Abstract
Purpose
Diagnosis of cancer in a child can be extremely stressful for parents. Bright IDEAS, a problem-solving skills training (PSST) intervention, has been shown to decrease negative affectivity (anxiety, depression, post-traumatic stress symptoms) in mothers of newly diagnosed patients. This study was designed to determine the specificity of PSST by examining its direct and indirect (eg, social support) effects compared with a nondirective support (NDS) intervention.
Patients and Methods
This randomized clinical trial included 309 English- or Spanish-speaking mothers of children diagnosed 2 to 16 weeks before recruitment. Participants completed assessments prerandomization (T1), immediately postintervention (T2), and at 3-month follow-up (T3). Both PSST and NDS consisted of eight weekly 1-hour individual sessions. Outcomes included measures of problem-solving skill and negative affectivity.
Results
There were no significant between-group differences at baseline (T1). Except for level of problem-solving skill, which was directly taught in the PSST arm, outcome measures improved equally in both groups immediately postintervention (T2). However, at the 3-month follow-up (T3), mothers in the PSST group continued to show significant improvements in mood, anxiety, and post-traumatic stress; mothers in the NDS group showed no further significant gains.
Conclusion
PSST is an effective and specific intervention whose beneficial effects continue to grow after the intervention ends. In contrast, NDS is an effective intervention while it is being administered, but its benefits plateau when active support is removed. Therefore, teaching coping skills at diagnosis has the potential to facilitate family resilience over the entire course of treatment.
INTRODUCTION
Diagnosis and initial treatment of childhood cancer is stressful and even traumatic for parents.1–5 They must face the life threat of the diagnosis and the many logistical demands of the patient's medical care while also managing the family's ongoing daily needs.1,6,7 Although many parents demonstrate emotional resilience, others are at risk for developing symptoms of anxiety and depression, compromising their ability to meet these multiple demands.2,8
It is known that family functioning and social support are important predictors of adjustment9–11 and that better-adjusted parents can buffer their children from the deleterious effects of stressful experiences.12–16 For example, we previously reported that mothers of children with cancer have reduced well-being, which is directly related to the behavioral/emotional adjustment in their healthy children.17
Problem-solving therapy (PST),18–20 a five-step cognitive-behavioral intervention, is used in many settings to address impaired well-being.21–24 The intervention is designed to empower individuals to manage adverse situations by using constructive coping strategies.
The Bright IDEAS Problem-Solving Skills Training (PSST) program, which is based on PST, has been established as an effective intervention for enhancing problem-solving skills and decreasing negative affectivity (ie, anxiety, depression, post-traumatic distress) in mothers of children recently diagnosed with cancer.25–27 Building on PST, problem-solving skills training is intended for individuals who may be highly distressed but do not exhibit clinical psychopathology. Skills training also connotes a sense of personal growth.
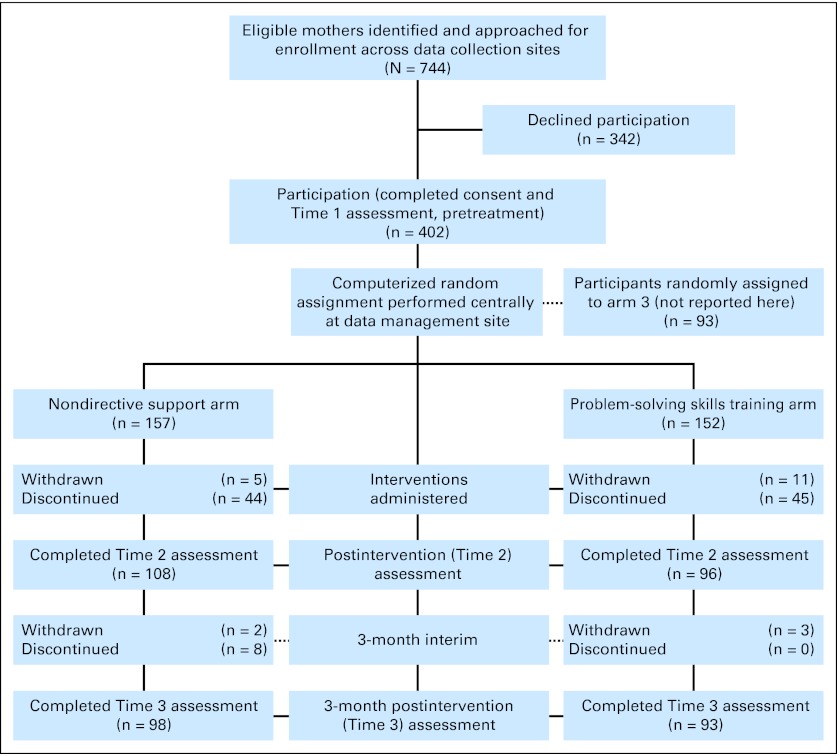
We have conducted large-scale multi-institutional randomized clinical trials (RCTs; CONSORT diagram in Fig 1) of PSST with mothers of children recently diagnosed with cancer according to the conceptual model in Figure 2.26,28 In these studies, PSST was compared with “usual psychosocial care” (ie, the supportive care typically provided at childhood cancer centers in the United States). We hypothesized that the primary effect of PSST would be increased problem-solving skills with a secondary effect of decreased negative affectivity. Our findings confirmed that PSST significantly decreased maternal distress and, in our mediational model, that an increase in problem-solving skills accounted for 27%, 20%, and 26% of the decrease in anxiety, depression, and post-traumatic stress symptoms, respectively. We interpreted the remaining effect as associated with other nonspecific elements of the intervention (eg, social support).26
Fig 1.
CONSORT diagram.
Fig 2.
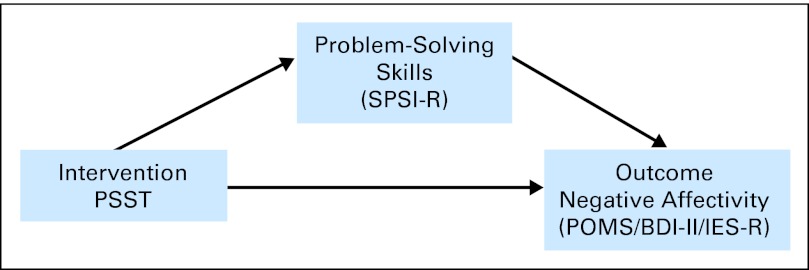
Conceptual model. BDI-II, Beck Depression Inventory; IES-R, Impact of Event Scale-Revised; POMS, Profile of Mood States; PSST, problem-solving skills training; SPSI-R, Social Problem-Solving Inventory-Revised.
Having demonstrated the efficacy of PSST in improving maternal well-being, we sought to examine its specificity by comparing PSST to an alternative intervention that provided similar nonspecific factors (time, attention, support, expectancy, therapeutic alliance) but did not include the specific skills-building characteristics of PSST. To accomplish this, we conducted the current RCT comparing PSST to nondirective support (NDS), a supportive psychotherapy focusing on the central activity of reflective listening, patterned after Rogers' client-centered approach.29 NDS is often used as a comparison condition in studies of cognitive-behavioral interventions.30,31 We chose NDS for two reasons: (1) we wished to provide mothers with a therapeutic experience structurally similar to PSST in number, length, and setting of sessions and degree of therapist support; and (2) nondirective supportive therapies are often used in populations such as ours, although efficacy is understudied. Thus, this study is a comparison of two active interventions, one of which (PSST) was designed to build problem-solving skills in addition to providing general support.
We hypothesized that, compared with mothers receiving NDS, mothers receiving PSST would demonstrate better problem-solving skills and greater reductions in negative affectivity as measured by anxiety, depression, and post-traumatic stress symptoms.
PATIENTS AND METHODS
This multi-institutional RCT was designed to investigate the efficacy of PSST relative to NDS. The original study design included a third arm consisting of PSST aided by the use of a personal digital assistant. Interim analyses indicated that this arm, although feasible, was no more effective than PSST alone and it was terminated.25 This report focuses on the comparison of patients randomly assigned to the PSST alone (our standard intervention) and NDS arms. Note that, throughout the trial, there was an equal probability of being assigned to either PSST alone or NDS, so the exclusion of the third arm does not affect the inferences drawn from the two arms presented here.
Participants
After approval by the institutional review board at each participating site, we recruited mothers 2 to 16 weeks after their child was diagnosed with any form of cancer at four sites (University of Texas/MD Anderson Cancer Center, Children's Hospital Los Angeles, Children's Hospital Pittsburgh, and Doernbecher Pediatric Hospital). Eligibility criteria included ability to speak and read English or Spanish and residence within 50 miles of the center (to reduce transportation issues). To minimize burden, mothers were excluded if their child was in medical crisis as determined by the oncologist.
Procedures
After giving informed consent, participants completed the baseline (T1) assessment and were randomly assigned to a treatment arm by using a block design of six stratified by site and language. Participants received a modest stipend as compensation for their time.
The interventions were delivered by research assistants (RAs) who had graduate education in clinical psychology or behavioral health. Spanish-speaking RAs provided the interventions for Spanish-speaking mothers. The RAs were initially trained together as a group. Site principal investigators then provided weekly supervision to promote therapeutic excellence in intervention delivery according to the specific manual for the arm to which a participant had been randomly assigned. All sessions were digitally recorded. On a monthly basis, treatment integrity procedures tracked RA performance via structured evaluation of randomly selected sessions by reviewers blinded to study arm (see Treatment Integrity).
PSST.
PSST consisted of eight 1-hour individual sessions conducted according to a comprehensive manual.26–28 Problem solving was presented as a general coping skill applicable to a range of challenging circumstances commonly encountered during childhood cancer treatment. To promote engagement, mothers selected the particular problems to address, prompted by a list of issues often confronting parents.
To make the overall philosophy and steps of PSST easily understood, the acronym “Bright IDEAS” and a logo with a graphic of a light bulb were developed. “Bright” signifies the optimism about solving problems essential for successful implementation. The letters I (identify the problem), D (determine the options), E (evaluate options/choose the best), A (act), and S (see if it worked) signify the five essential steps of problem solving. Instructional material included a treatment manual, a pocket-size Bright IDEAS booklet, and a Bright IDEAS refrigerator magnet. (PSST materials are available through the National Cancer Institute/National Institutes of Health National Registry of Evidence-Based Programs and Practices or from the corresponding author.)
Basic therapist interpersonal techniques in PSST include active listening, reflection of feelings, clarification, and support. Delivery of the content of PSST occurred as follows: session 1: rapport building and understanding relevant personal background and medical information; session 2: introduction of PSST and the Bright IDEAS paradigm; sessions 3 to 7: review of the mother's identified problems and promotion of problem-solving strategies and skill; session 8: review of PSST, identification of relapse prevention strategies (eg, persistence, learned optimism), and termination.
NDS.
As in PSST, basic therapist interpersonal techniques include active listening, reflection of feelings, clarification, and support. Essential characteristics of NDS include self-reflection in a safe, nonjudgmental environment and expression and acceptance of feelings.29 Session 1 included initial rapport building and understanding relevant personal background and medical information, and Session 8 included termination. Throughout all eight NDS sessions, the RA maintained focus on active listening and reflecting feelings. This approach is well suited to the initial phases of crisis intervention and can be used with people from diverse backgrounds.29
Both PSST and NDS were delivered by the same RAs to minimize confounding elements in a therapeutic relationship such as friendliness or nonspecific social skills. A detailed treatment manual was developed for NDS similar to that for PSST. The major element distinguishing the two interventions was use or avoidance of teaching problem-solving techniques during sessions. Adherence was monitored through treatment integrity review (see Treatment Integrity).
Measures
Demographic data were collected at baseline. Assessments of problem-solving skills and negative affectivity (operationalized as anxiety, depression, and post-traumatic stress symptoms) were completed at T1 (prerandomization), T2 (immediately postintervention), and T3 (three months postintervention). Expectancy and credibility scales were completed after sessions 1 and 4 of the interventions. To maximize the reliability of our intent-to-treat analyses (see Data Analysis), all participants, except those who withdrew because of their child's medical condition, were asked to complete all assessments whether or not they completed the intervention.
Demographics
Demographic information for children included age, diagnosis, and date of diagnosis and for mothers, it included age, marital status, educational level, and self-reported race/ethnicity.
Problem-Solving Skills
The Social Problem-Solving Inventory-Revised (SPSI-R),32,33 a 52-item self-report, linked to a multidimensional model of social problem-solving has strong reliability and validity estimates.
Negative Affectivity
The Profile of Mood States (POMS) Scale34 is a 65-item self-report of mood with excellent reliability and validity. We used the composite total mood disturbance (TMD) scale as the outcome. The Beck Depression Inventory (BDI-II),35 a 21-item self-report assessing depressive symptoms, is widely used for clinical and research purposes. Internal consistency ranges from 0.73 to 0.92, with good test-retest reliabilities. The Impact of Event Scale-Revised (IES-R),36 a 22-item self-report, assesses post-traumatic stress symptoms in response to a specific event (ie, child's diagnosis with cancer). Reliability and validity are well established.
Credibility and Expectancy
To assess expectations, patients rated the intervention to which they were assigned (PSST or NDS) on credibility (by using a three-item, nine-point credibility scale) and expectancy for improvement (0% to 100% scale) after sessions 1 and 4.
Treatment Integrity
All sessions were digitally recorded and uploaded to a central secure password-protected server. Ten percent of the recordings were randomly flagged for review of process and content by one of three senior investigators on the treatment integrity team. Each had been trained in PSST, had served as a site principal investigator in previous studies, and had been a primary developer of the NDS intervention. The reviewers were blinded to treatment condition. Reviews were conducted by using a structured assessment tool based on the respective manual. In both interventions, sessions were scored on the quality of the therapeutic alliance, supportive interaction, empathy, and being nonjudgmental. In the PSST condition, reviewers rated evidence of discussion of Bright IDEAS, explanation and review of PSST worksheets, and attention to homework or between-session use of problem-solving skills. In the NDS condition, reviewers looked for promotion of self-reflection and nondirective support and, crucially, the absence of discussion of PSST. Inter-rater reliability was determined at the beginning of the study and tested periodically. Compliance with these criteria was more than 95% in both arms.
Data Analysis
Data analyses were generated by using the SAS System for Windows v.9.2 (2006; SAS Institute, Cary, NC). Data from all participants were included by using an intent-to-treat approach. Longitudinal analyses were performed by using a repeated measures model for incomplete data with an unstructured covariance (SAS Proc Mixed). Time was included as an indicator variable in the two postintervention assessments. Note that a pooled estimate at T1, consistent with randomization, was used to increase precision in measuring changes. Child age and maternal age, education, marital status (single v other), and language were included as covariates. The trial was designed to have 89% to 98% power (depending on correlations over time) to detect differences of 0.3 standard deviations. Observed accrual and follow-up reduced power to 54% to 76%. No adjustments were made for multiple comparisons.
RESULTS
As shown in Figure 1, of the 744 eligible mothers, 402 consented to participate: 152 mothers were randomly assigned to the PSST arm and 157 were assigned to the NDS arm. Participants and nonparticipants did not differ in age (P = .42), primary language (P = .19), their child's age (P = .25), child's diagnosis (P = .32), or time since diagnosis (P = .13). Eleven PSST mothers and five NDS mothers withdrew because of their child's medical crisis.
Eighty-eight PSST mothers (58%) and 97 NDS mothers (62%) completed at least six sessions; the primary reason for not completing eight sessions was inability to schedule sessions within the 16-week window allowed. In all, 96 PSST mothers (63%) and 108 NDS mothers (69%) completed the postintervention (T2) assessment. Of those who completed the T2 assessment, 93 PSST mothers (97%) and 98 NDS mothers (91%) also completed the follow-up (T3) assessment. The primary reason for missing assessments was active or passive refusal (69%). Missing assessments were not associated with maternal or child demographics/baseline measures.
There were no between-group differences in demographics or baseline scores on assessment measures (Table 1). The distribution of diagnoses was typical of childhood cancer in the United States. Credibility and expectancy scores were not significantly different in the two groups, with mothers feeling equally positive about the potential benefit of the intervention to which she had been randomly assigned. The overall participation period for each patient averaged approximately 7 months. Table 2 lists the estimated outcome scores over time.
Table 1.
Demographic Characteristics of Study Participants
| Variable | PSST (n = 152) |
NDS (n = 157) |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Mother | ||||
| Age, years (mean ± SD) | 36.3 ± 8.1 | 38.3 ± 8.3 | ||
| Race/ethnicity | ||||
| Hispanic | 70 | 45.5 | 65 | 41.1 |
| Non-Hispanic | 82 | 54.5 | 92 | 58.9 |
| White | 61 | 40.3 | 72 | 46.2 |
| Black | 10 | 7.1 | 12 | 7.6 |
| Other | 11 | 7.1 | 8 | 5.1 |
| Language | ||||
| English | 104 | 68.2 | 109 | 69.6 |
| Spanish | 48 | 31.8 | 48 | 30.4 |
| Highest grade in school (mean ± SD) | 12.2 ± 3.9 | 12.9 ± 4.2 | ||
| Child | ||||
| Age, years (mean ± SD) | 8.2 ± 5.7 | 9.4 ± 6.0 | ||
| Sex | ||||
| Male | 77 | 50.6 | 88 | 56.3 |
| Female | 75 | 49.4 | 69 | 43.7 |
| Diagnosis | ||||
| Leukemia | 77 | 50.0 | 65 | 41.8 |
| Solid tumor | 20 | 13.0 | 25 | 16.5 |
| Brain tumor | 17 | 10.8 | 19 | 12.3 |
| Other | 38 | 24.7 | 48 | 31.0 |
Abbreviations: NDS, nondirective support; PSST, problem-solving skills training; SD, standard deviation.
Table 2.
Estimated Outcome Measure Scores at T1, T2, and T3 by Intervention Group
| Characteristic | Time | Group | Mean | SE | SD |
|---|---|---|---|---|---|
| SPSI-R, total score | T1 | Pooled | 13.3 | 0.15 | 2.65 |
| T2 | NDS | 13.7 | 0.21 | 2.69 | |
| PSST | 14.4 | 0.22 | |||
| T3 | NDS | 14.0 | 0.21 | 2.64 | |
| PSST | 14.6 | 0.22 | |||
| POMS-TMD | T1 | Pooled | 55.7 | 2.36 | 1.26 |
| T2 | NDS | 38.3 | 3.50 | 1.54 | |
| PSST | 33.6 | 3.66 | |||
| T3 | NDS | 35.5 | 3.22 | 1.53 | |
| PSST | 24.2 | 3.28 | |||
| BDI-SQRT | T1 | Pooled | 3.94 | 0.07 | 1.26 |
| T2 | NDS | 3.27 | 0.13 | 1.54 | |
| PSST | 3.25 | 0.13 | |||
| T3 | NDS | 3.13 | 0.13 | 1.53 | |
| PSST | 2.71 | 0.13 | |||
| IES-R, total score | T1 | Pooled | 35.5 | 1.07 | 18.8 |
| T2 | NDS | 29.7 | 1.54 | 18.7 | |
| PSST | 28.2 | 1.62 | |||
| T3 | NDS | 27.4 | 1.50 | 17.2 | |
| PSST | 24.2 | 1.53 |
Abbreviations: BDI-SQRT, Beck Depression Inventory-Square Root Transformation; IES-R, Impact of Event Scale-Revised; NDS, nondirective support; POMS-TMD, Profile of Mood States-Total Mood Disturbance; PSST, problem-solving skills training; SD, standard deviation; SPSI-R, Social Problem-Solving Inventory-Revised; T1, prerandomization; T2, immediately postintervention; T3, at 3-month follow-up.
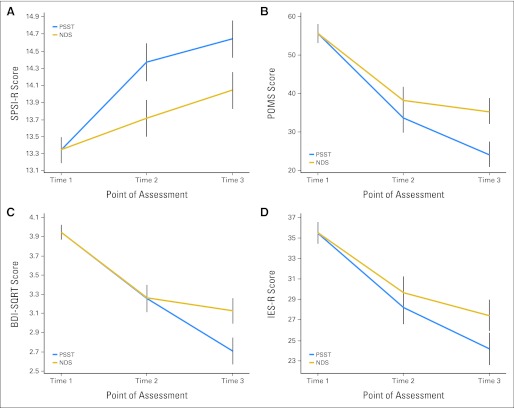
Table 3 indicates that, at T2, significant improvement in problem solving occurred only in the PSST group, but improvements in the three dimensions of negative affectivity occurred in mothers in both conditions, although the changes were slightly greater in the PSST group. Although there continued to be significant improvements in negative affectivity in the PSST group from T2 to T3, only minor improvements were found among the NDS group (Fig 3).
Table 3.
Within-Group Changes in Outcome Measures by Intervention
| Outcome | Desired Direction | Intervention | T2-T1 | P | T3-T2 | P |
|---|---|---|---|---|---|---|
| SPSI-R, total score | Positive | PSST | 1.03 | < .001 | 0.27 | N/S |
| NDS | 0.36 | .046 | 0.33 | .05 | ||
| POMS-TMD | Negative | PSST | −22.1 | < .001 | −9.33 | < .009 |
| NDS | −17.4 | < .001 | −2.78 | N/S | ||
| BDI-SQRT | Negative | PSST | −0.69 | < .001 | −0.54 | < .001 |
| NDS | −0.67 | < .001 | −0.14 | N/S | ||
| IES-R, total score | Negative | PSST | −7.30 | < .001 | −4.01 | .012 |
| NDS | −5.81 | < .001 | −2.27 | N/S |
Abbreviations: BDI-SQRT, Beck Depression Inventory-Square Root Transformation; IES-R, Impact of Event Scale-Revised; NDS, nondirective support; N/S, not significant; POMS-TMD, Profile of Mood States-Total Mood Disturbance; PSST, problem-solving skills training; SPSI-R, Social Problem-Solving Inventory-Revised; T1, prerandomization; T2, immediately postintervention; T3, at 3-month follow-up.
Fig 3.
Estimated outcome measure scores at T1 (prerandomization), T2 (immediately postintervention), and T3 (3-month follow-up). Mean + SE (vertical lines). BDI-SQRT, Beck Depression Inventory-Square Root Transformation; IES-R, Impact of Event Scale-Revised; NDS, nondirective support; POMS, Profile of Mood States; PSST, problem-solving skills training; SPSI-R, Social Problem-Solving Inventory-Revised.
Table 4 lists the between-group differences in outcome. Again, with the exception of the SPSI-R, mothers in the two conditions demonstrated equivalent therapeutic gains in negative affectivity from T1 to T2. However, at T3, the PSST condition proved superior, because continued improvements occurred in that group at a significantly greater rate.
Table 4.
Differences in Outcome Measures, PSST-NDS
| Outcome | Desired Direction | T2 | P | T3 | P |
|---|---|---|---|---|---|
| SPSI-R, total score | Positive | 0.66 | .011 | 0.60 | .023 |
| POMS-TMD | Negative | −4.70 | N/S | −11.2 | .010 |
| BDI-SQRT | Negative | −0.02 | N/S | −0.42 | .016 |
| IES-R, total score | Negative | −1.49 | N/S | −3.24 | .104 |
Abbreviations: BDI-SQRT, Beck Depression Inventory-Square Root Transformation; IES-R, Impact of Event Scale-Revised; NDS, nondirective support; N/S, not significant; POMS-TMD, Profile of Mood States-Total Mood Disturbance; PSST, problem-solving skills training; SPSI-R, Social Problem-Solving Inventory-Revised; T2, immediately postintervention; T3, at 3-month follow-up.
DISCUSSION
The major aim of this RCT was to examine the specificity of PSST in reducing distress in mothers of children recently diagnosed with cancer. For comparison, we developed an active nonspecific behavioral intervention, NDS, which provided the same time and attention from RAs and focused on nonjudgmental support and expression of feelings. Although virtually identical interpersonal elements were present in both conditions, NDS had none of the specific problem-solving elements of PSST, allowing us to measure the specific effects of training mothers in the use of this skill.
We found that, immediately following the intervention (T2), problem-solving skills were significantly higher in the PSST group, as expected, because these skills were specifically taught in PSST. However, there were no significant between-group differences in POMS, BDI-II, or IES-R scores, although improvements were slightly larger for the PSST group. Remarkably, at 3-month follow-up (T3), mothers in the PSST group had continued to improve after treatment cessation (T2), resulting in significant between-group differences (Table 4; Fig 3). Thus, it appears that having a caring person who provides empathic, nondirective support is, indeed, beneficial to the mother's well-being, but the effect is limited to the time that support is actually provided. In contrast, provision of problem-solving skills training allows for sustained and increasing positive effects, presumably a result of teaching coping skills.
We believe this is the first RTC to examine the benefits of a purely supportive intervention (NDS) with mothers of newly diagnosed children with cancer, despite its wide use in this population. Although this study did not have a no-treatment or usual care comparison group, the immediate effects of NDS appear superior to no treatment, as indicated by our previous findings of significant differences between PSST and usual care at T2.26 However, findings of this study indicate that the effects of NDS seem to plateau when the intervention ends.
Our assessment completion rates of 61% for PSST mothers and 63% for NDS mothers were lower than anticipated from previous work. This may be due, in part, to the fact that all participants were engaged in an intervention. In our experience, the possibility of being randomly assigned to usual care (with minimal commitment) may actually be an inducement to enrollment. However, our results are not atypical of the field, reflecting the reality that recruiting and retaining participants in psychosocial oncology research is difficult.37
Another limitation is inclusion of mothers only. Engaging fathers is challenging because of limited accessibility. Many parents are compelled to divide family responsibilities. Fathers often serve as primary wage earners, securing health benefits, as well as the main caregivers for siblings, especially during hospitalization. We recognize that fathers experience distress when their child is diagnosed and could profit from intervention. We must find ways to include them in future projects.
Follow-up was limited to 3 months. Six to 12 months would allow more time to explore the durability of PSST. The benefits of a longer study, however, in which retention may be problematic, must be balanced against a briefer follow-up such as ours with an exceptionally good retention rate of more than 90% between T2 and T3.
Despite these limitations, we remain confident of our findings for several reasons. (1) We had equal participation by mothers in both groups. (2) Intent-to-treat analysis included all enrollees who completed T1 regardless of participation (even zero), reflecting the most conservative estimates of effect. (3) More than 90% of mothers in both groups who completed T2 also completed T3. Thus, changes from T2 to T3, both within and between groups, represent data from the vast majority of patients, maximizing the stability of our findings.
RCTs are critical to identifying the active elements of an intervention. Our findings show that PSST has significant potency beyond the supportive elements and factors such as time and attention that characterize NDS, and these effects continue to manifest after PSST ends. However, our findings clearly support the need for longer follow-up to investigate the durability of these new skills and their effect on distress over time.
We strongly endorse including fathers and other caregivers and believe the simple steps of the Bright IDEAS paradigm are applicable to problems encountered across many illness types and situations. However, face-to-face PSST is labor intensive. Increased computer accessibility, social networking, and online training are likely key to broad dissemination especially because, once designed and implemented, the cost of an online intervention/participant decreases as usage increases. On the basis of experience with a computer-based intelligent agent38,39 and PDA-enhanced PSST,25 development and validation of an effective Internet version of PSST as an alternative to face-to-face training will make PSST a highly accessible intervention, especially at centers with limited behavioral health services. Bright IDEAS has been designated as a research-tested intervention program and is included in the National Registry of Evidence-Based Programs and Practices.
Supplementary Material
Footnotes
Supported by Grant No. R01 CA098954 from the National Institutes of Health, National Cancer Institute (O.J.Z.S.).
Presented in part at the Pediatric Academic Societies' Annual Meeting, Vancouver, British Columbia, Canada, May 1-4, 2010.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information: NCT00234793.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: Diane L. Fairclough, Martha A. Askins, Ernest R. Katz, Robert B. Noll, Robert W. Butler
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Kazak AE, Alderfer M, Rourke MT, et al. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29:211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- 2.Dolgin MJ, Phipps S, Fairclough DL, et al. Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. J Pediatr Psychol. 2007;32:771–782. doi: 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- 3.Boman K, Lindahl A, Björk O. Disease-related distress in parents of children with cancer at various stages after the time of diagnosis. Acta Oncol. 2003;42:137–146. doi: 10.1080/02841860310004995. [DOI] [PubMed] [Google Scholar]
- 4.Norberg AL, Boman KK. Parent distress in childhood cancer: A comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncol. 2008;47:267–274. doi: 10.1080/02841860701558773. [DOI] [PubMed] [Google Scholar]
- 5.Hoekstra-Weebers JE, Jaspers JP, Kamps WA, et al. Risk factors for psychological maladjustment of parents of children with cancer. J Am Acad Child Adolesc Psychiatry. 1999;38:1526–1535. doi: 10.1097/00004583-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Bonner MJ, Hardy KK, Willard VW, et al. Brief report: Psychosocial functioning of fathers as primary caregivers of pediatric oncology patients. J Pediatr Psychol. 2007;32:851–856. doi: 10.1093/jpepsy/jsm011. [DOI] [PubMed] [Google Scholar]
- 7.Goldbeck L. The impact of newly diagnosed chronic paediatric conditions on parental quality of life. Qual Life Res. 2006;15:1121–1131. doi: 10.1007/s11136-006-0068-y. [DOI] [PubMed] [Google Scholar]
- 8.Vrijmoet-Wiersma CM, van Klink JM, Kolk AM, et al. Assessment of parental psychological stress in pediatric cancer: A review. J Pediatr Psychol. 2008;33:694–706. doi: 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- 9.Varni JW, Katz ER, Colegrove R, Jr, et al. Family functioning predictors of adjustment in children with newly diagnosed cancer: A prospective analysis. J Child Psychol Psychiatry. 1996;37:321–328. doi: 10.1111/j.1469-7610.1996.tb01409.x. [DOI] [PubMed] [Google Scholar]
- 10.Varni JW, Katz E. Stress, social support and negative affectivity in children with newly diagnosed cancer: A prospective transactional analysis. Psychooncology. 1997;6:267–278. doi: 10.1002/(SICI)1099-1611(199712)6:4<267::AID-PON277>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 11.Dolgin MJ, Blumensohn R, Mulhern RK, et al. Sibling adaptation to childhood cancer collaborative study: Cross-cultural aspects. J Psychosoc Oncol. 1997;15:1–14. [Google Scholar]
- 12.Robinson KE, Gerhardt CA, Vannatta K. Parent and family factors associated with child adjustment to pediatric cancer. J Pediatr Psychol. 2007;32:400–410. doi: 10.1093/jpepsy/jsl038. [DOI] [PubMed] [Google Scholar]
- 13.Dockerty JD, Williams SM, McGee R, et al. Impact of childhood cancer on the mental health of parents. Med Pediatr Oncol. 2000;35:475–483. doi: 10.1002/1096-911x(20001101)35:5<475::aid-mpo6>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 14.Norberg AL, Lindblad F, Boman KK. Coping strategies in parents of children with cancer. Soc Sci Med. 2005;60:965–975. doi: 10.1016/j.socscimed.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Phipps S, Larson S, Long A, et al. Adaptive style and symptoms of posttraumatic stress in children with cancer and their parents. J Pediatr Psychol. 2006;31:298–309. doi: 10.1093/jpepsy/jsj033. [DOI] [PubMed] [Google Scholar]
- 16.Norberg AL, Lindblad F, Boman KK. Support-seeking, perceived support, and anxiety in mothers and fathers after children's cancer treatment. Psychooncology. 2006;15:335–343. doi: 10.1002/pon.960. [DOI] [PubMed] [Google Scholar]
- 17.Sahler OJ, Roghmann KJ, Mulhern RK, et al. Sibling Adaptation to Childhood Cancer Collaborative Study: The association of sibling adaptation with maternal well-being, physical health, and resource use. J Dev Behav Pediatr. 1997;18:233–243. [PubMed] [Google Scholar]
- 18.D'Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- 19.Chang EC, D'Zurilla TJ. Relations between problem orientation and optimism, pessimism, and trait affectivity: A construct validation study. Behav Res Ther. 1996;34:185–194. doi: 10.1016/0005-7967(95)00046-1. [DOI] [PubMed] [Google Scholar]
- 20.D'Zurilla TJ, Nezu AM. ed 3. New York, NY: Springer Publishing; 2007. Problem-Solving Therapy: A Positive Approach to Clinical Interventions. [Google Scholar]
- 21.Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psychol. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- 22.Nezu AM, Nezu CM, Perri MG. New York, NY: Sage Publications; 2006. Problem solving to promote treatment adherence, in O'Donohue WT, Levensky ER (eds): Promoting Treatment Adherence: A Practical Handbook for Health Care Providers; pp. 135–148. [Google Scholar]
- 23.Nezu AM, Nezu CM. Problem-solving therapy for relapse prevention in depression, In: Richards S, Perri MG, editors. Relapse Prevention for Depression. Washington, DC: American Psychological Association; 2010. pp. 99–130. [Google Scholar]
- 24.Nezu AM, Greenberg LM, Nezu CM. Psychooncology, In: Weiner IB, Craighead WE, editors. The Corsini Encyclopedia of Psychology. New York, NY: John Wiley and Sons; 2010. pp. 1354–1355. [Google Scholar]
- 25.Askins MA, Sahler OJ, Sherman SA, et al. Report from a multi-institutional randomized clinical trial examining computer-assisted problem-solving skills training for English- and Spanish-speaking mothers of children with newly diagnosed cancer. J Pediatr Psychol. 2009;34:551–563. doi: 10.1093/jpepsy/jsn124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sahler OJ, Fairclough DL, Phipps S, et al. Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: Report of a multisite randomized trial. J Consult Clin Psychol. 2005;73:272–283. doi: 10.1037/0022-006X.73.2.272. [DOI] [PubMed] [Google Scholar]
- 27.Varni JW, Sahler OJ, Katz ER, et al. Maternal problem-solving therapy in pediatric cancer. J Psychosoc Oncol. 1999;16:41–71. [Google Scholar]
- 28.Sahler OJ, Varni JW, Fairclough DL, et al. Problem-solving skills training for mothers of children with newly diagnosed cancer: A randomized trial. J Dev Behav Pediatr. 2002;23:77–86. doi: 10.1097/00004703-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Rogers CR. Boston, MA: Houghton Mifflin; 1961. On Becoming a Person: A Therapist's View of Psychotherapy. [Google Scholar]
- 30.Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- 31.Craske MG, Maidenberg E, Bystritsky A. Brief cognitive-behavioral versus nondirective therapy for panic disorder. J Behav Ther Exp Psychiatry. 1995;26:113–120. doi: 10.1016/0005-7916(95)00003-i. [DOI] [PubMed] [Google Scholar]
- 32.D'Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychol Assess. 1990;2:156–163. [Google Scholar]
- 33.D'Zurilla TJ, Nezu AM, Maydeu-Olivares A. North Tonawanda, NY: Multi-Health Systems; 1997. A manual for Social Problem-Solving Inventory-Revised (SPSI-R) [Google Scholar]
- 34.McNair DM, Lorr M, Droppleman LF. San Diego, CA: Educational and Industrial Testing Service; 1992. Manual for the Profile of Mood States. [Google Scholar]
- 35.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 36.Weiss DS, Marmar CR. The Impact of Event Scale-Revised, In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD. New York, NY: Guilford Press; 1997. pp. 399–411. [Google Scholar]
- 37.Kazak AE, Simms S, Alderfer MA, et al. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. J Pediatr Psychol. 2005;30:644–655. doi: 10.1093/jpepsy/jsi051. [DOI] [PubMed] [Google Scholar]
- 38.Marsella SC, Johnson WL, LaBore CM. New York, NY: ACM Press; 2008. Interactive Pedagogical Drama for Health Interventions; pp. 301–308. [Google Scholar]
- 39.Marsella SC, Johnson WL, LaBore C. An interactive pedagogical drama for health interventions. In: Hoppe U, Verdejo F, editors. Artificial Intelligence in Education: Shaping the Future of Learning Through Intelligent Technologies. Amsterdam, the Netherlands: IOS Press; 2003. pp. 341–348. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.