The movement beyond the mere description of protective factors was succinctly stated by Masten (2011) as the “how” questions in the resilience research. This objective, which encompassed several disciplines, was to ascertain using multiple levels of analysis and by considering neurobiological processes how individuals cope with stressful situations and adverse conditions. As research and theory progressed, this phase also generated a great deal of interest in preventative interventions. Finally, the most recent phase of developmental research and theory on resilience has moved toward an integrative perspective that can encompasses genes, neurobehavioral development and statistical analyses, and explores moderators of risk as well as the role of neural plasticity in resilience (Rutter, 2000; Sandler, Wolchik, Ayers, Tein, Kwok, Haine & Towhey-Jackobs, et al, 2008; Masten & Wright, 2010).
Emergent resilience
A key aspect of the observations about resilience in the developmental literature is that the vast majority of this research has focused on the emergence of favorable adjustment in the face of chronically aversive circumstances, including chronic poverty (Garmezy, 1993; Luthar, 1999), parental bereavement, civil war, and natural disasters (Luthar & Brown, 2007; Sandler et al., 2003; Betancourt, 2011). The study of positive outcomes in such enduring and pervasively aversive contexts in turn naturally lends itself to a contextual frame that emphasizes the measurement of adjustment over the broad sweep of time, and as a result, the conceptual understanding of resilience in the context of chronic adversity has tended to focus on long-term or distal outcomes (Masten 2001, Masten & Narayan, 2012).
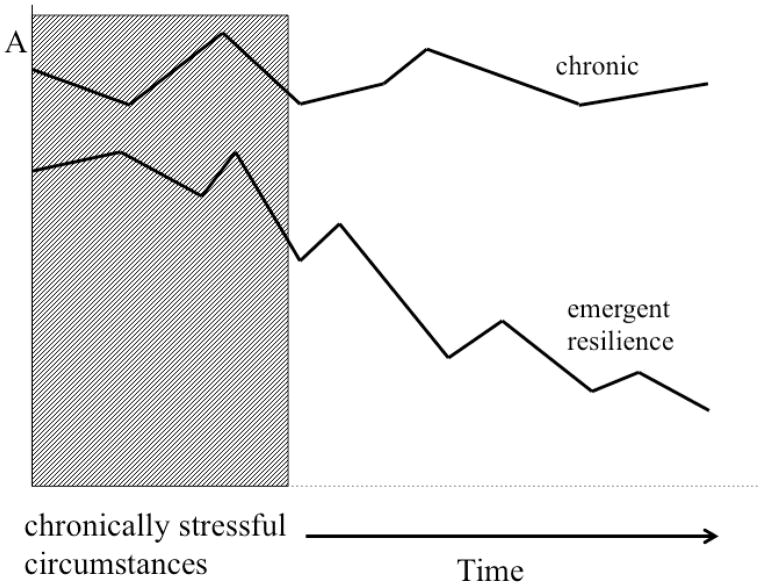
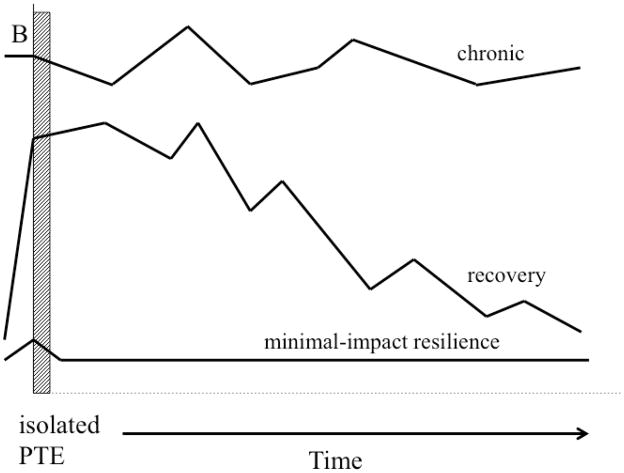
We refer to this form of resilience as emergent resilience (see Figure 1a). In humans isolated stressors typically produce transient perturbations in normal adjustment and functioning (e.g., Bisconti, Bergeman, & Boker, 2004; de Kloet, DeRijk, & Meijer, 2011). By contrast, chronically stressful and aversive circumstances tend to produce more enduring patterns of variability and tend to lead to more enduring changes in a wide-range of psychological and physiological functions (de Kloet et al., 2011; Offidani & Ruini, 2012). Assessments of overall adaptation in chronically stressful circumstances are necessarily relative, tempered by time and changing context, and in such circumstances the distinction between resilience and maladjustment is often not fully apparent until after the stressful context has to some degree abated (Masten & Narayan, 2012). A child might struggle for years against the caustic influence of an ongoing abusive family context, for example, but could reasonably be described as resilient if he or she eventually survived those influences and went on to meet normal developmental milestones and culturally relevant expectations for competence, (Elder, 1998; Masten & Coatsworth, 1995; Waters & Sroufe, 1983) and psychological adjustment (Luthar, Ciccetti, & Becker, 2000).
Figure 1. Graphic comparison of minimal-impact and emergent resilience.
The upper panel (a) represents minimal-impact resilience as a stable trajectory of healthy adjustment following an isolated PTE, with recovery as a gradual return to baseline. The lower panel (b) represents emergent resilience as a gradual movement toward healthy adjustment following a period of struggle with chronically aversive circumstances. The overall figure was modified from a similar figure presented by Masten and Narayan (2012). Aspects of panel 1a were adapted specifically from Masten and Narayan (2012) and aspects of panel 1b were adapted from Bonanno (2004).
The pivotal objective of developmental scientists concerned with emergent resilience has been to isolate factors that might contribute to the child’s long-term ability to modify the deleterious effects of caustic life circumstances, identifying key mechanisms or vulnerability markers found to exacerbate or ameliorate negative outcomes following aversive conditions. As a consequence, the last several decades of developmental research on resilience has identified factors that correlate with positive outcomes in “at risk” youth and more recent scholarly interest has focused on understanding the biological mediators of risk and processes underlying vulnerability and protective factors (Luthar, 2006).
Minimal-impact resilience
A somewhat different perspective on resilience has begun to emerge only in the past decade or so as the construct began to capture the attention of researchers and theorists who were primarily interested in the mental health and psychological well-being of adults (Bonanno, 2004; Bonanno et al., 2002: Ryff & Singer, 2002; Ryff, Singer, & Dienberg-Love, 2004). In contrast to the focus on chronic adversity and the gradual emergence of signs of favorable adjustment that characterized the developmental studies, the bulk of research on extreme adversity in adults has focused on loss, trauma and other forms of acute life events. Typically, but not always, these events occur as isolated stressors in an otherwise normative or non-caustic environment. Not surprisingly, then, when researchers and theorists interested in adult mental health began making observations about resilience, the conceptual focus shifted from chronic adversity and distal outcomes to more isolated, acute events and to relatively proximal patterns of healthy adjustment (Bonanno, 2004, 2005; Bonanno & Mancini, 2008; Bonanno et al., 2011).
Within this more acute context the nature of resilience necessarily takes on a different form, which we label minimal-impact resilience (see Figure 1b). As we elaborate in greater detail below, in contrast to the struggle with chronic adversity, which presents an organism with considerable psychological and biological challenges, isolated, acute stressors allow for more focused and relatively more proscribed coping efforts. As a result, rather than describe a gradual sweep toward positive outcome, the minimal-impact resilience following acute stressor events suggests little or no lasting impact on functioning and a relatively stable trajectory of continuous healthy adjustment from before to after the PTE.
Unfortunately, the research and theory on the types of positive outcomes we refer to as emergent resilience and minimal-impact resilience respectively, have developed in relative isolation from each other. This schism has lead to a somewhat fragmented body of literature that has yet to be adequately integrated. To make matters worse, different forms of resilience have been routine described using the same single word, resilience. Finally, the problems inherent in this kind of lexical ambiguity have been exacerbated by a number of conceptual misunderstandings (Bonanno, 2012; Panter-Brick & Eggerman, 2012). In the pages that follow, we review the most prominent of these misunderstandings and then attempt to elucidate in more detail how we understand the specific trajectory we have labeled minimal-impact resilience.
The Limits of Diagnoses and the Problem of Averages
One of the primary sources of misunderstanding in the broader psychological literature on adversity stems from a widely held assumption that long-term outcomes following significant life events can be captured by a single homogenous pattern of change (Duncan, Duncan, & Strycker, 2006; Muthén, 2004). This assumption has driven the approaches that have dominated the study of PTEs (see Bonanno et al., 2011). The most common perspective in the trauma literature, which we will call the diagnostic approach, conceptualizes responses to PTEs almost exclusively in terms of the simple, binary distinction between chronic psychopathology, such as posttraumatic stress disorder (PTSD) or Complicated Grief (CG) versus the absence of psychopathology. The study of resilience to PTEs is also often framed in simple, binary terms of pathology versus resilience (e.g., Feder, Nestler, & Charney, 2009; Rutter, 1985; Yehuda et al., 2006).
From a public health perspective the diagnostic approach makes perfect sense because it facilitates identification of those most in need of therapeutic intervention. Indeed, the diagnostic approach has fostered considerable advances in the development of research and intervention strategies. For example, the formal recognition of PTSD as a legitimate diagnostic category in the DSM lead to a marked surge in research on the etiology, prevalence, neurobiology, and treatment of extreme trauma reactions (McNally, 2003). The same increase in research also been evident in response to the recent articulation of diagnostic criteria for CG (Boelen, de Keijser, van den Hout, & van den Bout, 2007; Bonanno, Neria et al., 2007; Horowitz, Siegel et al., 1997; Shear, Frank, Houck, & Reynolds, 2005).
Despite these gains, it is important to note the crucial limitations of the diagnostic approach. An obvious problem is the lingering controversies that tend to surround diagnostic categories. Diagnostic entities are largely conceptual rather than empirical. As a consequence, determining precise empirical boundaries for these categories has proved elusive. The diagnostic criteria for PTSD for example have gradually expanded to allow greater weight to the subjective experience of trauma. This kind of “bracket creep” (McNally, 2003) has had the unintended consequences of reducing the validity of the diagnosis. In a similar vein, taxometric analyses, which determine the extent that a given dimension might form a natural latent boundary or category have consistently failed to support the assumed categorical integrity of both PTSD (M. Ruscio, J. Ruscio, & Keane, 2002; Broman-Fulks, Ruggiero, et al., 2006) and CG (Holland, Neimeyer, Boelen, & Prigerson, 2009). Rather, these analyses suggest that PTSD and CG are best understood as continuous dimensions and that any categorical variable that is used with these dimensions will be to some extent arbitrary.
The limitations of the diagnostic approach become markedly more pronounced when applied to the study of resilience. One major problem, for example, is that the diagnostic approach provides essentially no useful information about the distribution of individual differences. In other words, the demarcation of the presence or absence of psychopathology says nothing about the different types or variations in non-pathological responses to PTEs and other forms of adversity. Rather, the diagnostic approach simply lumps individuals who do not meet diagnostic criterion into a single, homogenous category. Of particular relevance to this article, the diagnostic approach says almost nothing about the prevalence or form of resilient outcomes (Bonanno et al., 2011). Indeed, for all intents and purposes, the study of resilience using a diagnostic approach provides no new information at all. Defining resilience as the absence of diagnosable psychopathology is essentially identical to defining pathology. Moreover, in a binary system (i.e., psychopathology versus non-psychopathological), the variables that predict an absence of psychopathology will always be the same variables that predict psychopathology; only the direction of prediction changes. In other words, if an absence of social support predicts psychopathology, then the presence of social support predicts the absence of psychopathology.
To put this more succinctly, in the words of Almedom and Glandon (2007), defining resilience as the absence of a disorder is akin to defining health as the absence of disease. We would not equate a person who is physically fit, within their expected weight range, and suffers only occasional minor illness with a person who has difficulty with any form of physical exercise, over- or under-weight, and constantly struggling with myriad health problems. If neither person were suffering from a major disease, we would not lump both individuals into the same category of not having a disease because, clearly the former case is healthier than the latter. Similarly, we should not equate someone with minimal symptoms and distress, the capacity for laughter and enjoyment, and positive social interactions with someone who suffers moderate or sub-clinical depression or anxiety, rarely enjoys positive experiences, and has conflicted social relations simply because neither meet criteria for a known form of psychopathology.
An alternative to the diagnostic approach that to some extent obviates the problem of arbitrary boundaries is to conceptualize responses to aversive life events in terms of average-level differences between exposed and non-exposed groups, or in terms of changes in average-level responses over time. This approach is focused primarily on the event itself rather than on individual reactions to the event. For example, studies using this approach have observed that on average PTSD symptoms are elevated in the weeks following exposure to a PTE and then rapidly decline. The rate of decline tapers off, however so that exposed groups will still show elevated symptoms relative to non-exposed groups for several years and often longer (Breslau, 2001). Average-level symptom scores have proved especially informative in studies that seek to determine within-group predictors of grief or posttraumatic outcome. Average-level scores are also informative in meta-analytic studies that summarize data across multiple data sets (e.g., (Currier, Neimeyer, & Berman, 2008; Norris, Friedman et al., 2002). Finally, as we note below, average-level outcomes have been used to understand general levels of adjustment as a form of resilience.
Unfortunately, the same type of problems that limited the definition of resilience as the absence of pathology is inherent in attempts to understand resilience using an average-level approach. Average-level approaches do provide descriptive details about the distribution of outcome scores, such as sample mean and standard deviation. However, in the aftermath of PTEs, more often than not these data are misleading because outcome data following PTEs is typically non-normal (Galatzer-Levy & Bonanno, 2012). Outcome data following PTEs are typically skewed. If measures of symptoms and distress are used to assess outcome, for example, then the data will typically be positively skewed, with a greater proportion of scores centered near the low symptom end of the scale and relatively fewer scores reaching the upper levels of symptoms and distress. In this case, measures of central tendency and variation will most likely obscure rather than illuminate the true nature of individual variation.
These points are best illustrated when we consider the literature on individual differences or trajectories of adjustment following PTEs (Bonanno, 2004; Bonanno et al., 2011). Most people exposed to PTEs do not develop lasting psychopathology and among this broad category, clear individuals differences in prospective or longitudinal patterns of adjustment have been consistently observed. Among these patterns is a stable trajectory of healthy adjustment or minimal-impact resilience that can be empirically distinguished from other non-pathological patterns, such as gradual recovery, improved adjustment, and delayed reactions. Moreover, as recent advances in latent growth modeling have shown, the variability in these different trajectories is not necessarily identical, which further underscores their unique characteristics. Average-level outcome scores condense this information into a single and often misleading pattern. Indeed, trajectory of change over time produced by average-level data often depicts a pattern that is not actually represented in the data (Bonanno et al., 2011).
Minimal-Impact Resilience as a Stable Trajectory of Healthy Functioning
We have argued above and elsewhere (Bonanno, 2004, 2005, 2012; Bonanno & Mancini, 2008; Bonanno et al., 2011) that resilience in the aftermath of an isolated PTE cannot be defined simply as the categorical absence of psychopathology or as average-level outcomes. Rather, as we elaborate below, resilience following an isolate PTE is most validly measured as a stable trajectory of healthy functioning before and after the event (i.e., minimal-impact resilience).
Although resilience is often described as a process, the only context in which it is realistically possible to understand that process is when there is a clearly referenced adversity and a clear, conceptually defensible outcome in response to that adversity (Bonanno, 2004; Luthar et al., 2000). These kinds of considerations are particularly apt in the study of minimal-impact resilience following PTEs. Although the effects of isolated PTEs can be enduring, the events themselves are typically characterized by a clearly observable and definable onset and offset. The parameters of outcome trajectories following a PTE are also clearly observable and definable. In contrast to the traditional approach to PTEs, which suggested a single homogeneous outcome distribution centered around a sample mean, recent advances in research and theory on the impact of significant life events more broadly defined has dramatically underscored the heterogeneity of long-term outcomes (Curran & Hussong, 2003; Duncan et al., 2006; Feldman, Maysn, & Conger, 2009; Muthén, 2004). Developmental researchers have long underscored the heterogeneity of response to adversity (e.g., Rutter, 1999). The perspective we advance here, and elsewhere encapsulates the heterogeneity of outcomes following PTEs (Bonanno, 2004, 2005; Bonanno, & Mancini 2008, 2012; Bonanno et al., 2011). More specifically, we have argued that individual differences in long-term outcome from pre- to post- PTEs are best captured by a set of prototypical trajectories (e.g., Bonanno, 2004). The form and proportion of these trajectories has been remarkably consistent across studies. Most prominent among these trajectories is a long-term outcome pattern we had referred to in past research as the resilience trajectory (Bonanno, 2004; Bonanno et al., 2010, 2011) and which we describe here as a form of minimal-impact resilience.
Latent Growth Modeling
Conceptually and in the practical reality of life event research, a minimal-impact resilience trajectory is only one of any number of possible longitudinal patterns that might be observed. In the early research on individual differences following PTEs, operationally defining a resilient pattern was a complex and not entirely uncontroversial matter. Although definitional issues are still far from resolved, thanks to recent statistical advances in latent growth modeling, it is now possible to determine the shape and frequency of these trajectories using a primarily empirical approach. As we noted earlier, in a traditional diagnostic perspective on trauma, variations in outcome are necessarily limited to pre-determined categories of adjustment. In the average-level approach to aversive life events, variations in outcome are also limited, in this case to a single, homogeneous distribution centered on the mean response pattern. Even advanced versions of the average-level approach, such as hierarchical linear modeling (HLM), are bounded by the same assumption of homogeneity. By contrast, newly developed latent growth modeling (LGM) techniques, such as latent class growth analysis (LCGA) and latent growth mixture modeling (LGMM), are able to relax the assumption of a single population. As a result, LGM approaches are able to identify heterogeneous subpopulations that comprise distinct response trajectories across time (Feldman et al., 2009).
The key feature of LGM is the incorporation of both continuous and categorical latent variables. Latent continuous variables are random effects that define parameters of growth across time (e.g., intercept, slope, and quadratic parameters). Growth parameters may also be defined to capture the idiosyncratic features of the sampled population (e.g., longitudinal variations in college student distress that conform to variation in the academic calendar (Galatzer-Levy, Burton, & Bonanno, 2012). These parameters may be fixed or may be allowed to vary across unobserved populations or trajectory classes, which are identified through latent categorical variables that group participants according to differing trajectories of growth. The number of trajectory classes in the final model is determined primarily by a set of fit statistics. Although the final trajectory model is also to some extent influenced by existing theory and interpretive rationale (Muthén, 2004), compared to more traditional approaches, LGM comes closest to allowing the data to speak for itself independent of a priori theoretical assumptions.
The empirical study of variations in long-term adjustment in relation to isolated PTEs has used both traditional growth modeling techniques and more recently the LGM approach. Although variation across studies is to be expected, the overall corpus of research in this area has been remarkably consistent in observing a finite set of common or prototypical trajectories. In Figure 2, we represent the six trajectories most commonly observed in research on isolated PTEs.
Figure 2. Prototypical outcome trajectories following isolated PTEs.
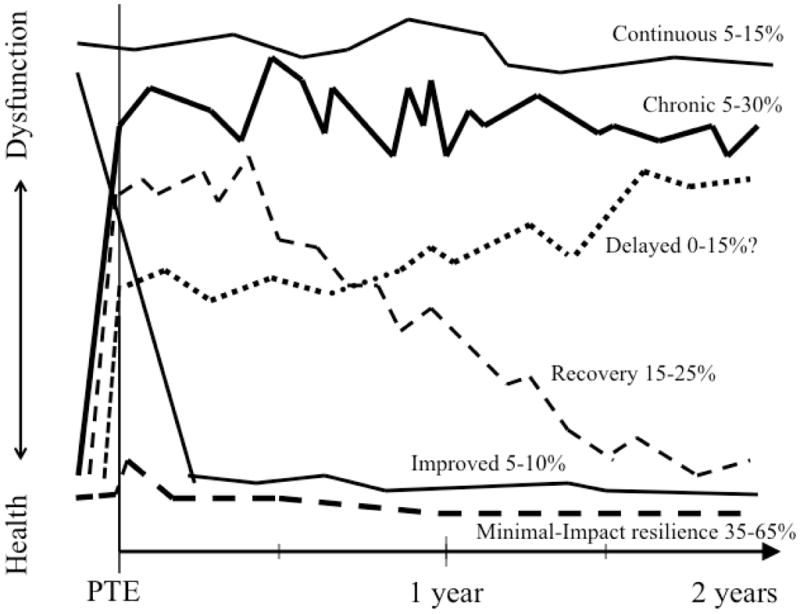
The six most common longitudinal trajectories observed in research on individual variation in response to isolated, potentially traumatic life events (PTEs). The health-dysfunction axis represents elevated symptoms and distress at one end and positive adjustment and the relative absence of symptoms and distress at the other end. The figure is adapted and expanded from Bonanno (2004).
Chronic dysfunction
The most obvious of the patterns illustrated in Figure 2, the chronic dysfunction trajectory, extends the diagnostic approach to PTEs by explicitly defining elevated symptoms and distress as a longitudinal pattern. More specifically, the chronic dysfunction trajectory describes a pattern in which symptom elevations are evident relatively soon after the occurrence of the PTE and continue unabated for several years and often longer. A key advantage of the trajectory approach over the more traditional diagnostic category approach however is that the threshold for chronic dysfunction need not be fixed nor established in advance. In other words, a chronic dysfunction trajectory may be defined simply by the fact that a group of individuals exhibit more or less the same basic pattern of elevated symptoms over time regardless of whether or not they had all met pre-determined diagnostic criteria for membership in a pathological category.
The minimal-impact resilience trajectory
The trajectory of adjustment associated with minimal-impact resilience is characterized by consistently low levels of symptoms and distress, or consistently positive adjustment, both before and after the occurrence of the PTE; in other words, a stable trajectory of healthy functioning. From a LGM perspective, minimal-impact resilience is defined by the latent category of participants who exhibit more or less the same pattern of healthy adjustment across time. Because latent categories can lead to definitional ambiguities, Bonanno (2012) proposed that the following criteria be used to clarify and evaluate the validity of evidence for minimal-impact resilience following isolated PTEs, as well as guide future research on the construct: (1) the temporal bounds of the PTE should be clearly operationally defined and (2) minimal-impact resilience should be explicitly categorized as a stable pattern of healthy adjustment following that event that is (a) more than the absence of diagnosable pathology, (b) based on measurements obtained at multiple points in time, (c) beginning as soon as possible after the occurrence of the aversive event (e.g., within several months or sooner) and if possible before the event (i.e., as pre-event baseline measurements).
Minimal-impact resilience versus resistance
The minimal-impact resilience trajectory does not necessarily imply a complete absence of a stress response, which has been referred to in the developmental literature as stress resistance (Layne, Warren, Shalev, & Watson, 2007; Masten, 2011). The vast majority of people exposed to PTEs, including those evidencing a minimal-impact response typically experience at least some transient distress during or immediately after the event (e.g., Bonanno, Wortman, & Nesse, 2004), The crucial point however is that in minimal-impact resilience the stress reaction is usually relatively mild, transient, and typically does not impact the ability to continue normal levels of functioning (Bonanno, 2004). Moreover, whereas complete stress resistance appears to be relatively rare (Layne, Steinberg et al., 2004), the transient stress associated with minimal-impact resilience is typically the most common outcome observed (Bonanno, 2004; Bonanno et al., 2011).
Minimal-impact resilience versus recovery
In contrast to the minimal-impact resilience pattern of stable adjustment, the recovery trajectory represents the prototypical arc of recovery from the impact of a PTE. More specifically, the recovery trajectory describes a pattern in which moderate to severe symptoms and distress are observed soon after the PTE and endure for at least several months before gradually declining to baseline levels of adjustment over the course of one or two years. The comparison of recovery with chronic adversity had emerged as an important avenue from which to understanding of development of clinically relevant grief and trauma reactions (Coifman & Bonanno, 2010; Yehuda & LeDoux, 2007). By contrast, the distinction between recovery and minimal-impact resilience has at times proved more elusive (e.g., King, King et al., 1999).
From the perspective we advance in this article, the confusion surrounding the distinction between resilience and recovery is due to a blurring of the distinction between chronic adversity and isolated PTEs (Bonanno, 2004; Bonanno & Mancini, 2008; Masten, Best, & Garmezy, 1990). An isolated PTE is a potentially traumatic life event that occurs in otherwise normal circumstances (Bonanno, 2005). In this context, minimal-impact resilience describes a trajectory in which there are only mild and transient disruptions in functioning and an otherwise stable pattern of adjustment from before to after the PTE. In this same context, the recovery trajectory connotes a significant but relatively short-lived (i.e., from several months to several years) disruption in normal functioning caused by the PTE and then a gradual return to the pre-trauma or normative baseline. In other words, a person showing this pathway was relatively healthy (i.e., had few psychiatric symptoms and showed clear signs of positive adjustment) prior to the PTE, then experienced a marked increase in symptoms and distress after the PTE and was only able to return to baseline levels of health after a considerable period of time had passed. The confusion arises, because the recovery trajectory bears some relation to the type of gradual movement toward health that characterizes emergent resilience. Indeed, in the context of prolonged or severe adversity, emergent resilience has been described as recovery (Masten et al., 1990). Although the temporal duration of the recovery trajectory following an isolated PTE is generally shorter than the recovery pattern described as emergent resilience, both trajectories share the same gradual arc toward healthy adjustment (see Figures 1a and 1b).
Importantly, only a very small portion of the research on adults exposed to chronic and enduring aversive situations has examined trajectories of adjustment. However, the available evidence suggests that when adversity is pervasive and enduring in adults sample, emergent resilience rather than minimal-impact resilience will be the common outcome. In one of the few studies of this type available, for example, Hobfoll et al. (2011) examined population-level data on adjustment at multiple time points over a 12 month period among Palestinians living in the disputed territories. The level of exposure to war violence, death and injury was extreme in this population, prompting the authors to describe their sample in terms of “chronic mass casualty.” Hobfoll et al. (2011) found little evidence in this context for the kind of stable healthy adjustment or minimal-impact resilience we have described in this article. Rather, they reported a common trajectory characterized by moderately elevated symptoms of PTSD and depression and then gradual improvement. In the context of an isolated PTE, this pattern would have connoted recovery. However, in the context of chronic and extreme adversity, this gradual movement toward healthy adjustment is more appropriately considered prognostic of emergent resilience.
Delayed symptom elevations
Another somewhat controversial but far less common trajectory describes an arc of increasing symptom elevations over time. Historically the delayed pattern was based largely on theoretical assumptions about the denial of grief and trauma reactions. Genuine resilience was thought to be rare, and consequently it was assumed that delayed grief and trauma typically emerged “out of the blue” among seemingly healthy individuals who had actively denied their initial distress (Bonanno, 2004, 2009; Wortman & Silver, 1989).
Several decades of longitudinal study suggests an alternative and more nuanced view (Andrews, Brewin, Philpott, & Stewart, 2007). In the context of bereavement, the available evidence argues that delayed grief may not occur at all, at least not as a common pattern of response. Several longitudinal bereavement studies have, for example, explicitly tested for delayed reactions and not found them (Bonanno & Field, 2001; Middleton, Burnett, Raphael, & Martinek, 1996). In the context of PTEs, the existence of delayed trauma reactions has also been called into question (Bryant & Harvey, 2002). A number of recent studies have however provided solid evidence for delayed elevations in PTSD symptoms. Importantly, delayed symptoms elevations in these studies did not describe a pattern of normal adjustment followed by a sharp rise in symptoms to the level of pathology, as predicted by the traditional denial theories. Rather, delayed symptoms were characterized by an initial moderate or sub-threshold level of symptoms levels that gradually worsened over time (e.g., Bonanno, Rennicke, & Dekel, 2005; Buckley, Blanchard, & Hickling, 1996; deRoon-Cassini et al., 2010). Thus delayed reactions are best described as an exacerbation of existing symptoms (Andrews et al., 2007).
Continued pre-existing distress and distress followed by improvement
Although the four patterns described above, chronic distress, minimal-impact resilience, recovery, and delayed elevations, tend to effectively capture most of the variation in long-term responses to PTEs, other trajectory patterns are also sometimes observed. One such pattern is a continuous pre-existing distress trajectory that describes a level of enduring impairment that pre-dates the PTE and continues afterwards. Since in the normal population, there is always a small but predictable subset of people with elevated symptoms and distress, it stands to reason that this group would be captured by longitudinal trajectory studies (e.g., Bonanno, Wortman et al., 2002). What is important to consider though is that in the absence of prospective data, people who experience continuous pre-existing distress are difficult to distinguish from people who were otherwise well adjusted prior to the marker PTE and only developed more pathological levels of symptoms in response to the PTE.
Another pattern sometimes observed, the distress-improvement trajectory, is characterized by elevated distress prior to the PTE that decreases markedly after the event. This pattern has been observed in prospective studies of bereavement (Bonanno, Wortman et al., 2002; Bonanno, Moskowitz, Papa, & Folkman, 2005; Schulz, Mendelsohn et al., 2003) and of combat deployment (Bonanno, Mancini et al., 2012; Dickstein, Suvak, Litz, & Adler, 2010). The distress-improvement pattern should not be confused with stress-related growth. Rather, the pattern represents a return to a normative or baseline level of adjustment. Although it is not clear that a single phenomenon drives this pattern, the most likely explanation is that improvement following a PTE results because the PTE in some way alleviates a previous extreme form of stress (Wheaton, 1990). During bereavement, the distress component of the trajectory has been associated with the stress of caregiving for an ill loved one while the improvement component of the trajectory has been described as relief from the stress of caregiving after the loved one’s death (Bonanno, 2009; Schulz et al., 2003). In the military studies, the distress component has been understood as reflection of anxieties about a pending combat deployment, whereas the improvement component reflects relief once the deployment is initiated (Dickstein et al., 2010).
Acute Adversity in Adults
In the next section, we consider in greater detail the empirical evidence in support of the construct of minimal-impact resilience as a trajectory of healthy adjustment following a PTE. Research on the mental health of New Yorkers after 9/11, for example, indicated that an impressive majority of New Yorkers evidenced minimal-impact resilience. The initial research assessed a large, representative sample of New York adults for the prevalence of trauma symptoms sampled repeatedly over the first 6 months after the attack. Although this initial research did not model trajectories, the use of repeated assessments allowed for an implicit categorization of minimal-impact resilience. A clear majority (65%) experienced only one or no trauma symptoms during this period, had almost no depression and reported significantly less substance use than other participants (Bonanno, Galea, Bucciarelli, & Vlahov, 2006, 2007). Even at considerably higher levels of exposure (e.g., people who were inside the World Trade Center (WTC) at the time of the attack), the proportion of respondents without symptoms remained high. A subsequent study examined data from this same population over a longer period of time and used a modeling approach similar to LGM (Norris, Tracy, & Galea, 2009). In this case, trajectories indicative of minimal-impact resilience were identified in 53% of the New Yorkers surveyed. Finally, another study modeled trajectories of both PTSD symptoms and depression symptoms in a smaller, independently collected sample with high levels of direct exposure to the 9/11 attacks (e.g., participants were in or near the World Trade Center at the time of the attack)(Bonanno, Rennicke, & Dekel, 2005). The proportion of this sample showing a minimal-impact trajectory for each outcome measure was similar to the groups in previous studies that had experienced high levels of exposure. Importantly, in further validation of the minimal-impact pattern, participants assigned to this trajectory also reported significantly less negative affect in response to being interviewed about their experiences on 9/11 and were independently and confidentially described as resilient by their long-time friends and relatives.
A growing number of studies have now mapped trajectories of minimal-impact resilience following a range of significant life transitions and PTEs. These studies defined minimal-impact resilience either as the stable trajectory of little or no symptoms and distress or as consistently high levels of positive health indicators (e.g., high well-being and life satisfaction) across time. Across all these studies the minimal-impact resilience trajectory was always the most common pattern observed. Prospective research on significant life transitions has, for example, found the minimal-impact trajectory of stable high well-being to be the most common pattern following job loss (Galatzer-Levy, Bonanno, Mancini, 2010), divorce, and bereavement (Mancini, Bonanno, & Clark, 2011). Research on PTEs using both prospective and longitudinal designs has reported that the minimal-impact resilient trajectory was the most common outcome observed following a diverse array of highly threatening and demanding events, including the death of a spouse or partner (Bonanno et al., 2002; Bonanno, Moskowtiz, Papa, & Folkman, 2005; Mancini et al., 2011), natural and man-made disaster (Bonanno, Ho et al., 2008; Norris, Tracy, & Galea, 2009; Tang, 2007), life-threatening medical procedures (Deshields, Tibbs, Fan, & Taylor, 2006; Lam et al., 2010), traumatic injury (deRoon-Cassini, Mancini, Rusch, & Bonanno, 2010), spinal cord lesion (Bonanno et al., in press), and deployment in military operations (Bonanno, Manciniet al., 2012; Dickstein et al., 2010).
Acute Adversity in children
What about resilience to PTEs in children? Millions of children worldwide are exposed to aversive life events and despite their high-risk status many experience good developmental outcomes (Laufer & Solomon, 2006). As we noted, however, the study of resilience in children has focused primarily on chronic and ongoing adversity and on patterns of emergent resilience. Developmental research has also gradually expanded to encompass children’s adjustment in the context of putatively acute stressor events, such as natural disasters and parental bereavement. Of note, however, given the emphasis in developmental science on the broader ecological context, much of this work has understandably retained the emphasis on emergent resilience and eschewed conclusions about minimal-impact resilience.
A poignant illustration of the complexity of this issue from a developmental perspective is provided by the case of parental bereavement. Population data indicate that approximately 4% of children in the United States under the age of 18 are likely to experience the death of a parent. The loss of a parent is indisputably one of the more grave stressors a child might face and several studies have presented intriguing yet mixed findings when assessing mental health problems in bereaved children. Depressive symptoms, social withdrawal and conduct problems have been evidenced in some children (Sandler, Wolchik, & Ayers, 2007) while other well-designed studies have found no association between a child’s mental health and the death of a parent (Chase-Landale, Mott, Brooks-Gunn, & Phillips, 1991).
How do we reconcile such diverse findings? Sandler et al (2008) proposed that the bereavement experience of a child must be considered as a process rather than an acute life event and, although resilience is the desired outcome, adaptation is what best characterizes the process. Resilience as defined by Sandler is thus “contextual” and emphasizes the role that person and environment has on healthy adaptation. Thus, although parental bereavement is a significant stressor for a child, it is necessarily conceptualized in more chronic or distal terms due to the varying long term effects and the changes over time as well as the child’s available resources for adapting to the loss following the death.
Another reason for the paucity of development research on minimal-impact resilience is that even when developmental researchers have turned their lens toward specific PTEs, the ecological emphasis in developmental science has tended to focus that lens widely to encompass the broader and more chronically aversive contextual backgrounds. For example, research on the impact of war in adults has generally pertained to deployed soldiers with and without acute combat exposure (Dohrenwend et al., 2006). By contrast, studies of how children are affected by war have understandably tended to focus more on the broader ecological context (Betancourt & Kahn, 2008). Betancourt and colleagues, for example, have assessed mental health outcomes in children following exposure to pervasive war violence, in particular the striking case of child soldiers caught up in the civil war in Sierra Leone. These researchers similarly argued that adjustment and mental health in children exposed to war violence must be viewed as a dynamic process wherein resilience is conceptualized from a socio-ecological perspective, inclusive of family systems, social support, and community settings extending beyond cultural belief systems (Betancourt et al, 2008; Betancourt et al., 2010, Betancourt, & Khan, 2008).
Children’s exposure to war is both an extreme disruption in the context of development and signifies an immediate threat to physical endangerment. Yet, there is also considerable variability to war-related PTE’s, both in context and by individual factors, such as gender. Developmental scientists have attempted to contextualize the role of the child and environment using an ecological perspective that considers family, school (micro), and characteristics of the neighborhood (meso), in addition to culture and society (macro) (Garbarino & Ganzel, 2000; Panter-Brick & Eggerman, 2012). In such a perspective, the quality of family relationships becomes central to developmental resilience (Sandler, et al. 2008) and, as we noted previously, the frame of reference for conceptualizing resilience necessarily expands to more distal outcomes.
These considerations point up the crucial importance of ongoing development processes and raise important questions about how these processes might interact with and inform childhood resilience. It is commonly assumed, for example, that trauma-exposed children who evidence resilience in one sphere of mental health may nonetheless suffer deficits in other areas. Multidimensional data from which to address this question are not yet available. However, indirect evidence challenges whether the assumption may apply to resilience following isolated potential traumas. A number of studies have demonstrated, for example, that children who do not develop PTSD after exposure to war-related stress do not differ from non-exposed controls in many important spheres of adjustment, such as academic achievement (Saigh, Mroueh, & Bremner, 1997), learning or memory performance (Yasik, Saigh, Oberfield, & Halamandaris, 2007), and the absence of behavioral problems (Saigh, Yasik et al., 2002).
Only a relatively limited number of studies on childhood adversity have focused on specific PTEs occurring as isolated events in otherwise normative (i.e., not chronically aversive) contexts (Norris et al., 2002; LaGreca, Silverman, Vernberg & Roberts, 2002). For example, recent studies have assessed children in New York City following 9/11 (Hoven, Duarte et al.,2005), in response to natural disasters, such as earthquakes (Chen & Wu, 2006) and hurricanes (La Greca, Silverman, Lai, & Jaccard, 2010), and in the context of war (Panter-Brick, Goodman, Tol & Eggerman, 2011; Saigh, Yasik et al., 2002). Although this research provided a great deal of useful information, and met many of the criteria for the study of minimal-impact resilience, most of these studies did not explicitly identify a minimal-impact trajectory and relied, instead, on the simple binary distinction between psychopathology and the absence of psychopathology.
In one of the only studies we are aware of to explicitly identify longitudinal trajectories in youth following an isolated PTE, Le Brocque, Hendrikz, and Kenardy (2010) tracked a sample of 190 children, ages 6 to 16, after they were hospitalized for a serious traumatic injury. They identified the best-fitting trajectories of posttraumatic stress symptoms using an LGM approach on data obtained within 72 hours of hospitalization and extending across several outcome points up to two-years post-hospitalization. The results were strikingly similar to those obtained on research on adults exposed to isolated PTEs. Specifically, similar to deRoon-Cassini et al.’s (2010) study of traumatic injury with adults, Le Brocque et al. (2010) reported that the majority of the children (57%) hospitalized for traumatic injury exhibited a stable trajectory of consistently low symptoms of posttraumatic stress, or minimal-impact resilience. Another third of the sample (33%) evidenced a gradual return to baseline adjustment and suggesting of the pattern we have labeled “recovery.”
Predictors of Minimal-Impact Resilience
Although research that explicitly defines multiple outcome patterns is nascent, sufficient data has accrued to allow for at least a preliminary catalogue of the factors that uniquely predict a minimal-impact resilient trajectory. Before we review these factors, two important points are worth considering.
First, no single predictor is likely to exert a dominant influence on resilient outcomes. Traditionally, trauma theorists have tended to assume that minimal-impact resilience, or stable healthy adjustment following PTEs, was rare. Consequentially, within this perspective it was assumed that resilience to PTEs could only result from extraordinary mental health or a denial-like state associated with dysfunction and psychopathology (Bonanno, 2004, 2009). The fact that minimal-impact resilience is not rare but, as abundant research has now shown, typically the most common outcome trajectory observed following PTEs clearly indicates the need for a different conceptualization. Because such a large portion of exposed individuals evidence minimal-impact resilience, for example, we should expect there to be considerable heterogeneity among resilient individuals. In other words, the large group of people showing the minimal-impact trajectory will tend to vary across demographic profiles, personality, life history, past and current stressors, social and economic resources, and a host of other factors.
Developmental researchers have long observed that children faced with chronically aversive life circumstances who manage to accomplish normal developmental milestones and exhibit healthy adjustment or emergent resilience appear to utilize an array of resilience-promoting factor. These included person-centered variables (e.g., personality), contextual factors (e.g., supportive relations) (e.g., Werner, 1985), and broader socio-cultural factors. We should expect the same to be true for minimal-impact resilience in both children and adults confronted with PTEs. Resilience, in other words, is not likely to result from one or even several factors but rather from multiple, independent predictors, with each accounting for a relatively small portion of the variance (Bonanno et al., 2011) and in many cases modified or mediated by other factors (Panter-Brick & Eggman, 2012). The available evidence is consistent with this point. Multivariate studies of risk and resilience factors measured in the aftermath of PTEs clearly shows that such factors tend to coalesce in a cumulative or additive manner, such that each contributes to or subtracts from the overall likelihood of a minimal-impact outcome (Bonanno, Galea et al., 2007).
Second, the overall matrix of risk and resilience factors is fluid and will likely change over time (Bonanno et al., 2010). It is important to remind ourselves that PTEs are by definition almost always unexpected and can occur in almost any context and at any point in the life cycle. However many of the factors that might predict how people respond to PTEs are also likely to change over time. Some of these factors that might predict resilience will be relatively more stable over time (e.g., personality) while others will likely fluctuate dramatically as life circumstances change or as various resources become more or less accessible (Hobfoll, 1989, 2002). At different points in time, then, the same person may be more or less resilient to acutely aversive life events, depending on both their recent history and the broader context of their lives.
Given these considerations, what are the factors that might combine to predict minimal-impact resilience? Below we briefly review some of the major categories of predictors that have emerged in recent research.
Demographic Variation
An obvious set of factors likely to inform minimal-impact resilient is demographic variables. Here we consider age, gender, and race/ethnicity.
Age
Age is often thought to describe a curvilinear risk factor. That is, both older adults and young children are assumed to be at greatest risk for negative outcomes following PTEs. Early reviews of the disaster literature have suggested, for example, that children may more frequently exhibit psychological impairment compared to adult disaster survivors (Norris et al., 2002). More recent reviews have noted, however, that research on children and disaster is methodologically heterogeneous and has frequently produced contradictory findings (Bonanno et al., 2010; Hoven et al., 2009) and no disaster studies have yet to explicitly measure the minimal-impact trajectory in children. Moreover, the only child study we are aware of that actually mapped trajectories of adjustment following a PTE is the Le Broque et al. (2010) study of traumatic injury, discussed earlier, and in that study the prevalence of minimal-impact resilience in children was strikingly similar to the prevalence of minimal-impact resilience obtained on research with adults exposed to isolated PTEs.
What about children in different age groups? There is some evidence to suggest that younger children are more fully impacted and less likely to show a rapid recovery from disaster-related PTSD than older children (Schwarzwald et al., 1994). The trajectory research in this case confirms this conclusion. Le Broque et al. (2010) reported that among children exposed to traumatic injury, older children were more likely to evidence a minimal-impact trajectory than were younger children.
At the opposite end of the age spectrum, the relative increase in dependency and physical vulnerability associated with aging has led to assumptions that older adults, like younger children are at greater risk following PTEs (Cook & Elmore, 2009). The empirical data fail to support this view. Although older adults tend to experience greater distress during disasters, they nonetheless evidence relatively lower long-term psychological costs than do younger adults (Huerta & Horton, 1978; Kato, Asuki et al., 1996; Knight et al., 2000). Following the 9/11 terrorist attacks, for example, older adults were more likely to exhibit the minimal-impact resilient pattern of stable healthy adjustment than were younger adults (Bonanno, Galea et al., 2007). Likewise, contrary to the assumption that older people frequently die of a broken heart in bereavement, older bereaved adults tend to have better adjustment (Bonanno & Kaltman, 1999; Mancini et al., 2011) and to show lower rates of mortality than younger bereaved adults (Martikainen & Valkonen, 1996; M. Stroebe & W. Stroebe, 1993). The positive adjustment seen in older adults has been attributed to their greater life experiences and knowledge gained from previous encounters with stressors (Knight et al., 2000) as well as their increased capacity to regulate negative emotion (Charles & Carstensen, 2010).
Gender
One of the more consistent predictors of resilience following PTEs in both children and adults is male gender (Brewin et al., 2000; Norris et al., 2002). Although the effects of gender are small, they are consistent and have held up in numerous studies that used multivariate modeling of possible confounding factors (Ahern, Galea et al., 2004; Bonanno, Ho et al., 2008; Bonanno, Galea et al., 2007; Carr et al., 1997a, b; Hoven, et al., 2005; Galea et al.,2008; Vernberg, LaGreca, Silverman, & Prinstein, 1996; Weems et al., 2010).
What might account for the consistency of the gender effect? One plausible explanation is that girls and women may experience greater objective exposure or may have previously experienced greater prior trauma than boys and men (Kimerling, Mack, & Alvarez, 2009). These experiences in turn would place women and possibly girls at greater risk than men and boys. Support for this explanation is weakened, however, by findings showing that the gender difference in trauma outcome has remained significant even in studies that controlled for exposure or prior trauma (Bonanno et al., 2010). Another possible explanation is that women and girls tend to subjectively experience greater initial threat during PTEs (Anderson & Manuel, 1994; Goenjian, Molina et al., 2001). This possibility has received some support from multivariate studies. Specifically, in several studies that showed an association between gender and trauma outcome, the gender effect disappeared when subjective trauma exposure was statistically controlled (Garrison, Weinrich et al., 1993; Norris et al., 2002).
Gender may also have other influences. For example, gender may moderate the impact of other variables. In a study of Kuwaiti children exposed to war violence during the Gulf war, for example, girls reported higher social support than boys but there was also a notable interaction of gender and social support. Social support ameliorated the impact of trauma exposure on distress in girls but not in boys (Betancourt & Khan 2008).
Race/Ethnicity
An oft-discussed risk factor pertains to racial and ethnic variation. However, empirical support for a link between racial/ethic differences and trauma outcome has been unconvincing. In disaster studies, for example, data on race and ethnicity is often limited or unavailable (Norris et al., 2002). In some studies, the lack of data can be attributed to the simple fact that communities most severely impacted by disasters are often racially and ethnically homogeneous (Bonanno et al., 2010). The vast majority of evacuees from Hurricane Katrina (94%), for example, identified as Black (Mortensen et al, 2009) whereas the vast majority of survivors of the 1993 Midwestern flood disaster (93%) were white (Ginexi et al., 2000). In some cases, the population under study was so homogeneous that race/ethnicity was not even assessed (Bonanno et al., 2010).
Studies in which race/ethnicity is more heterogeneous suffer from another problem. In this case, race/ethnicity is typically confounded with socio-economic status or other risk and resilience factors (Norris et al., 2002). Studies that that failed to control for such confounding factors often report significant racial/ethnic effects (e.g., Adams & Boscarino, 2005) and appear to indicate that certain racial/ethnic groups are less likely to evidence resilient outcomes (Bonanno, Galea et al., 2006). However, when multivariate analyses are possible and socioeconomic differences can be controlled, effects for racial/ethnic groups in both children and adults are often null (Bonanno, Galea et al., 2007; Hoven et al., 2005; Ruggiero et al., 2009).
Exposure
Bonanno and colleagues (2010) conceptualize the impact of exposure to PTEs on minimal-impact resilience and other outcome patterns in terms of the events and consequences that occur during the approximate period in which the PTE occurred, or proximal exposure, and events and consequences that arise in the PTE’s aftermath, such as the loss of resources or income, or distal exposure (Bonanno et al., 2010). Proximal exposure to PTEs has been consistently linked with greater levels of posttraumatic stress in both adults (Bonanno, Rennicke, & Dekel, 2005; Nolen-Hoeksema & Morrow, 1991) and children (La Greca, Silverman, Vernberg, & Prinstein, 1996). Importantly, although minimal-impact resilience is still often the most common outcome after even the severest of aversive life events, higher proximal exposure within an event nonetheless tends to reduce the prevalence of minimal-impact resilience levels for both children (Le Brocque et al. (2010) and adults (Bonanno et al., 2005, 2006) relative to less proximal exposure. Variables related to distal exposure have been found to describe a similar pattern of findings (see section of resources, below).
Personality
As developmental researchers have demonstrated in several classic longitudinal studies (Block, 1971, 1993; Robins et al., 1996), there is good reason to assume that personality may play at least some predictive role in resilient outcomes (e.g., Kim-Cohen et al., 2004). However, there has been considerable misunderstanding about the extent that personality traits inform resilience (Betancourt & Kahn, 2008; Bonanno, 2012; Bonanno & Mancini, 2008; Bonanno et al., 2011; Luthar, 2000).
A vital consideration here pertains to the timing of the assessments. Personality variables show at least some malleability across the lifespan. Changes in personality profiles are more pronounced during childhood, however, and appear to become more stable in adulthood (McCrea, Costa et al., 2000; Roberts et al., 2006). Unfortunately, in the vast majority of studies of personality and resilience in adults, the outcome measure and the personality measure are assessed concurrently with outcome (i.e., after the PTE had already occurred). Although personality is more stable in adulthood, it is not impervious to situational and environmental influences (McCrea et al., 2000). Consequently, the experience of a PTE is just as likely to have informed the personality variable as much as the other way around. This confound is especially likely in cases when the personality variable had been measured many months after the PTE (Bonanno & Mancini, 2008). Compounding the problem about direction of association is the simple fact that trait personality scales rarely explain more than a small portion of the actual variance in people’s behavior across situations (Mischel, 1969). Not surprisingly, when minimal-impact resilience is modeled using multivariate designs, most variables including personality variables produce relatively small effects (Bonanno, Brewin, Kaniasty, & La Greca, 2010).
The most compelling evidence for a role of personality in resilience comes from multivariate studies that measured the personality variable prior to the onset of the PTE. A small and growing number of studies meet this criterion. These studies have associated better outcome following a PTE with pre-event perceived control (Ullman & Newcomb, 1999), trait resilience (Ong et al., 2010), low negative affectivity (Weems et al., 2007), a ruminative response style (Nolen-Hoeksema & Morrow, 1991), and trait self-enhancement (Gupta & Bonanno, 2010). The latter study examined trait self-enhancement in relation to distress at various levels of exposure to PTEs. Low trait-self-enhancers had markedly increased distress at high levels of exposure. By contrast, high trait self-enhancers showed almost no change in distress across levels of exposure, suggesting a minimal-impact resilience pattern.
There is also a growing body of evidence linking personality explicitly with a minimal-impact outcome trajectory. Specifically, the minimal-impact resilience trajectory has been uniquely associated with trait self-enhancement among high exposure survivors of the 9/11 attacks in New York (Bonanno, Rennicke, & Dekel, 2005), with trait coping self-efficacy following traumatic injury (deRoon-Cassini et al., 2010), and with low negative affectivity and high positive affectivity following multiple physical traumas and spinal cord injury (Quale & Schanke, 2010).
Although the evidence demonstrating the role of personality in resilience outcomes is compelling, we strongly echo Luthar’s (2000) caution against equating personality with resilience. Illustrative of this trend is the growing number of ostensible measures of trait resilience that have begun to appear (e.g., Connor & Davidson, 2003; Friborg et al., 2003; Wagnild & Young, 1993). The explicit assumption is that these scales measure a resilient type. In other words, these scales promote the assumption that that people are resilient primarily because of who they are. The available evidence affirms that minimal-impact resilience is influenced to some extent by measureable traits. However, given the demonstrably small effects and general lack of prospective data, the assumption that resilience is primarily a matter of personality is clearly unfounded. We suggest therefore that personality is best thought of as one of many risk and resilience factors that might contribute to the course and ultimately the outcome of a person’s adjustment following PTEs (Bonanno & Mancini, 2008).
Social and Economic Resources
There is considerable research to support the association between social support resources and generally better adjustment following PTEs (Brewin et al,, 2000; Kaniasty & Norris, 2009; La Greca et al., 1996). Multivariate studies of disaster have also reported evidence linking social support uniquely with a minimal-impact resilience trajectory (Bonanno, Galea et al., 2007; Bonanno, Ho et al., 2008). Interestingly, prospective research on bereavement has failed to uphold the assumption that social support buffers the stress of loss (W. Stroebe, Zeck, M. Stroebe, & Abakoumkin, 2005). However, prospective bereavement research has shown that pre-bereavement levels of instrumental support (i.e., assistance with the tasks of daily living) do in fact predict the minimal-impact trajectory (Bonanno, Wortman et al., 2002).
Another important resource, education, has also been associated with the minimal-impact traejectory (Bonanno et al., 2007). However, somewhat surprisingly, although the availability of economic resources has consistently been linked with better adjustment following PTEs (Brewin et al., 2000; Norris et al., 2002), studies that have explicitly examined resilient outcome trajectories have failed to detect a relationship to economic variables (Bonanno, Rennicke, & Dekel, 2005; Bonanno, Galea et al., 2007). Importantly, however, as Hobfoll (1989, 2002) noted, the loss of resources is a primary source of event-related stress and not surprisingly individuals who experience significant resource loss (e.g., decrease in income) following a PTE were found to be less likely to exhibit a minimal impact resilience trajectory (Bonanno, Galea et al., 2007; Mancini et al., 2011).
Past and Current Stress
A considerable body of research associates past encounters with trauma and current life stress with both increased risk for PTSD (Brewin et al., 2000) and a decreased likelihood of minimal-impact resilience following PTEs (Bonanno et al., 2007). An important caveat in the findings regarding prior trauma however is that in the vast majority of this evidence was garnered retrospectively. Moreover, the little prospective research that is available indicates that only PTEs that actually result in PTSD tend to predict PTSD at subsequent exposure (Breslau, Peterson, & Schulz, 2008). In other words, exposure to PTEs in the past does not necessarily put someone at risk for subsequent trauma unless those PTEs had actually resulted in enduring psychopathology. It is worth noting as well that this finding does not necessarily lead to the opposite conclusion; namely that minimal-impact resilience to past stressors predicts subsequent resilience. One reason may be that many people often fail to recall prior PTEs unless they are experiencing great distress at the time of recall (LaLande & Bonanno, 2011). Thus, PTEs that do not result in PTSD may simply be forgotten. Importantly, there is even evidence that for some types of PTEs (e.g., disaster), prior experience with similar events may lead to better adjustment at subsequent exposures (see Bonanno et al., 2010). Presumably this type of matching prior experience fosters the ability to prepare for and understand the pending sequence of events.
Positive Emotions
The general benefits of positive emotions have received a great deal of attention in recent years. However, positive emotions appear to be especially salubrious in the context of acutely aversive contexts (Bonanno, 2004, 2005; Moskowitz, Folkman & Acree, 2003; Ong, Bergeman, & Chow, 2010). A recent prospective bereavement study showed, for example, that positive emotions may also mediate the physiological costs of grieving (Ong, Fuller-Rowell, Bonanno, & Almeidia, 2011). Compared to a matched group of married individuals, bereaved individuals in this study showed a flattened diurnal cortisol slope, suggesting a deregulation of the neuroendocrine system. The cortisol effects were robust and found to be statistically independent of a number of possible confounding factors, including age and socioeconomic status, personality, negative emotions, and health behaviors. Importantly, however, the cortisol deficits associated with bereavement were fully mediated by reductions in positive affect, thus suggesting a pathway between positive affect and a reduced physiological vulnerability to stress.
Several studies have documented links between positive emotion and adjustment to the 9/11 terrorist attacks. In an experimental study conducted just after the 9/11 attacks, New York college students were exposed to either a sadness induction or an amusement induction and then asked to talk for 5 minutes about their life since the terrorist disaster (Papa & Bonanno, 2008). The expression of genuine smiles during the monologue predicted better psychological adjustment two years later, but only for the students who were first made to feel sad, suggesting that genuine smiles are especially adaptive in the context of adversity (Bonanno & Keltner, 1997). Additionally, the effects of positive emotion on long-term adjustment were mediated by the students’ social network size and by greater reductions in negative emotion during the monologue, consistent with previous studies of the functional properties utility of positive emotion (Fredrickson, 2001; Keltner & Bonanno, 1997). A prospective study on remote reactions to the 9/11 attack among college students living in Michigan and thus geographically remote from New York, showed that the self-report of positive emotions mediated the relation between pre-event ego resilience, a trait-like personality characteristic, and post-9/11 depression and perceived growth (Fredrickson, Tugade, Waugh, & Larkin, 2003). Finally, the study mentioned earlier that associated trait self-enhancement uniquely with a minimal-impact resilience trajectory among high exposure survivors of the 9/11 attacks, also reported that trait self-enhancers were more likely to have experienced positive affect when they talked about the attack (Bonanno et al., 2005).
While there is compelling evidence in the adult literature for the adaptive benefits of positive emotion in response to PTEs, there remains a dearth of empirical work examining the salutary effects of positive emotion in children following PTEs. There is good reason to anticipate however that such evidence would be observed (Curtis & Cicchetti, 2007). Research on chronic adversity has demonstrated for example that high-risk children identified as resilient had “easy” temperaments and were able to actively recruit positive attention from adult caregivers (Werner & Smith, 1982). Moreover positive emotion has consistently been identified as a critical component of adaptation throughout development as well as in the specific context of chronic maltreatment (Werner & Smith, 1982; Cicchetti & Rogosch, 2009; Cicchetti, Rogosch, Lynch & Holt, 1993).
Coping and Appraisal
The ways that people interpret or “appraise” a stressful event is widely assumed to influence both the impact and the longer-term consequences of that event (Lazarus & Folkman, 1984). Appraisals of particular relevance to PTEs involve assessments of the potential for harm or “threat” versus the potential for growth, gain, and mastery or “challenge” (Ferguson, Mathews, & Cox, 1999). For example, in a longitudinal study of spinal cord injury (SCI) patients, appraisals of threat soon after the injury predicted higher levels of anxiety over time whereas appraisals of challenge predicted lower levels of depression over time (Kennedy, Lude, Efström, & Smithson, 2010). A recent trajectory study that examined anxiety and depression symptoms in SCI patients extending these findings to specific longitudinal patterns (Bonanno et al., in press). Specifically, patients showing a minimal-impact resilient trajectory were less likely to have made threat appraisals and more likely to have made challenge appraisals after the injury compared to other patterns.
Complimentary to the role of stress appraisal are specific strategies for coping (Lazarus & Folkman, 1984). Like appraisal, coping strategies have also consistently emerged as robust predictors of long-term outcome following PTEs (e.g., Nezu & Carnevale, 1987), including such aversive events as SCI (Buckelew et al., 1990; Frank, et al., 1987; Elfström, Kennedy, Lude, & Taylor, 2007; Kennedy, Lude, Elfström, & Smithson, 2011; Kennedy, Marsh et al., 2000). In the SCI trajectory study mentioned above, the minimal-impact resilience trajectory was uniquely associated with greater coping through SCL acceptance and SCL fighting spirit and less coping through SCL social reliance or behavioral disengagement (Bonanno, Kennedy et al., in press).
Flexibility
Historically, both the scholarly and popular literatures have emphasized the importance of direct and effortful processing of PTEs. More specifically, trauma theorists have championed the importance of reviewing, expressing and disclosing the thoughts, feelings, and memories associated with PTEs (e.g., Horowitz, 1986; Pennebaker, 1993). Yet, a considerable body of research has also highlighted the salutary value of seemingly opposite behaviors and processes that that appear to minimize the impact of PTEs, such as optimism (Scheier, Carver, & Bridges, 1994), self-serving cognitive biases (Taylor & Brown, 1988), and emotional avoidance (Bonanno, Keltner, Holen, & Horowitz, 1995). More recently, a third perspective has begun to emerge that integrates these ostensibly disparate processes around the construct of flexibility (Bonanno 2005; Cheng, 2001; Kashdan & Rottenberg, 2010). The core idea to this view is that PTEs vary greatly in both their characteristics and in the behaviors or strategies that might best help people survive them. Psychological flexibility means that people exposed to PTEs might utilize any number of behaviors and strategies and also that the optimal strategies within the same event may change over time. A somewhat similar concept has also been proposed in regard to coping with bereavement (Stroebe & Schut, 1999). Although research on self-regulatory flexibility in the context of extreme adversity is nascent, we review the literature on two promising areas: coping flexibility and emotional expressive flexibility.
Coping flexibility
Although the original intent of coping research was to empirically determine the strategies that were most and least effective in in promoting adaptation to stress uniquely by situation (e.g., Lazarus & Folkman, 1984), over time it became common practice to label certain types of coping a priori as inherently adaptive or as inherently maladaptive (e.g., Rippetoe & Rogers, 1987). This trend is countered however by the empirical reality that the same coping strategy might prove adaptive in one context and maladaptive in another, and by the fact that the use of coping strategies shows little consistency across situations (Compas, Forsythe, & Wagner, 1988). In response to these findings, coping theorists have increasingly emphasized that the success of coping efforts depends not so much on whether a person uses so-called adaptive or maladaptive coping behaviors, but rather on that person’s ability to utilize coping strategies flexibly and in a manner that best corresponds to the demands of the stressor situation (Aspinwell & Taylor, 1997; Block, 1993; Lazarus & Folkman, 1984).
Cheng (2001) was among the first researchers to develop a general methodology to capture flexibility in coping. Extending this research, our research team recently created a simple questionnaire measure to capture flexibility in the specific context of coping with potentially traumatic life events. The Perceived Ability to Cope with Trauma (PACT, Bonanno, Pat-Horenczk, & Noll, 2011) measures two broad sets of coping strategies captured in two brief self-report scales, the trauma focus scale and the forward focus scale. The trauma focus scale includes items that describe the temporary cessation of normal activities in favor of concerted trauma focus on the PTE, such as “Pay attention to the distressing feelings that result from the event”, “Reflect upon the meaning of the event”, “Reduce my normal social obligations”, and “Face the grim reality head on.” The forward focus scale includes items that describe an optimistic focus on maintaining normal goals and plans and using distracting activities, such as “Stay focused on my current goals and plans”, “Remind myself that things will get better”, “Find activities to help me keep the event off my mind”, “Enjoy something that I would normally find funny or amusing”, and “try to lessen the experience of painful emotions.” To assess coping flexibility, the trauma focus and forward focus scales can be assessed simultaneously as well as combined using a simple algorithm to create a single flexibility score.
Initial research with the PACT found that both the forward focus and trauma focus scales were associated with reduced symptoms of post-traumatic stress among Israeli college students exposed to terrorist violence (Bonanno et al., 2011). Moreover, participants low in overall coping flexibility showed marked increases in posttraumatic stress at high levels of trauma exposure whereas participants high in coping flexibility showed relatively little change in posttraumatic stress at higher levels of exposure. In other words, flexible copers showed a flat pattern of low symptoms across levels of exposure suggestive of minimal-impact resilience. Subsequent studies have shown a more divergent pattern, consistent with the concept that different dimensions of coping will be more or less adaptive across different types of stressors, (Burton et al., 2012). In a recent study of PTEs among college students (Galatzer-Levy et al., 2012), for example, the minimal-impact resilient trajectory was associated with greater use of forward focused coping but with less use of trauma focused coping.
Expressive flexibility
Emotional expression has long been viewed as an essential component of adaptive emotion regulation, while emotional suppression has been generally viewed as maladaptive (Gross, 1999). By the same token, however, emotion theorists have also noted the importance of both up-regulating and down-regulating emotion (Bonanno, 2001; Consedine, Magai, & Bonanno, 2002; Gupta & Bonanno, 2011, Gross, 1999). To test this idea, Bonanno et al. (2004) developed a within-subjects experimental paradigm to measure expressive flexibility, defined as the ability to either enhance or suppress emotional expression in accord with situational demands. Using a sample of New York City college students who had begun their studies just days before the 9/11 attacks, they found that students who were able to enhance and suppress emotional expression when asked to do so experienced less distress two years after the attack, net of initial levels of distress. A longer follow-up study on this same sample also linked expressive flexibility more explicitly with a resilient trajectory of stable low distress (Burton, Galatzer-Levy, & Bonanno, 2012). In another follow-up study, expressive flexibility was associated with positive health and well-being, obtained from confidential ratings provide by participants’ close friends (Westphal, Seivert, & Bonanno, 2010). Importantly, expressive flexibility in this study interacted with the frequency of acute life stressors. Acute life stress was associated with poorer adjustment but only for participants low in expressive flexibility. In other words, participants high in expressive flexibility showed little change in positive adjustment across levels of acute life stress, a pattern suggestive of minimal-impact resilience.
The adaptive benefits of expressive flexibility have to our knowledge not been studied in youth or child samples. However, there is reason to believe similar relations would emerge in these populations. Emotion regulation more broadly defined has been identified as an important resilience factor among children faced with adversity. In an analysis of Columbian child soldiers, for example, affect regulation was identified as one of six key themes that facilitated the ability of these youths to overcome the trauma of war (Cortes & Buchanan, 2007). Children who are engaging to others fare better following chronic adversity (Masten, Best, & Garmezy, 1990). It cannot be said that someone who is resilient never experiences negative affect, but the ability to modulate between negative and positive affective states, which can be described as a form of emotional flexibility, appears to be key mechanisms for resilience in children (Davidson, 2000).
Implications and Conclusion
The construct of psychological resilience can mean many things. In this article we focused on resilience in the specific context of isolated and potentially traumatic life events, or PTEs and distinguished this form of resilience from resilience in the context of chronic adversity. To illustrate these differences, we briefly reviewed the history of the resilience construct as it migrated from the child to adult literatures, and described some of the conceptual developments and misunderstandings that have arisen during the course of that migration. In the hopes of bringing a measure of clarity to this literature, we introduced the terms minimal-impact resilience and emergent resilience to represent specific trajectories of positive adjustment following isolated events and chronically aversive circumstances, respectively. Because emergent resilience has been well studied in the developmental literature, we devoted considerable space to reviewing the relatively new and growing body of evidence for the minimal-impact resilience trajectory in adult and to a lesser extent child samples and considered the available evidence for predictors of that trajectory.
It is important to emphasize that research on minimal-impact resilience is nascent. Although developmental researchers have examined emergent resilience in at-risk populations for decades, the study of minimal-impact resilience in the face of isolated PTEs has gained currency only relatively recently. It is our hope that research in this area will continue to blossom, and that some of the most salient conceptual implications this research suggests might be addressed. We close by briefly considering implications relevant to policy and media, resilience building, and neuroscience.
At a policy and media level, it is fair to say that relatively little of this new research has yet been integrated. The dominant paradigm for PTEs in the western media appears to swing between extreme viewpoints that either dramatize the psychological costs of PTEs, as in headlines like “Trauma of Iraq war haunting thousands returning home” (Welch, 2005, USA Today), or almost naively minimize the costs of trauma, as in headlines like “Trauma can be good for you” (Joseph, 2012, Daily Mail). This kind of conceptual bipolarity only leads to confusion at a policy level. In the aftermath of the 911 terrorist attacks, for example, an editorial in the news magazine of the American Psychiatric Association, the Psychiatric News, pondered whether the “post-9/11 resilience data” should be read as “good or troubling news?” (Arehart-Treichel, 2005). Such a position is predicated on the mistaken assumption that greater attention to psychological resilience obviates or at least minimizes the policy concerns for the care of those suffering form trauma-related psychopathology.
The research we reviewed suggests a broader perspective that potentially might help bring extreme viewpoints into perspective. PTEs can and most certainly do cause psychological harm. Indeed, the very same trajectory models that demonstrate minimal-impact resilience also consistently identify trajectories of chronic dysfunction and recovery. That these seemingly disparate pathways always co-occur is an empirical fact. Rather than focusing exclusively on one or another outcome, policy and media sources may be better served by grappling with the questions of how these divergent patterns come about (Masten, 2011)
A related issue pertains to the growing interest in programs that might build resilience en mass through large-scale prophylactic interventions. In recent years, a number of prophylactic interventions of this type have been attempted in response to important social problems such as eating disorders, suicide, and military preparedness. On the whole, the data for the effectiveness of such programs is far from impressive and, in fact, some findings suggest that prophylactic interventions may do more harm than good (for a more detailed discussion of these issues, see Bonanno, Westphal, and Mancini (2011) and McNally (2012)). We would argue that one reason for this putative failure is that not enough is yet known about minimal-impact resilience, or the factors that promote it. What we do know suggests, however, that no single factor or process will account for much of the variance in outcomes, and therefore that resilience building enterprises are not likely to produce much of an effect unless they focus on a wide-range of factors. Unfortunately, some of the factors that have been empirical associated with minimal-impact resilience, such as economic and social resources, are not readily amenable to short-term change. Further consideration of these findings and great attention to the basic research findings would no doubt enhance such efforts.
Finally, there is the compelling question of the neuroscience of resilience (Feder et al., 2009; Ryff & Singer, 2002; Ryff, Singer & Dienberg-Love, 2004). Advances in the understanding of brain structure and function, neuroendocrine response, and genetics have all ballooned over the past decade. The picture of how these processes interact during the stress response and they role they play in both health and dysfunction is increasingly coming in to focus (Conrad, 2011; Chrousos, 2009). For example, the specific mechanisms that appear to underlie PTSD and non-dysfunctional responses to PTEs are increasingly well-understood, both at the level of functional neuroscience (Liberzon & Sripada, 2007) and neuroendocrine responding (Yehuda & Ledoux, 2007). Particularly intriguing is the recent work by de Quervain and colleagues on the role of glutocorticoids in regulating memory for stressful events (de Quervain, 2006; de Quervain, Aemi, Schelling, & Roozendaal, 2009). Although still in progress, this work suggests the intriguing possibility that cortisol and other aspects of the HPA axis help to keep memories of a highly stressful event in check, allowing some memory consolidation of the event but at the same time limiting the extent that memories are elaborated through working memory and with material from long-term memory.
As promising as the neuroscience evidence may be, however, describing these advances in terms of resilience per se seems to us premature. To the best of our knowledge no published research has yet examined neuropsychological parameters specifically in relation to a minimal-impact trajectory or for that matter in relation to any types of longitudinal or prospective trajectories. Such findings would prove enormously important in illuminating the mechanisms that might underlie minimal-impact resilience. Perhaps even more importantly, research that relates neuroscience findings with trajectory research may help also help illuminate the conceptual limits of these constructs, and pave the way for new thinking and new research.
KEY POINTS.
Research on resilience to adversity has migrated from its origins in the study of chronic adversity in children to the study of isolated potentially traumatic events in adulthood.
To summarize this broad body of research, we propose the terms emergent resilience and minimal-impact resilience to represent resilience after chronic adversity and isolated potentially traumatic events, respectively, regardless of the population under study.
We consider limitations of traditional approaches to variability in outcome and review new research that uses Latent Growth Modeling to study resilient trajectories and their predictors.
This research suggests implications for understanding policy and media representations of aversive life events, the development of prophylactic interventions and resilience-building, and future research on the neuroscience of resilience.
DEFINITION OF KEY TERMS.
Emergent resilience: Positive adjustment measured in response to chronically stressful and aversive circumstances. Emergent resilience is typically observed only after the stressful circumstances have abated.
Minimal-impact resilience: Positive adjustment measured in response to isolated and acute stressor or potentially traumatic events (PTE). Minimal-impact resilience is measured as a relatively stable trajectory of continuous healthy adjustment following and (if known) prior to exposure to the stressor event.
Potentially traumatic event (PTE): Single-incident exposure to a violent, or life-threatening event that typically falls outside the painful but more common stressful experiences.
Recovery trajectory: Longitudinal trajectory in which normal functioning temporarily gives way to threshold or sub threshold distress and psychopathology (depressive symptoms, PTSD) for several months before gradually returning to pre-exposure levels.
Latent Growth Modeling: Suite of statistical procedures that relax the assumption of a single population and can potentially identify heterogeneous subpopulations comprising distinct response trajectories across time.
Trauma exposure: Degree of subject and objective exposure to a PTE
Trait self-enhancement: Dispositional tendency to perceive the world using self-serving biases
Coping self-efficacy: Dispositional tendency to believe in one’s ability to cope effectively with stress
Threat and challenge appraisals: Perception of aversive circumstances as a challenge that can be successfully overcome (challenge appraisal) or as a threat to that will most likely lead to negative consequences (threat appraisal).
Behavioral disengagement: A general form of coping aimed at reducing ones effort to engage with the stressor.
SCL acceptance, fighting spirit, and social reliance: Coping strategies/behaviors specific to spinal cord lesion. Acceptance is the ability to make the best of life despite the SCI, fighting spirit is illustrated by working to find ‘tricks’ to make life easier in relation to the injury, while social reliance is the adoption of beliefs that one is dependent on others because of injury.
-
Positive emotion: The experience or genuine expression of positive emotion.
Flexibility in coping and emotion regulation: The ability to utilize different forms of coping and emotion regulation as dictated by the demands of different circumstances rather than relying on the same coping or emotion regulation behaviors across situations.
FUTURE DIRECTIONS FOR RESEARCH ON MINIMAL IMPACT RESILIENCE IN CHILDREN.
It will be crucial to obtain data on children’s mental health and well-being following and if possible before isolated, potentially traumatic events. These data will make it possible to elucidate both the prevalence and the predictors of minimal impact resilience and to compare these findings with the growing body of evidence on minimal-impact resilience in adult populations.
A ‘multiple levels of analysis’ approach to investigating minimal-impact resilience in children is warranted with an emphasis on the processes of adaptation following a potentially traumatic event. In addition, researchers need to monitor children following a PTE across several domains of adjustment using an integrative, multidisciplinary approach.
Additional research is needed on important neuropsychological, biological and genetic processes that may mitigate or modify the impact of a PTE at different developmental stages.
Acknowledgments
This manuscript was made possible in part by grants from the National Institute of Mental Health (R01 MH091034) to George A. Bonanno.
Footnotes
Conflict of interest statement: No conflict of interest.
We report no conflict of interests in the development of this manuscript.
This review article was invited by the journal, for which the principal author has been offered a small honorarium payment towards personal expenses.
References
- Adams RE, Boscarino JA. Differences in mental health outcomes among Whites, African Americans, and Hispanics following a community disaster. Psychiatry. 2005;68(3):250–265. doi: 10.1521/psyc.2005.68.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahern J, Galea S, Resnick H, Vlahov D. Television images and probable posttraumatic stress disorder after September 11: the role of background characteristics, event exposures, and perievent panic. Journal of Nervous & Mental Disease. 2004;192(3):217–226. doi: 10.1097/01.nmd.0000116465.99830.ca. [DOI] [PubMed] [Google Scholar]
- Almedom AM, Glandon D. Journal of Loss & Trauma. 2. Vol. 12. Routledge; 2007. Resilience is not the Absence of PTSD any More than Health is the Absence of Disease; pp. 127–143. Retrieved from. [DOI] [Google Scholar]
- Andrews B, Brewin CR, Philpott R, Stewart L. Delayed-Onset Posttraumatic Stress Disorder: A Systematic Review of the Evidence. American Journal of Psychiatry. 2007;164(9):1319–1326. doi: 10.1176/appi.ajp.2007.06091491. [DOI] [PubMed] [Google Scholar]
- Arehart-Treichel J. Are post-9/11 resilience data good or troubling news? Psychiatric News. 2005;40:18. [Google Scholar]
- Aspinwall LG, Taylor SE. A stitch in time: Self-regulation and proactive coping. Psychological Bulletin. 1997;121(3):417–436. doi: 10.1037/0033-2909.121.3.417. [DOI] [PubMed] [Google Scholar]
- Betancourt Theresa S. Attending to the Mental Health of War-Affected Children: The Need for Longitudinal and Developmental Research Perspectives. Journal of the American Academy of Child and Adolescent Psychiatry. 2011 doi: 10.1016/j.jaac.2011.01.008. [DOI] [PubMed] [Google Scholar]
- Betancourt Theresa S, Agnew-Blais J, Gilman SE, Williams DR, Ellis BH. Past horrors, present struggles: The role of stigma in the association between war experiences and psychosocial adjustment among former child soldiers in Sierra Leone. Social Science & Medicine. 2010;70(1):17–26. doi: 10.1016/j.socscimed.2009.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt Theresa S, Simmons S, Borisova I, Brewer SE, Iweala U, de la Soudière M. High Hopes, Grim Reality: Reintegration and the Education of Former Child Soldiers in Sierra Leone. Comparative Education Review. 2008;52(4):565–587. doi: 10.1086/591298. CR -- Copyright © 2008 Comparative a. The University of Chicago Press on behalf of the Comparative and International Education Society. Retrieved from http://www.jstor.org/stable/10.1086/591298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt Theresa Stichick, Khan KT. International Review of Psychiatry. 3. Vol. 20. Informa Allied Health; 2008. The mental health of children affected by armed conflict: Protective processes and pathways to resilience; pp. 317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block J. Lives through time. Berkeley, CA: Bancroft Books; 1971. [Google Scholar]
- Block Jack. Studying personality the long way. In: Funder DC, Parke RD, Tomlinson-Keasey C, Widaman K, editors. Studying lives through time: Personality and development. Washington, DC, US: American Psychological Association; 1993. pp. 9–41. [DOI] [Google Scholar]
- Block Jack, Kremen AM. Journal of Personality and Social Psychology. 2. Vol. 70. American Psychological Association; US: 1996. IQ and ego-resiliency: Conceptual and empirical connections and separateness; pp. 349–361. [DOI] [PubMed] [Google Scholar]
- Block Jack, Robins RW. Child Development. 3. Vol. 64. Blackwell Publishing Ltd; 1993. A Longitudinal Study of Consistency and Change in Self-Esteem from Early Adolescence to Early Adulthood; pp. 909–923. Retrieved from http://dx.doi.org/10.1111/j.1467-8624.1993.tb02951.x. [DOI] [PubMed] [Google Scholar]
- Boelen PA, de Keijser J, van den Hout MA, van den Bout J. Treatment of Complicated Grief: A Comparison Between Cognitive-Behavioral Therapy and Supportive Counseling. Journal of Consulting and Clinical Psychology. 2007;75(2):277–284. doi: 10.1037/0022-006X.75.2.277. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. American Psychologist. 1. Vol. 59. US: American Psychological Assn; 2004. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? pp. 20–28. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. The Other Side of Sadness: What the new science of bereavement tells us about life after loss. New York: Basic Books; 2009. [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology. 2007 doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. The human capacity to thrive in the face of potential trauma. Pediatrics. 2008;121(2):369–375. doi: 10.1542/peds.2007–1648. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. Beyond resilience and PTSD: Mapping the heterogeneity of responses to potential trauma. Psychological Trauma: Theory, Research, Practice, and Policy 2008 [Google Scholar]
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. Psychological Science. 7. Vol. 15. United Kingdom: Blackwell Publishing; 2004. The importance of being flexible: The ability to both enhance and suppress emotional expression predicts long-term adjustment; pp. 482–487. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Pat-Horenczyk R, Noll J. Coping Flexibility and Trauma: The Perceived Ability to Cope With Trauma (PACT) Scale. Psychological Trauma-Theory Research Practice and Policy. 2011;3(2):117–129. doi: 10.1037/a0020921. [DOI] [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to Loss and Potential Trauma. Annual Review of Clinical Psychology. 2011 doi: 10.1146/annurev-clinpsy-032210–104526. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Wortman CB, Lehman DR, Tweed RG, Haring M, Sonnega J, Carr D, et al. Resilience to loss and chronic grief: A prospective study from preloss to 18-months postloss. Journal of Personality & Social Psychology. 2002;83(5):1150–1164. doi: 10.1037//0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- Bonanno George A. Emotion self-regulation. [References] In: Mayne TJ, Bonanno GA, editors. Emotions: Currrent issues and future directions. Emotions and social behavior. New York, NY: Guilford Press; 2001. pp. 251–285. [Google Scholar]
- Bonanno George A. Current Directions in Psychological Science. 3. Vol. 14. United Kingdom: Blackwell Publishing; 2005. Resilience in the face of loss and potential trauma; pp. 135–138. [Google Scholar]
- Bonanno George A. Uses and abuses of the resilience construct: Loss, trauma, and health-related adversities. Social Science & Medicine. 2012;74(5):753–756. doi: 10.1016/j.socscimed.2011.11.022. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Brewin CR, Kaniasty K, Greca AML. Weighing the Costs of Disaster. Psychological Science in the Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. Retrieved from http://psi.sagepub.com/content/11/1/1.short. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Field NP. American Behavioral Scientist. 5. Vol. 44. US: Sage Publications; 2001. Examining the delayed grief hypothesis across 5 years of bereavement; pp. 798–816. [Google Scholar]
- Bonanno George A, Galea S, Bucciarelli A, Vlahov D. Psychological Science. 3. Vol. 17. United Kingdom: Blackwell Publishing; 2006. Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack; pp. 181–186. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Ho SAYMY, Chan JCK, Kwong RSY, Cheung CKY, Wong CPY, Wong VCW. Health Psychology. 5. Vol. 27. American Psychological Association; US: 2008. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach; pp. 659–667. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Kaltman S. Psychological Bulletin. 6. Vol. 125. US: American Psychological Assn; 1999. Toward an integrative perspective on bereavement; pp. 760–776. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. Journal of Abnormal Psychology. 1997;106(1):126–137. doi: 10.1037//0021-843x.106.1.126. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Keltner D, Holen A, Horowitz MJ. When avoiding unpleasant emotions might not be such a bad thing: Verbal^autonomic response dissociation and midlife conjugal bereavement. Journal of Personality & Social Psychology. 1995;69(5):975–989. doi: 10.1037//0022-3514.69.5.975. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Mancini AD, Horton JL, Powell TM, LeardMann CA, Boyko EJ, Wells TS, et al. Trajectories of trauma symptoms and resilience in deployed US military service members: prospective cohort study. The British Journal of Psychiatry. 2012;200(4):317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Moskowitz JT, Papa A, Folkman S. Journal of Personality and Social Psychology. 5. Vol. 88. US: American Psychological Assn; 2005. Resilience to Loss in Bereaved Spouses, Bereaved Parents, and Bereaved Gay Men; pp. 827–843. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Rennicke C, Dekel S. Journal of Personality and Social Psychology. 6. Vol. 88. US: American Psychological Assn; 2005. Self-Enhancement Among High-Exposure Survivors of the September 11th Terrorist Attack: Resilience or Social Maladjustment? pp. 984–998. [DOI] [PubMed] [Google Scholar]
- Bonanno George A, Kennedy Paul, Galatzer-Levy Isaac, Lude Peter, Elfström ML. Trajectories of Resilience, Depression, and Anxiety Following Spinal Cord Injury. Rehabilitation Psychology. Rehabilitation Psychology. n.d doi: 10.1037/a0029256. [DOI] [PubMed] [Google Scholar]
- Breslau N. Outcomes of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62(Suppl 1):55–59. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11495098. [PubMed] [Google Scholar]
- Breslau Naomi, Peterson EL, Schultz LR. Archives of General Psychiatry. 4. Vol. 65. US: American Medical Assn; 2008. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiological study; pp. 431–437. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Journal of Consulting and Clinical Psychology. 5. Vol. 68. US: American Psychological Assn; 2000. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults; pp. 748–766. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG. Australian and New Zealand Journal of Psychiatry. 2. Vol. 36. United Kingdom: Blackwell Publishing; 2002. Delayed-onset posttraumatic stress disorder: A prospective evaluation; pp. 205–209. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Buckelew SP, Shutty MS, Jr, Hewett J, Landon T, Morrow K, Frank RG. Health locus of control, gender differences and adjustment to persistent pain. Pain. 1990;42(3):287–294. doi: 10.1016/0304-3959(90)91141-5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2250920. [DOI] [PubMed] [Google Scholar]
- Buckley TC, Blanchard EB, Hickling EJ. Journal of Abnormal Psychology. 4. Vol. 105. US: American Psychological Assn; 1996. A prospective examination of delayed onset PTSD secondary to motor vehicle accidents; pp. 617–625. [DOI] [PubMed] [Google Scholar]
- Burton CL, Yan OH, Pat-Horenczyk R, Chan ISF, Ho S, Bonanno GA. Coping flexibility and complicated grief: A comparison of American and Chinese samples. Depression and Anxiety. 2012;29(1):16–22. doi: 10.1002/da.20888. Retrieved from http://dx.doi.org/10.1002/da.20888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton CL, Galatzer-Levy I, Bonanno GA. Unpublished manuscript. 2012. Expressive flexibility and long-term adjustment: A prospective study. [Google Scholar]
- Carr VJ, Lewin TJ, Webster RA, Kenardy JA, Hazell PL, Carter GL. Psychosocial sequelae of the 1989 Newcastle earthquake: II. Exposure and morbidity profiles during the first 2 years post-disaster. Psychological Medicine. 1997;27(1):167–178. doi: 10.1017/s0033291796004278. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9122297. [DOI] [PubMed] [Google Scholar]
- Charles ST, Carstensen LL. Social and emotional aging. Annual Review of Psychology. 2010;61:383–409. doi: 10.1146/annurev.psych.093008.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase-Lansdale PL, Mott FL, Brooks-Gunn J, Phillips DA. Developmental Psychology. 6. Vol. 27. US: American Psychological Association; 1991. Children of the National Longitudinal Survey of Youth: A unique research opportunity; pp. 918–931. [DOI] [Google Scholar]
- Chen S-H, Wu Y-C. Natural Hazards. 1. Vol. 37. Springer; Netherlands: 2006. Changes of PTSD Symptoms and School Reconstruction: A Two-year Prospective Study of Children and Adolescents after the Taiwan 921 Earthquake; pp. 225–244. [DOI] [Google Scholar]
- Cheng C. Assessing coping flexibility in real-life and laboratory settings: a multimethod approach. Journal of Personality and Social Psychology. 2001;80(5):814–833. doi: 10.1037//0022-3514.80.5.814. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11374752. [DOI] [PubMed] [Google Scholar]
- Chrousos GP. Nat Rev Endocrinol. 7. Vol. 5. Nature Publishing Group; 2009. Stress and disorders of the stress system; pp. 374–381. Retrieved from http://dx.doi.org/10.1038/nrendo.2009.106. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Curtis WJ. Development and Psychopathology. 03. Vol. 19. Cambridge Journals Online; 2007. Multilevel perspectives on pathways to resilient functioning; pp. 627–629. Retrieved from href=“ http://dx.doi.org/10.1017/S0954579407000314. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. New Directions for Child and Adolescent Development. 124. Vol. 2009. Wiley Subscription Services, Inc., A Wiley Company; 2009. Adaptive coping under conditions of extreme stress: Multilevel influences on the determinants of resilience in maltreated children; pp. 47–59. Retrieved from http://dx.doi.org/10.1002/cd.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coifman KG, Bonanno GA. When Distress Does Not Become Depression: Emotion Context Sensitivity and Adjustment to Bereavement. Journal of Abnormal Psychology. 2010;119(3):479–490. doi: 10.1037/a0020113. [DOI] [PubMed] [Google Scholar]
- Compas BE, Forsythe CJ, Wagner BM. Cognitive Therapy and Research. 3. Vol. 12. Springer; Netherlands: 1988. Consistency and variability in causal attributions and coping with stress; pp. 305–320. [DOI] [Google Scholar]
- Connor KM, Davidson RT, Kathryn MC, Jonathan RTD, Davidson JRT. Depression and Anxiety. 2. Vol. 18. Wiley Subscription Services, Inc., A Wiley Company; 2003. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) pp. 76–82. [DOI] [PubMed] [Google Scholar]
- Conrad CD. In: Handbook of stress: Neuropsychological effects on the brain. Conrad CD, editor. West Sussex, United kingdom: Wiley-Blackwell Publishing Ltd; 2011. [Google Scholar]
- Consedine NS, Magai C, Bonanno GA. Review of General Psychology. 2. Vol. 6. US: Educational Publishing Foundation; 2002. Moderators of the emotion inhibition-health relationship: A review and research agenda; pp. 204–228. [Google Scholar]
- Cook JM, Elmore DL. Disaster mental health in older adults: Symptoms, policy, and planning. In: Neria F, Yuval, Galea, Sandro, Norris, editors. Mental Health and Disasters. New York: Cambridge University Press; 2009. pp. 233–263. [Google Scholar]
- Cortes L, Buchanan M. International Journal for the Advancement of Counselling. 1. Vol. 29. Springer; Netherlands: 2007. The Experience of Columbian Child Soldiers from a Resilience Perspective; pp. 43–55. [DOI] [Google Scholar]
- Curran PJ, Hussong AM. Journal of Abnormal Psychology. 4. Vol. 112. American Psychological Association; US: 2003. The use of latent trajectory models in psychopathology research; pp. 526–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currier JM, Neimeyer RA, Berman JS. Psychological Bulletin. 5. Vol. 134. American Psychological Association; US: 2008. The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review; pp. 648–661. [DOI] [PubMed] [Google Scholar]
- de Kloet ER, Derijk RH, Meijer OC. The Handbook of Stress. Wiley-Blackwell; 2011. Corticosteroid Receptor Involvement in the Stress Response; pp. 47–75. Retrieved from http://dx.doi.org/10.1002/9781118083222.ch3. [Google Scholar]
- de Quervain DJ-F, Aerni A, Schelling G, Roozendaal B. Glucocorticoids and the regulation of memory in health and disease. Frontiers in Neuroendocrinology. 2009;30(3):358–370. doi: 10.1016/j.yfrne.2009.03.002. Retrieved from http://www.sciencedirect.com/science/article/pii/S009130220900003X. [DOI] [PubMed] [Google Scholar]
- de Quervain DJ-F. Annals of the New York Academy of Sciences. 1. Vol. 1071. Blackwell Publishing Inc; 2006. Glucocorticoid-Induced Inhibition of Memory Retrieval; pp. 216–220. Retrieved from http://dx.doi.org/10.1196/annals.1364.016. [DOI] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabil Psychol. 2010;55(1):1–11. doi: 10.1037/a0018601. 2010-03250-001 [pii] [DOI] [PubMed] [Google Scholar]
- Deshields T, Tibbs T, Fan MY, Taylor M. Differences in patterns of depression after treatment for breast cancer. Psychooncology. 2006;15(5):398–406. doi: 10.1002/pon.962. [DOI] [PubMed] [Google Scholar]
- DiRago A, Vaillant G. Journal of Youth and Adolescence. 1. Vol. 36. Springer; Netherlands: 2007. Resilience in Inner City Youth: Childhood Predictors of Occupational Status Across the Lifespan; pp. 61–70. [DOI] [Google Scholar]
- Dickstein BD, Suvak M, Litz BT, Adler AB. Journal of Traumatic Stress. 3. Vol. 23. US: John Wiley & Sons; 2010. Heterogeneity in the course of posttraumatic stress disorder: Trajectories of symptomatology; pp. 331–339. Retrieved from http://rlib.pace.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2010-13183-004&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall RD. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling: concepts, issues, and applications. Quantitative methodology series. 2. Mahwah, N.J: Lawrence Erlbaum Associates; 2006. p. xii.p. 261. Retrieved from http://www.loc.gov/catdir/toc/ecip063/2005033734.html. [Google Scholar]
- Elder GH. The life course as developmental theory. Child Development. 1998;69(1):1–12. doi: 10.1111/j.1467-8624.1998.tb06128.x. [DOI] [PubMed] [Google Scholar]
- Elfstrom ML, Kennedy P, Lude P, Taylor N. Condition-related coping strategies in persons with spinal cord lesion: a cross-national validation of the Spinal Cord Lesion-related Coping Strategies Questionnaire in four community samples. Spinal Cord. 2007;45(6):420–428. doi: 10.1038/sj.sc.3102003. [DOI] [PubMed] [Google Scholar]
- Feder A, Nestler EJ, Charney DS. Nat Rev Neurosci. 6. Vol. 10. Nature Publishing Group; 2009. Psychobiology and molecular genetics of resilience; pp. 446–457. Retrieved from http://dx.doi.org/10.1038/nrn2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman BJ, Masyn KE, Conger RD. Developmental Psychology. 3. Vol. 45. US: American Psychological Association; 2009. New approaches to studying problem behaviors: A comparison of methods for modeling longitudinal, categorical adolescent drinking data; pp. 652–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank RG, Umlauf RL, Wonderlich SA, Askanazi GS, Buckelew SP, Elliott TR. Differences in coping styles among persons with spinal cord injury: a cluster-analytic approach. Journal of Consulting and Clinical Psychology. 1987;55(5):727–731. doi: 10.1037//0022-006x.55.5.727. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3454783. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. Journal of Personality and Social Psychology. 2. Vol. 84. US: American Psychological Assn; 2003. What good are positive emotions in crisis? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001; pp. 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. International Journal of Methods in Psychiatric Research. 2. Vol. 12. John Wiley & Sons, Ltd; 2003. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? pp. 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Mazursky H, Mancini AD, Bonanno GA. What We Don’t Expect When Expecting: Evidence for Heterogeneity in Subjective Well-Being in Response to Parenthood. Journal of Family Psychology. 2011;25(3):384–392. doi: 10.1037/a0023759. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy Isaac R, Bonanno GA. Beyond normality in the study of bereavement: Heterogeneity in depression outcomes following loss in older adults. Social Science & Medicine. 2012;74(12):1987–1994. doi: 10.1016/j.socscimed.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy Isaac R, Bonanno GA, Mancini AD. Journal of Neuroscience, Psychology, and Economics. 2. Vol. 3. US: Educational Publishing Foundation; 2010. From marianthal to latent growth mixture modeling: A return to the exploration of individual differences in response to unemployment; pp. 116–125. [DOI] [Google Scholar]
- Galatzer-Levy Isaac R, Burton CL, Bonanno GA. Journal of Social & Clinical Psychology. 6. Vol. 31. Guilford Publications Inc; 2012. Coping Flexibility, Potentially Traumatic Life Events, and Resilience: A Prospective Study of College Student Adjustment; pp. 542–567. [DOI] [Google Scholar]
- Garbarino J, Ganzel B. The human ecology of early risk. In: Shonkoff SJ, Meisels JP, editors. Handbook of early childhood intervention. 2. New York, NY: Cambridge University Press; 2000. pp. 76–94. [Google Scholar]
- Garmezy N. American journal of orthopsychiatry. Vol. 42. American Psychological Association; 1972. Invulnerable children: The fact and fiction of competence and disadvantage; p. 328. [Google Scholar]
- Garmezy N. Children in poverty: resilience despite risk. Psychiatry. 1993;56:127–136. doi: 10.1080/00332747.1993.11024627. [DOI] [PubMed] [Google Scholar]
- Garmezy Norman. Resilience and vulnerability to adverse developmental outcomes associated with poverty. American Behavioral Scientist. 1991;34(4):416–430. [Google Scholar]
- Garrison CZ, Weinrich MW, Hardin SB, Weinrich S, Wang L. Post-traumatic stress disorder in adolescents after a hurricane. American Journal of Epidemiology. 1993;138(7):522–530. doi: 10.1093/oxfordjournals.aje.a116886. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8213756. [DOI] [PubMed] [Google Scholar]
- Ginexi EM, Weihs K, Simmens SJ, Hoyt DR. Natural disaster and depression: a prospective investigation of reactions to the 1993 midwest floods. American Journal of Community Psychology. 2000;28(4):495–518. doi: 10.1023/a:1005188515149. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10965388. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, Alvarez ML, Goenjian HA, Pynoos RS. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after hurricane Mitch. The American Journal of Psychiatry. 2001;158(5):788–794. doi: 10.1176/appi.ajp.158.5.788. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11329403. [DOI] [PubMed] [Google Scholar]
- Gralinski-Bakker JH, Hauser ST, Stott C, Billings RL, Allen JP. Research in Human Development. 4. Vol. 1. Psychology Press; 2004. Markers of Resilience and Risk: Adult Lives in a Vulnerable Population; pp. 291–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: Past, present, future. Cognition & Emotion. 1999;13(5):551–573. [Google Scholar]
- Gupta S, Bonanno GA. Complicated Grief and Deficits in Emotional Expressive Flexibility. Journal of Abnormal Psychology. 2011;120(3):635–643. doi: 10.1037/a0023541. [DOI] [PubMed] [Google Scholar]
- Gupta S, Bonanno GA, Noll JG, Putnam FW, Keltner D, Trickett PK. Anger Expression and Adaptation to Childhood Sexual Abuse: The Role of Disclosure. Psychological Trauma-Theory Research Practice and Policy. 2011;3(2):171–180. doi: 10.1037/a0022044. [DOI] [Google Scholar]
- Hobfoll SE, Mancini AD, Hall BJ, Canetti D, Bonanno GA. The limits of resilience: Distress following chronic political violence among Palestinians. Social Science & Medicine. 2011;72(8):1400–1408. doi: 10.1016/j.socscimed.2011.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll Stevan E. American Psychologist. 3. Vol. 44. American Psychological Association; US: 1989. Conservation of resources: A new attempt at conceptualizing stress; pp. 513–524. [DOI] [PubMed] [Google Scholar]
- Hobfoll Stevan E. Review of General Psychology. 4. Vol. 6. US: Educational Publishing Foundation; 2002. Social and psychological resources and adaptation; pp. 307–324. [Google Scholar]
- Holland J, Neimeyer R, Boelen P, Prigerson H. Journal of Psychopathology and Behavioral Assessment. 3. Vol. 31. Springer; Netherlands: 2009. The Underlying Structure of Grief: A Taxometric Investigation of Prolonged and Normal Reactions to Loss; pp. 190–201. [DOI] [Google Scholar]
- Hoven CW, Duarte CS, Lucas CP, Wu P, Mandell DJ, Goodwin RD, Cohen M, et al. Psychopathology among New York city public school children 6 months after September 11. Archives of General Psychiatry. 2005;62(5):545–552. doi: 10.1001/archpsyc.62.5.545. [DOI] [PubMed] [Google Scholar]
- Hoven Christina W, Wasserman D, Wasserman C, Mandell DJ. Awareness in nine countries: A public health approach to suicide prevention. Legal Medicine. 2009;11(Supple 0):S13–S17. doi: 10.1016/j.legalmed.2009.01.106. Retrieved from http://www.sciencedirect.com/science/article/pii/S1344622309001266. [DOI] [PubMed] [Google Scholar]
- Huerta F, Horton R. The Gerontologist. 6. Vol. 18. US: Gerontological Society of America; 1978. Coping behavior of elderly flood victims; pp. 541–546. Retrieved from http://rlib.pace.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1980-25663-001&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Joseph S. The Daily Mail. London, England: 2012. Jan, Trauma can be GOOD for you, says psychologist who helped survivors of the Zeebrugge disaster; p. 1. [Google Scholar]
- Kagan J. Journal of Youth and Adolescence. 2. Vol. 5. Springer; Netherlands: 1976. New views on cognitive development; pp. 113–129. Retrieved from http://dx.doi.org/10.1007/BF01537487. [DOI] [PubMed] [Google Scholar]
- Kagan J, Klein RE. American Psychologist. 11. Vol. 28. US: American Psychological Association; 1973. Cross-cultural perspectives on early development; pp. 947–961. [DOI] [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato H, Asukai N, Miyake Y, Minakawa K, Nishiyama A. Acta Psychiatrica Scandinavica. 6. Vol. 93. Blackwell Publishing Ltd; 1996. Post-traumatic symptoms among younger and elderly evacuees in the early stages following the 1995 Hanshin-Awaji earthquake in Japan; pp. 477–481. [DOI] [PubMed] [Google Scholar]
- Keltner D, Bonanno GA. A study of laughter and dissociation: Distinct correlates of laughter and smiling during bereavement. Journal of Personality & Social Psychology. 1997;73(4):687–702. doi: 10.1037//0022-3514.73.4.687. [DOI] [PubMed] [Google Scholar]
- Kennedy P, Lude P, Elfstrom ML, Smithson EF. Psychological contributions to functional independence: a longitudinal investigation of spinal cord injury rehabilitation. Archives of Physical Medicine and Rehabilitation. 2011;92(4):597–602. doi: 10.1016/j.apmr.2010.11.016. [DOI] [PubMed] [Google Scholar]
- Kennedy Paul, Marsh N, Lowe R, Grey N, Short E, Rogers B. British Journal of Health Psychology. 2. Vol. 5. Blackwell Publishing Ltd; 2000. A longitudinal analysis of psychological impact and coping strategies following spinal cord injury; pp. 157–172. Retrieved from http://dx.doi.org/10.1348/135910700168838. [Google Scholar]
- Kimerling R, Mack KP, Alvarez J. Women and diasasters. In: Neria FHY, Galea S, Norris, editors. Mental health and disasters. New York: Cambridge University Press; 2009. pp. 203–217. [Google Scholar]
- King DW, King LA, Foy DW, Keane TM, Fairbank JA. Journal of Abnormal Psychology. 1. Vol. 108. US: American Psychological Association; 1999. Posttraumatic stress disorder in a national sample of female and male Vietnam veterans: Risk factors, war-zone stressors, and resilience-recovery variables; pp. 164–170. [DOI] [PubMed] [Google Scholar]
- Knight BG, Gatz M, Heller K, Bengtson VL. Psychology and Aging. 4. Vol. 15. US: American Psychological Association; 2000. Age and emotional response to the Northridge earthquake: A longitudinal analysis; pp. 627–634. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lai B, Jaccard J. Journal of Consulting and Clinical Psychology;Journal of Consulting and Clinical Psychology. 6. Vol. 78. US: American Psychological Association; 2010. Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children’s persistent posttraumatic stress symptoms; pp. 794–805. [DOI] [PubMed] [Google Scholar]
- LaGreca AM, Vernberg E, Roberts M. In: Helping children cope with disasters and terrorism. LaGreca MA, Silverman W, Vernberg E, Roberts, editors. Washington, D.C: American Psychological Assn; 2002. [Google Scholar]
- Lam WWT, Bonanno GA, Mancini AD, Ho S, Chan M, Hung WK, Or A, et al. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psycho-oncology. 2010;19(10):1044–1051. doi: 10.1002/pon.1658. [DOI] [PubMed] [Google Scholar]
- Laufer A, Solomon Z. Journal of Social and Clinical Psychology. 4. Vol. 25. Guilford Publications Inc; 2006. Posttraumatic Symptoms and Posttraumatic Growth Among Israeli Youth Exposed to Terror Incidents; pp. 429–447. [DOI] [Google Scholar]
- Layne CM, Warren JS, Watson PJ, Shalev AY. Risk, vulnerability, resistance, and resilience: Toward an integrative conceptualization of posttraumatic adapation. In: Friedman PARMJ, Keane TM, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 497–520. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Le Brocque RM, Hendrikz J, Kenardy JA. The Course of Posttraumatic Stress in Children: Examination of Recovery Trajectories Following Traumatic Injury. Journal of Pediatric Psychology. 2010;35(6):637–645. doi: 10.1093/jpepsy/jsp050. [DOI] [PubMed] [Google Scholar]
- Liberzon I, Sripada CS. The functional neuroanatomy of PTSD: a critical review. In: MSO, EVBT-P, Ronald De Kloet BRE, editors. Stress Hormones and Post Traumatic Stress Disorder Basic Studies and Clinical Perspectives. Vol. 167. Elsevier; 2007. pp. 151–169. Retrieved from http://www.sciencedirect.com/science/article/pii/S0079612307670113. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Poverty and children’s adjustment. Newbury Park, CA: Sage Publications; 1999. [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cohen DCDJ, editor. Developmental psychopathology, Vol 3: Risk, disorder, and adaptation. 2. Hoboken, NJ, US: John Wiley & Sons Inc; 2006. pp. 739–795. [Google Scholar]
- Luthar SS, Brown PJ. Development and Psychopathology. 03. Vol. 19. Cambridge Journals Online; 2007. Maximizing resilience through diverse levels of inquiry: Prevailing paradigms, possibilities, and priorities for the future; pp. 931–955. Retrieved from href=“ http://dx.doi.org/10.1017/S0954579407000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D. The construct of resilience: Implications for interventions and social policies. Development & Psychopathology. 2000;12(4):857–885. doi: 10.1017/s0954579400004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA, Clark AE. Stepping off the hedonic treadmill: Latent class analyses of individual differences in response to major life events. Journal of Individual Differences. 2011;32(3):144–1582. doi: 10.1027/1614-0001/a000047. [DOI] [Google Scholar]
- Martikainen P, Valkonen T. American Journal of Public Health. 8_Pt_1. Vol. 86. American Public Health Association; 1996. Mortality after the death of a spouse: rates and causes of death in a large Finnish cohort; pp. 1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten AS. Resilience in children threatened by extreme adversity: Frameworks for research, practice, and translational synergy. Development and Psychopathology. 2011;23(02):493–506. doi: 10.1017/S0954579411000198. [DOI] [PubMed] [Google Scholar]
- Masten AS, Best KM, Garmezy N. Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology. 1990;2(04):425–444. [Google Scholar]
- Masten AS, Narayan AJ. Annual Review of Psychology. 1. Vol. 63. Annual Reviews; 2012. Child Development in the Context of Disaster, War, and Terrorism: Pathways of Risk and Resilience; pp. 227–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Coatsworth JD. Competence, resilience, & psychopathology. In: DC, Cohen D, editors. Developmental Psychology. Vol. 2. New York: Wiley; 1995. pp. 715–752. [Google Scholar]
- Masten AS, Wright M. Resilience over the lifespan: Developmental Perspectives on Resistance, Recovery. In: Reich JS, Zautra JW, Hall AJ, editors. Handbook of adult resilience. New York, London: The Guilford Press; 2010. [Google Scholar]
- McCrae RR, Costa PT, Ostendorf F, Angleitner A, Hrebickova M, Avia MD, Sanz J, et al. Nature over nurture: Temperament, personality, and life span development. Journal of Personality and Social Psychology. 2000;78(1):173–186. doi: 10.1037/0022-3514.78.1.173. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Annual Review of Psychology. Vol. 54. US: Annual Reviews; 2003. Progress and controversy in the study of posttraumatic stress disorder; pp. 229–252. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Are We Winning the War Against Posttraumatic Stress Disorder? Science. 2012;336(6083):872–874. doi: 10.1126/science.1222069. Retrieved from http://www.sciencemag.org/content/336/6083/872.abstract. [DOI] [PubMed] [Google Scholar]
- Middleton W, Burnett P, Raphael B, Martinek N. The bereavement response: A cluster analysis. British Journal of Psychiatry. 1996;169(2):167–171. doi: 10.1192/bjp.169.2.167. [DOI] [PubMed] [Google Scholar]
- Mischel W. American Psychologist. 11. Vol. 24. US: American Psychological Assn; 1969. Continuity and change in personality; pp. 1012–1018. [DOI] [PubMed] [Google Scholar]
- Mortensen K, Wilson RK, Ho V. Physical and mental health status of Hurricane Katrina evacuees in Houston in 2005 and 2006. Journal of health care for the poor and underserved. 2009;20(2):524–538. doi: 10.1353/hpu.0.0130. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Folkman S, Acree M. Do positive psychological states shed light on recovery from bereavement? Findings from a 3-year longitudinal study. Death Studies. 2003;27(6):471–500. doi: 10.1080/07481180302885. [DOI] [PubMed] [Google Scholar]
- Murphy LB, Moriarty AE. Vulnerability, coping, and growth. New Haven, CT: Yale University Press; 1976. [Google Scholar]
- Murphy Lois B, Moriarty AE. Vulnerability, coping and growth from infancy to adolescence. Oxford, England: Yale U Press; 1976. p. xxiii.p. 460. [Google Scholar]
- Nolen-Hoeksema S, Morrow J. Journal of Personality and Social Psychology. 1. Vol. 61. US: American Psychological Association; 1991. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake; pp. 115–121. [DOI] [PubMed] [Google Scholar]
- Norris FH. Journal of Consulting and Clinical Psychology. 3. Vol. 60. American Psychological Association; US: 1992. Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups; pp. 409–418. [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M, Galea S. Social Science & Medicine. 12. Vol. 68. Netherlands: Elsevier Science; 2009. Looking for resilience: Understanding the longitudinal trajectories of responses to stress; pp. 2190–2198. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 Disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65(3):207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Offidani E, Ruini C. Psychobiological correlates of allostatic overload in a healthy population. Brain, Behavior, and Immunity. 2012;26(2):284–291. doi: 10.1016/j.bbi.2011.09.009. [DOI] [PubMed] [Google Scholar]
- Ong AD, Fuller-Rowell TE, Bonanno GA. Prospective Predictors of Positive Emotions Following Spousal Loss. Psychology and Aging. 2010;25(3):653–660. doi: 10.1037/a0018870. [DOI] [PubMed] [Google Scholar]
- Ong AD, Fuller-Rowell TE, Bonanno GA, Almeida DM. Spousal Loss Predicts Alterations in Diurnal Cortisol Activity Through Prospective Changes in Positive Emotion. Health Psychology. 2011;30(2):220–227. doi: 10.1037/a0022262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter-Brick C, Eggerman M. In: Understanding Culture, Resilience, and Mental Health: The Production of Hope. Ungar M, editor. Springer; New York: 2012. pp. 369–386. [DOI] [Google Scholar]
- Pennebaker JW. Putting stress into words: health, linguistic, and therapeutic implications. Behaviour Research and Therapy. 1993;31(6):539–548. doi: 10.1016/0005-7967(93)90105-4. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8347112. [DOI] [PubMed] [Google Scholar]
- Quale AJ, Schanke AK. Resilience in the face of coping with a severe physical injury: a study of trajectories of adjustment in a rehabilitation setting. Rehabilitation Psychology. 2010;55(1):12–22. doi: 10.1037/a0018415. [DOI] [PubMed] [Google Scholar]
- RUTTER M. Annals of the New York Academy of Sciences. 1. Vol. 1094. Blackwell Publishing Inc; 2006. Implications of Resilience Concepts for Scientific Understanding; pp. 1–12. Retrieved from http://dx.doi.org/10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. Journal of Personality and Social Psychology. 1987;52(3):596–604. doi: 10.1037//0022-3514.52.3.596. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3572727. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Psychological Bulletin. Vol. 132. American Psychological Association; US: 2006. Patterns of Mean-Level Change in Personality Traits Across the Life Course: A Meta-Analysis of Longitudinal Studies; pp. 1–25. [DOI] [PubMed] [Google Scholar]
- Robins RW, John OP, Caspi A, Moffitt TE, Stouthamer-Loeber M. Journal of Personality and Social Psychology. 1. Vol. 70. US: American Psychological Association; 1996. Resilient, overcontrolled, and undercontrolled boys: Three replicable personality types; pp. 157–171. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Amstadter AB, Acierno R, Kilpatrick DG, Resnick HS, Tracy M, Galea S. Social and psychological resources associated with health status in a representative sample of adults affected by the 2004 Florida hurricanes. Psychiatry. 2009;72(2):195–210. doi: 10.1521/psyc.2009.72.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Protective factors in children’s responses to stress and disadvantage. In: Kent MW, Rolf JE, editors. Primary prevention of psychopathology: Vol. 3: Social competence in children. Vol. 3. New Hampshire: University Press of New England; 1979. pp. 49–74. [Google Scholar]
- Rutter M. Resilience concepts and findings: Implications for family therapy. Journal of Family Therapy. 1999;21(2):119–144. [Google Scholar]
- Rutter Michael. The British Journal of Psychiatry. Vol. 147. United Kingdom: Royal College of Psychiatrists; 1985. Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder; pp. 598–611. [DOI] [PubMed] [Google Scholar]
- Rutter Michael. Resilience reconsidered: Conceptual considerations, empirical findings, and policy implications. In: Meisels JPSSJ, editor. Handbook of early childhood intervention. 2. New York, NY, US: Cambridge University Press; 2000. pp. 651–682. [DOI] [Google Scholar]
- Ryff CD, Singer BH, Dienberg-Love G. Positive health: connecting well–being with biology. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences. 2004;359(1449):1383–1394. doi: 10.1098/rstb.2004.1521. Retrieved from http://rstb.royalsocietypublishing.org/content/359/1449/1383.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff Carol D, Singer B. From social structure to biology: Integrative science in pursuit of human health and well-being. In: Snyder SJ, Lopez CR, editors. Handbook of positive psychology. Oxford: Oxford University Press; 2002. pp. 541–555. [Google Scholar]
- Saigh PA, Mroueh M, Bremner JD. Scholastic impairments among traumatized adolescents. Behaviour Research and Therapy. 1997;35(5):429–436. doi: 10.1016/s0005-7967(96)00111-8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9149452. [DOI] [PubMed] [Google Scholar]
- Saigh PA, Yasik AE, Oberfield RA, Halamandaris PV, McHugh M. An analysis of the internalizing and externalizing behaviors of traumatized urban youth with and without PTSD. Journal of Abnormal Psychology. 2002;111(3):462–470. doi: 10.1037//0021-843x.111.3.462. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12150422. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Laub JH. Annual Review of Sociology. Vol. 18. Annual Reviews; 1992. Crime and Deviance in the Life Course; pp. 63–84. Retrieved from http://www.jstor.org/stable/2083446. [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein J-Y, Kwok O-M, Haine RA, Twohey-Jacobs J, et al. The Family Bereavement Program: Efficacy evaluation of a theory-based prevention program for parentally bereaved children and adolescents. In: Sandler Irwin N., editor. Journal of Consulting and Clinical Psychology. 3. Vol. 71. Arizona State U, Dept of Psychology, P. O. Box 871104, Tempe, AZ, US, 85287-1104 irwin.sandler@asu.edu: American Psychological Association; 2003. pp. 587–600. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, Ayers TS. Death Studies. 1. Vol. 32. Routledge; 2007. Resilience Rather Than Recovery: A Contextual Framework on Adaptation Following Bereavement; pp. 59–73. [DOI] [PubMed] [Google Scholar]
- Sandler I, Wolchik S, Ayers T, Tein J-Y, Coxe S, Chow W. Handbook of Bereavement Research and Practice. Washington, D.C: American Psychological Association; 2008. Linking theory and intervention to promote resilience in parentally bereaved children. [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7815302. [DOI] [PubMed] [Google Scholar]
- Schulz R, Mendelsohn AB, Haley WE, Mahoney D, Allen RS, Zhang S, Thompson L, et al. New England Journal of Medicine. 20. Vol. 349. Massachusetts Medical Society; 2003. End-of-Life Care and the Effects of Bereavement on Family Caregivers of Persons with Dementia; pp. 1936–1942. [DOI] [PubMed] [Google Scholar]
- Schwarzwald J, Weisenberg M, Solomon Z, Waysman M. Stress reactions of school-age children to the bombardment by Scud missiles: a 1-year follow-up. Journal of Traumatic Stress. 1994;7(4):657–667. doi: 10.1007/BF02103013. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7820355. [DOI] [PubMed] [Google Scholar]
- Shear K, Houck PR, Reynolds CF, FE Treatment of complicated grief: A randomized controlled trial. JAMA: The Journal of the American Medical Association. 2005;293(21):2601–2608. doi: 10.1001/jama.293.21.2601. Retrieved from http://dx.doi.org/10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M, Schut H. The dual process model of coping with bereavement: Rationale and description. Death Studies. 1999;23(3):197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Zech E, Stroebe MS, Abakoumkin G. Journal of Social and Clinical Psychology. 7. Vol. 24. US: Guilford Publications; 2005. Does social support help in bereavement? pp. 1030–1050. Retrieved from. [DOI] [Google Scholar]
- Tang CS-kum. Trajectory of Traumatic Stress Symptoms in the Aftermath of Extreme Natural Disaster: A Study of Adult Thai Survivors of the 2004 Southeast Asian Earthquake and Tsunami. The Journal of Nervous and Mental Disease. 2007;195(1) doi: 10.1097/01.nmd.0000242971.84798.bc. Retrieved from http://journals.lww.com/jonmd/Fulltext/2007/01000/Trajectory_of_Traumatic_Stress_Symptoms_in_the.9.aspx. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Brown JD. Psychological Bulletin. 2. Vol. 103. US: American Psychological Assn; 1988. Illusion and well-being: A social psychological perspective on mental health; pp. 193–210. [PubMed] [Google Scholar]
- Ullman J, Newcomb M. I felt the earth move: A prospective study of the 1994 Northridge earthquake. In: Cohen L, Slomkowski P, Robins C, editors. Historical and Geographical influences on Psychopathology. 1999. p. 2170246. [Google Scholar]
- Vaillant GE, Davis JT. American Journal of Orthopsychiatry. 2. Vol. 70. Blackwell Publishing Ltd; 2000. Social/Emotional Intelligence and Midlife Resilience in Schoolboys With Low Tested Intelligence; pp. 215–222. Retrieved from http://dx.doi.org/10.1037/h0087783. [DOI] [PubMed] [Google Scholar]
- Vernberg EM, La Greca AM, Silverman WK, Prinstein MJ. Journal of Abnormal Psychology. 2. Vol. 105. American Psychological Association; US: 1996. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew; pp. 237–248. [DOI] [PubMed] [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–178. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7850498. [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Cannon MF, Marino RC, Romano DM, Scott BG, Perry AM, et al. Post traumatic stress, context, and the lingering effects of the Hurricane Katrina disaster among ethnic minority youth. Journal of abnormal child psychology. 2010;38(1):49–56. doi: 10.1007/s10802-009-9352-y. [DOI] [PubMed] [Google Scholar]
- Welch WM. USA Today. 2005. Trauma of Iraq war haunting thousands returning home. [Google Scholar]
- Werner EE. Stress and protective factors in childrens lives. In: Nicol AR, editor. Longitudinal studies in child psychology and psychiatry. New York: Wiley and Sons; 1985. pp. 335–355. [Google Scholar]
- Werner E, Smith R. Vulnerable but invincible: A study of resilient children. New York: McGraw-Hill; 1982. [Google Scholar]
- Westphal M, Seivert NH, Bonanno GA. Expressive Flexibility. Emotion. 2010;10(1):92–100. doi: 10.1037/a0018420. [DOI] [PubMed] [Google Scholar]
- Wheaton B. American Sociological Review. 2. Vol. 55. Albany; United States, Albany: 1990. Life Transitions, Role Histories, and Mental Health; p. 209. Retrieved from http://ezproxy.cul.columbia.edu/login?url=http://search.proquest.com/docview/218827025?accountid=10226. [Google Scholar]
- Wortman CB, Silver RC. Journal of Consulting and Clinical Psychology. 3. Vol. 57. US: American Psychological Assn; 1989. The myths of coping with loss; pp. 349–357. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Flory JD, Southwick S, Charney DS. Annals of the New York Academy of Sciences. 1. Vol. 1071. Blackwell Publishing Inc; 2006. Developing an Agenda for Translational Studies of Resilience and Vulnerability Following Trauma Exposure; pp. 379–396. Retrieved from http://dx.doi.org/10.1196/annals.1364.028. [DOI] [PubMed] [Google Scholar]
- Yehuda R, LeDoux J. Neuron. 1. Vol. 56. Cell Press; 2007. Response Variation following Trauma: A Translational Neuroscience Approach to Understanding PTSD; pp. 19–32. Retrieved from http://linkinghub.elsevier.com/retrieve/pii/S0896627307007040. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Yang R-K, Buchsbaum MS, Golier JA. Alterations in cortisol negative feedback inhibition as examined using the ACTH response to cortisol administration in PTSD. Psychoneuroendocrinology. 2006;31(4):447–451. doi: 10.1016/j.psyneuen.2005.10.007. Retrieved from http://www.sciencedirect.com/science/article/pii/S0306453005002222. [DOI] [PubMed] [Google Scholar]