Abstract
Despite growing interest in disparities in access to health care, relatively little is known about different facets of care among Latinas, their satisfaction with the care they receive, and the predictors of satisfaction. This study examined whether various health care access and context factors, the quality of the patient-physician interaction, and medical mistrust predict satisfaction with health care among Latina immigrants in New York City. Structured interviews were conducted with 220 Latinas predominantly from the Dominican Republic and aged 40 years or over. Of the access to health care variables examined, greater waiting time predicted dissatisfaction with health care. Greater quality of the patient-physician interaction predicted less dissatisfaction. The effect of the patient-physician interaction on dissatisfaction was mediated, in part, by waiting time. The results illustrate the important role of specific health care factors in satisfaction with care.
Keywords: Latino, Hispanic, access to health care, patient satisfaction
Numbering 35.3 million people, Latinos constitute 12.5% of the United States population. 1 As the largest ethnic minority group in the country,1 Latinos and their health status merit substantial study as indicators of the health of the nation. In 2003, the Institute of Medicine published a report on disparities in health care between the majority and racial and ethnic groups in the United States.2 The volume constituted a landmark report for many reasons. In addition to documenting numerous disparities, a crucial contribution was its specification and discussion of the multitude of factors that constitute health care. By describing features of health care systems and settings, of physicians, and of patients, the report emphasized the importance of considering access to health care as a multi-component concept.
Access to health care facilitates timely treatment, and it plays a critical role in promoting health and obtaining screening and preventive services. Moreover, satisfaction with health care has important implications for the utilization of health care services.3 Racial and ethnic differences in patient satisfaction with health care have been documented.4 However, satisfaction among Latinos warrants further investigation and attention given linguistic and cultural needs. Prior studies find that Spanish-speaking Latinos are more dissatisfied with health care than English-speaking Latinos.35 Latinos are more dissatisfied with health care than non-Latino Whites in some studies,3 but not others.6 Although factors such as patient-physician interaction are important predictors of patient satisfaction, we have yet to understand fully the mechanisms contributing to health care satisfaction among Latinos.
Although disparities in health care occur across the life course,2 in this study we focus on middle-aged and older women who are at increased risk of a variety of chronic and other health conditions relative to younger women. In addition, specific preventive and screening services (e.g., mammography) are recommended for this age group. Thus, access to care takes on particular importance for this population. Indeed, a recent review concluded that health care variables are the most consistent predictors of recent mammography among Latinas.7
In this study, we focus especially on women from the Dominican Republic living in New York City. Although Latinos share many traits, there is growing recognition of the heterogeniety of the Hispanic population in the United States, both in terms of sociodemographic and health characteristics.8 Census data indicate that the number of Dominicans in the U.S. (total 764,945 people) is approaching that of Cubans (total 1.2 million people), making Dominicans the 4th largest Latino group in the nation.1 New York City currently houses the largest settlement of Dominicans in the United States.9 Although Dominicans constitute a growing and significant group in the United States, very little is known about the health of this Latino population.
Conceptual framework
Adopting a multiple-component conceptualization of access to health care, the main goal of this study was to examine satisfaction with health care among a sample predominantly of Dominican women. This study borrows from a multi-dimensional framework of access to health care proposed by Penchansky and Thomas,10 focusing on four components: affordability, accessibility, accommodation, and acceptability. We use Penchansky and Thomas’s conceptual framework as a general guide, and, drawing from the Institute of Medicine’s landmark report,2 expand the model to further explore other important aspects of health care: the nature of the patient-physician relationship and medical mistrust.
Affordability—the ability to pay for medical care—is fundamental to obtaining preventive care and other health services.2 Lack of health insurance, a common affordability index, erects a significant barrier to care. Other components of access, accessibility and accommodation, may influence utilization of general health care and preventive services. Accessibility denotes the ease of obtaining services in the community, such as distance, transportation, and travel. Accommodation denotes the tailoring of health services to fit the needs of a community. Although accommodation might be assessed by various indicators, for Latinos the availability of services that promote effective communication are critical. A large proportion of Latinos have limited English proficiency or live in linguistically isolated households,2 and limited English is associated with lack of a usual source of care.11
Affordability, accessibility, and accommodation may play important roles in overall acceptability of health care. Acceptability refers to the actual and perceived value of care by the patient, and can be assessed as general satisfaction with care. Factors that predict satisfaction with health care among Latinos are not well-known. Nevertheless, there is evidence that Latinos are more likely to choose an ethnically-concordant than discordant physician,12 and that Latinos report high levels of satisfaction if their physicians are ethnically-concordant.13
Other features of the health care setting, such as having a usual source of medical care, are important in promoting high-quality care and continuity of services.2 Having a usual source of care could lead to better quality of care due to improved patient-physician interactions (e.g., increased duration and frequency of contact with patients, better communication, greater trust, or increased physician recommendations for preventive care).14 Thus, having a usual source of medical care may contribute to improved patient-physician interactions and satisfaction with health. However, these potential pathways have not been explored fully.
A number of studies point to medical mistrust as another important variable to consider in the context of patient-physician interactions and general satisfaction with health care. Medical mistrust stems from a variety of sources that include historic, salient cases of mistreatment of ethnic minorities, and racism and discrimination experienced in the health care system.2 Although the bulk of these studies focus on African Americans, Latinos, too, report racism as a significant problem in health care, they express concern about being mistreated because of their ethnic background, and they are more likely than Whites to believe that Hispanics receive poorer quality health care than Whites receive.15
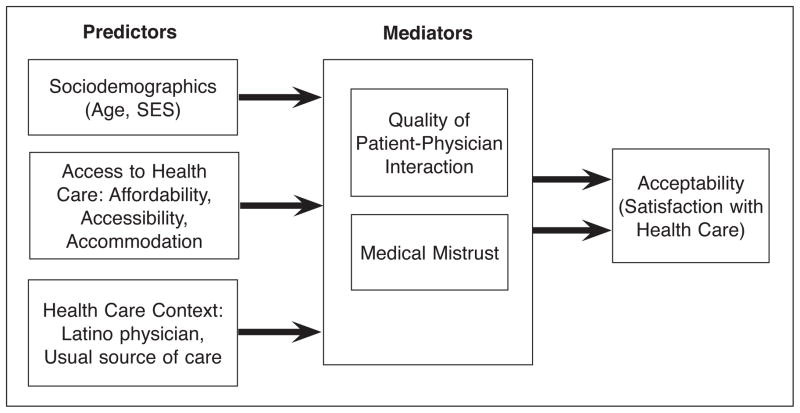
This study had two objectives: (1) to examine descriptive data on health care factors, quality of patient-physician interactions, and medical mistrust among Latinas; and (2) using a multi-dimensional framework, to determine whether various health care variables predict quality of patient-physician interactions, medical mistrust, and satisfaction with care. Figure 1 illustrates a schematic model concerning the specific associations of interest. Adjusting for sociodemographic factors, we test whether affordability, accessibility, language accommodation (access to health care variables), and having a usual source of care and ethnically-concordant physician (contextual variables) predict quality of the patient-physician interaction and medical mistrust, and whether these variables, in turn, predict satisfaction with care.
Figure 1.
Conceptual model.
Methods
Procedures
The data presented here are drawn from a larger study of breast cancer screening practices among women living in a section of New York City that is predominantly Dominican. We used several methods to recruit respondents. Women were recruited from an ambulatory care general medicine clinic of a major hospital located in the community. To maximize recruitment of women who may not access this clinic, flyers were posted in various locations throughout the medical center and surrounding neighborhood, and participants were asked to identify other eligible women living in the community. Finally, a university-based center for the study of urban minorities provided some recruitment assistance (e.g., by referring eligible participants to the study). Approximately one-third of the sample was recruited via the clinic, and two-thirds by other methods.* Eligibility criteria were: female aged 40 years or older, Hispanic ethnicity (defined as individuals of Dominican, Puerto Rican, Mexican, Cuban, South or Central American, or other Spanish culture or origin), and no prior diagnosis of any form of cancer. All participants gave their informed consent prior to their inclusion in the study, and the research was approved by the university’s medical center Internal Review Board. A total of 220 Latinas participated in the study.
Data were collected by a structured interview conducted in Spanish at the respondent’s site of choice (e.g., home or clinic). Interviews lasted an average of 41 minutes. Most (54.5%) took place in respondents’ homes, and the remaining 30.9% in the homes of friends or relatives, or in the clinic (14.1%). Respondents were paid $25 for their participation.
Measures
Spanish versions of all scales, except for the Group-Based Medical Mistrust Scale (for which a Spanish version already existed) were created for this study using a back-translation technique with two iterations and independent translators, as recommended by Marin and Marin.16 All translators were native Spanish speakers, with formal training in public health, psychology, or both, and prior experience in translating scales for research projects. Pilot tests were conducted to ensure that participants understood questionnaire items.
Sociodemographic variables
Age was coded in years as a continuous variable. Socioeconomic Status (SES) was assessed as highest level of education completed and household income as they are reliable indices of social class.17 Education was coded in years as the highest grade completed. Household income ranged from 1 (less than $10,000/year) to 8 ($70,000 per year or more).
Health care access variables
Affordability of health care was assessed as having any health insurance, coded as 0 = no health insurance, 1 = any type of health insurance (including private insurance or any form of public insurance, e.g., Medicaid, Medicare).
Accessibility of health care was operationalized as travel time, measured by asking respondents how long it takes to travel to their usual place of health care; and waiting time, measured as respondents’ reports of how long they normally have to wait to receive medical attention after arriving at their usual place of health care. We coded travel and waiting time in minutes.
Accommodation was operationalized as lack of language accommodation, specifically, communication difficulty, by asking respondents how they communicate with their physician. Response options included: in English without difficulty, in English with difficulty, in Spanish without difficulty, in Spanish with difficulty, or with a translator (which included medical, informal, or friend/family member). We recoded this item to create a communication difficulty dichotomous variable, where 0 = no difficulty, defined as respondents who communicate with their physicians without difficulty in either English or Spanish; and 1 = with difficulty, defined as communicating with difficulty in either English or Spanish, or requiring a translator.
Health care context variables
Usual source of health care was derived from two commonly-used indices of access to health care: (1) whether the respondent has a routine place for health care (yes/no), and (2) the usual source of care. Usual source of health care was coded with higher scores approximating greater access as follows: 0 = none (respondent has no usual health care provider); the usual source of care is 1 = emergency room, 2 = hospital outpatient clinic, 3 = health center or company clinic, 4 = private physician’s office. These indices are used commonly in national surveys to measure access to care.2 In the analyses described below, results remained virtually identical regardless of whether we used the dichotomus (yes/no) or the continuous variable (with higher values representing greater access to care). Thus, we used the continuous variable in analyses.
Latino physician, our measure of patient-physician ethnicity concordance, was a dichotomous variable coded on the basis of respondent’s reports, 1 = physician is Latino, 0 = physician is non-Latino (i.e., any other ethnic/racial category).
Preference for Latino physician was assessed by asking respondents, “Do you prefer to be seen by a doctor of your own ethnic group?” Response options were: Yes, No, I don’t care, or If he/she speaks Spanish, I don’t care.
Mediators
Quality of the patient-physician interaction was assessed using a slightly modified version of Saha et al.’s five-item interaction index, derived from the Commonwealth Fund’s 2001 Health Care Quality Survey.19 The scale measures the quality of general patient-physician interactions during the last visit (e.g., “The last time you visited your doctor, did the doctor listen to everything you had to say?,” “Did the doctor involve you in decisions about your care?,” “Did the doctor treat you with respect and dignity?”). We modified the scale slightly to standardize all items to a three-point response scale (as the original scale contained both two- and three-point responses), and recoded items such that greater scores indicate higher quality interaction, with scores that could range from 1 to 3. In the present study, the scale showed good reliability (Cronbach’s α=0.75).
Medical mistrust was assessed with the Spanish version of the Group-Based Medical Mistrust Scale (GBMMS),18 which taps suspicion (e.g., “People of my ethnic group cannot trust doctors and health care workers”), the perception that disparities in health care are rooted in race-based treatment (e.g., “People of my ethnic group are treated the same as people of other groups by doctors and health care workers”), and lack of support from health care providers (e.g., “Doctors and health care workers do not take the medical complaints of people of my ethnic group seriously”) on a scale of 1 = strongly disagree to 5 = strongly agree. After reverse-coding appropriate items, we calculated the mean across the 12 twelve items for each participant, yielding scores that may range from 1 to 5, with higher scores indicating greater levels of mistrust. In this study, the internal consistency of the GBMMS was good (Cronbach’s α=0.75).
Main dependent variable
Acceptability of health care was operationalized as overall dissatisfaction with care using a one-item measure previously used with diverse samples, including Latinos.19 Participants rated their dissatisfaction, “How satisfied are you with the quality of medical care that you receive in your usual place of medical care?”, on a four-point scale ranging from 1 = very satisfied to 4 = not at all satisfied. We modified the original item slightly by omitting the phrase “over the past 2 years” and adding “in your usual place of medical care.” Respondents with no usual place of care were asked to respond in reference to the place where they last received care.
Statistical analyses
To examine the relationships among variables depicted in Figure 1, we conducted a series of hierarchical multiple regression analyses. The principal paths involve the effects of sociodemographic characteristics and health care variables on dissatisfaction with care. Mediation hypotheses centered on whether quality of the patient-physician interaction and medical mistrust mediate the association between health care variables and dissatisfaction with health care.
We tested the model with path analysis using reduced form equations, a procedure involving a series of hierarchical regression equations in which each variable is entered in order of causal priority.20 Mediation is tested by examining indirect effects. An indirect effect of a variable via a specific mediator is calculated as the difference in the variable’s coefficient before and after the mediator enters the equation. At the final step of the equations, coefficients represent the direct effects of each predictor variable.
In these regression equations, sociodemographic characteristics (age, education, income) were entered as a set in the first step. In the second step, we entered as a set access to health care variables: affordability (health insurance), accessibility (travel time to care, waiting time), language accommodation (communication difficulty), and health care context variables (Latino ethnicity of the physician and having a usual source of care). On the third step, we entered quality of the patient-physician interaction and medical mistrust as a set to assess whether these variables mediate the effects of health care variables on dissatisfaction with care. Rather than entering mediating variables one by one, we entered them as a set to more accurately reflect the theoretical model that we were testing.
These equations yield path coefficients from predictor (sociodemographic characteristics, health care access, and contextual variables) and mediating variables (quality of patient-physician interaction and medical mistrust) to the criterion variable of dissatisfaction. To complete the model, paths from predictor to mediating variables were calculated (see Baron & Kenny21).
Results
Descriptive statistics
Table 1 provides data on sociodemographic, health care, and other variables. The majority of participants were from the Dominican Republic, and all were foreign-born. The average respondent had a low socioeconomic status.
Table 1.
SAMPLE CHARACTERISTICS (TOTAL N = 220)
| Place of Birth (N, %) | ||
| Dominican Republic | 209 | 95.0 |
| Central or South America | 6 | 2.7 |
| Puerto Rico | 5 | 2.3 |
| Years residing in U.S. (M, SD) | 23.3 | 11.7 |
| Speak English: Not at all or very little (N, %) | 158 | 71.8 |
| Age (M, SD) | 56.6 | 11.2 |
| Years of education (M, SD) | 9.4 | 4.5 |
| Household income less than $10,000/year (N, %) | 127 | 57.7 |
| Access to Health Care: | ||
| Affordability, accessibility, and language accommodation | ||
| Has health insurance (N, %) | 209 | 95.0 |
| Travel time (in minutes) to health care facility (M, SD) | 20.5 | 16.2 |
| Waiting time (in minutes) (M, SD) | 94.4 | 72.7 |
| Communication difficulty with health care provider | 40 | 18.2 |
| Health care contextual factors | ||
| Usual source of health care (N, %) | ||
| None | 10 | 4.5 |
| Emergency Room | 3 | 1.4 |
| Hospital outpatient clinic | 121 | 55.0 |
| Health center or company clinic | 28 | 12.7 |
| Private physician | 58 | 26.4 |
| Physician ethnic concordance and preferences (N, %) | ||
| Has Latino doctor | 123 | 55.9 |
| Prefers Latino doctor? | ||
| Yes | 89 | 40.5 |
| No | 8 | 3.6 |
| Does not care | 43 | 19.5 |
| If doctor speaks Spanish, does not care | 75 | 34.1 |
| Quality of patient-physician interaction (M, SD) | 2.9 | .2 |
| Medical mistrust (M, SD) | 2.2 | .9 |
| Acceptability of (dissatisfaction with) health care (M, SD) | 1.4 | .7 |
The vast majority of respondents had some type of health insurance, suggesting a high level of affordability of health care. Most (n=177, 80.5%) had public forms of insurance (e.g., Medicaid, Medicare, or both), the remainder had private health insurance or a combination of private insurance with Medicare (n=32, 14.5%) or no insurance (n=11, 5%). Accessibility was somewhat mixed. Although the average respondent traveled a short period of time to arrive at her usual place of care, she waited more than one and one-half hours to see a physician at that setting. Results indicated a high level of language accommodation in health care as few respondents (n=40, 18.2%) reported speaking with difficulty in either English (n=3) or Spanish (n=18), or needing a translator (n=19).
With regard to other health care context factors, very few respondents had no usual source of health care. Slightly over half had an ethnically-concordant (i.e., Latino) physician, and most either preferred a Latino physician or did not state a preference so long as the doctor speaks Spanish. Most respondents (n=174, 79.1%) had a physician whose characteristics matched their preferences (concerning ethnicity or Spanish fluency).
Having a Latino physician was associated with lower communication difficulty. The odds of experiencing communication difficulty were lower among respondents who had a Latino versus non-Latino physician, Odds Ratio (OR) = .045 (95% CI = .02, .13), p<.0001. This could be attributed to the higher rate of Spanish-speaking Latino vs. other physicians, chi-squared (30, n=206) = 117.42, p<.0001. Of the 122 women who had a Latino physician, the vast majority (96.7%) spoke with them in Spanish without difficulty. In contrast, half (50%) of the women with non-Hispanic White physicians reported no difficulty communicating in Spanish. For respondents with physicians of other racial/ethnic groups, rates of Spanish fluency in communicating (i.e., without difficulty) were lower (Asians, 35.0%; African Americans, 38.5%; other race or race unknown, 40.0%). In terms of language accommodation, overall, these data suggest good access to health care. Finally, the average respondent reported high-quality patient-physician interactions, low medical mistrust, and a low level of dissatisfaction with her health care.
Tests of model and main hypotheses
Table 2 presents bivariate correlations of variables used in the path analyses. Dissatisfaction with care was associated with greater waiting time, communication difficulty with the health care provider, and medical mistrust; it was inversely correlated with having a usual source of health care.
Table 2.
INTERCORRELATIONS OF VARIABLES IN THE CONCEPTUAL MODEL: ACCEPTABILITY OF (DISSATISFACTION WITH) HEALTH CARE, SOCIODEMOGRAPHIC VARIABLES, AND HEALTH CARE VARIABLESa
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Dissatisfaction with care | |||||||||||
| 2. Age | −.09 | ||||||||||
| 3. Years of education | .04 | −.47*** | |||||||||
| 4. Household income | −.01 | −.20** | .30*** | ||||||||
| 5. Health insurance | .06 | .19 | −.17** | .01 | |||||||
| 6. Travel time to care | .03 | .04 | .04 | .00 | −.04 | ||||||
| 7. Waiting time | .36*** | −.05 | −.12 | −.02 | −.02 | .08 | |||||
| 8. Communication difficulty | .14* | .03 | −.14* | −.16* | .02 | .15* | .04 | ||||
| 9. Latino physician | −.11 | .07 | −.03 | .08 | .10 | −.08 | .00 | −.49*** | |||
| 10. Usual source of care | −.06 | .11 | −.02 | .21** | .20** | −.10 | .08 | −.09 | .24*** | ||
| 11. Quality of patient-physician interaction | −.54*** | .03 | .01 | .00 | −.06 | .10 | −.13* | −.06 | .13 | −.05 | |
| 12. Medical mistrust | .19** | −.20** | .14* | .03 | .01 | .02 | .12 | −.04 | .02 | −.02 | −.09 |
Acceptability of health care is assessed as dissatisfaction with care; accessibility indices are travel time to usual source of care and waiting time to receive care; language accommodation is assessed as communication difficulty.
p<.05
p<.01
p<.001
Table 3 shows the results of regression analyses predicting dissatisfaction with health care. (Analyses predicting quality of patient-physician interaction and medical mistrust are not shown but are available from the authors.) Figure 2 illustrates direct paths obtained from the final steps in these models. Only significant paths are shown to simplify the diagram.
Table 3.
REGRESSION ANALYSIS OF PATIENT SOCIODEMOGRAPHIC CHARACTERISTICS, HEALTH CARE VARIABLES, QUALITY OF PATIENT-PHYSICIAN INTERACTION, AND MEDICAL MISTRUST AS PREDICTORS OF DISSATISFACTION WITH HEALTH CAREa
| Step and variable entered | Beta
|
R2 | ΔR2 | ΔF | Model F | ||
|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | |||||
| Step 1 | .01 | .01 | .60 | .60 | |||
| Age | −.10 | −.06 | −.03 | ||||
| Years of education | .00 | .09 | .08 | ||||
| Household income | −.03 | −.03 | −.02 | ||||
| Step 2 | .17 | .166 | .29*** | 4.42*** | |||
| Health insurance | .09 | .05 | |||||
| Travel time to care | −.01 | .04 | |||||
| Waiting time | .36*** | .28*** | |||||
| Communication difficulty | .11 | .11+ | |||||
| Latino physician | −.07 | .00 | |||||
| Usual source of care | .05 | .03 | |||||
| Step 3 | .41 | .24 | 38.49** | 12.01*** | |||
| Quality of pt-phys interaction | −.48*** | ||||||
| Medical mistrust | .10+ | ||||||
The final step contains coefficients for direct effects (illustrated in Figure 2). Indirect effects via mediators (e.g., quality of patient-physician interaction and medical mistrust) are calculated by subtracting the coefficient of a particular predictor from its coefficient at the previous step.
p≤.10
p≤.05
p≤.01
p≤.001
= Change
Pt-phys = Patient-physician
Figure 2.
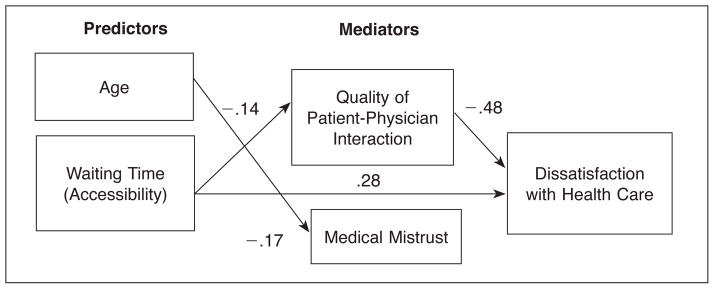
Results: conceptual model.
Table 3 (see also Figure 2) shows that greater waiting time predicted more dissatisfaction (β=.28), and increased quality of patient-physician interaction predicted less dissatisfaction (β= −.48). Communication difficulty (β=.11) and greater medical mistrust (β=.10) were also associated with more dissatisfaction, but these effects were marginally significant, p=.09 and .08, respectively. None of the sociodemographic variables or other health care factors predicted dissatisfaction. The full model accounted for almost one-half (41%), of the variance in dissatisfaction with health care, R2=.41, F(11, 204) = 12.01, p<.0001.
Figure 2 also illustrates paths to the mediating variables, quality of patient-physician interaction and medical mistrust (results not shown). Greater waiting time predicted lower quality of patient-physician interaction (β=−.14). Having a Latino physician was a marginally significant predictor of quality of patient-physician interaction (β=.15), p=.07. Medical mistrust was associated with lower age (β= −.17) and greater waiting time (β=.12), but the latter was marginally significant, p=.09. Overall, the final models predicted a very little and non-significant amount of the variance (6%) in both quality of patient-physician interaction, R2=.06, F(9, 204) = 1.27; and medical mistrust, R2=.06, F(9, 204) = 1.48.
In Table 3, inspection of the change in the coefficient for waiting time from step 2 (β=.36) to step 3 (β=.28) indicates that the effect of waiting time on dissatisfaction was partially mediated by quality of patient-physician interaction and medical mistrust.
Discussion
Despite growing interest in health disparities and access to health care, relatively little is known concerning whether various access factors predict satisfaction with care among Latinas. This study sought to address these gaps in the literature. With respect to affordability, accessibility, and language accommodation, overall, findings reveal good access to health care. The vast majority of participants had some form of health insurance, and the average respondent traveled a relatively short period of time to reach her place of care. The average wait time, however, was quite long (slightly more than 90 minutes), but most participants did not report having communication difficulties with their provider.
Resources related to Latino immigrant enclaves may contribute to the rates of access to health care observed in this study. Two studies22,23 suggest that access to health care varies by the racial/ethnic composition of the individual’s area of residence, with greater access in Latino enclaves. For example, Latinos are less likely to report experiencing difficulty in obtaining health care or to delay obtaining care when they live in a county with higher versus lower proportion of Latinos.22 Although predominantly low-income, the Latino enclave from which we recruited participants may provide a variety of resources, including access to community-based agencies that provide social and other services, as well as to Spanish-speaking Hispanic physicians. In addition, New York also has a “long history of providing access to poor people through public programs.”24[p.161] The high rate of health insurance among our participants is consistent with rates reported in larger surveys of the community from which our sample was drawn.25 It is possible that health coverage provided participants with access to the health care system and to a usual source of care.
Of the access to health care components examined, only waiting time significantly predicted dissatisfaction with care. This replicates prior observations on the link between shorter wait times and greater satisfaction.26 Whether waiting time affects Latinas’ satisfaction with care may depend on perceptions of what they consider acceptable27 or “normal.”28 Wait times that exceed patients’ expectations result in dissatisfaction with overall care. Longer waiting times may also depend on type of health coverage, as patients with Medicare or Medicaid are more likely to report long waits relative to those with private insurance.29
With regard to language accommodation, few participants reported communication difficulties with their health care provider. This result is probably due to physician characteristics. Specifically, about one-half of respondents had an ethnically-concordant (i.e., Latino) physician, which was associated with a lower likelihood of experiencing communication difficulties. Complementing findings that Latino patients are more likely than other racial groups to prefer having a provider of the same race,19,30,31 the majority of our sample—about two-thirds—either preferred an ethnically-concordant physician, or stated no ethnic background preference so long as their physician spoke Spanish. There is limited research on the reasons underlying patients’ preferences for health care providers of their own ethnic groups. Among Latinos, language appears to be an important factor in these preferences: almost one-half (42%) of Latinos who could select their health care provider chose a Latino physician due to language difficulties with other providers;12 and having an ethnically-concordant physician is associated with language fluency (i.e., reporting English as a second language13).
Limited research examines whether patient-physician ethnic-concordance is associated with improved interactions in clinical settings and satisfaction with health care, especially among Latino populations. Although not significant, in Chen et al.’s study,30 a greater number of Latinos who preferred and had an ethnically-concordant physician rated their provider as excellent compared with Latinos who preferred but did not have a Latino provider (40% vs. 29%). Saha et al.,19 however, found that race concordance did not increase Latino patient’s satisfaction with their health care, a finding that we replicated. In this study, quality of the patient-physician interaction played a significant role in dissatisfaction with care. Of note is that Latino cultural values include the expectation that individuals be treated with respeto (respect) and cortesía (courtesy), values that are tapped by Saha et al.’s19 measure of quality used in this study. These values may take on particular significance in the health care setting. In this study, having a Latino physician was marginally associated with better quality of the patient-physician interaction. Although only marginally significant, having an ethnically-concordant (i.e., Latino) physician familiar with cultural nuances and norms may contribute to better clinical interactions. Because culture influences how individuals define and express illness, suffering, and dying, lack of cross-cultural skills among health care providers or their failure to understand cultural values may lead to poor patient outcomes and inappropriate interactions in clinical settings. Recognition of the importance of understanding cultural beliefs and values has promoted a growing movement in cultural competence in the health professions. The results of this study underscore the importance of good quality and culturally relevant medical interactions in predicting satisfaction with health care.
Overall, respondents expressed low levels of medical mistrust. Greater age was associated with less mistrust, and greater mistrust was a marginally statistically significant predictor of dissatisfaction with health care. These results complement the Institute of Medicine’s conclusions that despite levels of mistrust, minority patients express satisfaction with their health care providers.2 In a study of Latinos with HIV, medical mistrust was lower among patients with a racial/ethnic concordant than discordant physician.32 However, other studies provide mixed findings such that concordance increases the likelihood of Latinos’ reporting mistreatment on some indicators (being treated with disrespect) but not others (unfair treatment due to race, language, and receiving differential treatment).33 Because many of our participants had a provider who met their racial/ethnic background and/or language preference, it is possible that they were less inclined to mistrust the medical system. Future studies are needed to further explore whether preferences for ethnic- and language-concordant providers predict medical mistrust.
Some limitations of our study include the lack of extensive questions on patient-physician interactions, and its cross-sectional design. Use of a single item for the main dependent variable also presents a potential limitation in assessing dissatisfaction with health care. In addition, by design, our sample consisted predominantly of women from the Dominican Republic living in New York City. Although this limits generalizability of the findings, our study contributes to a body of literature on the fourth largest subgroup of Latinos in the United States, for which there is very limited research (on any health-related topic). Nevertheless, our general findings should be considered in the context of our sample of Dominican women with relatively good access to care (e.g., most had health insurance and a physician whose ethnic background and language matched their preferences). Studies of Dominicans living in other geographic areas (as well as other Latinos) are required to determine if the findings of this study are replicable.
Despite these limitations, the strengths of this study include the examination of multiple dimensions of health care, as well as patient-physician interactions and medical mistrust as predictors of satisfaction with health care. This is one of the first studies to examine comprehensively health care access variables, in addition to contextual factors (such as patient-physician ethnicity concordance), and their associations with satisfaction with care among Latinas. Our findings suggest that even in a population where there is a high degree of affordability, other factors such as accessibility (i.e., waiting time) and quality of patient-physician interactions play a role in satisfaction with health care. Myriad health care access factors could influence acceptability of care, but many studies focus on the affordability component of access to health care. The model examined in this study does not capture all the health care or other factors that may influence satisfaction with care. For example, a growing literature documents implicit racial and ethnic biases34 that may influence clinical interactions. Nevertheless, few published studies examine various components or contexts of health care, or test potential mediators of the relationship between health care factors and satisfaction with care among Latinas. Thus, the results of this study help to narrow these gaps in the literature.
Footnotes
Due to an unfortunate oversight, a code for method of recruitment was not included in the interview booklet.
Contributor Information
Ana F. Abraído-Lanza, Associate Professor in the Department of Sociomedical Sciences, Mailman School of Public Health, Columbia University, New York.
Amarilis Céspedes, Doctoral student in the Steinhardt School of Education, New York University.
Shaira Daya, New York City Department of Health and Mental Hygiene.
Karen R. Flórez, Researcher at RAND Corporation in Santa Monica, California.
Kellee White, Assistant Professor, Department of Epidemiology and Biostatistics, Arnold School of Public Health, University of South Carolina.
Notes
- 1.Guzman B. The Hispanic population: Census 2000 brief. Washington, DC: U.S. Census Bureau; 2001. May, Available at: http://www.census.gov/prod/2001pubs/c2kbr01-3.pdf. [Google Scholar]
- 2.Haynes MA, Smedley BD, editors. The unequal burden of cancer: an assessment of NIH research and programs for ethnic minorities and medically underserved. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 3.Morales LS, Cunningham WE, Brown JA, et al. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999 Jul;14(7):409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray-Garcia JL, Selby JV, Schmittdiel J, et al. Racial and ethnic differences in a patient survey: patients’ values, ratings, and reports regarding physician primary care performance in a large health maintenance organization. Med Care. 2000 Mar;38(3):300–10. doi: 10.1097/00005650-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Napoles AM, Gregorich SE, Santoyo-Olsson J, et al. Interpersonal processes of care and patient satisfaction: do associations differ by race, ethnicity, and language? Health Serv Res. 2009 Aug;44(4):1326–44. doi: 10.1111/j.1475-6773.2009.00965.x. Epub 2009 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997 Dec;35(12):1212–9. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Wells KJ, Roetzheim RG. Health disparities in receipt of screening mammography in Latinas: a critical review of recent literature. Cancer Control. 2007 Oct;14(4):369–79. doi: 10.1177/107327480701400407. [DOI] [PubMed] [Google Scholar]
- 8.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005 Jul;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. Epub 2005 Jan 18. [DOI] [PubMed] [Google Scholar]
- 9.Kim M, Van Wye G, Kerker B, et al. The health of immigrants in New York City. New York, NY: New York City Department of Health and Mental Hygiene; 2006. Available at: http://www.nyc.gov/html/doh/downloads/pdf/episrv/episrv-immigrant-report.pdf. [Google Scholar]
- 10.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981 Feb;19(2):127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Shreffler KM, McQuillan J, Greil AL, et al. Odds of having a regular physician and perceptions of care: ethnic patterns for women ages 25–45. Fam Med. 2009 Apr;41(4):271–6. [PubMed] [Google Scholar]
- 12.Saha S, Komaromy M, Koepsell TD, et al. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999 May 10;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 13.LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002 Sep;43(3):296–306. [PubMed] [Google Scholar]
- 14.Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004 Jan;36(1):22–7. [PubMed] [Google Scholar]
- 15.Lillie-Blanton M, Brodie M, Rowland D, et al. Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev. 2000;57(Suppl 1):218–35. doi: 10.1177/1077558700057001S10. [DOI] [PubMed] [Google Scholar]
- 16.Marin G, Sabogal F, Marin BV, et al. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987 Jun;9(2):183–205. [Google Scholar]
- 17.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(Spec No):80–94. [PubMed] [Google Scholar]
- 18.Thompson HS, Valdimarsdottir HB, Winkel G, et al. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med. 2004 Feb;38(2):209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 19.Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003 Oct;93(10):1713–9. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen J, Cohen P. Applied multiple regression and correlation analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1984. [Google Scholar]
- 21.Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986 Dec;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 22.Haas JS, Phillips KA, Sonneborn D, et al. Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Med Care. 2004 Jul;42(7):707–14. doi: 10.1097/01.mlr.0000129906.95881.83. [DOI] [PubMed] [Google Scholar]
- 23.Gresenz CR, Rogowski J, Escarce JJ. Community demographics and access to health care among U.S. Hispanics. Health Serv Res. 2009 Oct;44(5 Pt 1):1542–62. doi: 10.1111/j.1475-6773.2009.00997.x. Epub 2009 Jul 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trevino FM. Quality of health care for ethnic/racial minority populations. Ethn Health. 1999 Aug;4(3):153–64. doi: 10.1080/13557859998119. [DOI] [PubMed] [Google Scholar]
- 25.Karpati A, Lu X, Mostashari F, et al. The health of Inwood and Washington Heights. New York City Community Health Profiles. 2003;1(24):1–12. [Google Scholar]
- 26.Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007 Feb 28;7:31. doi: 10.1186/1472-6963-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cassidy-Smith TN, Baumann BM, Bourdreaux ED. The disconfirmation paradigm: throughput times and emergency department patient satisfaction. J Emerg Med. 2007 Jan;32(1):7–13. doi: 10.1016/j.jemermed.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 28.Bender DE, Harbour C, Thorp J. Tell me what you mean by “si”: perceptions of quality of prenatal care among immigrant Latina women. Qual Health Res. 2001 Nov;11(6):780–94. doi: 10.1177/104973230101100607. [DOI] [PubMed] [Google Scholar]
- 29.Pippins JR, Alegria M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Med Care. 2007 Nov;45(11):1020–5. doi: 10.1097/MLR.0b013e31814847be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen FM, Fryer GE, Jr, Phillips RL., Jr Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005 Mar-Apr;3(2):138–43. doi: 10.1370/afm.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Napoles-Springer AM, Santoyo J, Houston K, et al. Patients’ perceptions of cultural factors affecting the quality of the medical encounters. Health Expect. 2005 Mar;8(1):4–17. doi: 10.1111/j.1369-7625.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sohler NL, Fitzpatrick LK, Linsay RG. Does patient-provider racial/ethnic concordance influence ratings of trust in people with HIV infection? AIDS Behav. 2007 Nov;11(6):884–96. doi: 10.1007/s10461-007-9212-0. Epub 2007 Mar 10. [DOI] [PubMed] [Google Scholar]
- 33.Blanchard J, Nayar S, Lurie N. Patient-provider and patient-staff racial concordance and perceptions of mistreatment in the health care setting. J Gen Intern Med. 2007 Aug;22(8):1184–9. doi: 10.1007/s11606-007-0210-8. Epub 2007 May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabin JA, Nosek BA, Greenwald AG. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009 Aug;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]