Abstract
Context
Over the past decade, a number of high-impact natural hazard events, together with the increased recognition of pandemic risks, have intensified interest in health systems’ ability to prepare for, and cope with, “surges” (sudden large-scale escalations) in treatment needs. In this article, we identify key concepts and components associated with this emerging research theme. We consider the requirements for a standardized conceptual framework for future research capable of informing policy to reduce the morbidity and mortality impacts of such incidents. Here our objective is to appraise the consistency and utility of existing conceptualizations of health systems’ surge capacity and their components, with a view to standardizing concepts and measurements to enable future research to generate a cumulative knowledge base for policy and practice.
Methods
A systematic review of the literature on concepts of health systems’ surge capacity, with a narrative summary of key concepts relevant to public health.
Findings
The academic literature on surge capacity demonstrates considerable variation in its conceptualization, terms, definitions, and applications. This, together with an absence of detailed and comparable data, has hampered efforts to develop standardized conceptual models, measurements, and metrics. Some degree of consensus is evident for the components of surge capacity, but more work is needed to integrate them. The overwhelming concentration in the United States complicates the generalizability of existing approaches and findings.
Conclusions
The concept of surge capacity is a useful addition to the study of health systems’ disaster and/or pandemic planning, mitigation, and response, and it has far-reaching policy implications. Even though research in this area has grown quickly, it has yet to fulfill its potential to generate knowledge to inform policy. Work is needed to generate robust conceptual and analytical frameworks, along with innovations in data collection and methodological approaches that enhance health systems’ readiness for, and response to, unpredictable high-consequence surges in demand.
Keywords: surge capacity, disease outbreaks, disaster planning/organization and administration, disaster medicine/manpower
Evidence shows that the frequency of recorded casualty-producing natural hazard events has increased more than fourfold across the world since the mid-1970s (ADRC 2009; Guha-Sapir et al. 2011). Whether this is a result of more frequent events or of heighted exposure and vulnerability to hazards is unclear, as the detection of patterns and trends in the frequency of physical hazards requires millions (or hundreds of millions) of years. What is clear, however, is that demographic, social, and environmental shifts are forcing increasing numbers of people to occupy (hitherto avoided) areas (Dobbs et al. 2011; UN 2005). Vulnerabilities to natural hazard–induced disasters may be amplified in the future as processes of environmental degradation, rapid urbanization, and social marginalization (themselves representing latent, serious challenges to sustain the capacity of the health system) exacerbate their impacts (ADRC 2009; Guha-Sapir et al. 2011; UNISDR 2011). While few countries are immune to risks from natural hazards, historically it is low-income countries, particularly those in Asia, that are subject to the highest incidence, and impacts, of natural hazard–induced disasters (ADRC 2009; Guha-Sapir et al. 2011).
A similar historical trajectory is evident in the prevalence of emerging infectious diseases (EIDs) (Jones et al. 2008). Global EID “hot spots” (presented in figure 1) are likewise disproportionately located in the global south, where a complex mix of societal (population density, antibiotic drug use, and agricultural systems and practices) and environmental (precipitation, temperatures, and prevalence of severe weather events) factors converge as important drivers of outbreaks and where surveillance efforts and control measures are currently weakest.
FIGURE 1.
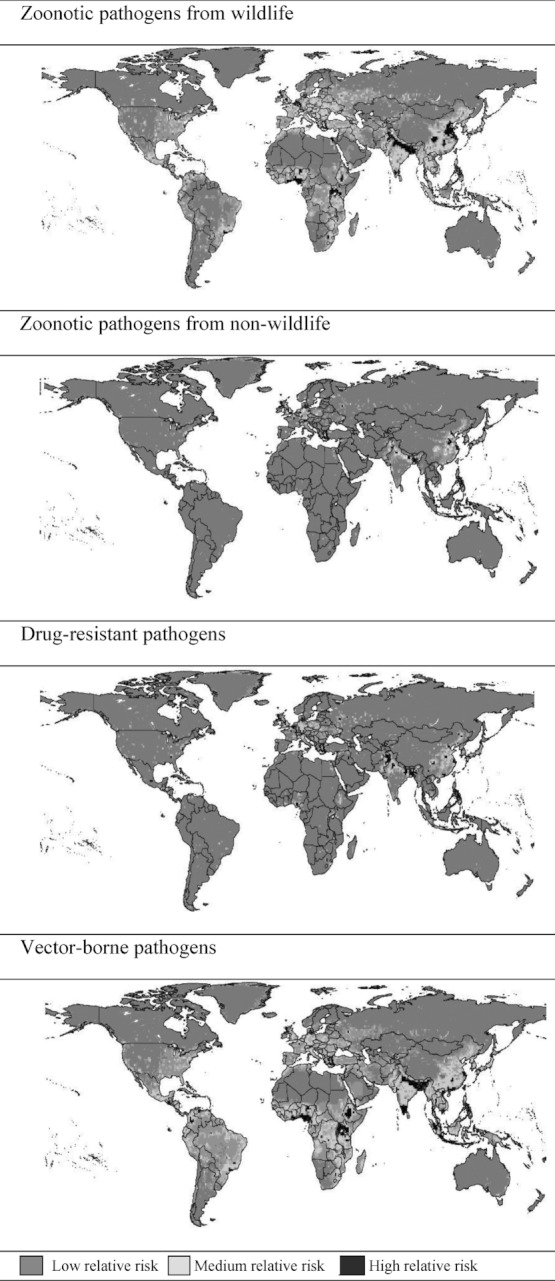
Risk “hot spots” for emerging infectious diseases.
Source: Jones et al. 2008.
These twin trends and the threats they represent are being taken increasingly seriously. International and national disaster mitigation initiatives now explicitly incorporate a strong proactive and preemptory dimension and recognize a key role for health systems in effective planning and response (EU 2009, 2011; UN 2005; WHA 2011). The priorities laid out in the United Nations’ Hyogo Framework for Action (HFA) for 2005–2015 and in the broader mandate of the UN International Strategy for Disaster Reduction (UNISDR) (UN 2005) are in line with this approach. So, too, is the European Union (EU)'s announcement in 2009 of its own commitment to disaster risk reduction in both Europe and the global south, which was articulated in its Community Approach to the Prevention of Natural and Manmade Disasters (EU 2009) and its Strategy for Supporting Disaster Risk Reduction in Developing Countries (EU 2011). The sixty-fourth World Health Assembly resolution, Strengthening National Health Emergency and Disaster Management Capacities and Resilience of Health Systems, builds on these recent global initiatives to highlight the centrality of health systems to disaster preparation, resilience, and response (WHA 2011).
These recent initiatives emphasize that natural hazard events do not translate directly or necessarily into disasters (defined by their impact on society and environment) (UN 2005), and both the UN and EU stress that the disaster risk of natural hazards can be reduced (EU 2011; UN 2005). Figures 2 and 3 demonstrate the global exposure and the global vulnerability to natural hazard risks. Comparison of figures 2 and 3 indicates that the two are not synonymous, for measures can be taken to reduce population vulnerability. The challenge, as many international organizations are beginning to acknowledge (EU 2011), lies in translating the uncoordinated ad hoc project/program approach into strategic and coordinated action at the global, regional, national, and local levels.
FIGURE 2.
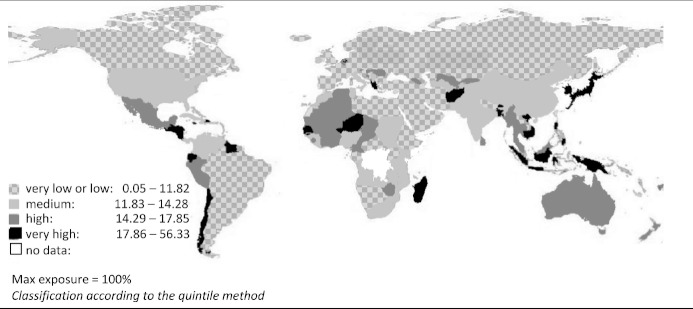
Population risk—exposure to natural hazards.
Source: BEH 2012.
FIGURE 3.
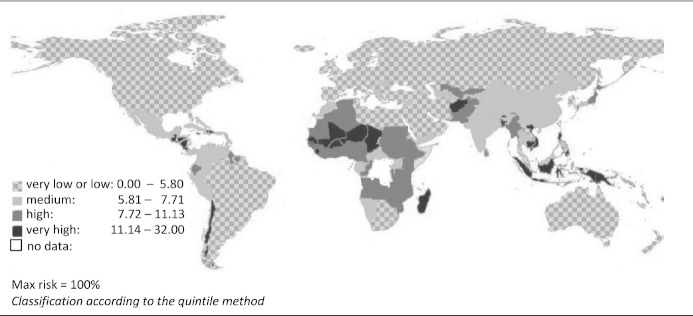
Population risk as a function of exposure (figure 2) and vulnerability.
Note: Vulnerability is a composite measure of (1) susceptibility (calculated as a function of public infrastructure status, population nutritional status, and income levels); (2) coping capacities (status of governance, medical care, and material security); and (3) adaptive capacities (projected risks).
Source: BEH 2012.
This approach can be extended to a parallel stream of research focused on the resources, procedures, and processes that need to be in place for pandemic readiness and response. In a recent comparative review of international pandemic preparedness plans, the World Health Organization (WHO) identified a widespread absence of subnational planning as a serious obstacle to coordinated action in the event of a pandemic (WHO 2011a). The WHO's report recommends revising international plans to spell out responsibilities, roles, and authorizations at the various subnational levels, a finding that is consistent with the recommendations of the various international agencies planning for natural hazard–induced disaster scenarios (EU 2009, 2011; UN 2005; WHA 2011).
The concept of health systems’ surge capacity provides a potential means to capture and coordinate the commonalities of pandemic and disaster planning needs in order to generate a model for health systems’ readiness for and response to a wide range of scenarios. In this article we systematically review the ways in which health systems’ surge capacity has been conceptualized since its inception as an area of research. We consider the multifaceted nature of the concept and draw out the different components that various seams in the literature have emphasized.
Methods
We conducted a comprehensive search of electronic databases to identify articles and records of conference proceedings that (re)conceptualize or define health system surge capacity, or some aspect thereof. Further search inclusion criteria were (online) publication (in English) before October 28, 2011, and presence in one of the following databases: Medline (accessed via Pubmed and OVID), Web of Science, and Web of Knowledge. No limitations on country of origin or of emphasis were included, as the (inter)national applicability of the concept formed an important area of interest. A number of articles applied the concept of surge capacity to day-to-day fluctuations in emergency room numbers. We included in our analysis those articles that considered this application of the concept within an extended framework that encompassed lessons for disaster or crisis scenarios, and we excluded those that limited the concept's application to operational issues surrounding emergency room overcrowding. We conducted our initial search in these databases using the following terms: (surge) AND (capacity OR ability OR response OR accommodate* OR capability OR cope OR absorption OR facilit*) AND (health OR medic* OR hospital) AND (disaster OR catastroph* OR critical OR epidemic OR pandemic OR terror* OR hazard* OR crisis OR emergency OR urgen* OR tragedy OR calamit*).
The following Medical Subject Heading (MeSH) terms were used in the PubMed search: “Surge capacity,” “Mass casualty incidents,” “Disease outbreaks,” “Disaster Medicine / Manpower,” “Disaster Medicine / organization & administration,” “Disaster Planning / organization & administration,” “Disaster Planning / standards,” “Disaster Planning / methods,” “Disasters.”
Widening the search criteria was a deliberate strategy designed to capture the anticipated variety in the concept's application and to avoid excluding relevant articles. Our initial electronic search produced 687 unique articles. The broad search strategy necessarily resulted in the capture of irrelevant articles (these commonly related to “surges” in viral or parasitic load in experimental laboratory or clinical settings). We excluded 508 such papers on the basis of their title and, if necessary, their abstract. In line with our objective to appraise the extent of the concept's recognition, we retained all articles concerned with the health system implications of “surge capacity” in a disaster (broadly defined) context even if the concept was used only in passing and was not defined.
These articles were screened for relevance in line with our stated exclusion and inclusion criteria, resulting in a total of 176 articles. We found ten more articles in the bibliographies of papers originating in the initial search, making a total of 186 academic, peer-reviewed articles that we reviewed. Although the earliest article (Loretti, Leus, and Van Hosteijn 2001) was published in the summer of 2001, only five articles on surge capacity were published before 2005.1 Samantha Watson and James Rudge separately and independently undertook this process. They agreed on the inclusion criteria before the search and then met to discuss their findings. Of the articles that they agreed were relevant, 167 (89.8%) related to the U.S. context and experience. Fifteen were related to a country other than the United States,2 and four3 pertained to a low-income country.
Although our primary objective was a systematic review of the concept's emergence and consolidation in the academic, peer-reviewed literature, we subsequently assessed whether the health systems’ surge capacity concept extended to the policy world. This entailed a search of online publications and web resources for a number of health services and/or policy- and management-related agencies, organizations, and consortia responsible for preparing for and/or responding to disaster scenarios, including national health departments/ministries, international organizations, and allied agencies: ALNAP, CARE, CARE Australia, CARE International, CRS, ECB (Emergency Capacity Building), HAP, ICRC, IFRC, Inter-Action, International, Medair, Mercy Corps, MSF, NRC, Oxfam, People in Aid, Save the Children, Sphere, UNDP, UNIASC, UNICEF, UNOCHA, WFP, WHO, and World Vision International. This extension was considered valid given that the value of the health system surge capacity concept is largely its relevance (or otherwise) to real-world “surge” scenarios. Our examination of government and NGO (nongovernmental organization) web resources, publications, and reports discovered a recent (and ongoing) crossover of the term “surge capacity” from the academic literature.
The following sections discuss the key sites of consensus and debate in the academic literature, drawing on the “gray” literature to inform our consideration of the scope for coordinating research and practice.
Findings
The Concept of “Surge”
Differences in the conceptions of health system surge capacity begin at the level of first principles, with contention over what constitutes a surge event, scenario, or process. This ambiguity is largely a result of the term's extension beyond its traditional application to disaster contexts to encompass daily, weekly, and seasonal fluctuations in emergency departments’ patient numbers, which historically were discussed in terms of (over)crowding. This extension was initiated by the 2006 Academic Emergency Medicine Consensus Conference, “The Science of Surge” (Kelen and McCarthy 2006). The debate turns on the term's applicability to this latter context, as well as the relationship (if any) between care need escalations embedded in regular fluctuations in patient inflow (widely termed “daily surge”) and those related to extraordinary events (known as “disaster surge”).
Three broad positions can be discerned in the academic literature. The first envisages these two surge contexts as a continuum of the same underlying phenomenon. The second presents them as separate but related categories, with the potential to mutually inform one another. The third restricts the term's use to exceptional events, deeming its application to routine fluctuations in health care needs to be inappropriate. Table 1 lists the characteristics of each position. Although the third conceptualization appears as the least represented in table 1, it is in fact the default position of the majority of the literature on surge, which does not recognize the concept of “daily surge” and in which the term “surge” (without the “disaster” precursor) refers exclusively to severe and unanticipated escalations in health system demand.
TABLE 1.
The Relationship between “Daily” and “Disaster” Surge
| Conceptualization | Characteristics | Authors |
|---|---|---|
| Continuum | The “surge” concept is applied to any peak in patient census, including those associated with day-to-day operations; the focus is on individual facilities and emergency departments. | Asplin et al. 2006; Bradt etal. 2009; Handler et al. 2006; Jenkins, O'Connor, and Cone 2006; Kelen and McCarthy 2006; McCarthy, Aronsky, and Kelen 2006; Rothman et al. 2006; Schull 2006; Schull et al. 2006 |
| Separate but related categories | The “surge” concept is applied equally to operational fluctuations and disaster contexts, which are acknowledged as different and distinct phenomena. | Avery et al. 2008; Barbisch and Koenig 2006; Kaji, Koenig, and Bey 2006 |
| Misnomer | The “surge” concept is reserved for scenarios occasioning departures from standard operational practices; its application to daily fluctuations is deemed inappropriate and confusing. | Bonnett et al. 2007; Hick, Barbera, and Kelen 2009; Rubinson et al. 2008 |
While numerous definitions of “surge” and “surge capacity” have been proposed in “daily” and “disaster” contexts, the expansion of the term to incorporate routine fluctuations in patient numbers seems to undermine, rather than enhance, the scope for clarity regarding its key components, sites of application, and wider implications. “Daily surge” tends to be conflated with acute periods of chronic ED overcrowding. The difficulty in this application is that such “spikes” represent a failure to accommodate routine (if growing) demands on services in a context of widespread ED closures and diminished bed numbers, rather than the large-scale, unanticipated, and sudden escalation that is implied by the term “surge.”
Attempts to invoke “surge” as an umbrella concept encompassing both “small spikes in patient volume…encountered…during routine operations” and “situation[s] where a healthcare system is overwhelmed and must expand its operations to accommodate a large influx of patients” have been criticized for misrepresenting, by conflating, the distinct nature and causes of each (Bonnett et al. 2007, 300). In the remainder of this article we will use the term “surge” only for sudden, unanticipated escalations in health system demand caused by exceptional events (such as natural hazard–induced disasters and pandemics). Our point is that hospital overcrowding is an important issue, relevant to the concept and creation of surge capacity, but that it is a qualitatively distinct phenomenon.
Recent research has sought to subtype the concept of surge capacity (Bonnett et al. 2007; Hanfling 2006; Potter and Brough 2004). In practice, this has entailed differentiating natural hazard–induced disaster events from communicable disease outbreaks, which ties in well with the international approach to disaster and pandemic planning that we described earlier. A range of terms have been proposed for distinguishing these broad event types on the basis of their injury/illness profiles, geographical coverage, oscillations and trajectories over time, and duration. Barbisch and Koenig (2006) use the terms “sudden impact” and “obscure” events. Others have proposed “fixed” and “extended” (Hanfling 2006), “focal, time-limited” and “widespread, prolonged” (Potter and Brough 2004), and “contained and “population-based” (Bonnett et al. 2007). Each is intended to frame the “surge capacity” concept flexibly enough to be useful for researching and planning the response needs of a range of disaster types (Bonnett et al. 2007; Hick, Barbera, and Kelen 2009; Hick et al. 2004, 2008b). One point to be highlighted is that while these typologies are a useful abstract tool, “real-world” scenarios cannot always be neatly classified using these terms.
Depending on the initial response and a variety of other site- and scenario-specific characteristics, surges in mortality and morbidity may be phased. The proximate surge (i.e., immediate to short-term direct morbidity profile) in trauma injuries following an earthquake, for example, might be followed by a phased, or latent (i.e., longer-term and possibly indirect), surge in diseases associated with poor sanitation and crowding (Noji 1992). The cholera outbreak that followed in the wake of Haiti's devastating 2010 earthquake illustrates the potential for enormous repercussions to follow from phased impacts. This event also highlights the uncertainty and unpredictability that can attend the transition from proximate to latent phases of disaster-induced health care demands. Before October 2010, cholera had been absent from Haiti for more than a century (see Piarroux et al. 2011). More work is needed to assess, record, and model the morbidity profiles and trajectories associated with disasters, an area that is recognized to be underresearched at present (Bourque et al. 2007).
The Concept of Surge Capacity
In the absence of a standardized definition of surge capacity, the literature has used a range of meanings, with key terms at times defined differently within a single article and, in many cases, not defined at all.4 There is a tendency to conflate the terms “surge” and “surge capacity” (Hanfling 2006; McManus, Huebner, and Scheulen 2006) to refer to both a demand-side increase in health system resources (“disaster events…generate definable surges in demand for care”; Hanfling 2006,1233) and the supply-side response that such an event precipitates (“surge can be defined as the ability to rapidly meet increased demand for medical care”; Hanfling 2006, 1232). The latter definition, in which “surge” describes the response rather than the phenomenon necessitating the response, is widely used (Barbisch 2005; Barbisch and Koenig 2006; Binns, Sheppeard, and Staff 2010; Estacio 2006; Hotchkin and Rubinson 2008; Tadmor, McManus, and Koenig 2006). Barbisch discusses “optimizing outcomes in terms of optimizing surge and the sub-components of surge”; employing “surge” as a verb rather than a noun, thereby describing the “health care community['s]…need to surge to meet patient care needs that exceed expectations” (Barbisch 2005, 1098, italics added). Hotchkin and Rubinson similarly adopt this unwieldy verb to talk of “surging critical care capacity” (2008, 68, italics added). The majority position is, however, to define and/or use the term “surge” to refer to a sudden escalation and/or intensification of demand.
While at their core, most definitions of “surge capacity” denote “the ability…to respond to a sudden increase in patient care demands” (Hick et al. 2008b, S51), the specificity of the term's meaning and applications varies substantially beyond this general premise. One prominent, and important, variation is the term's applicability to scenarios in which external assistance is required. The American College of Emergency Physicians’ definition of surge capacity as a “measurable representation of a health care system's ability to manage a sudden or rapidly progressive influx of patients within the currently available resources at a given point in time” (ACEP 2006, 1, italics added) has been widely influential (Asplin, Flottemesch, and Gordon 2006; Bradt et al. 2009; Handler et al. 2006; McCarthy, Aronsky, and Kelen 2006; Robertson and Cooper 2007; Rottman et al. 2010; Schull 2006; Schull et al. 2006; Schultz and Stratton 2007; Welzel et al. 2010) but risks excluding consideration of potentially important mobilizable resources.
Other authors emphasize that surge capacity relates to not merely the sufficiency of currently available resources but also the ability to effectively and rapidly expand capacity (AHRQ 2006; Bonnett et al. 2007; Dayton et al. 2008; Hick, Barbera, and Kelen 2009; Hick, Christian, and Sprung 2010; Hick et al. 2004, 2008a, 2008b; Rodgers et al. 2006; Schultz and Koenig 2006; Stratton and Tyler 2006). This conceptualization was articulated clearly by Hick and colleagues (Hick, Barbera, and Kelen 2009; Hick et al. 2004, 2008b), who defined surge capacity as “the ability to manage a sudden, unexpected increase in patient volume that would otherwise severely challenge or exceed the present capacity” (Hick et al. 2004, 1) of either an individual facility or the wider health care system (Hick et al. 2004). This latter point demonstrates another common variation in published definitions, related to the site(s) at which “surge capacity” is deemed applicable. There is also variation in the unit of analysis employed by different studies. While some authors limit the concept to the individual facility5 or single department (usually the emergency department or ICU),6 the importance of embedding facilities within the wider health system's context is increasingly stressed.7
Two broad applications are apparent, consistent with the priorities and objectives of the agencies involved. The first entails the concept's increasing occurrence in international guidelines and best practices. An early example of this is the United Kingdom's Department of Health's published guidelines on pandemic management (DoH 2009). Its approach is consistent with that advocated by Kelen and colleagues, which we discuss in some detail later. In its publication Hospital Emergency Response Checklist: An All-Hazards Tool for Hospital Administrators and Emergency Managers, the World Health Organization (WHO) took the lead in promoting “surge capacity” as a component of international good practice (2011b). This report advocates surge capacity as one of nine “key components” of health systems’ disaster readiness (the remaining eight are command and control, communication, safety and security, triage, continuity of essential services, human resources, logistics and supply management, and postdisaster recovery). “Surge capacity” is broken down into thirteen key sites of action, centered on calculating baseline resources, estimating surge requirements, and identifying gaps to be addressed. It follows the academic literature's emphasis on the “four S's” of surge capacity (staff, stuff, structure, and systems) and, while concentrating on the facility level, notes the need to attend to the potential to mobilize extrinsic resources in line with the wider health systems approach. The WHO draws explicitly on the 2009 pandemic guidance (DoH 2009) issued by the United Kingdom's Department of Health. The second, and more common, use of the term (without the “health systems’” prefix) is in its application to the ability of humanitarian and aid agencies to scale up their own operational capacity in response to sudden-onset needs (Emmens and Houghton 2008; Houghton and Emmens 2007).
The term “surge response capability” is a recent addition to the literature. Despite the increasing use of this term, there is little consensus on what it is, what it means, and whether (and in what ways) it differs from the concept of “surge capacity.” While the term “capability” is most commonly used as a synonym for “capacity,” another seam in the literature (Barbera and Macintyre 2002; Binns, Sheppeard, and Staff 2010; Felland et al. 2008; Hanfling 2006; Hick, Barbera, and Kelen 2009; Hick et al. 2004, 2008a, 2008b) has attempted to define a separate identity for the “capability” concept. This revolves around its designation to denote the availability and adequacy of specialized resources and skills needed to meet the needs of a specific injury group, such as burn victims. While it is useful to explicitly recognize that the treatment of disaster-induced injury profiles will likely require specialized equipment and skills, the value added by defining an additional concept in this way is unclear and, in its current form, may undermine attempts to develop standardized and comparable metrics.
Kelen and McCarthy (2006, 1089) proposed an alternative approach, advocating the concept of “surge response capability” as a means to capture “the extent to which surge capacity (… resource availability and maximized management …) can accommodate the surge (… demand for resources …).” This, then, presents surge capability as a measure that enables the proportion of surge cases that the available resources can accommodate to be quantified. This might usefully inform mathematical modeling to estimate the existing capacity and to reveal potential shortfalls. This potential remains untested, since there has been little engagement with (or application of) this proposed definition. Any future attempt to use it would require care to ensure it did not result in an unduly technical approach, which could lose sight of the importance of governance structures and legal frameworks for effective coordination, a point we expand on later.
The Components of Surge Capacity
Given the variability of definitions and applications of the terms “surge” and “surge capacity,” there is a striking degree of consensus on what comprises the ability of a health system (or an individual hospital facility within a health system) to “respond to a sudden increase in patient care demands” (Hick et al. 2008b, S51). This consensus has emerged in recent years, largely in response to increasing dissatisfaction with prior attempts to conceptualize (and measure) surge capacity in terms of bed numbers alone. This was largely a result of initial uncritical engagements with the U.S. Department of Homeland Security's recommendation (HRSA 2004) that surge capacity entail the provision of five hundred beds for every one million people for acute infectious disease scenarios, and fifty beds for every one million people for noninfectious disease and trauma scenarios. Other recommendations that represent surge capacity as synonymous with bed numbers suggest an ability to expand bed numbers by 25 to 30 percent (Schultz and Stratton 2007).
Barbisch and Koenig were among the first to problematize relying on bed numbers as a proxy for surge capacity. They proposed a multicomponent approach that could take into account the interactions and dependencies necessarily entailed by an effective health systems’ response to a disaster- or pandemic-induced surge: “It is not simply beds or ventilators, but appropriately trained personnel (staff), comprehensive supplies and equipment (stuff), facilities (structure), and, of imperative importance, integrated policies and procedures (systems) to develop optimized sustainable surge capacity” (2006, 1099).
Their four-component approach (staff, stuff, structure, and systems) has since proved influential, though there has been a tendency for the fourth component, systems, to be neglected in favor of concentrating on “staff, stuff, and structures” (Barbisch 2005; Barbisch and Koenig 2006; Felland et al. 2008; Hick et al. 2008a, 2008b; Hota et al. 2010; Hotchkin and Rubinson 2008; Nager and Khanna 2009; Schultz and Koenig 2006; Welzel et al. 2010). Some authors have appended “space” (which overlaps with the other definitions of “structures”) to this trio of components. We next consider the content of each key component.
Staff
There is a wide degree of consensus regarding the central importance of maintaining sufficient staffing levels throughout a surge scenario's duration. The integration of personnel numbers into estimates of existing capacity and diagnostics of potential shortfalls is widely understood to imply a need for analysis that goes beyond measuring available staffing levels. Kaji, Koenig, and Bey's assertion that “one must plan for what people will do, rather than what one wants them to do” (2006, 1158) is represented in analyses and recommendations that incorporate estimates of staff absenteeism and develop means of intervening to reduce its extent (Qureshi et al. 2005; Rottman et al. 2010; Steffen, Masterson, and Christos 2004; Welzel et al. 2010). Several survey-based studies (Qureshi et al. 2005; Rottman et al. 2010; Steffen, Masterson, and Christos 2004; Welzel et al. 2010) have attempted to discern the extent to which hospital (medical and nonmedical) staff would be willing and able to report to work and/or to remain there indefinitely, given scenarios of varying severity and risk. Care duties and distance between home and place of work are most commonly cited as impediments to response, with scenarios involving contagions and radiation most undermining staff's willingness to report (Qureshi et al. 2005; Rottman et al. 2010; Steffen, Masterson, and Christos 2004; Welzel et al. 2010).
As Iserson and colleagues (2008, 352) comment, “No uncontroversial way to establish a threshold at which risk acceptance becomes a duty” has, to date, been identified. The extent to which a health professional's sense of duty, understood as a matter for personal conscience, will overcome his or her anxiety of risk represents a major source of unpredictability for surge capacity planning. An opt-out option enabling staff unwilling to work in conditions they judge too risky to personal (and family) health to instead undertake tangential, low-risk, duties was suggested (Qureshi et al. 2005; Rottman et al. 2010; Steffen, Masterson, and Christos 2004; Welzel et al. 2010) and was reportedly tried out in the 2003 outbreak of SARS in Toronto (Iserson et al. 2008). Any planned role for reallocation must, however, rely on the expectation that few staff members will move, in order that a sufficient number of frontline staff will remain. The extent to which this expectation is credible is highly contingent on the nature of the surge event and its wider context. The mutual impact on, and of, relations between colleagues undertaking frontline and peripheral duties also will likely affect the practicality of any such arrangement. Another relevant point with regard to uncertainty is the extent to which health care professionals who do remain in their posts may deviate from professional, and wider social, norms of acceptable behavior under conditions of severe strain, particularly if they are prolonged. While high-profile incidents of deviation from duty of care have received disproportionate attention in the wake of disasters (Alley 1992; Iserson et al. 2008; Kunzelman 2010), the wider evidence (Alley 1992; Iserson et al. 2008; Simonds and Sokol 2009) is that the expectation that health care professionals will respond to patients’ needs despite personal risks is realistic.
The majority of studies have concentrated on the need to mobilize hospital staff, but others are beginning to consider roles for other medical personnel, with a greater role advised for general practitioners (Fisher et al. 2011; Nap et al. 2006; Schultz and Stratton 2007), on the twin grounds that they can divert patients from hospitals (performing a prehospital triage role, whose viability is important to future research) and that they also may be in a position to intervene earlier to diminish the growth rate of the surge. A number of authors have suggested using the military medical corps to supplement civilian staffing levels (Bonnett et al. 2007; Hanley and Bogdan 2008; Hick et al. 2004; Miller, Randolph, and Patterson 2008; Tadmor, McManus, and Koenig 2006). This has been countered (Hotchkin and Rubinson 2008; Sariego 2006) with concerns that relying on military medical resources (in terms of facility space and equipment as well as personnel) may not be feasible, since in severe disaster scenarios or those implying security threats, such resources would be reserved for military support (Bonnett et al. 2007). A number of authors recommend using existing (and creating new) registers of medical personnel who are willing to volunteer their assistance in the event of a disaster- or pandemic-induced surge (Hanley and Bogdan 2008), although they note the difficulties of mobilization in scenarios in which transport infrastructure is damaged; the ability for local commitments to override more distant (but more urgent) ones in the event of a large-scale scenario; and unwillingness to leave family members in hazardous situations (Hanley and Bogdan 2008).
“Stuff.”
“Stuff,” or “equipment,” typically denotes a very wide range of items, including beds, ventilators, and other medical apparatus; pharmaceuticals; and a range of other essential resources. Despite concerns regarding an overreliance on bed numbers as an exclusive indicator of capacity, there remains a wide consensus that the “availability of empty beds (along with requisite medical staff)” forms “a fundamental component of hospitals’ surge capacity…during the first hours and days of a disaster” (DeLia and Wood 2008, 1688). While much of the interest in bed numbers has centered on the level of individual facilities, the need for coordination among facilities was highlighted in a recent retrospective study of the effectiveness of Asian countries’ pandemic surge capacity, which found a high incidence of “hospitals with no available ICU beds …managing severe patients in emergency rooms or general wards while in nearby hospitals ICU beds were available” (Fisher et al. 2011, 878). This implies a need for simple updatable systems to enable resource use and depletion to be tracked over time and space. With regard to pharmaceuticals and other medical supplies, the literature emphasizes that little stockpiling and the shift toward “just-in-time” supply chains will hurt surge capacity. In the U.S. system, the ability of hospitals and health systems to develop and maintain emergency stockpiles is widely acknowledged8 to be severely undermined by “economic pressures to run lean operations…interpreted as minimizing inventory rather than managing the costs of inventory” (Avery et al. 2008, 11). Reliance on overseas suppliers for pharmaceuticals (as well as other essential supplies) has been highlighted as potentially exacerbating supply-chain problems in the event that imports are compromised (Bartlett and Borio 2008a).
A recent article by Hick, Barbera, and Kelen (2009) proposes the following measures that can be taken if stockpiled pharmaceuticals and supplies are insufficient: “substitute; adapt; conserve; reuse; reallocate.” These recommendations highlight an important point regarding the standard of care that surge capacity should try to provide. Hick, Barbera, and Kelen (2009) propose a formalized model of scalable surge capacity composed of a three-tier system of escalation in resource utilization, from conventional, to contingency, to (ultimately) crisis phases. The first two phases imply minimal disruption to normal standards of patient care, but the third implies a reallocation of priorities from maintaining the usual standard of care to providing the best standard of care possible in exceptional circumstances. This approach has been adopted in the U.S. Institute of Medicine's recommendations (Hanfling et al. 2012) regarding shifts in acceptable standards of care for disaster scenarios. Despite this recent intervention, this remains an issue that the literature rarely addresses directly, but one that is essential to the conceptualization and measurement of surge capacity. It is a subject that future research should confront directly.
Structures/Space
Hospitals are the “structures” most commonly cited as components of surge capacity. A recent trend in the literature is to explore means of incorporating surge capacity infrastructure into plans for new hospitals and to revise existing plans (Hick, Barbera, and Kelen 2009; Joshi and Rys 2011; Schultz and Koenig 2006; Schultz and Stratton 2007). More ambitious recommendations for new “surge-proof” hospital facilities include the creation of “universal patient rooms configurable for any purpose,” modular equipment, 100 percent air filtration, built-in radiation protection, and blast-protected walls (Romano 2005). Such proposals involve a substantial lead time and can be extremely expensive. The widespread creation of reserve wards and the resurrection of decommissioned spaces have been proposed as a less disruptive alternative (Dayton et al. 2008), but their cost has also been questioned (Robertson and Cooper 2007).
A number of ways that hospitals can efficiently use nonmedical spaces (such as restaurants, waiting areas, and corridors) have also been proposed in the event of a surge. These suggestions raise issues regarding the point at which measures can no longer reasonably be said to constitute “surge capacity.” One question is whether measures such as the use of unstaffed beds and/or of corridors and restaurants as treatment spaces represent “surge capacity” or, conversely, are indicative of its exhaustion. This again relates to what standard of care is appropriate when planning for, and implementing, surge capacity and is an area that has not been explored sufficiently in the existing literature.
Other ideas for creating treatment areas beyond the hospital facility have also been suggested (Dayton et al. 2008; DeLia and Wood 2008; Hick et al. 2004; Hogg et al. 2006; Romano 2005; Schultz and Koenig 2006). To create more space, Hogg and colleagues (2006) proposed home-based hospital care, which might feed into widely discussed plans to discharge or transfer patients early (Dayton et al. 2008; DeLia and Wood 2008). A wide range of potential “alternate sites” (Dayton et al. 2008; DeLia and Wood 2008; Hick et al. 2004; Hogg et al. 2006) or “sites of opportunity”(Barbisch and Koenig 2006; Romano 2005) have also been proposed as means of supplementing hospital space. Ideally, these areas should be close to existing hospital facilities, and their utilization should be carefully planned (including drills and exercises).
Plans for constructing temporary surge facilities have also been recommended, with the experiences of Hong Kong and Canada in dealing with SARS cited as examples (Dayton et al. 2008). The technology exists for surge wards with airborne isolation facilities to be constructed and outfitted for inpatient care in a matter of days (Dayton et al. 2008). This idea could help in the management of a prolonged surge scenario but is of limited applicability to short-term events. A proposed solution to the lead time required is the creation of prefabricated modular mobile hospitals that could be transported where needed as an integrated truck trailer-bed unit. Such a model was tried in the United States in response to Hurricane Katrina (Voelker 2006). The costs of storing and maintaining the units, together with the difficulties of licensing them as treatment spaces (complicated in the U.S. scenario due to restrictions imposed by health insurance providers) are, however, cited as barriers (Voelker 2006).
Systems
Although only a minority (Barbera and Macintyre 2002; Barbera, Yeatts, and Macintyre 2009; Bradt et al. 2009; Burkle 2006; Burkle et al. 2007; Fisher et al. 2011; Hanfling 2006; Hick, Barbera, and Kelen 2009; Hick et al. 2008b; Kelen and McCarthy 2006; Rubinson et al. 2008) of authors retain Barbisch and Koenig's (2006) systems element of “surge capacity,” it is arguably the most important of the four proposed components. In response to its widespread neglect, Hick, Barbera, and Kelen (2009) emphasize that without it, the other factors “cannot be appropriately managed.” Research on the efficacy of surge responses to earlier high-profile events has consistently found the main limiting factor to be management systems not matching resources to needs (Fisher et al. 2011; Schultz and Koenig 2006). This in turn has been found to lead to an underutilization of available resources in both the United States (Barbera and Macintyre 2002; Barbera, Yeatts, and Macintyre 2009; Bradt et al. 2009; Burkle 2006; Burkle et al. 2007; Hanfling 2006; Hick, Barbera, and Kelen 2009; Hick et al. 2008b; Kelen and McCarthy 2006; Rubinson et al. 2008; Schultz and Koenig 2006) and Asia (Fisher et al. 2011). Hick, Barbera, and Kelen (2009) expanded their earlier work (Hick et al. 2004) to describe the systems component, subdividing it into a series of requirements for command, control, communications, coordination, continuity of operations, and community infrastructure. The neglect of the “systems” aspect seems to lie in its essential difference from the other constitutive aspects (staff, “stuff,” space) of surge capacity in regard to operationalization and measurement. One approach might therefore be to develop an independent identity for systems, perhaps by elaborating the distinction between capacity and capability (a point discussed later).
Although the concentration on facility provides a comprehensive and coherent account of the systems that need to be in place at this level, it may represent a shortcoming. Other authors have made a strong case for a model of “central proactive coordination,” on the grounds that “during an emergency, normal referral practices are unlikely to work” (Fisher et al. 2011, 878). Barbisch and Koenig (2006) propose modeling this wider health system response on the U.S. National Incident Management System. Its requirements (command and control, communications systems, stress management, preventive medicine and public health, laboratory, mortuary affairs and funeral services, personnel, logistics, transportation, and veterinary services) does not deviate significantly from the inventory developed by Hick, Barbera, and Kelen (2009) but identifies the health system rather than the facility as the locus of response coordination and management. This approach is increasingly gaining ground among authors wanting to situate surge capacity in a wider health systems approach (Avery et al. 2008; Bonnett et al. 2007; Burkle 2006; Burkle et al. 2007; Dayton et al. 2008; Estacio 2006; Felland et al. 2008; Kaji, Koenig, and Bey 2006; Phillips 2006; Schultz and Koenig 2006; Schultz and Stratton 2007; Stratton and Tyler 2006).
Metrics and Measurement of Surge Capacity
Research identifying and conceptualizing the essential components of surge capacity (and their interactions) has developed largely in isolation from empirical work to measure existing, and to model optimal, capacity. The difficulty of translating the complex interdependencies inherent in the concept of surge capacity has meant that measures and metrics have tended to concentrate on the “stuff” component and to depend on static and simplified proxies for its measurement. The challenges of operationalizing any complex phenomenon are widely acknowledged to be heightened in this instance by a widespread lack of robust and comparable data (DeLia 2006; DeLia and Wood 2008; Handler et al. 2006; Hick, Barbera, and Kelen 2009; Rodgers et al. 2006). Most of the empirical studies assessing the existing surge capacity have measured the availability of “staffed beds” at the facility, regional, and/or national level (DeLia and Wood 2008), with the debate around whether licensed beds or maintained beds provide the better proxy (Bagust, Place, and Posnett 1999; Schull 2006; Schultz and Stratton 2007).
Dissatisfied with bed-number proxies, others have looked at ways to use staff numbers to proxy surge capacity (Welzel et al. 2010). This introduces its own difficulties, with surveys (Qureshi et al. 2005; Rottman et al. 2010) indicating that there is no guarantee that recorded staff levels will translate into personnel willing to respond to disaster- or pandemic-induced surges. Schull has cautioned against the tendency to base predictions of “surge capacity” on analyses of existing bed and staffing numbers. He warns that “a simple count of available staffed beds, however calculated, may give a false sense of alarm” (Schull 2006, 389), since under surge conditions, changes in operations and standards of care will alter the relationship between staffed bed numbers and patient treatment, or a false sense of security, since facilities could become inoperable or diminished as a result of the surge-inducing event. There is wide consensus9 that freeing the baseline capacity and, particularly, beds through the early discharge of inpatients and the cancellation or postponement of elective procedures and admissions would be a key first step in the event of a surge scenario. More research is needed to estimate the proportion of baseline resource utilization that is amenable to triage in various contexts and scenarios. Attempts to simulate surge capacity have generally entailed a wider number of indicators and parameters than those for survey or observational data analyses (Bagust, Place, and Posnett 1999; Baker et al. 2011; Balcan et al. 2009; Barthel et al. 2011; Krumkamp et al. 2010; Nap et al. 2006; Scheulen et al. 2009; Shi et al. 2008; Sobieraj et al. 2007; Ten Eyck 2008).
Models and simulations have enabled a range of surge parameters (most frequently in relation to pandemic influenza scenarios) to be tested, factoring in the availability of equipment (including beds, key medicines, and personnel) and controlling for the anticipated age structure and treatment durations of patients, together with expected levels of staff absenteeism (Bagust, Place, and Posnett 1999; Baker et al. 2011; Balcan et al. 2009; Barthel et al. 2011; Krumkamp et al. 2010; Nap et al. 2006; Scheulen et al. 2009; Shi et al. 2008; Sobieraj et al. 2007; Ten Eyck 2008). Currently, capacity modeling for pandemic-induced surges in demand is at a more advanced stage than is that for natural hazard–induced disasters (Anderson, Hart, and Kainer 2003; Ercole 2009; Krumkamp et al. 2010; Menon, Taylor, and Ridley 2005). The complexity and sophistication of such models are increasing, with more recent work exploring the potential for integrating parameterized feed-back loops to account for the dynamics of resource depletion over the duration of the surge (Adisasmito et al. 2011; Krumkamp et al. 2010; Rudge et al. 2012). Table 2 summarizes the findings presented in this section and introduces the concept of “resource command,” a concept prior to “surge capacity,” in order to avoid some of the conflationary tendencies identified earlier.
TABLE 2.
Summary of Future Research Priorities
| Term | Content | Research Priorities |
|---|---|---|
| Surge | A sudden, unexpected escalation in health care needs induced by a public health emergency. May be (adopting Bonnet and colleagues’ terms) geographically “contained” or widespread (“population-based”). | • Analysis of the past hazard-event's characteristics, duration, and phased impacts and of key event-site characteristics (demographic, geographic, and infrastructural) to inform mathematical modeling to estimate the care needs for a range of surge scenarios. |
| Health system's resource command | The total stock of resources (staff, “stuff,” and structures/space) on which a health system can legitimately draw. We propose that this be composed of five categories: “critical baseline,” “available,” “increasable,” “triagable baseline,” and “mobilizable.” | • Development of data sources and methods to quantify a health system's national baseline resource stocks, disaggregated by relevant geographical and administrative unit (province, district, facility). |
| • Development of methods and data to indicate proportion of “baseline” resources amenable to triage. | ||
| • Development of user-friendly, updatable systems to enable resource use and depletion to be tracked over time and space. | ||
| Staff | • Elaboration of the emerging literature on staff willingness (and ability) to respond to a range of event scenarios. Survey and interviews with medical and nonmedical health personnel. | |
| • Assessment of the relevance of existing research on the impacts of stress and trauma on ability to undertake and perform professional duties. | ||
| • Assessment of the feasibility of volunteer registers. | ||
| “Stuff” | • Identification of the key physical resources (beds, ventilators, other medical apparatus, pharmaceuticals, non-pharmaceutical equipment) that best articulate “surge capacity.” The literature indicates beds to be a necessary but not sufficient proxy, but it is impractical to incorporate every resource in estimates and models. A balance should be sought. Evaluation of the risks posed by supply chains in the event that imports are compromised. | |
| Structures/space | • Development of a framework to assess available in-house “surge spaces.” | |
| • Identification of feasible modifications to medical facilities to increase surge capacity. | ||
| • Appraisal of past experiments with spillover spaces (schools, sports arenas, community centers, etc.). | ||
| Health system's surge capacity | The portion of health system resources (staff, stuff, and structures/space) available to meet surge needs (excludes “critical baseline” resources committed to meeting non-surge-related needs). | • Development of data sources and methods to enable a health system's baseline resource demand to be accurately assessed and/or modeled. Analysis should, when possible, be sensitive to temporal fluctuations in baseline demand. |
| Health system's surge capability | What can actually be achieved with a health system's surge capacity; the systems (defined broadly to include governance arrangements, legal frameworks, and precedents; bilateral and multilateral agreements and precedents; feasible and practiced procedures and plans; communications and transport logistics; and the staff's and the public's response) can be thought of as the conversion factors translating capacity into capability. | • Identification of potential legal and bureaucratic obstacles to resource, staff, and patient mobilization across geographical and administrative boundaries. |
| • Identification of best-practice triage procedures under surge conditions. | ||
| • Case study analyses drawing on academic literature, national and international appraisals and reports, key-informant interviews, and “survivor” surveys and interviews to identify procedural barriers to effective (and equitable) application of a health system's resources in past surge events. | ||
| • Analysis of written procedures and plans and of practical exercises and “drills” identifying potential obstacles to an effective future response. | ||
| • Surveys and interviews identifying public expectations and potential obstacles to compliance with health advice in the event of a surge event. |
Conclusions
To date, a major hurdle to the development of surge capacity as a coherent sphere of research has been the absence of consensus regarding the definitions and applications of key terms. This has impeded conceptual clarity and has undermined the development of convincing measurements and metrics. Despite these difficulties, “surge capacity” is an important concept for the study of health systems’ disaster and pandemic readiness and response, and it has far-reaching policy relevance for public health and health systems interventions and investments. Work is, however, needed to generate robust conceptual and analytical frameworks, along with innovations in data collection and methodological approaches. Another key area for future research is the addition of a temporal dimension. This would allow surge (and surge capacity) time lines to be explicitly understood to involve phased impacts. The incorporation of proximate and latent health care burdens can enable key sites of health system intervention to be identified.
While the development of general conceptual and analytical frameworks, together with improvements in data quality and methodological innovations for data analysis, can be of widespread applicability, there is a need to complement this with site- and scenario-specific findings. Despite the disproportionately high occurrence of surge-generating events in low- and middle-income countries, and their considerably heightened vulnerability to such events, the research on surge capacity to date has focused largely on high-income countries, principally the United States. Research on other countries (and particularly low-income countries) is urgently required. Any general conceptual and/or analytical model will need to incorporate geographical, temporal, and social contingencies in the outcomes, so that surge and surge capacity scenarios derive from, and inform, real-world events.
Implicit in the literature on surge capacity is the expectation that a severe, prolonged surge event, and the response it engenders, necessarily entails a diminished standard of care (Barbera, Yeatts, and Macintyre 2009; Bonnett et al. 2007; Bradt et al. 2009; Felland et al. 2008; Hick, Christian, and Sprung 2010; Hick et al. 2004, 2008b; Kaji, Koenig, and Bey 2006; Kaji, Koenig, and Lewis 2007; Moser et al. 2006; Phillips 2006; Rothman et al. 2006; Welzel et al. 2010). While the three-tier standard of care model proposed by Hick, Barbera, and Kelen (2009) explicitly confronts the objectives and implications of surge capacity, the wider tendency has been to incorporate such concerns as an aside or afterthought. Future research should build on their work, with the objective(s) of surge capacity—and the standard of care appropriate to those scenarios whose needs markedly exceed resources—forming the point of departure for conceptualization and analysis.
A potential way forward conceptually and analytically may lie in the development of the debates around the distinction between surge capacity and surge capability. Kelen and McCarthy's definition of surge capability (2006) and the wider debate over the centrality of the “systems” aspect (and concerns voiced recently regarding its neglect) bring to mind the long philosophical tradition (dating back to Aristotle's formulation in The Nichomachean Ethics; Aristotle 1980) of distinguishing between capacity (as command over resources) and capability (as the ability to convert resource command into a valued potential outcome). Based on this distinction, surge capacity (the portion of health system resources that can be dedicated to meeting surge needs) would be an important (but not necessarily the most important) indicator. Systems (understood in a broad sense) can then be understood as the conversion factors enabling surge capacity to translate into surge capability.
A coherent conceptual and analytical framework would be an important step toward creating a defined research space to enhance the development of evidence and to inform policy and practice. This move has been called for more widely in relation to health systems research (Balabanova et al. 2010; Coker, Atun, and McKee 2008) and is an area that might be addressed in future surge capacity research. Locating the health system in a wider social context will enable the systems component, widely identified as integral to surge capacity (Barbera and Macintyre 2002; Barbera, Yeatts, and Macintyre 2009; Bradt et al. 2009; Burkle 2006; Burkle et al. 2007; Fisher et al. 2011; Hanfling 2006; Hick, Barbera, and Kelen 2009; Hick et al. 2008b; Kelen and McCarthy 2006; Rubinson et al. 2008), to be meaningfully embedded in its wider governance, regulatory, and legislative environment.
Acknowledgments
This article is part of ongoing research funded by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
Endnotes
Hick et al. 2004; Higgins et al. 2004; Loretti, Leus, and Van Holsteijn 2001; Shapiro 2003; Taylor 2003.
Aharonson-Daniel, Klein, and Peleg 2006; Anderson, Hart, and Kainer 2003; Baker et al. 2011; Barnett, Dennis-Rouse, and Martinez 2009; Downey and Hebert 2010; Fisher et al. 2011; Hall 2007; Menon, Taylor, and Ridley 2005; Robertson and Cooper 2007; Rykken et al. 2005; Shi et al. 2008; Shih and Koenig 2006; Sprung et al. 2010; Traub, Bradt, and Joseph 2007; WHO 2006.
Ablah et al. 2008; Barthel et al. 2011; Bartlett 2006; Burkle 2006; Burkle et al. 2007; Hick et al. 2008a; Hogg et al. 2006; Hotchkin and Rubinson 2008; Kaji et al. 2008; McManus, Huebner, and Scheulen 2006; Miller, Randolph, and Patterson 2008; Nap et al. 2006, 2008; Romano 2005; Satterthwaite and Atkinson 2010; Shih and Koenig 2006; Sprung et al. 2010.
Ablah et al. 2008; Adini et al. 2006; Asplin, Flottemesch, and Gordon 2006; Avery et al. 2008; Bar-Dayan 2010; Barbera, Yeatts, and Macintyre 2009; Barnett, Dennis-Rouse, and Martinez 2009; Bayram, Zuabi, and Subbarao 2011; Binns, Sheppeard, and Staff 2010; Chaffee 2009; Davis et al. 2005; DeLia 2006; DeLia and Wood 2008; Falconer and O'Neill 2007; Farmer and Carlton 2006; Hick et al. 2008a; Higgins et al. 2004; Hodge et al. 2011; Ippolito, Puro, and Heptonstall 2006; Kaji, Koenig, and Lewis 2007; Kaji, Langford, and Lewis 2008; Kaji and Lewis 2006; Kanter and Moran 2007a; Kelen et al. 2006, 2009; Kraus, Levy, and Kelen 2007; Li, Huang, and Zhang 2008; Lynch, Koller, and Cocciardi 2008; Manley et al. 2006; Mechem 2007; Miller, Randolph, and Patterson 2008; Peleg and Kellermann 2009; Sandrock 2010; Satterthwaite and Atkinson 2010; Scarfone et al. 2010; Schull 2006; Schull et al. 2006; Schultz and Koenig 2006; Schultz and Stratton 2007; Shapiro 2003; Shi et al. 2008; Smith et al. 2011; Sobieraj et al. 2007; Sprung et al. 2010; Standards 2009; Ten Eyck 2008; Tran et al. 2009; Van Cleve et al. 2011; Voelker 2006; Welzel et al. 2010; Yi et al. 2010; Zhang, Meltzer, and Wortley 2006; Zilm et al. 2008.
Balcan et al. 2009; Barthel et al. 2011; Bradt et al. 2009; Christian et al. 2008; Custer et al. 2011; Daugherty and Rubinson 2011; Fernandez et al. 2008; Griffiths, Estipona, and Waterson 2011; Joshi and Rys 2011; Joynt et al. 2010; Kaiser et al. 2011; Kallman and Feury 2010; Kanter and Moran 2007b; Lee et al. 2009; Lynch, Koller, and Cocciardi 2008; Markovitz 2009; Mazowita 2006; Meltzer, McNeill, and Miller 2011; Mercer, Levis, and Reyes 2011; Nager and Khanna 2009; Nap et al. 2008, 2010; NCBI 2010a, 2010b; Rubinson et al. 2008; Sprung et al. 2010; Tandberg and Qualls 1994; Van Cleve et al. 2011.
ACEP 2006; AHRQ 2006; Baker et al. 2011; Balcan et al. 2009; Bartlett 2006; Bartlett and Borio 2008b; Bonnett et al. 2007; D'Aoust et al. 2008; Eastman et al. 2007; ECRI Institute 2008; Emery et al. 2009; Estacio 2006; Felland et al. 2008; Fisher et al. 2011; Greenko et al. 2010; Hall 2007; Hick, Barbera, and Kelen 2009; Hick, Christian, and Sprung 2010; Hick et al. 2004; Hirshberg et al. 2005; Hoard et al. 2005; Hodge, Gable, and Calves 2005a, 2005b; Hogg et al. 2006; Hsu et al. 2007; Kaji et al. 2008; Kaji, Koenig, and Bey 2006; Koh et al. 2006; Kort, Stuart, and Bontovics 2005; Krumkamp et al. 2010; Langabeer et al. 2009; Levin, Gebbie, and Qureshi 2007; Meredith et al. 2011; Monto et al. 2006; Moser et al. 2005, 2006; Potter and Brough 2004; Robertson and Cooper 2007; Romano 2005; Roszak et al. 2009; Rykken et al. 2005; Scheulen et al. 2009; Sefrin and Kuhnigk 2008; Severance 2002; Shih and Koenig 2006; Stratton and Tyler 2006; Swanson et al. 2010; Tadmor, McManus, and Koenig 2006; Taylor 2003; Watkins et al. 2011; WHO 2006.
Adini et al. 2006; Avery et al. 2008; Balcan et al. 2009; Bartlett 2006; Bartlett and Borio 2008a; Bonnett et al. 2007; Burkle 2006; Estacio 2006; Felland et al. 2008; Fisher et al. 2011; Hanfling 2006; Hanley and Bogdan 2008; Hick, Barbera, and Kelen 2009; Hick et al. 2004, 2008b; Higgins et al. 2004; Hota et al. 2010; Hotchkin and Rubinson 2008; Hsu et al. 2006, 2007; Kaji, Koenig, and Bey 2006; Kaji and Lewis 2006; Kort, Stuart, and Bontovics 2005; Krumkamp et al. 2010; Miller, Randolph, and Patterson 2008; Moser et al. 2005, 2006; Nap et al. 2006; Peleg and Kellermann 2009; Phillips 2006; Robertson and Cooper 2007; Romano 2005; Rottman et al. 2010; Schull 2006; Schultz and Koenig 2006; Shapiro 2003; Shih and Koenig 2006; Sprung et al. 2010; Tadmor, McManus, and Koenig 2006.
Avery et al. 2008; Baker et al. 2011; Dayton et al. 2008; DeLia and Wood 2008; Felland et al. 2008; Hanfling 2006; Hanley and Bogdan 2008; Hick, Barbera, and Kelen 2009; Hick et al. 2004; Hogg et al. 2006; Jenkins, O'Connor, and Cone 2006; Kaji, Koenig, and Bey 2006; Kelen et al. 2006; Krumkamp et al. 2010; Miller, Randolph, and Patterson 2008; Moser et al. 2006; Peleg and Kellermann 2009; Satterthwaite and Atkinson 2010; Schull 2006; Schull et al. 2006; Schultz and Stratton 2007; Sprung et al. 2010; Welzel et al. 2010.
References
- Ablah E, Nickels D, Hodle A, Wolf DJ. “Public Health Investigation”: Focus Group Study of a Regional Infectious Disease Exercise. Public Health Nursing. 2008;25:546–53. doi: 10.1111/j.1525-1446.2008.00742.x. [DOI] [PubMed] [Google Scholar]
- ACEP (American College of Emergency Physicians) Healthcare System Surge Capacity Recognition, Preparedness, and Response. Irving, TX: 2006. [Google Scholar]
- Adini B, Goldberg A, Laor D, Cohen R, Zadok R, Bar-Dayan Y. Assessing Levels of Hospital Emergency Preparedness. Prehospital and Disaster Medicine. 2006;21:451–57. doi: 10.1017/s1049023x00004192. [DOI] [PubMed] [Google Scholar]
- Adisasmito W, Hunter BM, Krumkamp R, Latief K, Rudge JW, Hanvoravongchai P, Coker R. Pandemic Influenza and Health System Resource Gaps in Bali: An Analysis through a Resource Transmission Dynamics Model. Asia Pacific Journal of Public Health. 2011;20:1–21. doi: 10.1177/1010539511421365. [DOI] [PubMed] [Google Scholar]
- ADRC (Asian Disaster Reduction Centre) Natural Disaster Data Book 2009: An Analytic Overview. 2009. Kobe.
- Aharonson-Daniel L, Klein Y, Peleg K. Suicide Bombers Form a New Injury Profile. Annals of Surgery. 2006;244:1018–23. doi: 10.1097/01.sla.0000225355.06362.0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AHRQ (Agency for Healthcare Research and Quality) Addressing Surge Capacity in a Mass Casualty Event: Surge Capacity and Health System Preparedness. Rockville, MD: 2006. [Google Scholar]
- Alley E. Overcoming the Mythology of Disaster. In: Masellis M, Gunn WA, editors. The Management of Mass Burn Casualties and Fire Disasters. Hingham, MA: Kluwer Academic Publishers; 1992. pp. 19–23. [Google Scholar]
- Anderson TA, Hart GK, Kainer MA. Pandemic Influenza: Implications for Critical Care Resources in Australia and New Zealand. Journal of Critical Care. 2003;18:173–80. doi: 10.1016/j.jcrc.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Aristotle . In: The Nicomachean Ethics. Ross D, translator. Oxford: Oxford University Press; 1980. [Google Scholar]
- Asplin BR, Flottemesch TJ, Gordon BD. Developing Models for Patient Flow and Daily Surge Capacity Research. Academic Emergency Medicine. 2006;13:1109–13. doi: 10.1197/j.aem.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Avery GH, Lawley M, Garret S, Caldwell B, Durr MP, Abraham D, Lin F, DeLaurentis P-CC, Peralta ML, Russell A, Kopach-Conrad RA, Ignacio LM, Sandino R, Staples DJ. Planning for Pandemic Influenza: Lessons from the Experiences of Thirteen Indiana Counties. Journal of Homeland Security and Emergency Management. 2008;5(1):1–24. [Google Scholar]
- Bagust A, Place M, Posnett J. Dynamics of Bed Use in Accommodating Emergency Admissions: Stochastic Simulation Model. BMJ. 1999;319:155–58. doi: 10.1136/bmj.319.7203.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker P, Sun J, Morris J, Dines A. Epidemiologic Modeling with Flusurge for Pandemic (H1N1) 2009 Outbreak, Queensland, Australia. Emerging Infectious Diseases. 2011;17:1608–14. doi: 10.3201/eid1709.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balabanova D, McKee M, Mills A, Walt G, Haines A. What Can Global Health Institutions Do to Help Strengthen Health Systems in Low Income Countries? Health Research Policy and Systems. 2010;8:1478–1505. doi: 10.1186/1478-4505-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balcan D, Colizza V, Singer AC, Chouaid C, Hu H, Gonçalves B, Bajardi P, Poletto C, Ramasco JJ, Perra N, Tizzoni M, Paolotti D, Van den Broeck W, Valleron A, Vespignani A. Modeling the Critical Care Demand and Antibiotics Resources Needed during the Fall 2009 Wave of Influenza A(H1N1) Pandemic. PLoS currents. 2009;7(1):1133. doi: 10.1371/currents.RRN1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Dayan Y. Editorial Comments—Psychological Effects of Patient Surge in Large-Scale Emergencies: A Quality Improvement Tool for Hospital and Clinic Capacity Planning and Response. Prehospital and Disaster Medicine. 2010;25:115–16. doi: 10.1017/s1049023x00007822. [DOI] [PubMed] [Google Scholar]
- Barbera J, Macintyre A. Medical and Health Incident Management System: A Comprehensive Functional System Description for Mass Casualty Medical and Health Incident Management. Washington, DC: George Washington University Institute for Crisis, Disaster, and Risk Management; 2002. [Google Scholar]
- Barbera J, Yeatts D, Macintyre A. Challenge of Hospital Emergency Preparedness: Analysis and Recommendations. Disaster Medicine and Public Health Preparedness. 2009;3:S74–S82. doi: 10.1097/DMP.0b013e31819f754c. [DOI] [PubMed] [Google Scholar]
- Barbisch D. Regional Responses to Terrorism and Other Medical Disasters: Developing Sustainable Surge Capacity. In: Johnson JA, Ludlow GR, Jones WJ, editors. Community Preparedness and Response to Terrorism. Westport, CT: Praeger; 2005. pp. 77–88. [Google Scholar]
- Barbisch D, Koenig K. Understanding Surge Capacity: Essential Elements. Academic Emergency Medicine. 2006;13:1098–1102. doi: 10.1197/j.aem.2006.06.041. [DOI] [PubMed] [Google Scholar]
- Barnett J, Dennis-Rouse M, Martinez V. Wildfire Disaster Leads to Facilities Evacuation. Orthopaedic Nursing. 2009;28:17–20. doi: 10.1097/01.NOR.0000345849.32424.0a. [DOI] [PubMed] [Google Scholar]
- Barthel ER, Pierce JR, Goodhue CJ, Ford HR, Grikscheit TC, Upperman JS. Availability of a Pediatric Trauma Center in a Disaster Surge Decreases Triage Time of the Pediatric Surge Population: A Population Kinetics Model. Theoretical Biology and Medical Modelling. 2011;8:38. doi: 10.1186/1742-4682-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett JG. Planning for Avian Influenza. Annals of Internal Medicine. 2006;145:141–44. doi: 10.7326/0003-4819-145-2-200607180-00133. [DOI] [PubMed] [Google Scholar]
- Bartlett JG, Borio L. The Current Status of Planning for Pandemic Influenza and Implications for Health Care Planning in the United States. Clinical Infectious Diseases. 2008a;46:919–25. doi: 10.1086/528799. [DOI] [PubMed] [Google Scholar]
- Bartlett JG, Borio L. Healthcare Epidemiology: The Current Status of Planning for Pandemic Influenza and Implications for Health Care Planning in the United States. Clinical Infectious Disease. 2008b;46:919–25. doi: 10.1086/528799. [DOI] [PubMed] [Google Scholar]
- Bayram JD, Zuabi S, Subbarao I. Disaster Metrics: Quantitative Benchmarking of Hospital Surge Capacity in Trauma-Related Multiple Casualty Events. Disaster Medicine and Public Health Preparedness. 2011;5:117–24. doi: 10.1001/dmp.2010.19. [DOI] [PubMed] [Google Scholar]
- BEH (Bundnis Entwicklung Hilft) World Risk Report 2011. Berlin: Bundnis Entwicklung Hilft (Alliance Development Works); 2012. [Google Scholar]
- Binns PL, Sheppeard V, Staff MP. Isolation and Quarantine during Pandemic (H1N1) 2009 Influenza in NSW: The Operational Experience of Public Health Units. New South Wales Public Health Bulletin. 2010;21:10–15. doi: 10.1071/NB09036. [DOI] [PubMed] [Google Scholar]
- Bonnett CJ, Peery BN, Cantrill SV, Pons PT, Haukoos JS, McVaney KE, Colwell CB. Surge Capacity: A Proposed Conceptual Framework. American Journal of Emergency Medicine. 2007;25:297–306. doi: 10.1016/j.ajem.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Bourque LB, Siegel JM, Kano M, Wood MM. Morbidity and Mortality Associated with Disasters. In: Rodriguez H, Quarantelli EL, Dynes R, Anderson WA, editors. Handbook of Disaster Research. New York: Springer; 2007. pp. 97–112. [Google Scholar]
- Bradt DA, Aitken P, FitzGerald G, Swift R, O'Reilly G, Bartley B. Emergency Department Surge Capacity: Recommendations of the Australasian Surge Strategy Working Group. Academic Emergency Medicine. 2009;16:1350–58. doi: 10.1111/j.1553-2712.2009.00501.x. [DOI] [PubMed] [Google Scholar]
- Burkle FM., Jr Population-Based Triage Management in Response to Surge-Capacity Requirements during a Large-Scale Bioevent Disaster. Academic Emergency Medicine. 2006;13:1118–29. doi: 10.1197/j.aem.2006.06.040. [DOI] [PubMed] [Google Scholar]
- Burkle FM, Jr, Hsu EB, Loehr M, Christian MD, Markenson D, Rubinson L, Archer FL. Definition and Functions of Health Unified Command and Emergency Operations Centers for Large-Scale Bioevent Disasters within the Existing ICS. Disaster Medicine and Public Health Preparedness. 2007;1:135–41. doi: 10.1097/DMP.0b013e3181583d66. [DOI] [PubMed] [Google Scholar]
- Chaffee M. Willingness of Health Care Personnel to Work in a Disaster: An Integrative Review of the Literature. Disaster Medicine and Public Health Preparedness. 2009;3:42–56. doi: 10.1097/DMP.0b013e31818e8934. [DOI] [PubMed] [Google Scholar]
- Christian MD, Devereaux AV, Dichter JR, Geiling JA, Rubinson L. Definitive Care for the Critically Ill during a Disaster: Current Capabilities and Limitations. A Task Force for Mass Critical Care Summit Meeting, January 2 and 27, 2007, Chicago. Chest. 2008;133:8S–17S. doi: 10.1378/chest.07-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker RJ, Atun RA, McKee M. Health Systems and the Challenge of Communicable Diseases: Experiences from Europe and Latin America. New York: Open University Press; 2008. [Google Scholar]
- Custer JW, Watson CM, Dwyer J, Kaczka DW, Simon BA, Easley RB. Critical Evaluation of Emergency Stockpile Ventilators in an In Vitro Model of Pediatric Lung Injury. Pediatric Critical Care Medicine. 2011;12(6):357–61. doi: 10.1097/PCC.0b013e31820ab891. [DOI] [PubMed] [Google Scholar]
- D'Aoust MA, Lavoie PO, Couture MM, Trepanier S, Guay JM, Dargis M, Mongrand S, Landry N, Ward BJ, Vézina LP. Influenza Virus-Like Particles Produced by Transient Expression in Nicotiana Benthamiana Induce a Protective Immune Response against a Lethal Viral Challenge in Mice. Plant Biotechnology Journal. 2008;6:930–40. doi: 10.1111/j.1467-7652.2008.00384.x. [DOI] [PubMed] [Google Scholar]
- Daugherty EL, Rubinson L. Preparing Your Intensive Care Unit to Respond in Crisis: Considerations for Critical Care Clinicians. Critical Care Medicine. 2011;39:2534–39. doi: 10.1097/CCM.0b013e3182326440. [DOI] [PubMed] [Google Scholar]
- Davis DP, Poste JC, Hicks T, Polk D, Rymer TE, Jacoby I. Hospital Bed Surge Capacity in the Event of a Mass-Casualty Incident. Prehospital and Disaster Medicine. 2005;20:169–76. doi: 10.1017/s1049023x00002405. [DOI] [PubMed] [Google Scholar]
- Dayton C, Ibrahim J, Augenbraun M, Brooks S, Mody K, Holford D, Roblin P, Arquilla B. Integrated Plan to Augment Surge Capacity. Prehospital and Disaster Medicine. 2008;23:113–19. doi: 10.1017/s1049023x00005719. [DOI] [PubMed] [Google Scholar]
- DeLia D. Annual Bed Statistics Give a Misleading Picture of Hospital Surge Capacity. Annals of Emergency Medicine. 2006;48:384–88. doi: 10.1016/j.annemergmed.2006.01.024. [DOI] [PubMed] [Google Scholar]
- DeLia D, Wood E. TRENDS The Dwindling Supply of Empty Beds: Implications for Hospital Surge Capacity. Health Affairs. 2008;27:1688–94. doi: 10.1377/hlthaff.27.6.1688. [DOI] [PubMed] [Google Scholar]
- Dobbs R, Smit S, Remes J, Manyika J, Roxburgh C, Restrepo A. Urban World: Mapping the Economic Power of Cities. Seoul: McKinsey Global Institute; 2011. [Google Scholar]
- DoH (Department of Health) Pandemic Flu: Managing Demand and Capacity in Health Care Organizations (Surge) London: 2009. [Google Scholar]
- Downey E, Hebert A. Best Practices of Hospital Security Planning for Patient Surge—A Comparative Analysis of Three National Systems. Journal of Healthcare Protection Management. 2010;26:55–74. [PubMed] [Google Scholar]
- Eastman AL, Rinnert KJ, Nemeth IR, Fowler RL, Minei JP. Alternate Site Surge Capacity in Times of Public Health Disaster Maintains Trauma Center and Emergency Department Integrity: Hurricane Katrina. Journal of Trauma-Injury Infection and Critical Care. 2007;63:253–57. doi: 10.1097/TA.0b013e3180d0a70e. [DOI] [PubMed] [Google Scholar]
- ECRI Institute. Planning Together: Community and Hospital Response to Disasters. Healthcare Hazard Management Monitor. 2008;21(9):1–9. [PubMed] [Google Scholar]
- Emery RJ, Sprau DD, Morecook RC, Herbold J. Surge Capacity Volunteer Perspectives on a Field Training Exercise Specifically Designed to Emphasize Likely Roles during a Disaster Response. Health Physics. 2009;97:S155–60. doi: 10.1097/HP.0b013e3181aeb3d5. [DOI] [PubMed] [Google Scholar]
- Emmens B, Houghton R. Understanding Surge Capacity within International Agencies. Humanitarian Exchange Magazine. 2008 Issue 39, June. Available at http://www.odihpn.org/humanitarian-exchange-magazine/issue-39/understanding-surge-capacity-within-international-agencies (accessed September 26, 2012) [Google Scholar]
- Ercole A. Modelling the Impact of an Influenza A H1N1 Pandemic on Critical Care Demand from Early Pathogenicity Data: The Case for Sentinel Reporting. Anaesthesia. 2009;64:937–41. doi: 10.1111/j.1365-2044.2009.06070.x. [DOI] [PubMed] [Google Scholar]
- Estacio PL. Surge Capacity for Health Care Systems: Early Detection, Methodologies, and Process. Academic Emergency Medicine. 2006;13:1135–37. doi: 10.1197/j.aem.2006.07.018. [DOI] [PubMed] [Google Scholar]
- EU (European Union) A Community Approach on the Prevention of Natural and Man-Made Disasters. Brussels: Commission of the European Communities; 2009. [Google Scholar]
- EU (European Union) Implementation Plan of the EU Strategy for Supporting Disaster Risk Reduction in Developing Countries 2011–2014. Brussels: Council of the European Union; 2011. [Google Scholar]
- Falconer M, O'Neill D. Age-Proofing Hospital Surge Capacity. The Lancet. 2007;369:822–23. doi: 10.1016/S0140-6736(07)60400-0. [DOI] [PubMed] [Google Scholar]
- Farmer JC, Carlton PK. Providing Critical Care during a Disaster: The Interface between Disaster Response Agencies and Hospitals. Society of Critical Care Medicine. 2006;34(3):56–59. doi: 10.1097/01.CCM.0000199989.44467.2E. [DOI] [PubMed] [Google Scholar]
- Felland LE, Katz A, Liebhaber A, Cohen GR. Developing Health System Surge Capacity: Community Efforts in Jeopardy. HSC Research Brief. 2008 no. 5. Available at http://www.hschange.com/CONTENT/991/ (accessed September 26, 2012) [PubMed] [Google Scholar]
- Fernandez JB, Glotzer DL, Triola MM, Psoter WJ. A Unique Role for Dental School Faculty: Telephone Triage Training and Integration into a Health Department's Emergency Response Planning. American Journal of Disaster Medicine. 2008;3:141–46. [PubMed] [Google Scholar]
- Fisher D, Hui DS, Gao Z, Lee C, Oh M-D, Cao B, Hien TT, Patlovich K, Farrar J. Pandemic Response Lessons from Influenza H1N1 2009 in Asia. Respirology. 2011;16:876–82. doi: 10.1111/j.1440-1843.2011.02003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenko JA, Armellino D, Mahoney M, Haran MA, Nullet S, Ginocchio C, Nagleberg J, Pardo S, Edwards B. Novel Influenza A (H1N1) Outbreak Response: An Exercise in Health System Preparedness. American Journal of Infection Control. 2010;38(5):22. [Google Scholar]
- Griffiths JL, Estipona A, Waterson JA. A Framework for Physician Activity during Disasters and Surge Events. American Journal of Disaster Medicine. 2011;6:39–46. [PubMed] [Google Scholar]
- Guha-Sapir D, Vos F, Below V, Ponserre P. Annual Disaster Statistical Review 2010: The Numbers and Trends. Brussels: Centre for Research on the Epidemiology of Disasters (CRED); 2011. [Google Scholar]
- Hall RC. The 1995 Kikwit Ebola Outbreak—Model of Virus Properties on System Capacity and Function: A Lesson for Future Viral Epidemics. American Journal of Disaster Medicine. 2007;2:270–76. [PubMed] [Google Scholar]
- Handler JA, Gillam M, Kirsch TD, Feied CF. Metrics in the Science of Surge. Academic Emergency Medicine. 2006;13:1173–78. doi: 10.1197/j.aem.2006.07.006. [DOI] [PubMed] [Google Scholar]
- Hanfling D. Equipment, Supplies, and Pharmaceuticals: How Much Might It Cost to Achieve Basic Surge Capacity? Academic Emergency Medicine. 2006;13:1232–37. doi: 10.1197/j.aem.2006.03.567. [DOI] [PubMed] [Google Scholar]
- Hanfling D, Altevogt B, Viswanathan K, Gostin L. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington, DC: Institute of Medicine; 2012. [Google Scholar]
- Hanley ME, Bogdan GM. Mechanical Ventilation in Mass Casualty Scenarios. Augmenting Staff: Project XTREME. Respiratory Care. 2008;53:176–88. [PubMed] [Google Scholar]
- Hick J, Barbera JA, Kelen GD. Refining Surge Capacity: Conventional, Contingency, and Crisis Capacity. Disaster Medicine and Public Health Preparedness. 2009;3:S59–S67. doi: 10.1097/DMP.0b013e31819f1ae2. [DOI] [PubMed] [Google Scholar]
- Hick J, Chipman J, Loppnow G, Conterato M, Roberts D, Heegaard WG, Beilman G, Clark M, Pohland J, Ho JD, Brunette DD, Clinton JE. Hospital Response to a Major Freeway Bridge Collapse. Disaster Medicine and Public Health Preparedness. 2008a;2:S11–S16. doi: 10.1097/DMP.0b013e31817196bf. [DOI] [PubMed] [Google Scholar]
- Hick J, Christian MD, Sprung CL. Chapter 2. Surge Capacity and Infrastructure Considerations for Mass Critical Care. Recommendations and Standard Operating Procedures for Intensive Care Unit and Hospital Preparations for an Influenza Epidemic or Mass Disaster. Intensive Care Medicine. 2010;36(suppl. 1):S11–S20. doi: 10.1007/s00134-010-1761-4. [DOI] [PubMed] [Google Scholar]
- Hick J, Hanfling D, Burstein JL, DeAtley C, Barbisch D, Bogdan GM, Cantrill S. Health Care Facility and Community Strategies for Patient Care Surge Capacity. Annals of Emergency Medicine. 2004;44:253–61. doi: 10.1016/j.annemergmed.2004.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hick J, Koenig KL, Barbisch D, Bey TA. Surge Capacity Concepts for Health Care Facilities: The CO-S-TR Model for Initial Incident Assessment. Disaster Medicine and Public Health Preparedness. 2008b;2:S51–S57. doi: 10.1097/DMP.0b013e31817fffe8. [DOI] [PubMed] [Google Scholar]
- Higgins W, Wainright C, Lu N, Carrico R. Assessing Hospital Preparedness Using an Instrument Based on the Mass Casualty Disaster Plan Checklist: Results of a Statewide Survey. American Journal of Infection Control. 2004;32:327–32. doi: 10.1016/j.ajic.2004.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshberg A, Scott BG, Granchi T, Wall MJ, Mattox KL, Stein M. How Does Casualty Load Affect Trauma Care in Urban Bombing Incidents? A Quantitative Analysis. Journal of Trauma-Injury Infection and Critical Care. 2005;58:686–93. doi: 10.1097/01.ta.0000159243.70507.86. [DOI] [PubMed] [Google Scholar]
- Hoard M, Homer J, Manley W, Furbee P, Haque A, Helmkamp J. Systems Modeling in Support of Evidence-Based Disaster Planning for Rural Areas. International Journal of Hygiene and Environmental Health. 2005;208:117–25. doi: 10.1016/j.ijheh.2005.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge JG, Anderson ED, Kirsch TD, Kelen GD. Facilitating Hospital Emergency Preparedness: Introduction of a Model Memorandum of Understanding. Disaster Medicine and Public Health Preparedness. 2011;5:54–61. doi: 10.1001/10-v4n2-hsf10003. [DOI] [PubMed] [Google Scholar]
- Hodge JG, Gable LA, Calves SH. Volunteer Health Professionals and Emergencies: Assessing and Transforming the Legal Environment. Biosecurity and Bioterrorism-Biodefense Strategy Practice and Science. 2005a;3:216–23. doi: 10.1089/bsp.2005.3.216. [DOI] [PubMed] [Google Scholar]
- Hodge JG, Gable LA, Calves SH. The Legal Framework for Meeting Surge Capacity through the Use of Volunteer Health Professionals during Public Health Emergencies and Other Disasters. Journal of Contemporary Health Law and Policy. 2005b;22:5–71. [PubMed] [Google Scholar]
- Hogg W, Lemelin J, Huston P, Dahrouge S. Increasing Epidemic Surge Capacity with Home-Based Hospital Care. Canadian Family Physician. 2006;52:563–64. [PMC free article] [PubMed] [Google Scholar]
- Hota S, Fried E, Burry L, Stewart TE, Christian MD. Preparing Your Intensive Care Unit for the Second Wave of H1N1 and Future Surges. Critical Care Medicine. 2010;38:E110–E119. doi: 10.1097/CCM.0b013e3181c66940. [DOI] [PubMed] [Google Scholar]
- Hotchkin DL, Rubinson L. Modified Critical Care and Treatment Space Considerations for Mass Casualty Critical Illness and Injury. Respiratory Care. 2008;53:67–74. [PubMed] [Google Scholar]
- Houghton R, Emmens B. Surge Capacity in the Humanitarian Relief and Development Sector: A Review of Surge Capacity and Surge Capacity Mechanisms within International NGOs. London: People in Aid; 2007. Available at http://www.ecbproject.org/downloads/resources/surge-final.pdf (accessed September 26, 2012) [Google Scholar]
- HRSA (Health Resource and Service Administration) U.S. Department of Health and Human Services: National Bioterrorism Hospital Preparedness Program (NBHPP) Washington, DC: 2004. [Google Scholar]
- Hsu EB, Casani JA, Romanosky A, Millin MG, Singleton CM, Donohue J, Feroli ER, Rubin M, Subbarao I, Whyne DM, Kelen G. Are Regional Hospital Pharmacies Prepared for Public Health Emergencies? Biosecurity and Bioterrorism-Biodefense Strategy Practice and Science. 2006;4:237–43. doi: 10.1089/bsp.2006.4.237. [DOI] [PubMed] [Google Scholar]
- Hsu EB, Casani JA, Romanosky A, Millin MG, Singleton CM, Donohue J, Feroli ER, Rubin M, Subbarao I, Whyne DM, Snodgrass TD, Kelen GD. Critical Assessment of Statewide Hospital Pharmaceutical Surge Capabilities for Chemical, Biological, Radiological, Nuclear, and Explosive Incidents. Prehospital and Disaster Medicine. 2007;22:214–18. doi: 10.1017/s1049023x00004696. [DOI] [PubMed] [Google Scholar]
- Ippolito G, Puro V, Heptonstall J. Hospital Preparedness to Bioterrorism and Other Infectious Disease Emergencies. Cellular and Molecular Life Sciences. 2006;63:2213–22. doi: 10.1007/s00018-006-6309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iserson KV, Heine CE, Larkin GL, Moskop JC, Baruch J, Aswegan AL. Fight or Flight: The Ethics of Emergency Physician Disaster Response. Annals of Emergency Medicine. 2008;51:345–53. doi: 10.1016/j.annemergmed.2007.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins JL, O'Connor RE, Cone DC. Differentiating Large-Scale Surge versus Daily Surge. Academic Emergency Medicine. 2006;13:1169–72. doi: 10.1197/j.aem.2006.07.022. [DOI] [PubMed] [Google Scholar]
- Jones KE, Patel N, Levy M, Storeygard A, Balk D, Gittleman J, Daszak P. Global Trends in Emerging Infectious Diseases. Nature. 2008;451:990–93. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi AJ, Rys MJ. Study on the Effect of Different Arrival Patterns on an Emergency Department's Capacity Using Discrete Event Simulation. International Journal of Industrial Engineering-Theory Applications and Practice. 2011;18:40–50. [Google Scholar]
- Joynt GM, Loo S, Taylor BL, Margalit G, Christian MD, Sandrock C, Danis M, Leoniv Y, Sprung CL. Chapter 3. Coordination and Collaboration with Interface Units. Recommendations and Standard Operating Procedures for Intensive Care Unit and Hospital Preparations for an Influenza Epidemic or Mass Disaster. Intensive Care Medicine. 2010;36(suppl. 1):S21–S31. doi: 10.1007/s00134-010-1762-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser HE, Barnett DJ, Hayanga AJ, Brown ME, Filak AT. Medical Students’ Participation in the 2009 Novel H1N1 Influenza Vaccination Administration: Policy Alternatives for Effective Student Utilization to Enhance Surge Capacity in Disasters. Disaster Medicine and Public Health Preparedness. 2011;5:150–53. doi: 10.1001/dmp.2011.33. [DOI] [PubMed] [Google Scholar]
- Kaji A, Bair A, Okuda Y, Kobayashi L, Khare R, Vozenilek J. Defining Systems Expertise: Effective Simulation at the Organizational Level—Implications for Patient Safety, Disaster Surge Capacity, and Facilitating the Systems Interface. Academic Emergency Medicine. 2008;15:1098–1103. doi: 10.1111/j.1553-2712.2008.00209.x. [DOI] [PubMed] [Google Scholar]
- Kaji A, Koenig K, Bey T. Surge Capacity for Healthcare Systems: A Conceptual Framework. Academic Emergency Medicine. 2006;13:1157–59. doi: 10.1197/j.aem.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Kaji A, Koenig K, Lewis R. Current Hospital Disaster Preparedness. JAMA. 2007;298:2188–90. doi: 10.1001/jama.298.18.2188. [DOI] [PubMed] [Google Scholar]
- Kaji A, Langford V, Lewis R. Assessing Hospital Disaster Preparedness: A Comparison of an On-Site Survey, Directly Observed Drill Performance, and Video Analysis of Teamwork. Annals of Emergency Medicine. 2008;52:195–201. doi: 10.1016/j.annemergmed.2007.10.026. [DOI] [PubMed] [Google Scholar]
- Kaji A, Lewis R. Hospital Disaster Preparedness in Los Angeles County. Academic Emergency Medicine. 2006;13:1198–1203. doi: 10.1197/j.aem.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Kallman M, Feury KJ. Preparing for Patient Surge in Emergency Departments during a Disaster. Journal of Emergency Nursing. 2010;37:184–85. doi: 10.1016/j.jen.2010.11.012. [DOI] [PubMed] [Google Scholar]
- Kanter RK, Moran JR. Hospital Emergency Surge Capacity: An Empiric New York Statewide Study. Annals of Emergency Medicine. 2007a;50:314–19. doi: 10.1016/j.annemergmed.2006.10.019. [DOI] [PubMed] [Google Scholar]
- Kanter RK, Moran JR. Pediatric Hospital and Intensive Care Unit Capacity in Regional Disasters: Expanding Capacity by Altering Standards of Care. Pediatrics. 2007b;119:94–100. doi: 10.1542/peds.2006-1586. [DOI] [PubMed] [Google Scholar]
- Kelen GD, Kraus CK, McCarthy ML, Bass E, Hsu EB, Li G, Scheulen JJ, Shahan JB, Brill JD, Green GB. Inpatient Disposition Classification for the Creation of Hospital Surge Capacity: A Multiphase Study. The Lancet. 2006;368:1984–90. doi: 10.1016/S0140-6736(06)69808-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelen GD, McCarthy ML. The Science of Surge. Academic Emergency Medicine. 2006;13:1089–94. doi: 10.1197/j.aem.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Kelen GD, McCarthy ML, Kraus CK, Ding R, Hsu EB, Li G, Shahan JB, Scheulen JJ, Green GB. Creation of Surge Capacity by Early Discharge of Hospitalized Patients at Low Risk for Untoward Events. Disaster Medicine and Public Health Preparedness. 2009;3:S10–S16. doi: 10.1097/DMP.0b013e3181a5e7cd. [DOI] [PubMed] [Google Scholar]
- Koh HK, Shei AC, Bataringaya J, Burstein J, Biddinger PD, Crowther MS, Serino RA, Cohen BR, Nick GA, Leary MC, Judge CM, Campbell PH, Brinsfield KH, Auerbach J. Building Community-Based Surge Capacity through a Public Health and Academic Collaboration: The Role of Community Health Centers. Public Health Reports. 2006;121:211–16. doi: 10.1177/003335490612100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kort R, Stuart AJ, Bontovics E. Ensuring a Broad and Inclusive Approach: A Provincial Perspective on Pandemic Preparedness. Canadian Journal of Public Health. 2005;96:409–11. doi: 10.1007/BF03405178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus CK, Levy F, Kelen GD. Lifeboat Ethics: Considerations in the Discharge of Inpatients for the Creation of Hospital Surge Capacity. Disaster Medicine and Public Health Preparedness. 2007;1:51–56. doi: 10.1097/DMP.0b013e318065c4ca. [DOI] [PubMed] [Google Scholar]
- Krumkamp R, Kretzschmar M, Rudge JW, Ahmad A, Hanvoravongchai P, Westenhoefer J, Stein M, Putthasri W, Coker R. Health Service Resource Needs for Pandemic Influenza in Developing Countries: A Linked Transmission Dynamics, Interventions and Resource Demand Model. Epidemiology and Infection. 2010;139:59–67. doi: 10.1017/S0950268810002220. [DOI] [PubMed] [Google Scholar]
- Kunzelman M. Trial Opens in Katrina Hospital Death Case. Bioscience Technology. 2010 January 12. Available at http://biosciencetechnology.com/News/FeedsAP/2010/01/trial-opens-in-katrina-hospital-death-case/ (accessed September 26, 2012) [Google Scholar]
- Langabeer JR, II, DelliFraine JL, Tyson S, Emert JM, Herbold J. Investment, Managerial Capacity, and Bias in Public Health Preparedness. American Journal of Disaster Medicine. 2009;4:207–15. [PubMed] [Google Scholar]
- Lee WH, Ghee C, Wu KH, Hung SC. Barriers to Surge Capacity of an Overcrowded Emergency Department for a Serious Foodborne Disease Outbreak. Emergency Medicine Journal. 2009;27:779–83. doi: 10.1136/emj.2009.079475. [DOI] [PubMed] [Google Scholar]
- Levin PJ, Gebbie EN, Qureshi K. Can the Health-Care System Meet the Challenge of Pandemic Flu? Planning, Ethical, and Workforce Considerations. Public Health Reports. 2007;122:573–78. doi: 10.1177/003335490712200503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Huang J, Zhang H. An Analysis of Hospital Preparedness Capacity for Public Health Emergency in Four Regions of China: Beijing, Shandong, Guangxi, and Hainan. BMC Public Health. 2008;8:319. doi: 10.1186/1471-2458-8-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loretti A, Leus X, Van Holsteijn B. Relevant in Times of Turmoil: WHO and Public Health in Unstable Situations. Prehospital and Disaster Medicine. 2001;16:184–91. doi: 10.1017/s1049023x00043296. [DOI] [PubMed] [Google Scholar]
- Lynch AC, Koller T, Cocciardi JA. Creating Isolation Surge Capacity. Journal of Healthcare Protection Management. 2008;24:33–38. [PubMed] [Google Scholar]
- Manley WG, Furbee PM, Coben JH, Smyth SK, Summers DE, Althouse RC, Kimble RL, Kocsis AT, Helmkamp JC. Realities of Disaster Preparedness in Rural Hospitals. Disaster Management & Response. 2006;4:80–87. doi: 10.1016/j.dmr.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Markovitz BP. Pediatric Critical Care Surge Capacity. Journal of Trauma-Injury Infection and Critical Care. 2009;67:S140–S142. doi: 10.1097/TA.0b013e3181ac81b2. [DOI] [PubMed] [Google Scholar]
- Mazowita G. Role for Primary Care in Epidemic Surge Capacity. Canadian Family Physician. 2006;52:951. [PMC free article] [PubMed] [Google Scholar]
- McCarthy ML, Aronsky D, Kelen GD. The Measurement of Daily Surge and Its Relevance to Disaster Preparedness. Academic Emergency Medicine. 2006;13:1138–41. doi: 10.1197/j.aem.2006.06.046. [DOI] [PubMed] [Google Scholar]
- McManus J, Huebner K, Scheulen J. The Science of Surge: Detection and Situational Awareness. Academic Emergency Medicine. 2006;13:1179–82. doi: 10.1197/j.aem.2006.06.038. [DOI] [PubMed] [Google Scholar]
- Mechem CC. Surge Capacity: We All Need It. How Do We Get It? Journal of Emergency Medical Services. 2007;32:48–50. doi: 10.1016/S0197-2510(07)72413-0. [DOI] [PubMed] [Google Scholar]
- Meltzer MI, McNeill KM, Miller JD. Laboratory Surge Capacity and Pandemic Influenza. Emerging Infectious Diseases. 2011;16:147–48. doi: 10.3201/eid1601.091741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon DK, Taylor BL, Ridley SA. Modelling the Impact of an Influenza Pandemic on Critical Care Services in England. Anaesthesia. 2005;60(10):952–54. doi: 10.1111/j.1365-2044.2005.04372.x. [DOI] [PubMed] [Google Scholar]
- Mercer MP, Levis JT, Reyes V. Personal Disaster Preparedness of Emergency Department Staff. Annals of Emergency Medicine. 2011;58:313. [Google Scholar]
- Meredith LS, Eisenman DP, Tanielian T, Taylor SL, Basurto-Davila R, Zazzali J, Diamond D, Cienfuegos B, Shields S. Prioritizing “Psychological” Consequences for Disaster Preparedness and Response: A Framework for Addressing the Emotional, Behavioral, and Cognitive Effects of Patient Surge in Large-Scale Disasters. Disaster Medicine and Public Health Preparedness. 2011;5:73–80. doi: 10.1001/dmp.2010.47. [DOI] [PubMed] [Google Scholar]
- Miller G, Randolph S, Patterson JE. Responding to Simulated Pandemic Influenza in San Antonio, Texas. Infection Control and Hospital Epidemiology. 2008;29:320–26. doi: 10.1086/529212. [DOI] [PubMed] [Google Scholar]
- Monto AS, Comanor L, Shay DK, Thompson WW. Epidemiology of Pandemic Influenza: Use of Surveillance and Modeling for Pandemic Preparedness. Journal of Infectious Diseases. 2006;194:S92–S97. doi: 10.1086/507559. [DOI] [PubMed] [Google Scholar]
- Moser R, Jr, Connelly C, Baker L, Barton R, Buttrey J, Morris S, Saffle J, Whitney JR. Development of a State Medical Surge Plan, Part I: The Procedures, Process, and Lessons Learned or Confirmed. Disaster Management & Response. 2005;3:112–17. doi: 10.1016/j.dmr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Moser R, Jr, Connelly C, Baker L, Barton R, Buttrey J, Morris S, Saffle J, Whitney JR. Development of a State Medical Surge Plan, Part II: Components of a Medical Surge Plan. Disaster Management & Response. 2006;4:19–24. doi: 10.1016/j.dmr.2005.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nager AL, Khanna K. Emergency Department Surge: Models and Practical Implications. Critical Care. 2009;67:96–99. doi: 10.1097/TA.0b013e3181ad2aaa. [DOI] [PubMed] [Google Scholar]
- Nap RE, Andriessen M, Meessen NEL, Albers M, van der Werf TS. Pandemic Influenza and Pediatric Intensive Care. Pediatric Critical Care Medicine. 2010;11:185–98. doi: 10.1097/PCC.0b013e3181cbdd76. [DOI] [PubMed] [Google Scholar]
- Nap RE, Andriessen M, Meessen NEL, Miranda DDR, van der Werf TS. Pandemic Influenza and Excess Intensive-Care Workload. Emerging Infectious Diseases. 2008;14:1518–25. doi: 10.3201/eid1410.080440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nap RE, Andriessen M, Meessen NEL, van der Werf TS. Pandemic Influenza and Hospital Resources. Emerging Infectious Diseases. 2006;13:1714–19. doi: 10.3201/eid1311.070103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCBI (National Center for Biotechnology Information) EDs Credit Drills, Community Engagement with Helping Them Manage Casualties from Tornado Crises. ED Management. 2010a;23:73–76. [PubMed] [Google Scholar]
- NCBI (National Center for Biotechnology Information) Preparations Enable Children's Eds to Effectively Handle H1N1 Surge. ED Management. 2010b;22:25–27. [PubMed] [Google Scholar]
- Noji EK. Disaster Epidemiology: Challenges for Public Health Action. Journal of Public Health Policy. 1992;13:332–40. [PubMed] [Google Scholar]
- Peleg K, Kellermann AL. Enhancing Hospital Surge Capacity for Mass Casualty Events. JAMA. 2009;302:565–67. doi: 10.1001/jama.2009.1119. [DOI] [PubMed] [Google Scholar]
- Phillips S. Current Status of Surge Research. Academic Emergency Medicine. 2006;13:1103–8. doi: 10.1197/j.aem.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Piarroux R, Barrais R, Faucher B, Haus R, Piarroux M, Gaudart J. Understanding the Cholera Epidemic, Haiti. Emerging Infectious Diseases. 2011;17:1161–68. doi: 10.3201/eid1707.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter C, Brough R. Systemic Capacity Building: A Hierarchy of Needs. Health Policy and Planning. 2004;19:336–45. doi: 10.1093/heapol/czh038. [DOI] [PubMed] [Google Scholar]
- Qureshi K, Gershon RR, Sherman MF, Straub T, Gebbie E, McCollum M, Erwin MJ, Morse SS. Health Care Workers’ Ability and Willingness to Report to Duty during Catastrophic Disasters. Journal of Urban Health. 2005;82:378–88. doi: 10.1093/jurban/jti086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson AG, Cooper DM. Disaster Surge Planning in Australia: Measuring the Immeasurable. Medical Journal of Australia. 2007;186:388–89. doi: 10.5694/j.1326-5377.2007.tb00969.x. [DOI] [PubMed] [Google Scholar]
- Rodgers J, Foushee R, Terndrup TE, Gaddis GM. Research Methods of Inquiry. Academic Emergency Medicine. 2006;13:1183–92. doi: 10.1197/j.aem.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Romano M. At Capacity and Beyond. Ideas Such as ‘Surge’ Hospitals Are Getting a More Careful Look as Healthcare Wrestles with Planning for Large-Scale Disasters. Modern Healthcare. 2005;35(39):6–7. [PubMed] [Google Scholar]
- Roszak AR, Jensen FR, Wild RE, Yeskey K, Handrigan MT. Implications of the Emergency Medical Treatment and Labor Act (EMTALA) during Public Health Emergencies and on Alternate Sites of Care. Disaster Medicine and Public Health Preparedness. 2009;3:S172–S175. doi: 10.1097/DMP.0b013e3181c6b664. [DOI] [PubMed] [Google Scholar]
- Rothman RE, Hsu EB, Kahn CA, Kelen GD. Research Priorities for Surge Capacity. Academic Emergency Medicine. 2006;13:1160–68. doi: 10.1197/j.aem.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Rottman SJ, Shoaf KI, Schlesinger J, Klein Selski E, Perman J, Lamb K, Cheng J. Pandemic Influenza Triage in the Clinical Setting. Prehospital and Disaster Medicine. 2010;25:99–104. doi: 10.1017/s1049023x00007792. [DOI] [PubMed] [Google Scholar]
- Rubinson L, Hick JL, Hanfling DG, Devereaux AV, Dichter JR, Christian MD, Talmor D, Medina J, Curtis JR, Geiling JA. Definitive Care for the Critically Ill during a Disaster: A Framework for Optimizing Critical Care Surge Capacity. Chest. 2008;133:18S–31S. doi: 10.1378/chest.07-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudge JW, Hanvoravongchai P, Krumkamp R, Chavez I, Adisasmito W, Ngoc Chau P, Phommasak B, Putthasri W, Shih C-S, Stein M, Timen A, Touch S, Reintjes R, Coker R, Cowling BJ. Health System Resource Gaps and Associated Mortality from Pandemic Influenza across Six Asian Territories. PloS ONE. 2012;7(2):1–10. doi: 10.1371/journal.pone.0031800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rykken D, Heiderscheidt P, Dever G, Kuartei S, Maramoto P. Palau's Current and Future Capacity for Disaster Management. Pacific Health Dialog. 2005;12:99–104. [PubMed] [Google Scholar]
- Sandrock C. Manpower. Intensive Care Medicine. 2010;36:S32–S37. doi: 10.1007/s00134-010-1767-y. [DOI] [PubMed] [Google Scholar]
- Sariego J. A Military Model for Civilian Disaster Management. Disaster Management & Response. 2006;4:114–17. doi: 10.1016/j.dmr.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Satterthwaite PS, Atkinson CJ. Using “Reverse Triage” to Create Hospital Surge Capacity: Royal Darwin Hospital's Response to the Ashmore Reef Disaster. Emergency Medicine Journal. 2010;29(2):160–62. doi: 10.1136/emj.2010.098087. [DOI] [PubMed] [Google Scholar]
- Scarfone RJ, Coffin S, Fieldston ES, Falkowski G, Cooney MG, Grenfell S. Hospital-Based Pandemic Influenza Preparedness and Response Strategies to Increase Surge Capacity. Pediatric Emergency Care. 2010;27:565–72. doi: 10.1097/PEC.0b013e31821dc9d1. [DOI] [PubMed] [Google Scholar]
- Scheulen JJ, Thanner MH, Hsu EB, Latimer CK, Brown J, Kelen GD. Electronic Mass Casualty Assessment and Planning Scenarios (EMCAPS): Development and Application of Computer Modeling to Selected National Planning Scenarios for High-Consequence Events. Annals of Emergency Medicine. 2009;53:226–32. doi: 10.1016/j.annemergmed.2008.09.014. [DOI] [PubMed] [Google Scholar]
- Schull MJ. Hospital Surge Capacity: If You Can't Always Get What You Want, Can You Get What You Need? Annals of Emergency Medicine. 2006;48:389–90. doi: 10.1016/j.annemergmed.2006.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schull MJ, Stukel TA, Verrneulen MJ, Guttmann A, Zwarenstein M. Surge Capacity Associated with Restrictions on Nonurgent Hospital Utilization and Expected Admissions during an Influenza Pandemic: Lessons from the Toronto Severe Acute Respiratory Syndrome Outbreak. Academic Emergency Medicine. 2006;13:1228–31. doi: 10.1197/j.aem.2006.04.011. [DOI] [PubMed] [Google Scholar]
- Schultz C, Koenig K. State of Research in High-Consequence Hospital Surge Capacity. Academic Emergency Medicine. 2006;13:1153–56. doi: 10.1197/j.aem.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Schultz C, Stratton S. Improving Hospital Surge Capacity: A New Concept for Emergency Credentialing of Volunteers. Annals of Emergency Medicine. 2007;49:602–9. doi: 10.1016/j.annemergmed.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Sefrin P, Kuhnigk H. Big Damaging Event—Treatment Capacities and Distribution Strategies. Anasthesiologie Intensivmedizin Notfallmedizin Schmerztherapie. 2008;43:232–35. doi: 10.1055/s-2008-1070975. [DOI] [PubMed] [Google Scholar]
- Severance HW. Mass-Casualty Victim “Surge” Management. Preparing for Bombings and Blast-Related Injuries with Possibility of Hazardous Materials Exposure. North Carolina Medical Journal. 2002;63:242–46. [PubMed] [Google Scholar]
- Shapiro DS. Surge Capacity for Response to Bioterrorism in Hospital Clinical Microbiology Laboratories. Journal of Clinical Microbiology. 2003;41:5372–76. doi: 10.1128/JCM.41.12.5372-5376.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Zeng G, Ma H-L, Shi G-Q, Zhong H-J, Dou F-M, Zhang P, Ruan F, Zhang J, Sun H. Assessment of Current Hospital Capacity in Beijing in Responding to Potential Influenza Pandemic: An Application of Flu Surge Model. Zhonghua Liu Xing Bing Xue Za Zhi. 2008;29:191–94. [PubMed] [Google Scholar]
- Shih FY, Koenig KL. Improving Surge Capacity for Biothreats: Experience from Taiwan. Academic Emergency Medicine. 2006;13:1114–17. doi: 10.1197/j.aem.2006.06.044. [DOI] [PubMed] [Google Scholar]
- Simonds AK, Sokol DK. Lives on the Line? Ethics and Practicalities of Duty of Care in Pandemics and Disasters. European Respiratory Journal. 2009;34:303–9. doi: 10.1183/09031936.00041609. [DOI] [PubMed] [Google Scholar]
- Smith D, Paturas JL, Tomassoni A, Albanese J. Resource Allocation: An Approach for Enhancing Hospital Resiliency. Journal of Business Continuity & Emergency Planning. 2011;5:140–49. [PubMed] [Google Scholar]
- Sobieraj JA, Reyes J, Dunemn KN, Carty IH, Pennathur A, Gutierrez RS, Harris MD. Modeling Hospital Response to Mild and Severe Influenza Pandemic Scenarios under Normal and Expanded Capacities. Military Medicine. 2007;172:486–90. doi: 10.7205/milmed.172.5.486. [DOI] [PubMed] [Google Scholar]
- Sprung CL, Zimmerman JL, Christian MD, Joynt GM, Hick JL, Taylor B, Richards GA, Sandrock C, Cohen R, Adini B. Recommendations for Intensive Care Unit and Hospital Preparations for an Influenza Epidemic or Mass Disaster: Summary Report of the European Society of Intensive Care Medicine's Task Force for Intensive Care Unit Triage during an Influenza Epidemic or Mass Disaster. Intensive Care Medicine. 2010;36:428–43. doi: 10.1007/s00134-010-1759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standards and Guidelines for Healthcare Surge during Emergencies: Roles to Be Played by Hospital Security. Journal of Healthcare Protection Management. 2009;25:72–80. [PubMed] [Google Scholar]
- Steffen C, Masterson L, Christos S. Willingness to Respond: A Survey of Emergency Department Personnel and Their Predicted Participation in Mass Casualty Terrorist Events. Annals of Emergency Medicine. 2004;44:S34. doi: 10.1016/j.jemermed.2007.10.074. [DOI] [PubMed] [Google Scholar]
- Stratton SJ, Tyler RD. Characteristics of Medical Surge Capacity Demand for Sudden-Impact Disasters. Academic Emergency Medicine. 2006;13:1193–97. doi: 10.1197/j.aem.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Swanson RC, Bongiovanni A, Bradley E, Murugan V, Sundewall J, Betigeri A, Nyonator F, Cattaneo A, Harless B, Ostrovsky A, Labonte R. Toward a Consensus on Guiding Principles for Health Systems Strengthening. PLoS Med. 2010;7:e1000385. doi: 10.1371/journal.pmed.1000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tadmor B, McManus J, Koenig KL. The Art and Science of Surge: Experience from Israel and the US Military. Academic Emergency Medicine. 2006;13:1130–34. doi: 10.1197/j.aem.2006.06.043. [DOI] [PubMed] [Google Scholar]
- Tandberg D, Qualls C. Time Series Forecasts of Emergency Department Patient Volume, Length of Stay, and Acuity. Annals of Emergency Medicine. 1994;23:299–306. doi: 10.1016/s0196-0644(94)70044-3. [DOI] [PubMed] [Google Scholar]
- Taylor CW. Surge Capacity: Preparing Your Healthcare System. Emergency Medical Services. 2003;32:91–92. [PubMed] [Google Scholar]
- Ten Eyck RP. Ability of Regional Hospitals to Meet Projected Avian Flu Pandemic Surge Capacity Requirements. Prehospital and Disaster Medicine. 2008;23:103–12. doi: 10.1017/s1049023x00005707. [DOI] [PubMed] [Google Scholar]
- Tran P, Weireter L, Sokolowski W, Lawsure K, Sokolowski J. HAZUS Modeling for Hurricane Effect on a Healthcare Campus: Implications for Health Care Planning. American Surgeon. 2009;75:1059–64. [PubMed] [Google Scholar]
- Traub M, Bradt DA, Joseph AP. The Surge Capacity for People in Emergencies Study in Australasian Hospitals. Medical Journal of Australia. 2007;186:394–98. doi: 10.5694/j.1326-5377.2007.tb00971.x. [DOI] [PubMed] [Google Scholar]
- UN (United Nations) Report on the World Conference on Disaster Reduction. International Strategy for Disaster Reduction. Geneva: 2005. [Google Scholar]
- UNISDR (United Nations International Strategy for Disaster Reduction) Vulnerability to Natural Hazards Rising Rapidly in Europe. Geneva: 2011. [Google Scholar]
- Van Cleve WC, Hagan P, Lozano P, Mangione-Smith R. Investigating a Pediatric Hospital's Response to an Inpatient Census Surge during the 2009 H1N1 Influenza Pandemic. Joint Commission Journal on Quality and Patient Safety / Joint Commission Resources. 2011;37:376–82. doi: 10.1016/s1553-7250(11)37048-1. [DOI] [PubMed] [Google Scholar]
- Voelker R. Mobile Hospital Raises Questions about Hospital Surge Capacity. JAMA. 2006;295:1499–1503. doi: 10.1001/jama.295.13.1499. [DOI] [PubMed] [Google Scholar]
- Watkins SM, Perrotta DM, Stanbury M, Heumann M, Anderson H, Simms E, Huang M. State-Level Emergency Preparedness and Response Capabilities. Disaster Medicine & Public Health Preparedness. 2011;5:134–42. doi: 10.1001/dmp.2011.26. [DOI] [PubMed] [Google Scholar]
- Welzel TB, Koenig KL, Bey T, Visser E. Effect of Hospital Staff Surge Capacity on Preparedness for a Conventional Mass Casualty Event. Western Journal of Emergency Medicine. 2010;11:189–96. [PMC free article] [PubMed] [Google Scholar]
- WHA (World Health Assembly) 64th World Health Assembly Agenda Item 13.4: Strengthening National Health Emergency and Disaster Management Capacities and Resilience of Health Systems. Geneva: 2011. [Google Scholar]
- WHO (World Health Organization) Health Aspects of Disaster Preparedness and Response. Report from a Regional Meeting of Countries of South East Asia. Bangkok, Thailand, November 21–23, 2005. Prehospital & Disaster Medicine. 2006;21:S62–78. [PubMed] [Google Scholar]
- WHO (World Health Organization) Comparative Analysis of National Pandemic Influenza Preparedness Plans. Geneva: 2011a. Available at http://www.who.int/influenza/resources/documents/comparative_analysis_php_2011_en/en/index.html (accessed September 26, 2012) [Google Scholar]
- WHO (World Health Organization) Hospital Emergency Response Checklist: An All-Hazards Tool for Hospital Administrators and Emergency Managers. Copenhagen; 2011b. Available at http://www.euro.who.int/en/what-we-do/health-topics/emergencies/disaster-preparedness-and-response/publications/2011/hospital-emergency-response-checklist (accessed September 26, 2012) [Google Scholar]
- Yi P, George SK, Paul JA, Lin L. Hospital Capacity Planning for Disaster Emergency Management. Socio-Economic Planning Sciences. 2010;44:151–60. [Google Scholar]
- Zhang X, Meltzer MI, Wortley PM. FluSurge—A Tool to Estimate Demand for Hospital Services during the Next Pandemic Influenza. Medical Decision Making. 2006;26:617–23. doi: 10.1177/0272989X06295359. [DOI] [PubMed] [Google Scholar]
- Zilm F, Berry R, Pietrzak MP, Paratore A. Integrating Disaster Preparedness and Surge Capacity in Emergency Facility Planning. Journal of Ambulatory Care Management. 2008;31:377–85. doi: 10.1097/01.JAC.0000336556.54460.25. [DOI] [PubMed] [Google Scholar]


