Abstract
Context
Policymakers and practitioners continue to pursue initiatives designed to engage individuals in their health and health care despite discordant views and mixed evidence regarding the ability to cultivate greater individual engagement that improves Americans’ health and well-being and helps manage health care costs. There is limited and mixed evidence regarding the value of different interventions.
Methods
Based on our involvement in evaluating various community-based consumer engagement initiatives and a targeted literature review of models of behavior change, we identified the need for a framework to classify the universe of consumer engagement initiatives toward advancing policymakers' and practitioners' knowledge of their value and fit in various contexts. We developed a framework that expanded our conceptualization of consumer engagement, building on elements of two common models, the individually focused transtheoretical model of behavior and the broader, multilevel social ecological model. Finally, we applied this framework to one community's existing consumer engagement program.
Findings
Consumer engagement in health and health care refers to the performance of specific behaviors (“engaged behaviors”) and/or an individual's capacity and motivation to perform these behaviors (“activation”). These two dimensions are related but distinct and thus should be differentiated. The framework creates four classification schemas, by (1) targeted behavior types (self-management, health care encounter, shopping, and health behaviors) and by (2) individual, (3) group, and (4) community dimensions. Our example illustrates that the framework can systematically classify a variety of consumer engagement programs, and that this exercise and resulting characterization can provide a structured way to consider the program and how its components fit program goals both individually and collectively.
Conclusions
Applying the framework could help advance the field by making policymakers and practitioners aware of the wide range of approaches, providing a structured way to organize and characterize interventions retrospectively, and helping them consider how they can meet the program's goals both individually and collectively.
Keywords: consumer engagement, patient activation, health behavior, conceptual framework
The ongoing pursuit of policies and programs to engage individuals in their health and health care is in large part based on their conceptual appeal. This is both the philosophical argument that individuals should have more say in their care (e.g., patient centeredness) and the performance-based argument that if obstacles to being engaged are removed (e.g., lack of information or motivation), then these active consumers will make informed decisions to behave in ways, such as selecting high-quality providers or helping design a care plan to follow, that improve the quality of their health care, their health, and their well-being and also may help contain their health care costs (e.g., Arnold 2007; DHHS 2008; Duggan et al. 2006; Epstein and Street 2011). Some people are skeptical about the power of this pathway to achieve all these desired results, especially system transformation (e.g., Berenson 2005; Hurley et al. 2009; Nichols et al. 2004), as the existing evidence for successful interventions is still limited and mixed, especially for efforts to stimulate behavior change in large numbers of consumers (e.g., Haynes et al. 2008; Ketelaar et al. 2011). When one community leader was asked about his community's efforts to improve consumer engagement, he said, “I think consumer engagement is the wild card. On the one hand, I think a lot of people are hopeful and see it as the missing link [to improving quality and controlling costs]. … On the other hand, I think it's a new enough topic that there's probably a fair amount of skepticism. I'll tell you [there is] skepticism; [colleagues ask,] ‘Is that even possible? Why should we be spending our time on that?’” (Alexander et al. 2009). This debate suggests the need for additional research into consumer engagement and for an evaluation of consumer engagement initiatives.
Meanwhile, public and private entities continue to experiment with consumer engagement initiatives. For example, the 2010 Patient Protection and Affordable Care Act (ACA) included multiple provisions to support consumer engagement, such as increasing the availability of information and assistance to consumers for decision making and resources for wellness and self-management programs (DHHS 2012). Private purchasers’ efforts, such as offering personal health coaching or consumer-directed health plans, also continue to grow: from 11 percent and 13 percent in 2008 to 27 percent and 23 percent in 2011, respectively (KFF-HRET 2008, 2011). The $300-million Aligning Forces for Quality (AF4Q) initiative, supported by the Robert Wood Johnson Foundation, is another large national program whose goal is to improve the quality of health and health care for individuals (12.5% of the U.S. population) residing in sixteen communities nationwide by, in part, implementing community-based interventions to improve consumer engagement (AF4Q 2012; Painter and Lavizzo-Mourey 2008).
We are part of the independent team hired by the Robert Wood Johnson Foundation to evaluate the AF4Q initiative, which began in 2006 (Scanlon et al. 2012). Our early efforts to “make sense of” the AF4Q communities’ varied consumer engagement activities revealed that consumer engagement is multidimensional and that these dimensions need to be made explicit and to be distinguished from one another in order to describe and compare them. We needed a framework to systematically characterize the diverse and evolving array of interventions that the AF4Q communities were piloting. While there were a range of thoughtful and useful conceptual models addressing important elements of consumer engagement in the literature, none on its own could be used to characterize the diversity of strategies reflected in the current consumer engagement initiatives. The need for such a framework was revealed in our in-depth interviews with AF4Q participants, who suggested that “everyone comes at [consumer engagement] differently,” which contributed to difficulties to “thinking through … and bring[ing] some cohesion to [the consumer engagement piece]” (Alexander et al. 2009).
In this article we present a conceptual framework that distills the multifaceted concept of consumer engagement in health and health care into the critical analytic components that characterize community-based efforts to improve consumer engagement and help stimulate productive discussions about advancing health and health care through consumer engagement initiatives. After a brief discussion of our data and methods, we examine the meaning of the term “consumer engagement” and related concepts; offer a conceptual framework to typify and differentiate initiatives and to serve as a foundation for broad thinking and debate about the consumer engagement universe; and apply the framework to one community's consumer engagement initiative.
Data and Methods
In January 2009, we searched and reviewed the health services literature available through the PubMed database for existing conceptual models of consumer engagement in health. The phrase “consumer engagement” generated citations for twelve papers (Barraclough and Birch 2006; Brown et al. 2005; Draper and Claxton 2004; Fronstin 2008; Hibbard 2009b; Hurley et al. 2009; Jones et al. 2006; Lee and Hoo 2006; Maillet and Halterman 2004; Northrop, Pittam, and Caan 2008; Rolfe, Sheehan, and Davidson 2008; Shaller 2007), of which only three (Hibbard 2009b; Hurley et al. 2009; Shaller 2007) discussed multiple aspects of consumer engagement, and only one discussed a conceptual framework that linked higher patient “activation” to the performance of more “productive health behaviors” (Hibbard 2009b, 10).
We then turned to the gray literature, using Google to search for the phrase “‘consumer engagement’ definition health,” reviewing the first twenty web links, of which only Gruman and colleagues’ 2009 report, “A New Definition of Patient Engagement: What Is Engagement and Why Is It Important?” was useful. It alone provided a definition and a framework of consumer engagement behaviors based on a review of the literature on “patient engagement” and on environmental scans of organizations and recent conferences likely to address patient engagement.
These materials showed consumer engagement to be multidimensional and fundamentally about individual behavior change. We used Gruman and colleagues’ (2009) and Hibbard's (2009a, 2009b) papers as the basis for our consumer engagement framework. These two papers suggested two core dimensions of consumer engagement: (1) behavioral (e.g., what do engaged individuals do?), represented by four types of behaviors (consumer/consumeristic, patient/medical encounter, self-management, healthy), and (2) cognitive (e.g., what are individuals’ capacity and motivation to change?), represented by activation. We built our framework from these elements and expanded it with additional, targeted review of the literature about how activation and behaviors relate to one another and how individual change is related to community change (which is the ultimate goal of AF4Q).
First, we investigated Hibbard's patient activation concept more closely, reviewing the six articles generated from a new PubMed search of “patient activation” and “Hibbard” (Hibbard and Cunningham 2008; Hibbard et al. 2004, 2005, 2007a, 2007b; Mosen et al. 2007). Second, we identified and reviewed key models of behavior change in the social sciences for how the behavioral and cognitive dimensions of consumer engagement were treated. We began by searching PubMed with “‘behavior change’ models literature review,” which resulted in 114 articles, reduced to 65 by eliminating those published before 2000. Mittler reviewed the abstracts for the 65 papers, reading in full the one systematic review of models used in health behavior research (Painter et al. 2008). This paper identified five main theories based on their use: the transtheoretical model, social cognitive theory, health belief model, theory of reasoned action / planned behavior, and social networks / social support theory. We then investigated these five models, plus the microeconomic consumer choice theory, using textbooks and handbooks in which the literature is synthesized and distilled (Culyer and Newhouse 2000; Fiske, Gilbert, and Lindzey 2010; Glanz, Rimer, and Viswanath 2008; Schumaker, Ockene, and Riekert 2009). Martsolf wrote one-page overviews of these models, highlighting their logic, key variables, and use and findings to date. Then Mittler reviewed and further clarified these summaries, using seminal references identified as those that established and/or reviewed the theories and models being investigated.
Although Mittler was responsible for developing the framework, all of us discussed the framework's logic, variables, linkages, and scope during the first year of its development. We debated the framework's gaps, clarity, and level of detail, and our desire to develop a parsimonious framework for classifying the wide array of consumer engagement behaviors. Throughout the process, we also drew on knowledge gained from our interviews of AF4Q community members about their consumer engagement strategies and on other program materials, such as the AF4Q communities’ reports to the national program office and the Robert Wood Johnson Foundation (Scanlon et al. 2012).
Recognizing the lack of group- and community-level elements in the six initial models explored and based on Mittler's subsequent reading of eight review chapters (Glanz and Rimer 2008; Glanz and Schwartz 2008; Heaney and Israel 2008; Kegeler and Glanz 2008; McAlister, Perry, and Parcel 2008; Minkler, Wallerstein, and Wilson 2008; Sallis, Owen, and Fisher 2008; Viswanath 2008) about interpersonal, group, and community theories and evidence, and Painter and colleagues’ (2008) review of the model's use, we settled on the social ecological model. We decided to use this nested, multilevel model to structure the overall framework because of its ability to accommodate the universe of consumer intervention approaches. To better understand the group and community levels and dynamics, we reviewed the social cognitive, social network, and support theories and also read several updated syntheses of the social-psychology literature (Fiske 2010; Leary 2010; Swann and Bosson 2010; Yzerbyt and Demoulin 2010) and other selected, social science treatments of these levels (Helman 2001; Herrmann-Pillath 2010; Kleinman 1980; Kleinman and Hall-Clifford 2009; Lynch et al. 2002; Parsons 1951; Roblin and Becker 2009).
To answer questions as they arose and to keep abreast of new developments, we periodically searched for new reviews in PubMed and Google Scholar, using the terms “‘consumer engagement’ health” with “review” or “model,” and “behavior change” with “review.” In addition, when looking up seminal papers or searching for answers to questions as they arose, we used a “snowballing” process, looking at references that appeared in search engines’ “article cited by” and “articles like these” features, in order to identify relevant new or updated publications. Here we cite the most recent updated versions of materials wherever possible.
We “tested” and improved the framework by applying it to different types of engagement activities being implemented by AF4Q participants. We further refined the framework using feedback on the schematic and draft explanation by the other AF4Q evaluation investigators, several AF4Q consumer engagement leaders, and ultimately from reviewers during the publication process. Finally, we applied the framework to one AF4Q community, Washington State's Puget Sound Health Alliance, which had many consumer engagement activities of different scope, used a variety of approaches, and targeted different engaged behaviors. Its consumer engagement program in 2008/2009 provided a good opportunity to show how the framework could be used to help make sense of existing consumer engagement initiatives by classifying the program's activities. Information about the Puget Sound Health Alliance's current program can be found on its website: http://www.pugetsoundhealthalliance.org.
Consumer Engagement: What Are We Talking About?
Community members who are developing and operating consumer engagement programs have many definitions of consumer engagement (Hurley et al. 2009), ranging from “educating the public about quality and healthcare initiatives and overall health and wellness” to “involving consumers in the process … [of] deciding [about care]” to “empower[ing] people to be their own personal health care managers” (Alexander et al. 2009). Our review of the literature, however, revealed few explicit definitions and several different conceptualizations. Later we discuss the different meanings of the terms “consumer” and “engagement” and conclude with a suggested vocabulary meant to distinguish between the two key dimensions of consumer engagement that emerged: the capacity and motivation to act and the actual behaviors. Most important, we call for a clearer articulation of what these or other shorthand terms mean when used to characterize consumer engagement.
Consumer versus Patient
As we mentioned earlier, clear definitions of the “consumer” component of “consumer engagement” were scarce. “Consumer” most often referred to the dictionary definition of “one that utilizes economic goods” (Merriam-Webster 2012b), but its contextual use implied an economics-based depiction of a consumer as an individual who makes autonomous, informed, rational decisions that maximize his or her individual welfare (Culyer and Newhouse 2000). This contrasts with the historical interpretation of “patient” as one who relies on his or her providers to make health-related decisions on his or her behalf (Brody 1980; Charles, Gafni, and Whelan 1997; Parsons 1951).
Some definitions differentiated consumers from patients. Whereas Longo (2005) distinguished a consumer from a patient based on whether the individual was healthy or sick, Gruman and colleagues (2010, 351) labeled individuals as consumers when they were “making decisions about obtaining health care—choosing among plans, providers and hospitals, for example,” and applied the term “patients” when individuals were “interacting directly with health care providers and services about personal health concerns.”
Engagement: Individual Capacity and Motivation to Act versus Acting
We found that the “engagement” component of “consumer engagement” was used unsystematically to describe a person's “emotional involvement and commitment” to his or her health and role in health care and/or to the act of being “involved in an activity” (Merriam-Webster 2012c), including behavior related to one's health and health care. Examples of the former describe engaged consumers as individuals “empowered to be in control of their care” (Leape et al. 2009, 426) or “valu[ing] clinical quality, insist[ing] on shared decision-making, and accept[ing] the responsibility to bear results of choosing lower-quality treatment options” (Schaeffer and McMurtry 2004, 119). Examples of the latter refer to behaviors to manage one's health and health care, such as participating in “fully” shared decisions about treatments (Gruman et al. 2010; Leape et al. 2009), including discussing “various lifestyle choices associated with … treatment” (Maillet and Halterman 2004, 1); undertaking “responsible individual behaviors … [such as] selecting competent physicians and safe hospitals [and] interacting successfully with health providers and institutions” (Shaller 2007, 309); and talking about “actions individuals must take to obtain the greatest benefit from the health care services available to them” (Gruman et al. 2010, 351). Although these two dimensions are related, they are not the same: the former describes an individual's capacity to act and his or her degree of motivation (cognitive and emotional elements), and the latter is about behavior.
Engagement as Individual Capacity and Motivation
When engagement is used to characterize an individual's capacity and commitment to taking an active role in his or her own health and health care, those who are more “engaged” are perceived as being more emotionally invested and dedicated to taking charge of their health (Hibbard and Mahoney 2010), as well as being more motivated, willing, and able to undertake a constructive role in their health and care. In this context, an individual's degree of engagement is expected to affect the likelihood that he or she will perform engaged behaviors, although this use of the term “engagement” does not refer to any particular behavior.
This dimension of engagement has come to be synonymous with the term “patient activation,” which emerged primarily from the work of Judith Hibbard and her colleagues (e.g., Hibbard and Cunningham 2008; Hibbard et al. 2004). Hibbard and Cunningham (2008, 2) defined patient activation as “people's ability and willingness to take on the role of managing their health and health care.” This refers not only to people's technical capacity to be active but also to how much they are “disposed to action” (Merriam-Webster 2012a). People's degree of activation is thus related to their personal beliefs, attitudes, knowledge, confidence, and positive feelings toward their role in their own health and health care (Hibbard and Cunningham 2008; Hibbard and Mahoney 2010), but it is not equivalent to any one of these attributes. Rather, “activation” is a separate quality reflecting one's overall predilection to engage in certain behaviors.
Engagement as a Set of Behaviors
Some scholars define consumer engagement as an individual's performance of specific behaviors. Gruman and colleagues’ (2009) typology classifies behaviors into two overarching domains: (1) “managing health” behaviors, which is both the self-management of chronic disease and the adoption of healthy behaviors, and (2) “managing health care” behaviors, which can be both patient and “consumeristic” behaviors. We modified this typology by renaming “patient behaviors” as “health care encounter behaviors” to make clear that this category refers to individuals’ interactions with health care providers. We also renamed “consumeristic behaviors” as “shopping behaviors.” The term “shopping”—“examin[ing] goods or services with the intent to buy” (Merriam-Webster 2012d)—provides a more precise description of the type of behavior being referenced and thus avoids interpreting “consumer” as referring to both a person and a behavior type. Finally, we described the difference between self-management and healthy behaviors.
Self-Management Behaviors
Self-management behaviors are the “day-to-day tasks an individual must undertake to control or reduce the impact of disease on physical health status” (Clark et al. 1991, 5). These behaviors, such as diabetics monitoring their blood sugar, are believed either to help prevent the deterioration of health or to improve the well-being of individuals with chronic conditions. For conceptual clarity, we classified behaviors related to an individual's acute or chronic illness as “self-management.” For example, a person with diabetes engaging in healthy eating to control his or her blood sugar is undertaking a self-management behavior, whereas healthy eating by an individual with no chronic illnesses would be classified as a healthy behavior.
Healthy Behaviors
Healthy behaviors are undertaken by individuals to maintain their health and well-being and to prevent the development of illness. These behaviors include healthy eating, not smoking or stopping smoking, and getting regular exercise, all of which are known to improve health (Schumaker, Ockene, and Riekert 2009).
Health Care Encounter Behaviors
Health care encounter behaviors refer to activities that individuals perform to become more effective self-advocates with their health care providers. Patients engaging in such behaviors ask their providers more and better-informed questions about their care, more effectively communicate their health goals and wishes to their providers, and participate in decisions about their care.
Shopping Behaviors
Shopping behaviors refer to the activities that individuals perform in order to become more effective purchasers of health care. These behaviors include using quality reports to choose a physician, hospital, or health plan, as well as seeking out and using information to help select among treatment options.
In Sum: Proposed Vocabulary for Consumer Engagement
In this section we suggest some terms to help differentiate the meanings of “consumer engagement” and to communicate the intended meanings more clearly. These suggestions are based on the terms just defined. Strict adherence to a particular set of terms is not required to advance our understanding of consumer engagement, so regardless of the terms chosen, we are arguing for a clearer articulation of assumptions and meanings in developing, assessing, and discussing consumer engagement interventions.
To differentiate between the two main dimensions of engagement just described, we propose that the degree to which individuals (i.e., “patients” or “consumers”) are inclined to take an active role in managing their health and health care be referred to as the degree of “activation.” Our tracking of the consumer engagement field suggests that “activation” (coined by Hibbard and colleagues) is becoming the favored term. We propose that “engaged behaviors” be used as a general term to refer to actions to manage health and health care and that self-management, healthy, health care encounter, and shopping behaviors be used to describe the four general kinds of engaged behavioral domains defined earlier.
When selecting a term to represent the individual (or individuals as a class), neither “consumer” nor “patient” is objectively superior to the other. As described earlier, the normative interpretations of each of these terms reflect different values and assumptions regarding an individual's role in his or her health and health care. But the language is continuously evolving, and so even these interpretations are not absolute or universal. For example, discussions about promoting individuals’ greater involvement in their care plans and treatment decisions often refer to individuals as “patients.” However, the intent of this shared decision-making movement is for individuals to partner with providers, thereby contradicting the common meaning of “patient” as a person who relies on the provider to make treatment decisions on his or her behalf and passively accepts the provider's instructions. Thus, we contend that it is very important to be mindful of the language used to communicate about “consumer engagement” concepts, especially by those outside academic circles, whose assumptions may vary but may not be communicated (e.g., in an office visit, in an issue brief). Overall, we found that the literature and the conversations we conducted for the AF4Q evaluation implicitly reflected Gruman and colleagues’ (2010) distinctions. “Patient” was used when an individual was interacting directly with health care providers (and provider entities) about personal health concerns, and “consumer” was used when an individual was making decisions about obtaining health care. We endorse following this trend and do so for the remainder of this article.
A Framework for Consumer Engagement
We found no single conceptual model or framework that satisfactorily accounted for the key dimensions of consumer engagement; depicted individual, group, and community dynamics; and was applicable to all four behavior types (self-management, health care encounter, shopping, and healthy). First, most of the existing models addressing individual health behavior change do not consider group and community elements or a variety of behavior types, even though this is important for classifying and evaluating programs like AF4Q that involve multiple and diverse consumer engagement interventions (Glanz, Rimer, and Viswanath 2008; Painter et al. 2008). The models of individual behavior, which focus almost exclusively on intrapersonal dimensions, are the health belief model, the microeconomic consumer choice theory, the theory of planned behavior, and the transtheoretical model (table 1).
TABLE 1.
Selected Behavior Change Models
| Model | Description | Selected Citations |
|---|---|---|
| Focus on the Individual | ||
| Health belief model | Originally developed to predict adoption of preventive behaviors, this model posits that an individual's decision to act stems from people's perceptions of (1) the severity of the threat to their health, (2) their susceptibility to this threat, and (3) the benefits of and barriers to action. | Janz and Becker 1984 |
| Microeconomic consumer choice theory | The microeconomic theory describes how individual consumers make consumption choices under income and other constraints, given their preferences and the opportunity costs. | Kolstad and Chernew 2009 |
| Theory of planned behavior/ theory of reasoned action | The theory of planned behavior is an extension of the theory of reasoned action. It adds the individual's control over the behavior to the individual's attitude toward the behavior, and the norms for behavior as determinants of an individual's intent to perform a behavior. This intent is identified as the mediator for all the other individual attributes and influences. | Ajzen 1991; Armitage and Conner 1999; Fishbein 1979 |
| Transtheoretical model | This model describes five stages of change: precontemplation, contemplation, preparation, action, and maintenance of behaviors. Individual change processes occur within each stage. | Prochaska et al. 1994; Prochaska, Redding, and Evers 2008 |
| Focus on Interactions with People and Environment | ||
| Social cognitive theory | This theory posits that human behavior is learned through social interactions. Individual beliefs about the ability to perform behaviors (self-efficacy), control behaviors (self-regulation), and expected outcomes are shaped by interactions in social environment, and vice versa (reciprocal determinism). | Bandura 1986, 2004 |
| Social network theory and social support | Social network theory focuses on how the characteristics of interpersonal relationships, such as number and degree of reciprocity, influence outcomes like health behaviors. Social support theories also focus on interpersonal relationships and how these relationships provide support that is protective or detrimental to health. | Christakis and Fowler 2012; Heaney and Israel 2008; Uchino et al. 2012 |
| Social ecological model | This model focuses on the relationship between the individual and the environment. While individuals are responsible for their own lifestyle choices, behavior is largely determined by the context of the social environment (e.g., community norms, policy, regulation). | Bronfenbrenner 1979; Richard, Gauvin, and Raine 2011 |
The health belief model explains why large numbers of individuals do not obtain beneficial health services, such as preventive screenings (Janz and Becker 1984). It assumes that individuals value their health very highly and that their decision to act is based on their perceptions of the gravity of the threat to their health and the benefits and costs of action (table 1). But it does not delineate the process for individual decision making and does not take into account that people do not always value health above almost everything else (e.g., smoking to “fit in” with one's friends). The microeconomic consumer choice theory is also based on an individual's cost-benefit assessment of the expected value of acting in a particular way, but the influences on the assessment of value are defined rather broadly as one's “preferences” (Kolstad and Chernew 2009).
The transtheoretical model (Prochaska et al. 1994) posits that individuals progress through five stages while considering, undertaking, and possibly maintaining a new behavior: precontemplation, contemplation, and preparation (stages 1 through 3); taking action (stage 4); and maintaining the behavior (stage 5). Neither this model nor the theory of planned behavior depicts the relationships with contextual influences. The theory of planned behavior (Ajzen 1991; Armitage and Conner 1999), which is an extension of the theory of reasoned action (Fishbein 1979), posits that a person's intention to perform a behavior drives his or her actions and that a person's beliefs about behavioral outcomes, behavior norms, and perceptions of his or her control over the behavior converge to create this intent (table 1). Although this model includes the role of normative beliefs, it does not go beyond this to connect individual attributes to broader contextual factors.
Models based on social support and network theory, social cognitive theory, and social ecological theory emphasize the influence of interpersonal, group and/or community dimensions on behavior (table 1). The first two theories are built on social learning. Models of social support and networks associate characteristics of relationships (e.g., closeness, number of relationships) with behaviors (Berkman and Kawachi 2000; Christakis and Fowler 2012; Uchino et al. 2012); models based on social cognitive theory also account for interpersonal factors but place a greater emphasis on the interaction between individual factors (most notably, self-efficacy, which was developed as part of this theory) and the social environment (Bandura 1986, 2004). Finally, while the social ecological model clearly illustrates that multiple levels of factors influence health behaviors, nesting individuals in their intrapersonal environment and then within the larger contexts of community and even society, it does not depict individual mechanisms (Bronfenbrenner 1979; Richard, Gauvin, and Raine 2011).
None of these models alone served our need to classify and understand the wide variety of consumer engagement interventions with which the AF4Q communities were experimenting (e.g., directly or indirectly targeting individuals, targeting different sets of behaviors, targeting different stages of “readiness”). However, to develop a framework for such varied consumer engagement programs, which we titled the Engaging Consumers in Health and Health Care in Communities (ECHC) framework, we drew collectively on these existing models. Before examining the ECHC's particulars, we provide a brief overview of the framework's structure.
The ECHC's Structure
The overall structure of the ECHC framework (figure 1) is drawn from social ecology, which posits that factors outside the individual influence his or her behavior (Bronfenbrenner 1979). That is, individuals are nested within groups, which are embedded in the broader community. We selected this multilevel structure because consumer engagement interventions can take group or population approaches, and contextual factors influence individual behavior and the success of interventions. The ECHC's structure of concentric circles shows that individuals, groups, and communities may influence one another at any point in time, but not necessarily in a linear fashion or with equal importance.
FIGURE 1.
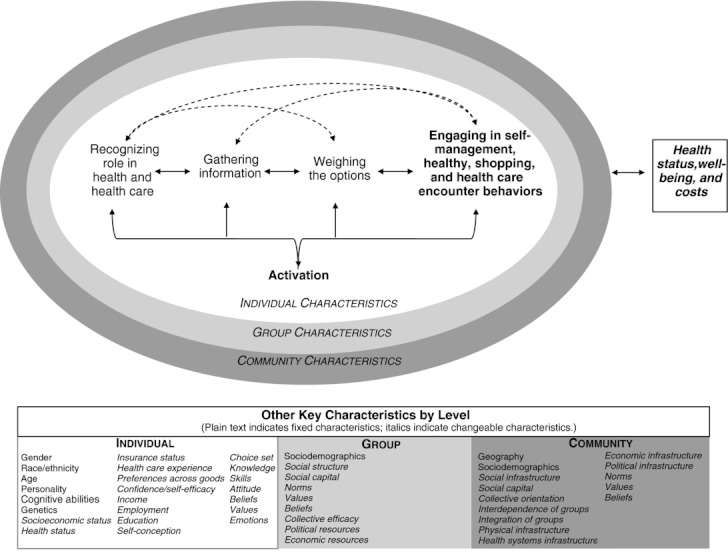
The Engaging Consumers in Health and Health Care in Communities (ECHC) framework.
The first level is concerned with individuals’ engagement in their health and health care and is the most detailed because, as we noted earlier, consumer engagement is fundamentally about individual behaviors. Although groups and communities can have unique identities and act collectively, most consumer engagement is ultimately acted out by individuals (Hibbard 2009a). The surrounding group level focuses on individuals’ interactions with and influences on one another (i.e., interpersonal relationships and behaviors). Thus, in the ECHC framework, the term “group” refers to relationships among two or more individuals whose relationship may be based, for example, on friendship, family, religion, ethnicity, exchange of services, or employment.1 The community level represents the larger geographic space, consisting of the physical, economic, sociocultural, and political structures in which individuals (and the groups with which they identify) navigate (Buttimer 1969; Hunter 1975). Although some literature uses the term “community” to describe a large group of people with a common attribute (e.g., the breast cancer community), the ECHC framework considers these collections of people as groups. Finally, at the bottom of the framework we list those characteristics identified in the literature as likely influencing consumer engagement within and across levels.
Next we examine more closely each of the framework's three levels and the relationships within and among them. Our goal was to develop a framework for classifying consumer engagement interventions, specifically interventions sponsored by or put in place by a community's multistakeholder entities, to facilitate dialogue about their logic and role. Here, however, we cannot present an exhaustive set of specific hypotheses about how any or all of a level's characteristics could impact an individual's engagement.
Individual Level
At the center of the ECHC framework is an adapted version of the transtheoretical model of individual behavior change (Prochaska 2008; Prochaska et al. 1994). The transtheoretical model is not, however, a theory but a model that reflects a common, but not universal (e.g., see Herzog 2010), conceptualization of behavior change as an individual's progression through a series of stages and processes that can be targeted by interventions (Prochaska 2008; Prochaska et al. 1994). For example, in the precontemplation and contemplation stages, a key process may be becoming increasingly aware of how a particular behavior affects an individual's health and well-being (Prochaska et al. 1994). Because of its widespread use in the literature (Glanz, Rimer, and Viswanath 2008; Painter et al. 2008) and its intuitive, staged approach (Munro et al. 2007; Prochaska, Redding, and Evers 2008), we chose this model as a starting point, modifying it to incorporate the role of activation and to emphasize the dynamic nature and varied time horizon of change.
The original transtheoretical model consists of five stages of change: (1) precontemplation (no change intended within six months), (2) contemplation (change intended within next six months), (3) preparation (change intended within a month), (4) action (already has made changes), and (5) maintenance (sustaining change beyond six months) (Prochaska et al. 1994); the time frames reflect the original focus on using the model to design interventions to guide the planned behavior change. The ECHC framework specifies activation as a distinct characteristic that influences an individual's decision-making process and actions taken to change his or her behavior. This decision-making process has four stages: (1) recognizing one's role in health and health care, (2) gathering information, (3) weighing the options, and (4) engaging in healthy, self-management, shopping, or health care encounter behaviors. In figure 1, the two core conceptual dimensions of consumer engagement discussed earlier in this article—activation and one or more of the four behavior types—are denoted in boldface. In addition, we eliminated any reference to specific time frames and added bidirectional links to better reflect the dynamic nature of decision making and behaviors over time. For various reasons, individuals may implicitly or explicitly (re)consider their behaviors.
To improve activation and the performance of engaged behaviors, individuals must be aware of, acknowledge, and embrace the idea that there is room to improve their own health and that they have an important, active role in doing so. This step primarily concerns individuals’ self-perception of their role and ability to be engaged in their health and health care (Bandura 1986, 2004; Prochaska et al. 1994; Swann and Bosson 2010; Terry 2005). Recognizing their role provides motivation to pursue behavior change, and how individuals perceive this role affects their motivation to pursue behavior change, including the scope and types of information sought. Individuals’ effort in looking for information and where they seek it can vary greatly and include searching the Internet, asking friends or family for advice, reading pamphlets in their provider's office or at the pharmacy, and talking to their provider about their health and health care. The information gathered and how it is interpreted can further shape how an individual perceives his or her role.
The next step is weighing the options, or understanding, assessing, and synthesizing information to evaluate the direct or indirect benefits and costs of engagement alternatives. In economics, this process is known as estimating trade-offs to maximize utility, or assessing the “opportunity costs” when choosing one's behavior (Culyer and Newhouse 2000). In the transtheoretical model of behavioral change, this concept is referred to as individuals’ “decisional balance sheet” of pros and cons (Prochaska et al. 1994). Weighing the options may be executed as an intrinsic, unconscious process or as one that is more explicit and deliberate. If individuals conclude that the benefits of change sufficiently outweigh the costs, they will be expected to perform and maintain the engaged behaviors. Individuals’ choosing to take (or not to take) action may affect their health and well-being over time. Finally, the framework indicates that an individual's degree of activation is associated with the behavior change and that his or her degree of activation can change over time (Fowles et al. 2009; Greene and Hibbard 2011; Harvey et al. 2012; Hibbard 2009b; Hibbard et al. 2007a; Mosen et al. 2007; Remmers et al. 2009).
The ECHC framework assumes that individuals may progress (or regress) among these stages at different rates. Individuals have different capacities, and different constraints on their capacities, that affect motivation and movement. For example, a diagnosis of diabetes may prompt individuals to rethink their role in managing their own health and instigate information gathering about diabetes-specific management recommendations. However, these same people may not view themselves as active “shoppers” for high-quality providers and may not look for information about their provider's record on diabetes care. Or they may not have “real” choices because of insurance restrictions or because other providers are not taking new patients. Since we designed our framework to accommodate these variations, defined time periods are not assigned to a stage.
In addition, although we presented our framework linearly, we recognize that the consumer engagement process is dynamic (Hibbard and Mahoney 2010; Prochaska 2008). The bidirectional arrows indicate the potential to progress or regress in linear and nonlinear ways over time. For example, an individual who exercises regularly may move from taking action to gathering information to understanding better why he or she has not seen a change in weight or decrease in blood pressure. In another case, an individual may believe that the costs associated with using performance reports and switching physicians are prohibitively high but may revisit this calculus when he or she moves to another town or his or her physician retires.
While the process is dynamic, individuals may pause at any point. For instance, individuals may gather information about one of their providers or possible treatments but stall and do nothing because they find the information hard to understand and believe that the additional effort to comprehend the information (e.g., time, potential embarrassment in seeking help, likely relevance) outweighs expected benefits. Or an individual who did not lose weight despite exercising may not return to gather more information but move back to role recognition because this feedback altered his or her self-conception as a confident, apt manager of his or her own health. One factor affecting progress is the source of an individual's motivation to change. Individual change that is more intrinsically than extrinsically motivated is thought to be more powerful, especially when people are experiencing stress, because the intention and motivation is grounded in their own values and interests, not in others’ (Anderson and Funnell 2010; Ryan and Deci 2000).
As indicated by our examples, static traits like age, gender, personality, cognitive abilities, race, and ethnicity and more variable states such as health status, income, socioeconomic status, self-efficacy, emotions, experiences, self-conception, degree of self-regulation, knowledge, awareness of choices, skills, and beliefs and values can influence the engagement process and degree of engagement (Hibbard and Mahoney 2010; IOM 2001; Protheroe, Nutbeam, and Rowlands 2009; Rosen, Anell, and Hjortsberg 2001; Schumaker, Ockene, and Riekert 2009; Swann and Bosson 2010).
Group Level
Group membership affects access to potentially beneficial information, social support, and material resources (Berkman and Kawachi 2000; Granovetter 1973; Hermann-Pillath 2010). Most individuals are members of social networks and psychologically identify with one or more groups, each of which has its own identity and culture (Charles et al. 2006; Leary 2010; Tajfel and Turner 1979). Group culture, which is made up of the values, attitudes, and beliefs that are learned and transmitted among group members, is expressed through implicit and explicit rules that regulate and reinforce appropriate, socially sanctioned behavior and punish unacceptable displays of values and beliefs (Kreuter and Haughton 2006; Leary 2010; Link and Phalen 2001). This ongoing socialization can impede or enhance consumer engagement, depending on how consumer engagement in health and health care is defined and valued (Swann and Bosson 2010).
For example, some groups of consumers might not trust specific sources of information or might believe it is disrespectful to question providers about treatment (Cutilli 2010; Hesse et al. 2005; Kleinman 1980). Members of these groups also may disregard institutionally sponsored campaign materials encouraging people to ask their providers specific questions about their health care or prevent a family member from asking questions during a visit with a provider. Alternatively, groups that strongly value being “informed” or “not pushed around” may be positively affected by the same campaign efforts, if the campaign affirms these core elements of their identity. Instead of automatically discarding these materials, members of these groups may bring them to their next office visit for easy reference. For their part, providers may adhere to and reinforce nonactivated consumer roles in health care encounters, for example, by repeatedly interrupting patients and outwardly dismissing their concerns, or they may affirm activated roles by soliciting patients’ input in a collaborative manner and making them aware of any options (Dy and Purnell 2012; Emanuel and Emanuel 1992).
A group's influence on a consumer's engagement is likely to be greater if a member strongly identifies with, is attached to, and is embedded in the group; the group has a strong identity; and it has a high degree of cohesiveness and interdependence (Berkman and Kawachi 2000; Friedkin 2004; Lau 1989; Swann and Bosson 2010). For example, Ahern and colleagues (2009) found that the same high degree of collective efficacy was associated with more smoking in neighborhoods having permissive smoking norms and with less smoking in neighborhoods having strong antismoking norms. The forces that prevail may depend on the issue and situation. For example, if a minority woman with diabetes identifies with her ethnic group more strongly than she does as a diabetic, she may hesitate to discuss alternative medicine treatments with her mainstream medical providers (Graham et al. 2005; Shelley et al. 2009), even if others in her diabetes support group encourage this discussion.
Other group-level characteristics that can shape consumer engagement are sociodemographic makeup, integration into mainstream culture, and economic, political, and social2 resources (Fiske 2010; Link and Phalen 2001; Reitz and Sklar 1997; Yzerbyt and Demoulin 2010).
Community Level
A community's economic, political, social, and physical infrastructures influence (1) the relevance and role of consumer engagement in improving the community's health and health care; (2) the will and ability to take collective action with respect to consumer engagement; and (3) the legitimate, acceptable options for consumer engagement initiatives in the community. Although scholars and practitioners disagree on the relative influence of these factors (Helman 2001; Lynch et al. 2002; McLeroy et al. 1988; Roblin and Becker 2009), powerful individuals and entities can have tremendous influence over community agendas, including how resources are distributed (Fiske 2010; Gradstein and Schiff 2006). Context is important to understanding the opportunities for and characteristics of community consumer engagement initiatives (Hibbard 2009a, 2009b; Larson et al. 2009).
A community's economic infrastructure affects both the total amount of resources available for improving a community's health and the locus of power. For example, if a few large purchasers have significant economic power in a community's health care sector, they may use this power to compel providers to supply performance data for their employees to use in choosing providers or for the employer to use in deciding payments. The purchasers may also pursue this performance-reporting agenda, regardless of the providers’ readiness. In turn, providers may use their social power to persuade patients to maintain their existing provider relationships, despite any purported quality differences.
Likewise, a community's “mainstream culture” represents historically powerful groups’ values and beliefs, such as the role of collectivism versus individualism in community life or the role of folk medicine versus Western medicine. The importance of the mainstream culture is its power to set norms that influence behavior, as observed in the evolution of smoking behavior and the treatment of depression (Kleinman and Hall-Clifford 2009; Stuber, Meyer, and Link 2008). Its influence may vary with the matter being considered and how embedded a group is in the mainstream (Swann and Bosson 2010; Wolff et al. 2010). Finally, geography and physical infrastructure affect consumer engagement by shaping the connections among people, groups, and resources (Sampson, Morenoff, and Gannon-Rowley 2002; Williams and Collins 2001). Geography affects access to resources that can reduce the costs of engagement like social support, healthy food, safe places to exercise, and the accessibility and availability of high-quality providers (Cohen, Inagami, and Finch 2008; Larson, Story, and Nelson 2009; Nemet and Bailey 2000; Stanley, Cantor, and Guarnaccia 2008).
Applying the Framework: An Example from the Aligning Forces for Quality (AF4Q) Initiative
In this section, we show how policymakers and practitioners can “make sense” of existing consumer engagement initiatives by applying the ECHC framework to a real program. Our intent is to show how the framework can be used to systematically classify different program elements that can contribute to discussions of the purpose, value, fit, and realistic potential of consumer engagement initiatives in particular contexts.
The case is Washington State's Puget Sound Health Alliance's (“the Alliance”) consumer engagement program in 2008/2009. It is one of the communities participating in the Aligning Forces for Quality (AF4Q) program, which provides resources to grantee communities to develop localized, multistakeholder, communitywide efforts to improve health care quality and overall health through several mechanisms, including improving consumer engagement (Painter and Lavizzo-Mourey 2008). We chose to apply the ECHC framework to this program because it included several activities with varied scopes, mechanisms, and purposes and thus provided a good test of the framework's utility in effectively understanding complex consumer engagement initiatives and generating a productive dialogue among policymakers and practitioners.
We begin with a brief description of the Alliance's four program activities in 2008/2009, followed by our examination of the program by the ECHC framework's targeted behaviors, individual stages and processes, and levels (i.e., individual, group, and community).
Overview of Activities
In 2008/2009 the Alliance's four main consumer engagement activities were (1) a public, communitywide, Internet-based performance report on physicians, hospitals, and health plans known as the Community Checkup; (2) a monthly health column by a local physician for use in newspapers and local organizations’ websites and newsletters; (3) Rx for Information, in which physicians in a small number of practices wrote “prescriptions” for patients with diabetes, congestive heart failure, or depression to go to the library to learn about their conditions from trained librarians; and (4) Healthy Incentives, one public employer's employee incentive program to engage in healthy and shopping behaviors. Table 2 provides additional details.
TABLE 2.
Description of Puget Sound Health Alliance's Consumer Engagement Activities in 2008–2009
| Community Checkup | Community Checkup is an interactive, web-based public report of provider and health plan performance. Users can search for quality data on managing chronic disease, taking preventive care, and using medications and technology at the clinic, group, and hospital levels. Links to additional resources and tools teaching quality care, managing one's health or chronic condition, and effectively communicating with providers are included. Some information was developed or modified by a consumer engagement committee. |
| Health column by local physician | Health columns by a local family physician appeared on the Alliance's website between 2009 and 2010. Topics included the use and interpretation of quality reports, questions consumers should ask about treatment options, and tips on managing health or chronic conditions. To facilitate widespread dissemination from various communication outlets, the Alliance considered multiple literacy levels and various aspects of column subjects. |
| Rx for Information | Rx for Information encouraged consumers with diabetes, heart disease, and depression to obtain disease-specific information in order to become better “self-managers.” Physicians gave patients “prescriptions” to go to the local library. The consumers met with librarians who helped them find information related to chronic condition(s), including one-page self-management checklists, the Community Checkup report, and health literacy brochures. Although the program formally ended in 2009, links to library resources still appear on the Community Checkup website. |
| Healthy Incentives | Healthy Incentives is King County's effort to engage its 19,000 employees and eligible beneficiaries in healthy behaviors by providing financial incentives. When a county employee meets specific nutrition, exercise, stress management, and weight management goals, he or she receives reduced out-of-pocket costs for care under the county's health insurance plan. In 2009, 91 percent of employees and 86 percent of all eligible individuals participated in Healthy Incentives (Seven 2009). |
Source: Authors’ analysis.
Analysis by Engaged Behavior Type
The four activities tackle multiple types of engaged behavior (figure 2): three address healthy behaviors (Community Checkup, health columns, and Healthy Incentives); three speak to self-management and shopping behaviors (Community Checkup, health columns, and Rx for Information); and two take up health care encounter behaviors (Community Checkup and health columns). The activities do not emphasize engaged behaviors equally. For example, although the Community Checkup is predominantly focused on shopping behaviors (i.e., comparing and selecting providers), this report could influence the other three behavior types by increasing awareness of what is involved in preventing and managing chronic illnesses and stimulating discussions with providers. The heart of Rx for Information is improving self-management behaviors by connecting individuals with information about their conditions, but this activity also may encourage discussion of their care with their physicians (health care encounter behavior) or comparison of providers’ performance (shopping behavior).
FIGURE 2.
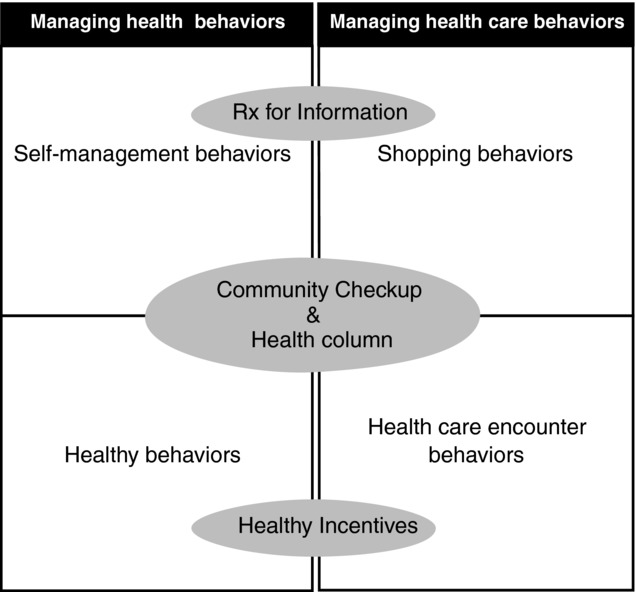
Classification of Puget Sound Health Alliance's consumer engagement program activities by consumer behavior type, 2008–2009.
Source: Authors’ analysis.
Our review of this classification of activity by type generated several questions that the Alliance could use to structure a dialogue about how these activities work individually and together to meet Alliance's goals, including
Is it important to have activities that collectively address all four types of engaged behaviors? How does this fit into the Alliance's overall strategy for consumer engagement? How do these behaviors correspond to the needs of the targeted populations and the community as a whole?
Do certain activities effectively address more than one behavior (e.g., do they provide evidence? Existing infrastructure in the community?) Are activities intended to be independent or interdependent?
Is there evidence of the activities’ potential success? What would success look like in Puget Sound, and how would the Alliance measure it (e.g., more “hits” on the Alliance's website? More employees eligible for the workplace incentive? More individuals reporting that they consult the performance information?)
Analysis by Individual Stage
The Alliance's consumer engagement program as a whole emphasizes the information-gathering stage of the individual engagement process; all four activities address this aspect, and most prioritize it (figure 3). The Community Checkup targets information gathering for selecting providers through its performance metrics and searchable website; the health column offers information related to all four engagement behaviors; Rx for Information tries to make information gathering easier by helping with accessing and using existing resources; and Healthy Incentives offers several opportunities in the workplace to gather general and more individualized information about healthy living in multiple forms (e.g., print resources, Internet, and classes). Finally, the Community Checkup and the health column reflect a cognitive approach to change (i.e., if minds are changed, behavior will follow), whereas Rx for Information and Healthy Incentives take a behavioral approach (i.e., if behavior is changed, beliefs will follow).
FIGURE 3.
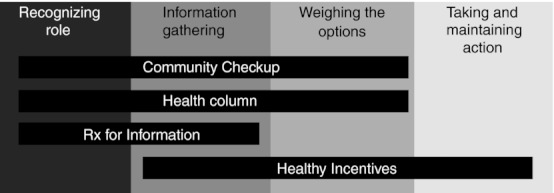
Classification of the Puget Sound Health Alliance's consumer engagement program by individual change process, 2008–2009.
Source: Authors’ analysis.
This description led us to several more questions that could guide our discussion about the program's priorities (e.g., selection of targeted populations) and operating assumptions (e.g., logic, evidence, and expectations for different types of changes), such as
Is it important to serve consumers’ needs across the continuum of change? Does this continuum differ by degree of activation, engaged behavior type, or population (e.g., persons with diabetes, low literacy, no Internet access, no provider choice)?
Are the targeted stages consistent with the target population's capacity and needs? Do these activities adequately consider consumers’ capacity, interest, and willingness to use these resources?
What is known about the approach to and effectiveness of these activities for the target population(s)? Is a cognitive or a behavioral approach better suited to some people or behaviors? Has the timing and sequencing of activities been taken into account?
How will the Alliance know if the activities are working and which activities should be modified, sustained, or eliminated? How do assumptions about how individual change occurs and how the selected interventions work affect expectations for success?
Analysis by Level: Individuals, Groups, and Communities
The scope and reach of the Alliance's consumer engagement elements vary widely. Rx for Information focuses on individual-level change for consumers with specific chronic illnesses through one-on-one interactions with a physician and librarian. This program was implemented in only a few physicians’ practices. However, it was the only activity to explicitly use individual physicians’ influence with consumers, which can be a very powerful force for activating consumers (Becker and Roblin 2008; Cutilli 2010; Hesse et al. 2005). Healthy Incentives targets the individual and group levels, offers individual financial incentives for meeting program goals, and supports new and naturally existing employee subgroups to reinforce activation and engaged behaviors. Examples are on-site support groups for specific health issues (e.g., weight loss) and organized group exercise activities. Focused, narrower efforts like these reach many fewer people and are more costly to operate per consumer. But some would argue that these approaches may more effectively motivate engagement than do the aforementioned broad-audience interventions, since they are more personalized and delivered by proximal, influential sources.
Alternatively, the Community Checkup and health columns take a “top-down,” communitywide approach; they were designed for broad dissemination and use by Puget Sound's consumers, providers, employers, and insurers to create a community environment that encourages activation and engaged behaviors. These activities have the potential to reach large numbers of people but may not be helpful for consumers who, for example, do not already recognize their role, trust the Internet, or know how to interpret performance measures. The Alliance addressed community diversity and population scope in several ways. The health column was made available in multiple lengths and reading levels. The Alliance's websites allow some customization in their search capabilities (e.g., for certain conditions) and provide resources in Spanish, access to a dictionary of health terms, and a link to EthnoMed (http://ethnomed.org), which offers health and medical information on and for various cultural groups in several languages.
The process of categorizing the activities by level raised questions for reviewing the Alliance's strategy for consumer engagement, including the appropriate level(s) for interventions:
Do the activities complement or reinforce one another across levels? What are the trade-offs of taking narrow and/or broad approaches? What is desirable and realistic for this particular community?
Are activities deliberately matched and tailored to level? Are certain activities better suited to certain goals and levels? For example, are activities to improve recognition of an active role more effective at the individual, group, or community level? Is there an optimal order of interventions? What are the comparative advantages of different approaches for the Alliance's targeted populations?
Will the Alliance know if these activities are increasing activation or engaged behaviors? Is it important to establish the cost-effectiveness of any or all of the activities?
In sum, this example illustrates how the ECHC framework can be used to differentiate among consumer engagement program components and to catalyze thinking about the purpose, scope, potential, and fit of these initiatives for specific contexts. While we applied the framework retrospectively, we also think that this framework could have value prospectively when planning consumer engagement interventions. Even though it is not a self-contained analytic tool that produces an optimal solution, it could help policymakers and practitioners successfully develop and assess the fit of their consumer engagement programs by providing a structure for discussion and prompting broad thinking about vital program dimensions.
Discussion
Defining consumer engagement and understanding its role in generating better health and improving the value of health care is especially important as the United States implements health reform and as the number and types of consumer engagement initiatives continue to grow. Employers will provide consumer-directed health plans; Medicare and private employer coalitions will offer consumers reports on hospital quality; cities will implement a broad health education campaign urging individuals to ask their providers about their care, participate in treatment choices, or make healthy behavior choices; and hospitals or community organizations will add small, peer-led classes to help patients manage their chronic diseases (CDC 2010; Fronstin 2010; Galvin et al. 2005; Harris and Buntin 2008; Lorig et al. 2001, 2009; National Patient Safety Foundation 2009).
A key question confronting policymakers and practitioners is how to achieve effective, widespread change. For consumer engagement, consensus on the most effective approaches is still elusive. For example, some stage-specific interventions targeting individuals have been more effective in moving individuals toward more physical exercise than have interventions not matched to stage (Lippke et al. 2010), but others have not been able to do so (Jepson et al. 2010; Van Sluijs, Van Poppel, and Van Mechelen 2004). The relatively scant evidence for community-level change also is mixed. For example, cigarette taxes and smoking bans in workplaces and restaurants have proved effective, but the effect on consumer behavior of environmental changes like the production and wide dissemination of provider performance reports or providing caloric information on fast food and restaurant items is debatable (e.g., Elbel et al. 2009; Harris and Buntin 2008; Ketelaar et al. 2011; Kolstad and Chernew 2009; Roberto et al. 2010).
In addition, the effectiveness of community coalitions in improving health, focused mostly on public health issues, has been “modest at best” (Glanz, Rimer, and Viswanath 2008, 395), with the exception of antismoking efforts (Warner and Mendez 2010). From the existing knowledge, we cannot confidently state that the most prudent strategy to improve engagement is somehow to “scale up” individual interventions or to take a fundamentally different approach targeting broader environmental factors, or some combination of the two. Accordingly, some argue that the implementation of consumer engagement programs may be ahead of the research, suggesting the need for more scientific evidence that consumer engagement initiatives work and can improve the quality of health care (Arnold and Scanlon 2009).
In this article we identified the need for a framework to classify the wide array of consumer engagement interventions to help “make sense” of them as an important step to advancing knowledge of their value in improving the quality of health care through community-based efforts, or otherwise. The Puget Sound Health Alliance example illustrated how applying the framework could advance the field by making policymakers and practitioners aware of the wide range of approaches, providing a structured way to organize interventions retrospectively, and, perhaps prospectively, to help consider how they can meet program goals both individually and collectively.
Acknowledgments
The authors thank their AF4Q evaluation team colleagues and the anonymous reviewers for their thoughtful and valuable feedback during this manuscript's development. This work was supported by a grant from the Robert Wood Johnson Foundation.
Endnotes
Unless noted, we use the terms “group” and “social network” interchangeably in this article because we are primarily concerned with the individual's interactions with other people, ranging from a dyad to a much larger collection of people. In some fields, however, the terms “group” and “social network” carry different connotations, with “group” suggesting a clearly bounded collection of people (e.g., class, geography, religion), whereas “social networks” typically cut across these groups (Berkman and Kawachi 2000, 140–41). Finally, we consider an organization (employment or otherwise) to be a group.
Social capital is intangible resources, such as trust and reciprocity, generated by the social structure for use by individuals and collectives. Because it is a public good, social capital is a characteristic of a collective, not an individual (Berkman and Kawachi 2000; Coleman 1990; Putnam 1995). Social capital facilitates action and coordination, shaping the “obligations and expectations for transactions” (Berkman and Kawachi 2000, 175–76) among people and in markets (Herrmann-Pillath 2010), thereby reinforcing existing structures.
References
- AF4Q (Aligning Forces for Quality) About Us. 2012. Available at http://forces4quality.org/about-us (accessed July 9, 2012)
- Ahern J, Galea S, Hubbard A, Syme SL. Neighborhood Smoking Norms Modify the Relation between Collective Efficacy and Smoking Behavior. Drug and Alcohol Dependency. 2009;100(1–2):138–45. doi: 10.1016/j.drugalcdep.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- Alexander JA, Beich J, Christianson JB, Hasnain-Wynia R, Hurley R, Keenan PS, Mittler JN, Scanlon DP. Confidential Interviews with Aligning Forces for Quality Participants. 2009. Verbatim Transcripts.
- Anderson RM, Funnell MM. Patient Empowerment: Myths and Misconceptions. Patient Education and Counseling. 2010;79:277–82. doi: 10.1016/j.pec.2009.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the Theory of Planned Behavior: A Meta-Analytic Review. British Journal of Social Psychology. 1999;38:195–222. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Arnold SB. Improving Quality Health Care: The Role of Consumer Engagement. 2007. Available at http://www.academyhealth.org/files/issues/ConsumerEngagement.pdf (accessed November 16, 2009)
- Arnold SB, Scanlon DP. Realizing True Consumer Directed Health Care: What the Policy Community Needs. Medical Care Research and Review. 2009;66(1):3S–8S. doi: 10.1177/1077558708327579. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Saddle River, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Health Promotion by Social Cognitive Means. Health Education and Behavior. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Barraclough JH, Birch J. Health Care Safety and Quality: Where Have We Been and Where Are We Going. Medical Journal of Australia. 2006;184(suppl. 10):S48–50. doi: 10.5694/j.1326-5377.2006.tb00362.x. [DOI] [PubMed] [Google Scholar]
- Becker ER, Roblin DW. Translating Primary Care Practice Climate into Patient Activation: The Role of Patient Trust in Physician. Medical Care. 2008;46(8):795–805. doi: 10.1097/MLR.0b013e31817919c0. [DOI] [PubMed] [Google Scholar]
- Berenson RA. Which Way for Competition? None of the Above. Health Affairs. 2005;24(6):1536–42. doi: 10.1377/hlthaff.24.6.1536. [DOI] [PubMed] [Google Scholar]
- Berkman L, Kawachi I. Social Epidemiology. Oxford: Oxford University Press; 2000. [Google Scholar]
- Brody DS. The Patient's Role in Clinical Decision-Making. Annals of Internal Medicine. 1980;93:718–22. doi: 10.7326/0003-4819-93-5-718. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Brown AD, Alikhan LM, Sandoval GA, Seeman N, Baker GR, Pink GH. Acute Care Hospital Strategic Priorities: Perceptions of Challenges, Control, Competition and Collaboration in Ontario's Evolving Healthcare System. Healthcare Quarterly. 2005;8(3):36–47. [PubMed] [Google Scholar]
- Buttimer A. Social Space in Interdisciplinary Perspective. Geographical Review. 1969;59(2):417–26. [Google Scholar]
- CDC (Centers for Disease Control and Prevention) Communities Putting Prevention to Work: CDC Awards $372.8 Million to 44 Communities. 2010. Available at http://www.cdc.gov/Features/ChronicPreventionGrants/ (accessed January 3, 2010)
- Charles C, Gafni A, Whelan T. Shared Decision-Making in the Medical Encounter: What Does It Mean? (Or It Takes Two to Tango) Social Science & Medicine. 1997;44(5):681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T, O'Brien A. Cultural Influences on the Physician-Patient Encounter: The Case of Shared Treatment Decision-Making. Patient Education and Counseling. 2006;63:262–67. doi: 10.1016/j.pec.2006.06.018. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. Social Contagion Theory: Examining Dynamic Social Networks and Human Behavior. Statistics in Medicine. 2012 doi: 10.1002/sim.5408. June 18 (e-pub before print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-Management of Chronic Disease by Older Adults: A Review and Questions for Research. Journal of Aging and Health. 1991;3(1):3–27. [Google Scholar]
- Cohen DA, Inagami S, Finch B. The Built Environment and Collective Efficacy. Health Place. 2008;14(2):198–208. doi: 10.1016/j.healthplace.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JS. Social Capital in the Creation of Human Capital. American Journal of Sociology. 1990;94(suppl):S95–S120. [Google Scholar]
- Culyer A, Newhouse JP. The Handbook of Health Economics. Amsterdam: North Holland; 2000. [Google Scholar]
- Cutilli CC. Seeking Health Information: What Sources Do Your Patients Use? Orthopedic Nursing. 2010;29(3):214–19. doi: 10.1097/NOR.0b013e3181db5471. [DOI] [PubMed] [Google Scholar]
- DHHS (Department of Health and Human Services) Value-Driven Health Care. 2008. Available at http://archive.hhs.gov/valuedriven/#top (accessed November 16, 2009)
- DHHS (Department of Health and Human Services) Key Features of the Affordable Care Act, by Year. 2012. Available at http://www.healthcare.gov/law/timeline/full.html (accessed July 5, 2012) [Google Scholar]
- Draper DA, Claxton G. Managed Care Redux: Health Plans Shift Responsibilities to Consumers. Center for Studying Health System Change: Issue Brief. 2004;(79):1–4. [PubMed] [Google Scholar]
- Duggan PS, Geller G, Cooper LA, Beach MC. The Moral Nature of Patient-Centeredness: Is It “Just the Right Thing to Do”? Patient Education and Counseling. 2006;62(20):271–76. doi: 10.1016/j.pec.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Dy SM, Purnell TS. Key Concepts Relevant to Quality of Complex and Shared Decision-Making in Health Care: A Literature Review. Social Science & Medicine. 2012;74(4):582–87. doi: 10.1016/j.socscimed.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B, Kersh R, Brescoll VL, Dixon B. Calorie Labeling and Food Choices: A First Look at the Effects on Low-Income People in New York City. Health Affairs. 2009;28(6):1110–21. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Emanuel LL. Four Models of the Physician-Patient Relationship. JAMA. 1992;267(16):2221–26. [PubMed] [Google Scholar]
- Epstein RM, Street RL. The Values and Value of Patient-Centered Care. Annals of Family Medicine. 2011;9(2):100–103. doi: 10.1370/afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M. A Theory of Reasoned Action: Some Applications and Implications. Nebraska Symposium on Motivation. 1979;27:65–116. [PubMed] [Google Scholar]
- Fiske ST. Interpersonal Stratification: Status, Power, and Subordination. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 941–82. [Google Scholar]
- Fiske ST, Gilbert DT, Lindzey G. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. [Google Scholar]
- Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring Self-Management of Patients’ and Employees’ Health: Further Validation of the Patient Activation Measure (PAM) Based on Its Relation to Employee Characteristics. Patient Education Counseling. 2009;77(1):116–22. doi: 10.1016/j.pec.2009.02.018. [DOI] [PubMed] [Google Scholar]
- Friedkin N. Social Cohesion. Annual Review of Sociology. 2004;30:409–25. [Google Scholar]
- Fronstin P. Findings from the 2008 EBRI Consumer Engagement Health Care Survey. ERBI Issue Brief. 2008;323:1–42. [PubMed] [Google Scholar]
- Fronstin P. Findings from the 2010 EBRI/MGA Consumer Engagement Health Care Survey. EBRI Issue Brief. 2010;352:1–42. [PubMed] [Google Scholar]
- Galvin RS, Delbanco S, Milstein A, Belden G. Has the Leapfrog Group Had an Impact on the Health Care Market? Health Affairs. 2005;24(1):228–33. doi: 10.1377/hlthaff.24.1.228. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK. Perspectives on Using Theory: Past, Present, and Future. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 509–18. [Google Scholar]
- Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- Glanz K, Schwartz MD. Stress, Coping and Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 211–36. [Google Scholar]
- Gradstein M, Schiff M. The Political Economy of Social Exclusion with Implications for Immigration Policy. Journal of Population Economics. 2006;19:327–44. [Google Scholar]
- Graham RE, Ahn RC, Davis RB, O'Connor BB, Eisenbers DM, Phillips RS. Use of Complementary and Alternative Medical Therapies among Racial and Ethnic Minority Adults: Results from the 2002 National Health Interview Survey. Journal of the National Medical Association. 2005;97(3):535–45. [PMC free article] [PubMed] [Google Scholar]
- Granovetter M. The Strength of Weak Ties. American Journal of Sociology. 1973;78(6):1360–80. [Google Scholar]
- Greene J, Hibbard J. Why Does Patient Activation Matter? An Examination of the Relationships between Patient Activation and Health-Related Outcomes. Journal of General Internal Medicine. 2011 doi: 10.1007/s11606-011-1931-2. November 30 (e-pub before print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruman J, Rovner MH, French ME, Jeffress D, Sofaer S, Shaller D, Prager DJ. From Patient Education to Patient Engagement. Patient Education and Counseling. 2010;78:350–56. doi: 10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Gruman J, Rovner MH, Jeffress D, Sofaer S, Shaller D, Prager D. A New Definition of Patient Engagement: What Is Engagement and Why Is It Important? Washington, DC: Center for the Advancement of Health; 2009. [Google Scholar]
- Harris KM, Buntin MB. Choosing a Health Care Provider: The Role of Quality Information. Research Synthesis Report: Robert Wood Johnson Foundation. 2008;14:1–26. [PubMed] [Google Scholar]
- Harvey L, Fowles JB, Xi M, Terry P. When Activation Changes, What Else Changes? The Relationship between Change in Patient Activation Measure (PAM) and Employees’ Health Status and Health Behaviors. Patient Education and Counseling. 2012 doi: 10.1016/j.pec.2012.02.005. March 26 (e-pub before print) [DOI] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, MacDonald HP, Yao X. Interventions for Enhancing Medication Adherence. Cochrane Database of Systematic Reviews. 2008;16(2):CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- Heaney CH, Israel BA. Social Networks and Social Support. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 189–210. [Google Scholar]
- Helman C. Culture, Health, & Illness. London: Arnold; 2001. [Google Scholar]
- Herrmann-Pillath C. What Have We Learnt from 20 Years of Economic Research into Culture? International Journal of Cultural Studies. 2010;13(4):317–35. [Google Scholar]
- Herzog TA. A Welcomed and Overdue Debate. Health Psychology. 2010;29(1):102–3. [Google Scholar]
- Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK, Viswanath K. Trust and Sources of Health Information. Archives of Internal Medicine. 2005;165(22):2618–24. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- Hibbard JH. Community-Based Participation Approaches and Individual Health Activation. Journal of Ambulatory Care Management. 2009a;32(4):275–77. doi: 10.1097/JAC.0b013e3181ba6f63. [DOI] [PubMed] [Google Scholar]
- Hibbard JH. Using Systematic Measurement to Target Consumer Activation Strategies. Medical Care Research and Review. 2009b;66(suppl. 1):9S–27S. doi: 10.1177/1077558708326969. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Cunningham PJ. How Engaged Are Consumers in Their Health and Health Care, and Why Does It Matter? Research Brief: Center for Studying Health System Change. 2008;8:1–9. [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER. Toward a Theory of Patient and Consumer Activation. Patient Education and Counseling. 2010;78:377–81. doi: 10.1016/j.pec.2009.12.015. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stock R, Tusler M. Do Increases in Patient Activation Result in Improved Self-Management Behaviors? Health Services Research. 2007a;42(4):1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and Testing of a Short Form of the Patient Activation Measure. Health Services Research. 2005;40(6, part 1):1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Peters E, Dixon A, Tusler M. Consumer Competencies and the Use of Comparative Quality Information: It Isn't Just about Literacy. Medical Care Research and Review. 2007b;64(4):379–94. doi: 10.1177/1077558707301630. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Services Research. 2004;39(4, part 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter A. The Loss of Community: An Empirical Test through Replication. American Sociology Review. 1975;40(5):537–52. [Google Scholar]
- Hurley RE, Keenan PS, Martsolf GR, Maeng DD, Scanlon DP. Early Experiences with Consumer Engagement Initiatives to Improve Chronic Care. Health Affairs. 2009;28(1):277–83. doi: 10.1377/hlthaff.28.1.277. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine), Committee on Health and Behavior. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A Decade Later. Health Education Quarterly. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jepson RG, Harris FM, Platt S, Tannahill C. The Effectiveness of Interventions to Change Six Health Behaviors: A Review of Reviews. BMC Public Health. 2010;10:538–54. doi: 10.1186/1471-2458-10-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JA, Meehan-Andrews TA, Smith KB, Humphreys JS, Griffin L, Wilson B. “There's No Point in Complaining, Nothing Changes”: Rural Disaffection with Complaints as an Improvement Method. Australian Health Review. 2006;30(3):322–32. doi: 10.1071/ah060322. [DOI] [PubMed] [Google Scholar]
- Kegeler MC, Glanz K. Perspectives on Group, Organization, and Community Interventions. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 389–404. [Google Scholar]
- Ketelaar NA, Faber MJ, Flottorp S, Rygh LH, Deane KH, Eccles MP. Public Release of Performance Data in Changing Behavior of Consumers, Health Care Professionals or Organisations. Cochrane Database of Systematic Reviews. 2011;9(11):CD004538. doi: 10.1002/14651858.CD004538.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KFF-HRET (Kaiser Family Foundation and Health Research and Education Trust) Employer Health Benefits: 2008 Annual Survey, September 24. 2008. Available at http://ehbs.kff.org/pdf/7790.pdf (accessed July 3, 2012)
- KFF-HRET (Kaiser Family Foundation and Health Research and Education Trust) Employer Health Benefits: 2011 Annual Survey, September 27. 2011. Available at http://ehbs.kff.org/pdf/2011/8225.pdf (accessed July 3, 2012)
- Kleinman A. Patients and Healers in the Context of Culture: An Exploration of the Borderland between Anthropology, Medicine, and Psychiatry. Berkeley: University of California Press; 1980. [Google Scholar]
- Kleinman A, Hall-Clifford R. Stigma: A Social, Cultural and Moral Process. Journal of Epidemiology and Community Health. 2009;63(6):418–19. doi: 10.1136/jech.2008.084277. [DOI] [PubMed] [Google Scholar]
- Kolstad JT, Chernew ME. Quality and Consumer Decision Making in the Market for Health Insurance and Health Care Services. Medical Care Research & Review. 2009;66(suppl.1):28S–52S. doi: 10.1177/1077558708325887. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Haughton LT. Integrating Culture into Health Information for African American Women. American Behavioral Scientist. 2006;49(6):794–811. [Google Scholar]
- Larson C, Schlundt D, Patel K, Goldzweig I, Hargreaves M. Community Participation in Health Initiatives for Marginalized Populations. Journal of Ambulatory Care Management. 2009;32(4):264–70. doi: 10.1097/JAC.0b013e3181ba6f74. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood Environments: Disparities in Access to Healthy Foods in the U.S. American Journal of Preventive Medicine. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lau R. Individual and Contextual Influences on Group Identification. Social Psychology Quarterly. 1989;52(3):220–31. [Google Scholar]
- Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, Lawrence D, Morath J, O'Leary D, O'Neill P, Pinakiewicz D, Isaac T. Transforming Health Care: A Safety Imperative. Quality Safety in Health Care. 2009;28(6):424–28. doi: 10.1136/qshc.2009.036954. [DOI] [PubMed] [Google Scholar]
- Leary M. Affiliation, Acceptance, and Belonging: The Pursuit of Interpersonal Connection. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 864–97. [Google Scholar]
- Lee PV, Hoo E. Beyond Consumer-Driven Health Care: Purchasers’ Expectations of All Plans. Health Affairs. 2006;25(6):w544–48. doi: 10.1377/hlthaff.25.w544. [DOI] [PubMed] [Google Scholar]
- Link BG, Phalen JC. Conceptualizing Stigma. Annual Review of Sociology. 2001;27:363–85. [Google Scholar]
- Lippke S, Schwarzer R, Ziegelmann JP, Scholz U, Schuz B. Targeting Stage-Specific Effects of a Stage-Matched Intervention: A Randomized Controlled Trial Targeting Physical Exercise and Its Predictors. Health Education Behavior. 2010;37(4):533–46. doi: 10.1177/1090198109359386. [DOI] [PubMed] [Google Scholar]
- Longo DR. Understanding Health Information, Communication, and Information Seeking of Patients and Consumers: A Comprehensive & Integrated Model. Health Expectations. 2005;8:189–94. doi: 10.1111/j.1369-7625.2005.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Villa FJ, Armas J. Community-Based Peer-Led Diabetes Self-Management: A Randomized Trial. Diabetes Education. 2009;35(4):641–51. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a Self-Management Program on Patients with Chronic Disease. Effective Clinical Practice. 2001;4(6):256–62. [PubMed] [Google Scholar]
- Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, Wolfson M. Is Income Inequality a Determinant of Population Health? Part 1: A Systematic Review. The Milbank Quarterly. 2002;82(1):5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maillet P, Halterman S. The Consumer-Driven Approach: Defining and Measuring Success. Benefits Quarterly. 2004;2:1–9. [PubMed] [Google Scholar]
- Merriam-Webster. Activate. 2012a. Available at http://merriam-webster.com/dictionary/activate (accessed January 7, 2012)
- Merriam-Webster. Consumer. 2012b. Available at http://merriam-webster.com/dictionary/consumer (accessed January 7, 2012)
- Merriam-Webster. Engagement. 2012c. Available at http://merriam-webster.com/dictionary/engagement (accessed January 7, 2012)
- Merriam-Webster. Shopping. 2012d. Available at http://merriam-webster.com/dictionary/shopping (accessed January 7, 2012)
- McAlister AL, Perry CL, Parcel GS. How Individuals, Environments and Health Behaviors Interact: Social Cognitive Theory. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 167–88. [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An Ecological Perspective on Health Promotion Programs. Health Education Quarterly. 1988;15:351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N, Wilson N. Improving Health through Community Organization and Community Building. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 283–309. [Google Scholar]
- Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is Patient Activation Associated with Outcomes of Care for Adults with Chronic Conditions? Journal of Ambulatory Care Management. 2007;30(1):21–29. doi: 10.1097/00004479-200701000-00005. [DOI] [PubMed] [Google Scholar]
- Munro S, Lewin S, Swart T, Volmink J. A Review of Health Behaviour Theories: How Useful Are These for Developing Interventions to Promote Long-Term Medication Adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:104–20. doi: 10.1186/1471-2458-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Patient Safety Foundation. Ask-Me-Three. 2009. Available at http://www.npsf.org/askme3/ (accessed November 20, 2009)
- Nemet GF, Bailey AJ. Distance and Health Care Utilization among the Rural Elderly. Social Science & Medicine. 2000;50(9):1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- Nichols LM, Ginsburg PB, Berenson RA, Christianson J, Hurley BE. Are Market Forces Strong Enough to Deliver Efficient Health Care Systems? Confidence Is Waning. Health Affairs. 2004;23(2):8–21. doi: 10.1377/hlthaff.23.2.8. [DOI] [PubMed] [Google Scholar]
- Northrop M, Pittam G, Caan W. The Expectations of Families and Patterns of Participation in a Trailblazer Sure Start. Community Practitioner. 2008;81(2):24–28. [PubMed] [Google Scholar]
- Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The Use of Theory in Health Behavior Research from 2000 to 2005: A Systematic Review. Annals of Behavioral Medicine. 2008;33(3):358–62. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- Painter MW, Lavizzo-Mourey R. Aligning Forces for Quality: A Program to Improve Health and Health Care in Communities across the United States. Health Affairs. 2008;27(5):1461–63. doi: 10.1377/hlthaff.27.5.1461. [DOI] [PubMed] [Google Scholar]
- Parsons T. The Social System. Glencoe, IL: Free Press; 1951. [Google Scholar]
- Prochaska JO. Decision Making in the Transtheoretical Model of Behavior Change. Medical Decision Making. 2008;28(6):845–49. doi: 10.1177/0272989X08327068. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Evers KE. The Transtheoretical Model and Stages of Change. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 97–122. [Google Scholar]
- Prochaska JO, Velcier W, Rossi J, Goldstein M, Marcus B, Rakowski W, Fiore C, Harlow L, Redding C, Rosenbloom D, Rossi S. Stages of Change and Decisional Balance for 12 Problem Behaviors. Health Psychology. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Protheroe J, Nutbeam D, Rowlands G. Health Literacy: A Necessity for Increasing Participation in Health Care. British Journal of General Practice. 2009;59(567):721–23. doi: 10.3399/bjgp09X472584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam RD. Bowling Alone. New York: Simon & Schuster; 1995. [Google Scholar]
- Reitz JG, Sklar SM. Culture, Race, and Economic Assimilation of Immigrants. Sociological Forum. 1997;12(2):233–77. [Google Scholar]
- Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is Patient Activation Associated with Future Health Outcomes and Healthcare Utilization among Patients with Diabetes? Journal of Ambulatory Care Management. 2009;32(4):320–27. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- Richard L, Gauvin L, Raine K. Ecological Models Revisited: Their Uses and Evolution in Health Promotion over Two Decades. Annual Review of Public Health. 2011;32:307–26. doi: 10.1146/annurev-publhealth-031210-101141. [DOI] [PubMed] [Google Scholar]
- Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the Impact of Menu Labeling on Food Choices and Intake. American Journal of Public Health. 2010;100:312–18. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roblin DW, Becker ER. The Community Counts! But the Question Remains, How Much? Journal of Ambulatory Care Management. 2009;32(4):292–94. doi: 10.1097/JAC.0b013e3181ba6e62. [DOI] [PubMed] [Google Scholar]
- Rolfe T, Sheehan B, Davidson R. Are Consumers on Community Treatment Orders Informed of Their Legal and Human Rights? A West Australian Study. International Journal of Mental Health Nursing. 2008;17(1):36. doi: 10.1111/j.1447-0349.2007.00509.x. [DOI] [PubMed] [Google Scholar]
- Rosen P, Anell A, Hjortsberg C. Patient Views on Choice and Participation in Primary Health Care. Health Policy. 2001;55:121–128. doi: 10.1016/s0168-8510(00)00122-6. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological Models of Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 465–86. [Google Scholar]
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “Neighborhood Effects”: Social Processes and New Directions in Research. Annual Review of Sociology. 2002;28:443–78. [Google Scholar]
- Scanlon DP, Alexander JA, Beich J, Christianson JB, Hasnain-Wynia R, McHugh MC, Mittler JN, Shi Y, Bodenschatz LJ. Evaluating a Community-Based Program to Improve Healthcare Quality: Research Design for the Aligning Forces for Quality Initiative. American Journal of Managed Care. 2012;18(6):eS165–eS176. [PubMed] [Google Scholar]
- Schaeffer LD, McMurtry DE. When Excuses Run Dry: Transforming the U.S. Health Care System. Health Affairs. 2004:117–20. doi: 10.1377/hlthaff.var.117. web suppl.:VAR. [DOI] [PubMed] [Google Scholar]
- Schumaker S, Ockene J, Riekert K. The Handbook of Health Behavior Change. New York: Springer; 2009. [Google Scholar]
- Seven R. King County's “Health Incentives” Program Relies on the Power of Preventative Care. 2009. Seattle Times, March 1.
- Shaller D. Consumer Engagement: Whose Responsibility Is It? American Journal of Medical Quality. 2007;22(5):309–10. doi: 10.1177/1062860607305596. [DOI] [PubMed] [Google Scholar]
- Shelley BM, Sussman AL, Williams RL, Crabtree BF. “They Don't Ask Me So I Don't Tell Them”: Patient-Clinician Communication about Traditional, Complementary, and Alternative Medicine. Annals of Family Medicine. 2009;7(2):139–47. doi: 10.1370/afm.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley A, Cantor JC, Guarnaccia P. Holes in the Safety Net: A Case Study of Access to Prescription Drugs and Specialty Care. Journal of Urban Health. 2008;85(4):555–71. doi: 10.1007/s11524-008-9282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuber J, Meyer I, Link B. Stigma, Prejudice, Discrimination, and Health. Social Science & Medicine. 2008;67(3):351–57. doi: 10.1016/j.socscimed.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann WB, Bosson JK. Self and Identity. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 589–628. [Google Scholar]
- Tajfel H, Turner J. An Integrative Theory of Intergroup Conflict. In: Austin WG, Worchel S, editors. The Social Psychology of Intergroup Relations. Monterey, CA: Brooks/Cole; 1979. pp. 33–48. [Google Scholar]
- Terry M. Health Care Consumerism: Engaging the Real Buyers—Employees. Benefits Quarterly. 2005;21(2):18–21. [PubMed] [Google Scholar]
- Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological Pathways Linking Social Support to Health Outcomes: A Visit with the “Ghosts” of Research Past, Present and Future. Social Science & Medicine. 2012;74:949–57. doi: 10.1016/j.socscimed.2011.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Sluijs EMF, van Poppel MNM, van Mechelen W. Stage-Based Lifestyle Interventions in Primary Care: Are They Effective? American Journal of Preventive Medicine. 2004;26(4):330–43. doi: 10.1016/j.amepre.2003.12.010. [DOI] [PubMed] [Google Scholar]
- Viswanath K. Perspectives on Models of Interpersonal Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 271–82. [Google Scholar]
- Warner K, Mendez D. Tobacco Control Policy in Developed Countries: Yesterday, Today, and Tomorrow. Nicotine & Tobacco Research. 2010;12(9):876–87. doi: 10.1093/ntr/ntq125. [DOI] [PubMed] [Google Scholar]
- Williams D, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff LS, Subramanian SV, Acevedo-Garcia D, Weber D, Kawachi I. Compared to Whom? Subjective Social Status, Self-Rated Health, and Referent Group Sensitivity in a Diverse US Sample. Social Science and Medicine. 2010;70(12):2019–28. doi: 10.1016/j.socscimed.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yzerbyt V, Demoulin S. Intergroup Relations. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 1024–83. [Google Scholar]


