Abstract
The Working Group on Electrocardiographic Diagnosis of Left Ventricular Hypertrophy, appointed by the Editor of the Journal of Electrocardiology, presents the alternative conceptual model for the ECG diagnosis of left ventricular hypertrophy (LVH). It is stressed that ECG is a record of electrical events, not of mechanical events and/ or anatomical characteristics. Considering the electrical characteristics of pathologically changed myocardium should lead to better understanding and improved clinical usefulness of the ECH in the clinical diagnosis of LVH.
Keywords: Electrocardiography, Left ventricular hypertrophy, Diagnostic conceptual model, Shift in paradigm
“We dance around a ring and suppose—But the secret sits in the middle and knows.” (Robert Frost)
Introduction
Clinicians and electrocardiographers have “danced around the ring” for over a half century, and yet the secret in the middle remains a secret. Perhaps, we should ask ourselves why we engage in this strange dance. The clinician desires an indicator to guide treatment of the patient. Should treatment be intensified? Is the current treatment producing the desired effect? Can we predict the clinical course with more precision? The electrocardiographer has a more complex objective. The investigator wants, above all, to understand the secret message. The clinical electrocardiographer wants to assist the clinician in answering his or her questions. For differing reasons, all of us want to uncover and understand the secret in the middle.
The first statement
The first statement of this group1 outlined the working group’s opinion that interpretation of the electrocardiogram (ECG) should look beyond the prediction of increased left ventricular (LV) mass and aim at predicting clinical outcomes and underlying myocardial alterations leading to the ECG changes. The obstacles to attaining this goal were discussed, and an ambitious pathway to this goal was outlined. This second statement proposes another step, that of modifying the conceptual model, which we use in framing our thoughts about this process and in presenting it to others.
Together, these statements reflect our hope that, instead of saying “these changes reflect left ventricular hypertrophy (LVH),” the ECG report of the future will indicate the probable myocardial basis of the change and the prognostic implications of the array of ECG findings.
The conceptual model
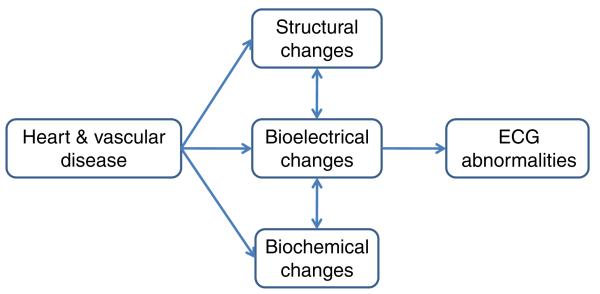
A half century ago, the independent measure of disease was LV dimensions and mass and various associated electrocardiographic alterations. At this time, we used a conceptual model of the task as seen below (Fig. 1).
Fig. 1.

“Classical” simple conceptual model of ECG diagnosis of left ventricular hypertrophy.
As time has gone by and various technical, methodological, and statistical issues have emerged, this model seems vastly oversimplified and inadequate. It has become clear that there is not a direct relationship between LV enlargement and the ECG changes we have used to conclude a “diagnosis” of LVH. Better methods of detecting and quantitating increased LV mass, such as the echocardiogram or magnetic resonance imaging, have shown us that the ECG lacks both sensitivity and specificity in this task.
Although most of us intuitively accept the inadequacy of the above model, the model still stands, as evidenced by repeated attempts to devise ECG criteria to improve the specificity and sensitivity of the ECG in indicating what is termed LVH—increased LV mass. We propose that our efforts will be enhanced by replacing the old model and substituting a new model, which we believe will lead to both better understanding and improved clinical usefulness of the ECG.
Proposed alternative model
Discussion of new model
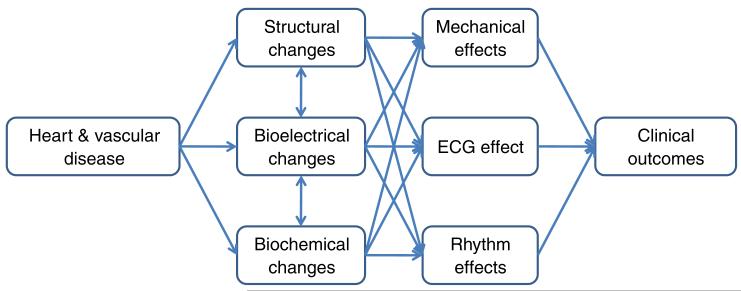
The alternative model is also greatly simplified but conveys the central idea that we believe necessary in rationalizing past observations, in moving ahead to a better understanding of changes in the ECG, and in making it a more useful tool for the clinician and patient. The ECG is a record of electrical events, not mechanical events. We should not assume that these changes are directly related to one another as cause and effect (Fig. 2).
Fig. 2.
Proposed simplified alternative model for ECG diagnosis of left ventricular hypertrophy.
The model asserts that structural events, electrical events, and chemical events are interrelated and imply that the nature and degree of these interrelationships are a critical area for research and better understanding. The need for such research is underscored by the relatively recent observation that the development of electrical manifestations is a predictor of a more severe clinical outcome, independent of anatomical hypertrophy.2-4 The exact manner in which this adverse outcome is produced remains obscure, but it seems logical that all 3 (or more) categories of “events” are involved. In addition to trying to find links between chamber size and the ECG, we should be trying to identify and understand the links between heart disease and mechanical, bioelectrical and biochemical changes, and their interrelations with each other and with clinical outcomes.
Each of the components of the model can and should be expanded to accommodate the known and yet to be discovered complexities of the altered state produced by cardiovascular disease. For example, “Structural Effects” would encompass concentric hypertrophy, dilated hypertrophy, asymmetrical hypertrophy, and so on, as well as changes in cell size and branching. Electrocardiogram effects would include amplitude, ST-T wave changes, P-wave changes, axis deviation, and QRS duration. Chemical effects would include gap junction remodeling and changes in transmitter substances.
Superimposed on this already complex model is a temporal dimension. Heart disease develops slowly, and the changes implied in the model occur even more slowly. A study at an early phase of this development would not produce the same findings as a study at a later phase.
The model can also be expanded to include the prognostic and therapeutic implications inherent in recent reports of a more severe clinical course among those who develop ECG changes of “LVH,” and improved outlook among those in whom these changes are reversed with treatment.5-8 These reports imply that the ECG may be a much more important tool than previously thought and worthy of full exploration.
The expanded version of the model can be envisioned as in the following diagram. It is complex but no less than the physiologic processes it is intended to represent. It is our hope that it will be useful in promoting discussion, new thinking, and new research, especially research across disciplinary bounds, and become a force for moving electrocardiography forward toward uncovering “the secret.” The secret is, of course, not a single fact or concept but a complex interplay of secrets, involving causation, relationships, sequence, and reversibility (Fig. 3).
Fig. 3.
Proposed extended alternative model for ECG diagnosis of left ventricular hypertrophy.
Footnotes
The Working Group on Electrocardiographic Diagnosis of Left Ventricular Hypertrophy appointed by the Editor of the Journal of Electrocardiology: Ljuba Bacharova, E. Harvey Estes, Lia E. Bang, Ian Rowlandson, Joseph A. Hill, Peter W. Macfarlane, and Giuseppe Schillaci.
References
- 1.Bacharova L, Estes H, Bang L, et al. The first statement of the Working Group on Electrocardiographic Diagnosis of Left Ventricular Hypertrophy. J Electrocardiol. 2010;43:197. doi: 10.1016/j.jelectrocard.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease. The Framingham study. Ann Intern Med. 1970;72:813. doi: 10.7326/0003-4819-72-6-813. [DOI] [PubMed] [Google Scholar]
- 3.Schillaci G, Pirro M, Pasqualini L, et al. Mannarino: prognostic significance of isolated, non-specific left ventricular repolarization abnormalities in hypertension. J Hypertens. 2004;22:407. doi: 10.1097/00004872-200402000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Sundström J, Lind L, Arnlöv J, Zethelius B, Andrén B. Lithell HO. Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation. 2001;103:2346. doi: 10.1161/01.cir.103.19.2346. [DOI] [PubMed] [Google Scholar]
- 5.Okin PM, Devereux RB, Nieminen MS, et al. LIFE Study Investigators. Electrocardiographic strain pattern and prediction of cardiovascular morbidity and mortality in hypertensive patients. Hypertension. 2004;44:48. doi: 10.1161/01.HYP.0000132556.91792.6a. [DOI] [PubMed] [Google Scholar]
- 6.Okin PM, Devereux RB, Jern S, et al. Regression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular events. JAMA. 2004;292:2343. doi: 10.1001/jama.292.19.2343. [DOI] [PubMed] [Google Scholar]
- 7.Mathew J, Sleight P, Lonn E, et al. Heart Outcomes Prevention Evaluation (HOPE) Investigators Reduction of cardiovascular risk by regression of electrocardiographic markers of left ventricular hypertrophy by the angiotensin-converting enzyme inhibitor ramipril. Circulation. 2001;104:1615. doi: 10.1161/hc3901.096700. [DOI] [PubMed] [Google Scholar]
- 8.Fagard RH, Staessen JA, Thijs L, et al. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Prognostic significance of electrocardiographic voltages and their serial changes in elderly with systolic hypertension. Hypertension. 2004;44:459. doi: 10.1161/01.HYP.0000142169.17298.54. [DOI] [PubMed] [Google Scholar]