Abstract
Objectives:
This prospective, randomized, medium-term trial aimed to assess the efficiency, safety and postoperative results of bipolar plasma vaporization (BPV) in comparison with monopolar transurethral resection (TUR) in cases of secondary bladder neck sclerosis (BNS).
Methods:
A total of 70 patients with BNS secondary to transurethral resection of the prostate (TURP; 46 cases), open prostatectomy for benign prostatic hypertrophy (BPH; 18 cases) and radical prostatectomy for prostate cancer (6 cases) were enrolled in the trial. The inclusion criteria consisted of maximum flow rate (Q max) <10 ml/s and International Prostate Symptom Score (IPSS) >19. All patients were evaluated preoperatively and at 1, 3, 6, 12 and 18 months after surgery by IPSS, quality of life score (QoL), Q max and postvoiding residual urinary volume (PVR).
Results:
The mean operation time (10.3 versus 14.9 minutes), catheterization period (0.75 versus 2.1 days) and hospital stay (1.1 versus 3.2 days) were significantly reduced in the BPV series. During the immediate postoperative follow up, recatheterization for acute urinary retention only occurred in the TUR series (5.7%). The medium-term retreatment requirements due to BNS recurrence were lower in the BPV study arm (2.8% versus 8.5%). At the 1, 3, 6, 12 and 18 months assessments, statistically similar parameters were found concerning the IPSS and QoL symptom scores, Q max and PVR values specific for the two therapeutic alternatives.
Conclusions:
BPV constitutes a valuable endoscopic treatment approach for secondary BNS. The method emphasized superior efficacy, a satisfactory safety profile and similar medium-term follow-up features when compared with standard TUR.
Keywords: bipolar plasma vaporization, monopolar transurethral resection, secondary bladder neck sclerosis.
Introduction
Secondary bladder neck sclerosis (BNS) represents a significant late complication secondary to prostate surgery. Obstruction caused by this pathology has been found to determine an increased intravesical voiding pressure while aiming to counteract the elevated outlet resistance [Tanagho and McAninch, 2007]. When we considered the available literature, the reported incidence of this condition varied between 0.14% and 20% [Robinson and Greene, 1962; Chiu et al. 1990; Bruskewitz et al. 1986; Edwards et al. 1985]. According to the EAU Guidelines, the risk of developing this complication subsequent to transurethral resection of the prostate (TURP) is about 4.7% [Oelke et al. 2012], while after open surgery, the respective rate is described as around 6% [Naspro et al. 2006; Skolarikos et al. 2008; Kuntz et al. 2008]. Moreover, radical prostatectomy for prostate cancer emphasizes a BNS incidence ranging between 0.5% and 14.6% [Heidenreich et al. 2012].
As far as the BNS endoscopic approach is concerned, monopolar transurethral incision (TUI) [Jocius and Sukys, 2002] and transurethral resection (TUR) [Sataa et al. 2009] have been described as the most reliable endoscopic approaches. In recent years, the holmium:yttrium–aluminum–garnet (Ho:YAG) and the thulium:yttrium–aluminum–garnet (Th:YAG) lasers have emphasized satisfactory postoperative outcomes in BNS treatment [Lagerveld et al. 2005; Bader et al. 2010; Bach et al. 2007].
Bipolar electrosurgical technology using the PlasmaKinetic [Basok et al. 2008] and transurethral resection in saline (TURis) [Sevriukov et al. 2007] systems have been described as viable techniques in minimally invasive bladder neck contracture therapy. On the other hand, bipolar plasma vaporization (BPV) constitutes a new development of this procedure, recently introduced in clinical practice with satisfactory clinical outcomes concerning relief of lower urinary tract symptoms (LUTS) [Geavlete et al. 2010]. After initially performing this approach in average size BPH cases [Geavlete et al. 2009], the technique started to be applied in secondary BNS patients as well [Geavlete et al. 2012].
This trial aimed to assess the therapeutic efficiency, overall safety and postoperative results of the plasma-button vaporization procedure in cases of bladder neck contracture while considering a parallel with the standard resection in a randomized setting. Monopolar TUR was considered most suitable for an initial comparative study intended to determine the viability of the newly introduced BPV technique, although bipolar resection could also constitute an interesting perspective for future trials.
Methods
A single-centre, prospective, medium-term, randomized trial was performed, aiming to compare plasma vaporization and standard monopolar TUR in secondary BNS patients. The primary endpoint of the study was to evaluate the efficiency of the two types of approach with regards to perioperative features and follow-up parameters.
The study was approved by the local ethics and research committee. A total of 70 cases with a mean age of 71.4 (range 61–88), BNS and severe LUTS were enrolled in the trial. All patients were included under approved written informed consent, randomized by means of sealed envelopes and blinded to treatment. The BNS process was secondary to TURP in 46 cases, to open surgery for BPH in 18 patients and to radical prostatectomy for prostate cancer in six cases (with no clinical, biochemical or imagistic signs of recurrence).
The standard investigation protocol performed in all patients consisted of general clinical evaluation with digital rectal examination (DRE), blood tests, prostate specific antigen (PSA), urinalysis, urine culture, International Prostate Symptom Score (IPSS), quality of life score (QoL), uroflowmetry (evaluating the maximum flow rate Q max), abdominal and transrectal ultrasound (measuring the prostate volume and the postvoiding residual urinary volume [PVR]) and flexible urethrocystoscopy. The latter investigation method provided a more accurate diagnostic based on the direct visualization of the fibrous scar formation obstructing the bladder neck area and cancelled the need for retrograde cystography.
The inclusion criteria were represented by Q max <10 ml/s and IPSS >19. Standard TUR was performed with a 26F Storz continuous flow monopolar resectoscope and single-wire resection loops. For the bipolar vaporization technique, the endoscopic equipment consisted of the Olympus SurgMaster UES-40 bipolar generator, the OES-Pro bipolar resectoscope and ‘button’-type vaporesection electrodes (Olympus Europe, Hamburg, Germany). In all prostate cancer patients, bipolar loop resection from the bladder neck area was used in order to obtain specimens for the pathological analysis.
From the perspective of the surgical technique, after an initial urethrocystoscopic assessment, the plasma-button vaporization was used for opening up the obstructed bladder neck (Figure 1). Basically, the fibrous tissue was gradually vaporized, layer by layer, until reaching the prostatic capsule (the so-called ‘hovering’ technique), while the coagulation with the same ‘button’ was rarely necessary (Figure 2). At all times, a close contact between the hemispheric electrode and the sclerotic surface was maintained in order to produce a constant vaporization effect. The complete ablation of the sclerotic tissue was confirmed by the clear visualization of the capsular muscular fibres, as a wide prostatic fossa with a neat surface and no irregularities, debris or obstruction was obtained (Figure 3).
Figure 1.
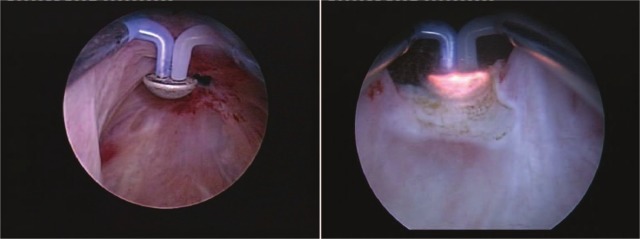
Initial urethrocystoscopic assessment and plasma-button vaporization.
Figure 2.
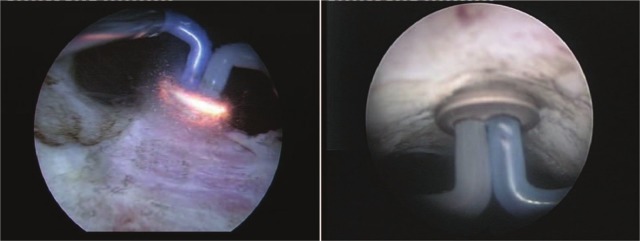
Fibrous tissue gradual plasma removal and eventual bipolar coagulation.
Figure 3.
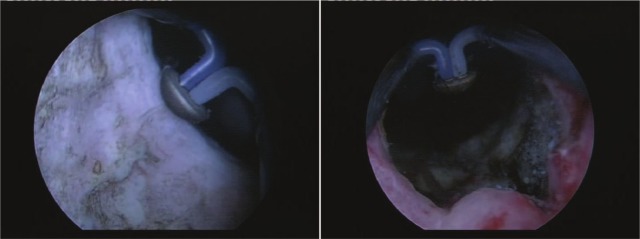
Clear capsular fibres and wide bladder neck and prostatic fossa.
As part of the follow-up protocol, all cases were assessed at 1, 3, 6, 12 and 18 months after the initial procedure by IPSS, QoL, Q max and PVR.
Using the SPSS 15.0 software (SPSS Inc., Chicago, IL, USA), the binomial test, the Mann–Whitney U-test and the independent samples t-test were applied in order to determine the statistical significance of differences between various parameters of the two series. The primary endpoint was to test the null hypothesis that the perioperative and follow-up features were similar in the BPV and TUR groups. With a sample size of 35 patients in each treatment arm and a confidence level of at least 95%, the trial was determined to have an 82% power to reject the null hypothesis.
Results
Similar preoperative values were determined in terms of mean IPSS, QoL, Q max and PVR for the two series, with no statistically significant differences between them (Table 1).
Table 1.
Preoperative parameters.
| Preoperative parameters | BPV (n = 35) | TUR (n = 35) | p-value* |
|---|---|---|---|
| IPSS | 23.2 | 22.9 | 0.404 |
| QoL | 4.0 | 4.1 | 0.587 |
| Q max (ml/s) | 7.8 | 7.5 | 0.965 |
| PVR (ml) | 107.5 | 112.8 | 0.991 |
Mann–Whitney U-test.
BPV, bipolar plasma vaporization; TUR, monopolar transurethral resection; IPSS, International Prostate Symptom Score; QoL, quality of life score; Q max, maximum flow rate; PVR, postvoiding residual urinary volume.
Both types of procedures were successfully performed in all cases. As far as the intraoperative complications were concerned, the prostatic capsule perforation (8.5%) and intraoperative bleeding (5.7%) were only present in the TUR study arm. With regards to the perioperative features, the mean operation time, catheterization period and hospital stay were significantly shorter for BPV by comparison to standard resection (10.3 versus 14.9 minutes, 0.75 versus 2.1 days and 1.1 versus 3.2 days) (Table 2).
Table 2.
Perioperative features.
| Perioperative features | BPV (n = 35) | TUR (n = 35) | p-value* |
|---|---|---|---|
| Operation time (minutes) | 10.3 | 14.9 | 0.005 |
| Catheterization period (days) | 0.75 | 2.1 | < 0.0001 |
| Hospital stay (days) | 1.1 days | 3.2 days | < 0.0001 |
Binomial test.
BPV, bipolar plasma vaporization; TUR, monopolar transurethral resection.
During the immediate postoperative follow up, hematuria (2.8%) and recatheterization for acute urinary retention (5.7%) only occurred in the TUR group. From the perspective of the short-term adverse events, similar rates of early irritative symptoms (still more frequent secondary to BPV, 14.2% versus 11.4%) and urinary tract infection (2.8% versus 2.8%) were described. Moreover, the medium-term retreatment requirements due to BNS recurrence were substantially reduced when the plasma vaporization technique was initially applied (2.8% versus 8.5%), despite the lack of statistical significance caused by the insufficient number of cases (Table 3).
Table 3.
Complication rates.
| Complications | BPV (n = 35) | TUR (n = 35) | p-value* |
|---|---|---|---|
| Early irritative symptoms | 5 (14.2%) | 4 (11.4%) | 0.369 |
| Urinary tract infections | 1 (2.8%) | 1 (2.8%) | 0.637 |
| BNS re-treatment rate | 1 (2.8%) | 3 (8.5%) | 0.317 |
Binomial test.
BPV, bipolar plasma vaporization; TUR, monopolar transurethral resection; BNS, secondary bladder neck sclerosis.
Along the course of the trial, four patients failed to complete the evaluation protocol and three were disregarded from the rest of the study. At the 1, 3, 6, 12 and 18 months follow up, statistically similar parameters were found concerning the IPSS and QoL symptom scores specific for the two therapeutic alternatives. Also, no significant difference was outlined with regard to the urodynamic features provided by BPV and TUR in terms of maximum flow rate. In addition, similar PVR values were established at the respective ultrasound evaluations (Table 4).
Table 4.
Medium-term follow-up parameters.
| Results | BPV (n = 31) | TUR (n = 32) | p-value |
|---|---|---|---|
| IPSS | |||
| 1 month | 3.8 | 4.0 | 0.766** |
| 3 months | 3.6 | 3.9 | 0.629** |
| 6 months | 3.5 | 3.6 | 0.892** |
| 12 months | 3.3 | 3.5 | 0.714** |
| 18 months | 3.4 | 3.3 | 0.881** |
| QoL | |||
| 1 month | 1.4 | 1.5 | 0.939* |
| 3 months | 1.2 | 1.4 | 0.525* |
| 6 months | 1.1 | 1.2 | 0.962* |
| 12 months | 1.1 | 1.1 | 0.696* |
| 18 months | 1.2 | 1.1 | 0.179* |
| Qmax (ml/s) | |||
| 1 month | 23.0 | 23.3 | 0.880** |
| 3 months | 23.2 | 23.6 | 0.817** |
| 6 months | 23.5 | 23.8 | 0.868** |
| 12 months | 23.9 | 24.2 | 0.852** |
| 18 months | 23.8 | 24.0 | 0.922** |
| PVR (ml) | |||
| 1 month | 31 | 28 | 0.460** |
| 3 months | 24 | 23 | 0.733** |
| 6 months | 22 | 21 | 0.694** |
| 12 months | 19 | 18 | 0.699** |
| 18 months | 21 | 17 | 0.133** |
Mann–Whitney U-test.
Independent samples t-test.
BPV, bipolar plasma vaporization; TUR, monopolar transurethral resection; IPSS, International Prostate Symptom Score; QoL, quality of life score; Q max, maximum flow rate; PVR, postvoiding residual urinary volume.
Discussion
First described by Danslow in 1918 [Coulange et al. 1987], BNS was defined as a block of fibrous scar located at the bladder neck area [Sataa et al. 2009]. Secondary BNS still remains an important problem of modern urology, in most situations being related to the endoscopic resection of small prostates [Al-Singary et al. 2004]. Moreover, BNS practically constitutes a complication frequently caused by the excessive resection or prolonged coagulation of the bladder neck area. Subsequently, an obstructive diaphragm of sclerotic tissue is formed resulting in the narrowing of the bladder neck circumference, thus impeding on the voiding process [Sinescu et al. 2008].
According to the literature, the BNS frequency among large series of patients described a 3.4–9.7% rate during a mean follow-up period of 3–4 years [Lee et al. 2005; Al-Singary et al. 2004]. On a related subject, patients undergoing early surgery and those with inflammatory lesions such as chronic prostatitis appear to be predisposed to developing the postoperative sclerosis of the bladder neck [Pérez Aebej et al. 1991a]. On the other hand, transurethral incision performed as an adjunct procedure to standard TURP was associated with a significant frequency reduction of secondary bladder neck contracture [Lee et al. 2005].
Moreover, transvesical adenomectomy was not spared of this kind of late complication, registered in 1.64–3.3% of cases [Sataa et al. 2009; Varkarakis et al. 2004]. Also, the stenosis of the vesico-urethral anastomosis subsequent to radical prostatectomy was proved as a rather frequent event, encountered in 9.4% of the cases [Besarani et al. 2004].
Nowadays, the endoscopic approach represents the main treatment alternative for this type of pathology [Sataa et al. 2009], mostly related to the transurethral bladder neck incision and/or resection [Jocius and Sukys, 2002]. From this perspective, the excision of sclerotic tissue by transurethral encircling resection was emphasized as the most widely used procedure, enjoying the highest success rate, clearly superior to that of cold-knife incision of the obstructive diaphragm [Pérez Aebej et al. 1991b]. In contrast, other authors sustained the superiority of the two-incision endoscopic cervicotomy over the perimetric resection of the sclerotic ring due to the lower recurrence rate [Martín-Laborda y Bergasa et al. 1995].
In any case, BNI and TUR of the contracture area were underlined as definitely better in preventing recurrence when compared with simple dilation. Further on, the 5 and 7 o’clock incision with the 70 W 2-µm continuous wave laser (Th:YAG) was described as a fast and safe technique in recurrent BNS [Bach et al. 2007]. In cases of bladder neck contracture subsequent to radical prostatectomy, graduated dilation under light sedation [Besarani et al. 2004], neodymium:yttrium–aluminum– garnet (Nd:YAG) [Silber and Servadio, 1992] and Ho:YAG [Bader et al. 2010] laser incision of the anastomotic stricture seemed to constitute viable treatment alternatives. As far as bipolar electrosurgery was concerned, both the transurethral resection in saline [Sevriukov et al. 2007] and PlasmaKinetic bipolar vaporization [Basok et al. 2008] were taken into consideration as possibly successful BNS therapeutic approaches.
The bipolar plasma vaporization using the ‘button’ electrode was introduced as a remarkably promising BPH treatment alternative, providing improved short-term [Geavlete et al. 2010] as well as medium-term [Geavlete et al. 2011] results when compared with either monopolar [Geavlete et al. 2010, 2011] or bipolar [Geavlete et al. 2011] TURP. The remarkable efficacy of this type of endoscopic technique in safely and rapidly ablating medium size prostates soon translated into a further application in secondary BNS cases due to the rather similar type of approach.
Practically, the plasma corona produced on the surface of the hemispherical shape electrode was shown as effective in removing the specific bladder neck fibrous tissue as during the average BPH tissue vaporization. Still, due to the increased consistency of the scar formation, a power increase from 260–280 W to 300–320 W became necessary. Otherwise, the same as during the prostate plasma vaporization, a clear endoscopic vision was maintained at all times, thus creating the premise for an accurate delineation between the pathologic sclerotic tissue and the normal fibres of the prostatic capsule. Consequently, the complete bladder neck scar ablation was achieved, providing the conditions for an effective prevention of BNS recurrence. Therefore, plasma vaporization seemed promising enough in matching the literature-stated ability of laser energy in enabling the immediate vaporization and disintegration of the fibrous area, followed by secondary bladder neck re-epithelization, unimpaired by scar tissue recurrence [Silber and Servadio, 1992].
When referring to the surgical safety of the two techniques assessed in the present trial, BPV appeared to emphasize an optimistic perspective, based on the absence of capsular perforation and intraoperative bleeding, intraoperative adverse events that were only present in the TUR series (8.5% and 5.7%, respectively). More so, together with an increased efficacy suggested by the significantly shorter operation time (10.3 versus 14.9 minutes), the plasma vaporization patients also benefited from a reduced convalescence period when compared with TUR (0.75 versus 2.1 days of catheterization and 1.1 versus 3.2 days of hospital stay). As far as the cost-effectiveness of the BPV procedure was concerned, it was observed that, while the price of the plasma-button electrodes naturally remained higher when compared with the standard monopolar resection loops, the overall cost per procedure was relatively lower for the plasma vaporization technique when drawing a parallel with conventional TUR due to the significantly shorter hospital stay. Of course, the initial equipment investment related to the plasma vaporization technical setup was, as expected, higher than that implied by an average standard monopolar TUR endoscopic line.
Also, the permeability of the lower urinary tract seemed to be better preserved following BPV, which was not marked by any case of postoperative recatheterization for acute urinary retention (unlike monopolar TUR in 5.7% of the cases). Last but not least, the BPV-specific learning curve emphasized by our experience previous to the present trial was rather short and was generally based on an average number of 10 bipolar vaporization procedures.
One of the most challenging issues when discussing BNS pathology is related to the substantial percentage of recurrence secondary to transurethral surgery. For example, the standard monopolar circular resection of the bladder neck sclerotic area resulted in an elevated restenosis rate (27.5–36%) [Martín-Laborda y Bergasa et al. 1995; Sataa et al. 2009]. Results on this subject are quite variable in the available literature, as for example bilateral longitudinal bladder neck incision and local anti-inflammatory therapy induced a 5% recurrence [Gómez Veiga et al. 1991]. In addition, Th:YAG laser incision was characterized by a 14.3% recurrence rate at 12 months [Bach et al. 2007].
Based on these premises, the substantially lower BNS retreatment rate in the plasma vaporization study arm (2.8% versus 8.5%) of the present trial could be considered as a solid argument supporting the durability of the therapeutic outcome. Unfortunately, the respective difference did not present statistical significance, most likely as a result of the limited number of patients included. On the other hand, gathering 70 BNS cases in a clinical analysis could be considered as a step forward, since the series mentioned in previous studies generally varied between 25 and 40 [Martín-Laborda y Bergasa et al. 1995; Sataa et al. 2009].
Unfortunately, while considering the rather remote number of trials published so far on the subject of secondary BNS, the clinical data evaluating the results of various endoscopic approaches remained limited. For example, the bipolar PlasmaKinetic vaporization (a precursor of the more recent plasma-button procedure) produced a Q max increase at 12.2 months after surgery from the preoperative value of 3.4 to 16.2 ml/s [Basok et al. 2007]. The urodynamic features characterizing BPV and monopolar TUR were statistically similar and revealed a 1-year maximum flow rate improvement from 7.8 to 23.9 ml/s and from 7.5 to 24.2 ml/s, respectively. So, the voiding capabilities of the plasma-button vaporization patients appear satisfactory, at least in the medium term.
Naturally, laser treatment should be part of the comparative analysis when aiming to introduce a new method in the treatment armamentarium for bladder neck contracture. In this regard, when drawing a parallel with the baseline features, Th:YAG laser incision and vaporization determined a 1-year significant amelioration of Q max (from 9 to 23 ml/s), symptom score (from 22 to 8 points) and QoL index (from 4 to 1) [Bach et al. 2007]. At the same time intervals, BPV emphasized substantial progresses concerning these parameters (from 7.8 to 23.9 ml/s, from 23.2 to 3.8 points and from 4.0 to 1.1, respectively).
Overall, the medium-term data gathered at 1, 3, 6, 12 and 18 months after the initial intervention displayed similar figures for the mean IPSS, QoL, Q max and PVR values in the BPV and standard TUR groups, thus underlining the reliable positive effect of the plasma-button technique in secondary BNS cases. When considering the advantage of bipolar technology in terms of costs by comparison to laser treatment [Basok et al. 2007], a promising perspective seems to define the developing ‘button’ vaporization procedure.
Conclusions
BPV was found to constitute a valuable endoscopic treatment alternative for secondary BNS patients. In a randomized analysis, the method emphasized superior efficacy, satisfactory surgical safety as well as a similar medium-term improvement in follow-up parameters by comparison with the standard TUR.
The significantly decreased operation length, catheterization period and hospital stay represent favourable arguments for this new procedure. Moreover, the absence of prostatic capsule perforation, intraoperative bleeding, postoperative hematuria and recatheterization for acute urinary retention, otherwise present in the TUR group, substantially contributed to the superior safety profile specific for the plasma-button vaporization technique.
Regarding the medium-term restenosis rate requiring a repeated treatment, BPV also seemed quite promising, although additional extensive studies will be necessary in order to confirm this aspect. The results obtained after an 18 months assessment period emphasized a significant and stable amelioration of the mean IPSS and QoL scores, Q max and PVR. The statistical similarity of BPV and standard resection results with regard to symptom scores and voiding parameters supported the viability of this new type of approach.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: Bogdan Geavlete presented lectures and received honorariums during Olympus sponsored symposiums.
Contributor Information
Bogdan Geavlete, ‘Saint John’ Emergency Clinical Hospital, Department of Urology, Bucharest, Romania.
Cristian Moldoveanu, ‘Saint John’ Emergency Clinical Hospital, Department of Urology, Bucharest, Romania.
Catalin Iacoboaie, ‘Saint John’ Emergency Clinical Hospital, Department of Urology, Bucharest, Romania.
Petrisor Geavlete, ‘Saint John’ Emergency Clinical Hospital, Department of Urology, Vitan Barzesti Street No. 13, Sector 4, Code: 042122, Bucharest, Romania.
References
- Al-Singary W., Arya M., Patel H. (2004) Bladder neck stenosis after transurethral resection of prostate: does size matter? Urol Int 73: 262-265 [DOI] [PubMed] [Google Scholar]
- Bach T., Herrmann T., Cellarius C., Gross A. (2007) Bladder neck incision using a 70 W 2 micron continuous wave laser (RevoLix). World J Urol 25: 263-267 [DOI] [PubMed] [Google Scholar]
- Bader M., Tilki D., Gratzke C., Sroka R., Stief C., Reich O. (2010) Ho:YAG-laser: treatment of vesicourethral strictures after radical prostatectomy. World J Urol 28: 169-172 [DOI] [PubMed] [Google Scholar]
- Basok E., Basaran A., Gurbuz C., Yildirim A., Tokuc R. (2008) Can bipolar vaporization be considered an alternative energy source in the endoscopic treatment of urethral strictures and bladder neck contracture? Int Braz J Urol 34: 577-584 [DOI] [PubMed] [Google Scholar]
- Besarani D., Amoroso P., Kirby R. (2004) Bladder neck contracture after radical retropubic prostatectomy. BJU Int 94: 1245-1247 [DOI] [PubMed] [Google Scholar]
- Bruskewitz R., Larsen E., Madsen P., Dørflinger T. (1986) Three year follow-up of urinary symptoms after transurethral resection of the prostate. J Urol 136: 613–615 [DOI] [PubMed] [Google Scholar]
- Chiu A., Chen M., Chang L., Huang J., Chen K., Lin A., et al. (1990) Prophylactic bladder neck incision in the treatment of small benign prostatic hyperplasia. Zhonghua Yi Xue Za Zhi 45: 22-25 [PubMed] [Google Scholar]
- Coulange C., Albert P., Leremboure H., Vaillant J., Hernandez F., Rampal M. (1987) Sclérose récidivante de la loge prostatique après résection transurethrale. J Urol 94: 372-373 [Google Scholar]
- Edwards L., Bucknall T., Pittam M., Richardson D., Stanek J. (1985) Transurethral resection of the prostate and bladder neck incision: a review of 700 cases. Br J Urol 57: 168–171 [DOI] [PubMed] [Google Scholar]
- Geavlete B., Drăguţescu M., Mulţescu R., Georgescu D., Jecu M., Geavlete P. (2009) TURIS plasma vaporization–initial Romanian experience with a new technology. J Med Life 2: 325-332 [PMC free article] [PubMed] [Google Scholar]
- Geavlete B., Georgescu D., Multescu R., Stanescu F., Jecu M., Geavlete P. (2011) Bipolar plasma vaporization vs monopolar and bipolar TURP-A prospective, randomized, long-term comparison. Urology 78: 930-935 [DOI] [PubMed] [Google Scholar]
- Geavlete B., Multescu R., Dragutescu M., Jecu M., Georgescu D., Geavlete P. (2010) Transurethral resection (TUR) in saline plasma vaporization of the prostate vs standard TUR of the prostate: ‘the better choice’ in benign prostatic hyperplasia? Br J Urol Int 106: 1695-1699 [DOI] [PubMed] [Google Scholar]
- Geavlete B., Stanescu F., Nita Gh., Jecu M., Moldoveanu C., Geavlete P. (2012) Bipolar plasma vaporization in secondary bladder neck sclerosis – initial experience with a new technique. J Med Life 5: 120-125 [PMC free article] [PubMed] [Google Scholar]
- Gómez Veiga F., González Martín M., Sánchez Rodríguez J., Chantada Abal V., Busto Castañón L., Sousa Escandón A. (1991) Endoscopic cervicotomy in post-prostatectomy sclerosis of the bladder neck. Arch Esp Urol 44: 727-732 [PubMed] [Google Scholar]
- Heidenreich A., Bastian P., Bellmunt J., Bolla M., Joniau S., Mason M., et al. (2012) Guidelines on prostate cancer. European Association of Urology Guideline 50, available at: http://www.uroweb.org/gls/pdf/08%20Prostate%20Cancer_LR%20March%2013th%202012.pdf
- Jocius K., Sukys D. (2002) Treatment of bladder neck obstruction (sclerosis): personal experience and literature review. Medicina (Kaunas) (Suppl. 1) 38: 48-55 [PubMed] [Google Scholar]
- Kuntz R., Lehrich K., Ahyai S. (2008) Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol 53: 160-166 [DOI] [PubMed] [Google Scholar]
- Lagerveld B., Laguna M., Debruyne F., De La Rosette J. (2005) Holmium:YAG laser for treatment of strictures of vesicourethral anastomosis after radical prostatectomy. J Endourol 19: 497-501 [DOI] [PubMed] [Google Scholar]
- Lee Y., Chiu A., Huang J. (2005) Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology 65: 498-503 [DOI] [PubMed] [Google Scholar]
- Martín-Laborda y Bergasa F., Vallejo Herrador J., Sánchez de la Muela Naverac P.L. (1995) Endoscopic cervicotomy: elective treatment in bladder neck sclerosis. Arch Esp Urol 48: 36-41 [PubMed] [Google Scholar]
- Naspro R., Suardi N., Salonia A., Scattoni V., Guazzoni G., Colombo R., et al. (2006) Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur Urol 50: 563-568 [DOI] [PubMed] [Google Scholar]
- Oelke M., Bachmann A., Descazeaud A., Emberton M., Gravas S., Michel M.C., et al. et al (2012) Guidelines on the treatment of non-neurogenic male LUTS. European Association of Urology Guideline 41, available at: http://www.uroweb.org/gls/pdf/12_Male_LUTS.pdf
- Pérez Aebej J., Cameo Rico M., Valdivia Uría J., Espuela Orgaz R. (1991a) Postoperative sclerosis of the bladder neck: pathogenic mechanisms. Arch Esp Urol 44: 1167-1176 [PubMed] [Google Scholar]
- Pérez Arbej J., Cameo Rico M., Valdivia Uría J., Espuela Orgaz R. (1991b) Postoperative sclerosis of the bladder neck: surgical treatment. Arch Esp Urol 44: 1177-1184 [PubMed] [Google Scholar]
- Robinson H., Greene L. (1962) Postoperative contracture of the vesical neck. I. Review of cases and proposed theory of etiology. J Urol 87: 601-609 [DOI] [PubMed] [Google Scholar]
- Sataa S., Yassine N., Horchani A. (2009) Bladder neck sclerosis after surgical or transurethral resection of the prostate: a report of 40 cases. Tunis Med 87: 810-813 [PubMed] [Google Scholar]
- Sevriukov F., Puchkin A., Krupin V., Chebykin A., Sorokin D., Karpukhin I., et al. (2007) Transurethral electrosurgery of a new generation (TURis) in the treatment of the lower urinary tract and prostate diseases. Urologiia 35: 28-32 [PubMed] [Google Scholar]
- Silber N., Servadio C. (1992) Neodymium:YAG laser treatment of bladder neck contracture following prostatectomy. Laser Surg Med 12: 370-374 [DOI] [PubMed] [Google Scholar]
- Sinescu I., Gluck G., Miclea F., Boiborean P., Botoca M., Cumpanas A. (2008) Treaty of urology. Benign Prostatic Hyperplasia 28: 2338 [Google Scholar]
- Skolarikos A., Papachristou C., Athanasiadis G., Chalikopoulos D., Deliveliotis C., Alivizatos G. (2008) Eighteen-month results of a randomised prospective study comparing transurethral photoselective vaporisation with transvesical open enucleation for prostatic adenomas greater than 80 cc. J Endourol 22: 2333-2340 [DOI] [PubMed] [Google Scholar]
- Tanagho E., McAninch J. (2007) Smith’s General Urology, 17th Edition New York: McGraw-Hill Professional, p. 173 [Google Scholar]
- Varkarakis I., Kyriakakis Z., Delis A., Protogerou V., Deliveliotis C. (2004) Long-term results of open transvesical prostatectomy from a contemporary series of patients. Urology 64: 306-310 [DOI] [PubMed] [Google Scholar]


