Abstract
Extensive evidence has suggested that at least some of the effects of estrogens on bone are mediated via extranuclear estrogen receptor α signaling. However, definitive proof for this contention and the extent to which such effects may contribute to the overall protective effects of estrogens on bone maintenance have remained elusive. Here, we investigated the ability of a 17β-estradiol (E2) dendrimer conjugate (EDC), incapable of stimulating nuclear-initiated actions of estrogen receptor α, to prevent the effects of ovariectomy (OVX) on the murine skeleton. We report that EDC was as potent as an equimolar dose of E2 in preventing bone loss in the cortical compartment that represents 80% of the entire skeleton, but was ineffective on cancellous bone. In contrast, E2 was effective in both compartments. Consistent with its effect on cortical bone mass, EDC partially prevented the loss of both vertebral and femoral strength. In addition, EDC, as did E2, prevented the OVX-induced increase in osteoclastogenesis, osteoblastogenesis, and oxidative stress. Nonetheless, the OVX-induced decrease in uterine weight was unaltered by EDC but was restored by E2. These results demonstrate that the protection of cortical bone mass by estrogens is mediated, at least in part, via a mechanism that is distinct from the classic mechanism of estrogen action on reproductive organs.
Binding of estrogens to estrogen receptor (ER) α or β leads to direct interactions with DNA or to protein-protein interactions with other transcription factors and thereby activation or repression of the transcriptional machinery (1). In addition, estrogens can evoke nongenomic or nongenotropic actions triggered by the activation of cytoplasmic signaling cascades (2). Such actions result from ligand binding to ERs localized in the plasma membrane or the cytoplasm, followed by downstream kinase–induced changes in the activation of transcription factors that mediate some of the gene regulatory effects of estrogens (3, 4). What is as yet not well understood is which of the diverse biological effects of estrogens are being regulated through the extranuclear-initiated pathway of ER action and which by the nuclear-initiated pathway (5).
Extensive work by us and others during the last 2 decades has suggested that synthetic ligands of the ER that can selectively activate cytoplasmic kinases and kinase-dependent changes in the activity of transcription factors but have reduced or minimal effect on ER conformations that lead to direct or indirect interactions with DNA, may be capable of dissociating the effects of estrogens on bone from their effects on reproductive organs. Based on this evidence, we had proposed that such ligands, dubbed ANGELS (activators of nongenomic estrogen like signaling), may represent a safer alternative to estrogen replacement therapy (3, 6–8). This notion was challenged because 4-estren-3α-17β-diol (estren), the prototypic ANGELS we had used in our earlier work, has weak affinity for the androgen receptor (approximately 30-fold lower than dihydrotestosterone) and can affect reproductive organs under certain experimental conditions (9, 10). Nonetheless, Page et al (11) subsequently demonstrated that an isomer of estren is very potent in maintaining muscle and bone in orchidectomized rats, whereas it has markedly reduced effects on the prostate and seminal vesicles. Moreover, Otto and colleagues (12, 13) have identified compounds that selectively activate Akt and extracellular signal-regulated kinases but exhibit only weak genomic properties; specific ER ligands with such properties exhibit a better dissociation of bone vs uterine and mammary gland effects than 17β-estradiol (E2) and are as effective as E2 in mediating vasorelaxation.
Estrogen deficiency causes an increase in bone remodeling, increased osteoclastogenesis and osteoblastogenesis, increased osteoclast and osteoblast numbers, and increased resorption and formation, albeit unbalanced (14–17). Selective deletion of ERα from cells of the osteoclast lineage increases osteoclastogenesis, abrogates the effects of estrogens on osteoclast apoptosis, increases bone resorption in the female but not the male, and results in decreased cancellous bone (18, 19). However, deletion of ERα from osteoclasts does not affect cortical bone, indicating that effects of estrogens on other cell types may be responsible for their effects on cortical bone. By deleting ERα at different stages of osteoblast differentiation, we have more recently determined that the unliganded ERα present in osteoblast precursors stimulates bone formation in the periosteum by potentiating Wnt/TCF–mediated transcription (20). In addition, osteoblast progenitor ERα mediates a protective effect of estrogens against endocortical, but not cancellous, bone resorption. Therefore, ERα plays essential roles in the accumulation and maintenance of bone mass via direct actions on both osteoblast progenitors and osteoclasts. However, the role of ERα in these 2 cell types is different in distinct bone compartments and the role of ERα in osteoblast progenitors is characterized by both ligand-mediated and ligand-independent actions.
Work by us and others has also suggested that at least some of the beneficial effects of estrogen on bone result from antioxidant actions and that estrogen deficiency accelerates the effect of aging on bone (15, 21). Specifically, estrogens decrease oxidative stress and the activation of p66Shc (a 66-kDa isoform of the growth factor adapter Shc with a pivotal role in oxidative stress, apoptosis, and aging) and antagonize reactive oxygen species (ROS)–induced osteoblast apoptosis and nuclear factor-κB activation and cytokine production by attenuating a PKCβ/p66Shc signaling cascade in osteoblastic cells (22, 23) and decrease ROS production in the bone marrow (22, 24, 25). On the other hand, estrogens attenuate the prosurvival effects of receptor activator of nuclear factor-κB ligand (RANKL) on osteoclasts also via antioxidant mechanisms. These effects of estrogens are preserved in a mouse model bearing an ERα knock-in mutation that prevents binding to DNA (18, 26). Conversely, estrogen deficiency, similar to aging, increases the generation of ROS and the activity of the tumor suppressor p53 and p66Shc in the murine skeleton. Moreover, the adverse effects of the acute loss of ovarian function on the murine skeleton can be prevented by antioxidants (22, 24).
Here, we have attempted to dissect the effects of estrogens on bone that result from non-nuclear–initiated actions using an estrogen-macromolecule conjugate in which estrogen is attached to a large, positively charged nondegradable poly(amido)amine (PAMAM) dendrimer via a hydrolytically stable linkage (27). This 17β-estradiol dendrimer conjugate (EDC), with a short tether linking the PAMAM to E2 through a 17α-phenylethynyl unit, affords optimal ligand access to ERs and gives a binding affinity indistinguishable from that of the E2 derivative used for attachment to the PAMAM dendrimer (28). In breast cancer cells, EDC is excluded from the nucleus, and it is highly effective in stimulating non-nuclear signaling but ineffective in stimulating nuclear ER target gene expression (27). Because PAMAM dendrimers have been widely used for drug delivery in animal models (29, 30), EDC provides a unique means to interrogate non-nuclear estrogen actions in vivo. In support of this notion, we have found that EDC promotes cardiovascular protection but not uterine or breast cancer growth in mice (31). In addition, we showed earlier that EDC is as potent as E2 in attenuating p66Shc phosphorylation and osteoblast apoptosis, as well as in promoting osteoclast apoptosis in vitro (18, 23).
Materials and Methods
Animal experimentation
Fifteen-week-old female C57BL/6 mice were purchased from The Jackson Laboratory (Bar Harbor, Maine). Animals were allowed to acclimate for 1 week before measurement for baseline bone mineral density (BMD). Mice were stratified by spinal BMD measurement and housed 5 per cage with enrichment devices. At 17 weeks of age, the mice were allocated into 5 groups of 20 mice each. The first group was sham operated, and the rest were ovariectomized and implanted with ip osmotic minipumps (model 2006; DURECT Corp, Cupertino, California) prepared to deliver 6 μg/d E2, an estrogen equivalent amount of EDC, the vehicle for E2, or empty dendrimer at a rate identical to that delivered with EDC. The circulating concentrations of E2 and estrogen equivalents of EDC achieved with the same doses in the study by Chambliss et al (31) ranged from 12 to 49 and 14 to 36 nM, respectively. After 6 weeks, BMD measurements were taken, animals were euthanized, and the tissues were dissected for further analyses. An experiment identical to the one described above (with the same number of animals per group) was performed 14 months after the original one to establish the reproducibility of the findings. In addition to all the measurements performed in the original experiment, in the repeat experiment we also determined mechanical strength, osteoblastogenesis, serum osteocalcin and collagen type 1 cross-linked C-telopeptide (CTx), and gene expression profiles. All procedures were approved by the institutional animal care and use committees of University of Arkansas for Medical Sciences and Central Arkansas Veterans Healthcare System.
Bone imaging
BMD measurements were performed by dual-energy x-ray absorptiometry (DEXA) using a PIXImus densitometer (GE Lunar, Madison, Wisconsin), as described previously (32), in mice sedated with 2% isoflurane. The spine window was a rectangle depending on animal body length, reaching from just below the skull to the base of the tail. The femoral window captured the entire left femur. Micro–computed tomography (CT) analysis was done after the bones were dissected, cleaned, fixed in 10% Millonig formalin, and transferred to 100% ethanol, loaded into 10-mm diameter scanning tubes, and imaged (μCT40; Scanco Medical, Brüttiselen, Switzerland), and the vertebral and femoral cancellous bone was analyzed as described previously (33). Transverse CT slices (n = 61) were also acquired at the vertebrae to assess cortical thickness. Scans were integrated into 3-dimensional voxel images (1024 × 1024 pixel matrices for each individual planar stack). A Gaussian filter (σ = 0.8, support = 1) was applied to all analyzed scans. Key parameters were x-ray tube potential = 55 kVp, x-ray intensity = 145 μA, integration time = 200 ms, and threshold = 200 mg/cm3. Image processing language scripts including the “cl_image” command were used to obtain the femoral endocortical and periosteal circumference. Micro-CT measurements are expressed in 3-dimensional nomenclature (34).
Biomechanical testing
The load-bearing properties of the fifth lumbar vertebrae (L5) and left femur were measured using a single-column material testing machine and a calibrated tension/compression load cell (model 5542; Instron Corp, Grove City, Pennsylvania) as described previously (32).
Cell culture
To quantify osteoclast progenitor cells, bone marrow was flushed from femurs and cultured for 4 to 5 days in α-MEM medium, supplemented with 10% FBS, 1% PSG, 30 ng/mL macrophage colony-stimulating factor (M-CSF), and 30 ng/mL RANKL. Osteoclasts were fixed with 10% neutral buffered formalin for 15 minutes and stained for tartrate-resistant acid phosphatase (TRAP). Multinuclear TRAP+ cells were quantified. Colony-forming unit osteoblast (CFU-OB) number was determined in cultured bone marrow from femurs as described previously (35), using guinea pig feeder cells (36), 15% FBS, and 1 mM ascorbate-2-phosphate. Half of the medium was replaced every 5 days. CFU-OBs were enumerated at 25 days of culture after von Kossa staining.
RNA analysis
Total RNA was purified from the fourth lumbar vertebrae (L4) and femoral bone shafts using Ultraspec reagent (Biotecx Laboratories, Houston, Texas), according to the manufacturer's directions. TaqMan quantitative PCR was performed as described previously (37) to determine mRNA levels using the following primer probe sets (Applied Biosystems, Foster City, California): osteocalcin, SEQ_0_OG2-TRETM; cathepsin K, Mm00484039_m1; calcitonin receptor, Mm00432271_m1; Acp5 (TRAP), Mm00475698_m1; and Mrsp2 (mitochondrial ribosomal protein S2), Mm00475528_m1. mRNA expression levels were normalized to the housekeeping gene ribosomal protein S2 using the ΔCt method (38).
Western blot
The phosphorylation status of p66Shc was analyzed by immunoblotting in L5 lysates as described previously (4), using a mouse monoclonal antibody recognizing Ser36 phosphorylated p66Shc (Calbiochem, San Diego, California). Protein levels of p66Shc were analyzed using a rabbit polyclonal antibody recognizing p66Shc (BD Biosciences, Palo Alto, California).
Other assays
Protein concentration was measured using a Bio-Rad detergent–compatible kit (Bio-Rad Laboratories, Hercules, California) as described previously (39). Bone marrow aspirates were extracted from femurs (n = 4 mice per group). ROS were determined using dichlorodihydrofluorescein diacetate dye. Glutathione (GSH) was assayed using a kit from Cayman Chemical Company (Ann Arbor, Michigan). Blood was collected at the time of euthanasia for determination of serum osteocalcin levels, using an ELISA kit (Biomedical Technologies Inc, Stoughton, Massachusetts) and serum CTx levels (Immunodiagnostic Systems Ltd, Fountain Hills, Arizona).
Statistical analysis
All data are reported as the mean ± SD. Group mean values were compared to OVX, vehicle-treated by 1-way ANOVA after determining that the data were normally distributed and exhibited equivalent variances. A P value ≤ .05 was considered significant.
Results
It was established previously that the effects of EDC are mediated via ERα (5). Specifically, we have shown that blocking of ER function by anti-estrogen (ICI182,780) or ERα knockdown using small interfering RNA abolishes EDC-mediated (and E2-mediated) gene stimulation in MCF7 breast cancer cells. To confirm that ER is the mediator of the effects of EDC on bone cells as well, we searched for and found that the effect of both EDC and E2 on murine bone marrow-derived osteoclasts was abrogated by the anti-estrogen ICI (Supplemental Figure 1 published on The Endocrine Society's Journals Online web site at http://mend.endojournals.org.doc).
EDC prevents loss of BMD but not uterine atrophy after OVX
In the present work, we studied the effects of a dose of E2 and an equimolar dose of EDC that were chosen to match the doses of the 2 compounds used in the earlier studies on the efficacy of EDC on the cardiovascular system (31). As a result of this comparison, the dose of E2 in this work is considerably higher than that required for estrogen replacement in ovariectomized mice (7).
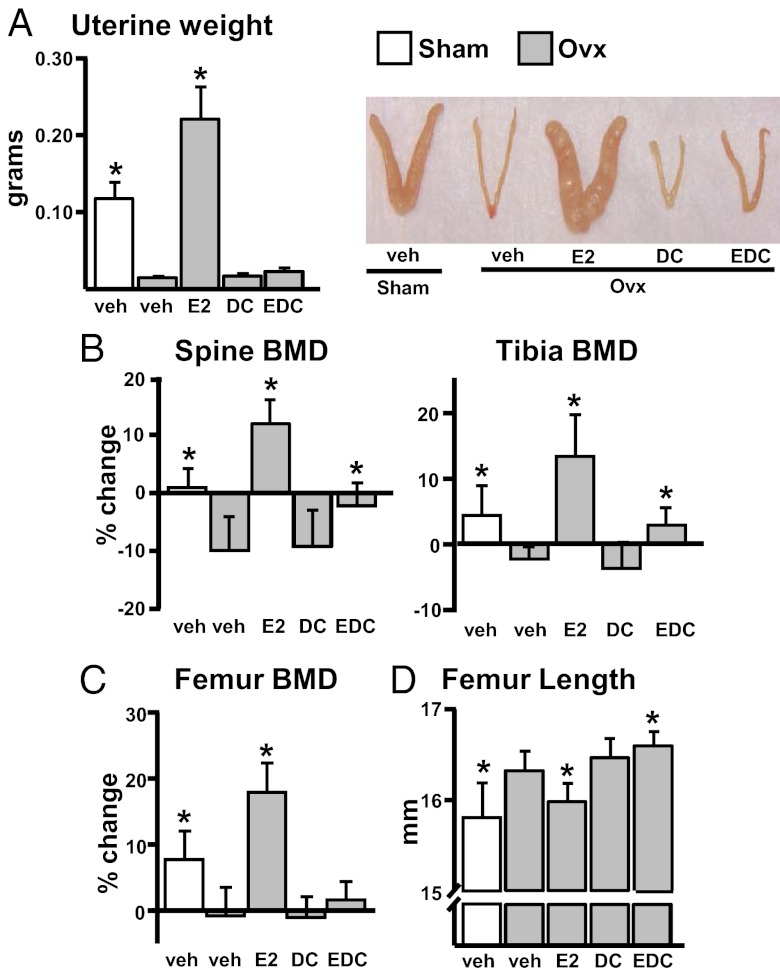
As shown in Figure 1A, the loss of uterine weight caused by OVX was unaffected by EDC (Figure 1A), as had been observed in prior work (7), and is consistent with the inability of EDC to initiate nuclear ER target gene expression. However, with the supraphysiological dose of E2, uterine weight was almost doubled in mice receiving E2 compared with that of the sham controls. In sharp contrast to the lack of an effect of EDC on the uterus, the loss of BMD at the spine and tibia was prevented by EDC and increased over those of the sham controls with E2 replacement (Figure 1B). EDC had no effect on femoral BMD, whereas E2 increased it to levels higher than those of the sham controls (Figure 1C). These results were reproduced in a repeat of this experiment using a similar number of animals per group (Supplemental Figure 2, A–C). Also in contrast to E2, which prevented the OVX-induced increase in femoral length, EDC administration increased, rather than decreased, the OVX-induced lengthening of the femur (Figure 1C), suggesting that closure of the epiphyseal growth plate is the result of nuclear ER target gene expression and that non-nuclear ER signaling may have an effect opposite to that of E2 on growth plate chondrocytes, perhaps by stimulating the production and/or action of growth factors (40, 41).
Figure 1.
The loss of spinal BMD, but not uterine atrophy, after OVX is prevented by EDC. A–D, 15-week-old female mice were sham operated or ovariectomized and treated with the indicated compounds for 6 weeks (n = 20 animals per group). A, Uterine weight determined immediately after euthanasia. B and C, percentage of change from the initial BMD was determined by DEXA measurements 1 day before surgery and before death. D, Femur length was measured with calipers after euthanasia. Bars represent means and SD. *, P < .05 vs OVX, vehicle-treated by 1-way ANOVA. DC, empty dendrimer; veh, vehicle.
EDC preserves cortical, but not cancellous, bone mass in both the spine and the femur
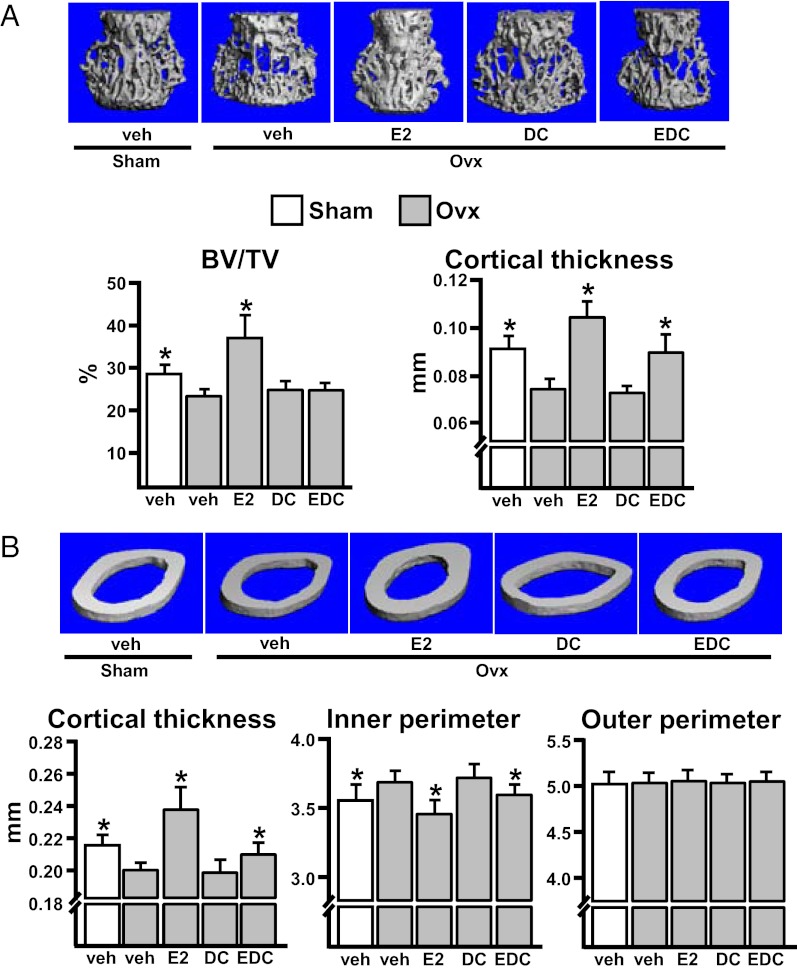
To dissect the effects of EDC on cancellous vs cortical bone envelope, we analyzed vertebrae (Figure 2A) and femurs (Figure 2B) by micro-CT. In contrast to E2, EDC had no effect on the mass or the microarchitecture of the cancellous compartment (Figure 2A and Supplemental Figure 3A). However, similar to E2, EDC prevented the OVX-induced cortical bone loss (Figure 2A and Supplemental Figure 3B), demonstrating that the effect of EDC on spinal BMD was exclusively due to the preservation of bone mass in the cortical compartment. Despite the lack of a discernible effect of EDC on femoral BMD, EDC attenuated the loss of cortical thickness in the femur (Figure 2B and Supplemental Figure 3C). Significant changes could not be discerned in the cancellous compartment of the femur among the groups because very little cancellous bone remained at this age (23 weeks). The effect of EDC on the cortical thickness of the femur was the result of the preservation of bone mass in the endocortical (inner) envelope, as evidenced by the effect of EDC on the endosteal, but not the periosteal (outer), perimeter of the femur (Figure 2B and Supplemental Figure 3D). Therefore, our inability to detect an effect of EDC on femoral BMD change by DEXA could be accounted for by a weaker effect compared with that for the spine. The apparently weaker effect of EDC notwithstanding, it is important to note that the effect of E2 at this higher than replacement dose is a pharmacological rather than a physiological one, documented earlier by several studies (42, 43). E2 was effective in both the cancellous and the cortical compartments.
Figure 2.
EDC preserves cortical bone mass after OVX. A, Cancellous and cortical bone measurements determined by micro-CT in L5. B, Cortical bone measurements determined by micro-CT in the midshaft region of femurs. Bars represent means and SD (n = 20 animals per group). *, P < .05 vs OVX, vehicle-treated by 1-way ANOVA. BV/TV, bone volume per tissue volume; DC, empty dendrimer; veh, vehicle.
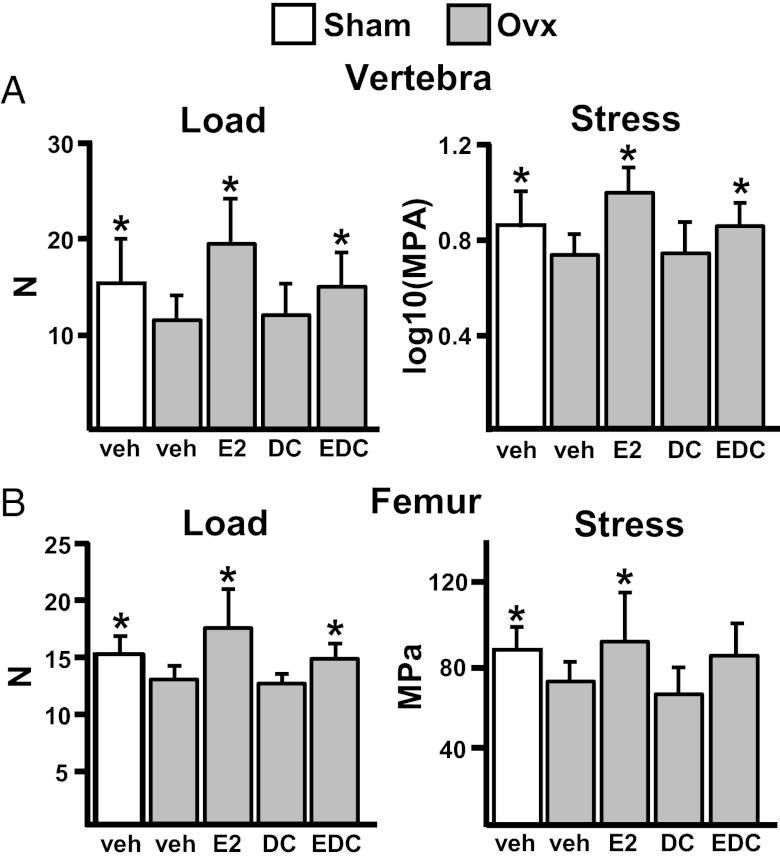
EDC prevents the loss of bone strength in both the spine and the femur
Consistent with its protective effect on the cortical compartment, EDC, similar to E2, preserved vertebral bone strength (Figure 3A). Likewise, EDC prevented, at least partially, the decrease in femoral strength as evidenced by its effect on load at the maximum bending point. E2 prevented the decreased of both load and stress (Figure 3B).
Figure 3.
EDC prevents the loss of bone strength in both the spine and the femur. Load (load tolerated at the breaking point adjusted for bone size) and stress (maximum compressive stress at the breaking point) were measured in L5 (A) and femur (B). Bars represent means and SD (n = 20 animals per group). *, P < .05 vs OVX, vehicle-treated by 1-way ANOVA. DC, empty dendrimer; veh, vehicle.
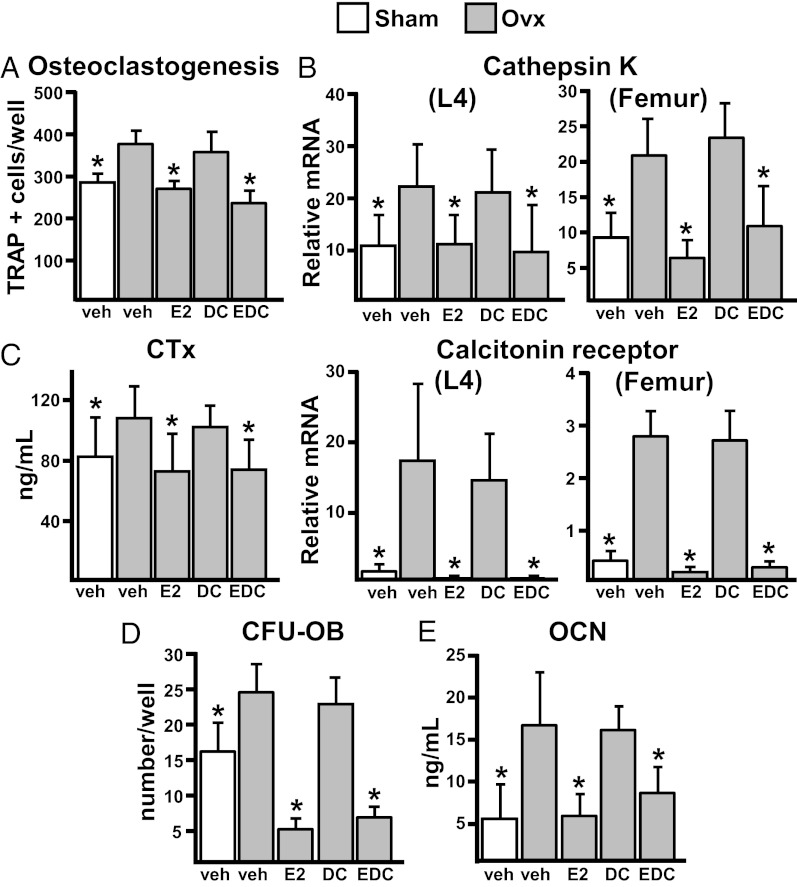
EDC prevents osteoclastogenesis and the increase in bone remodeling
In line with the protective effects of EDC against the OVX-induced loss of cortical bone mass, EDC appeared as effective as E2 in preventing the increased osteoclastogenesis caused by OVX in ex vivo bone marrow cultures (Figure 4A and Supplemental Figure 4). Likewise, EDC prevented the increased expression of the mRNAs for cathepsin K and calcitonin receptor (osteoclast-specific genes) in both the vertebrae and femoral shafts (Figure 4B). Serum CTx levels were also decreased by both EDC and E2 (Figure 4C). Furthermore, EDC was as potent as E2 in preventing the OVX-induced increase in CFU-OBs (Figure 4D). In line with this finding, the serum levels of osteocalcin (an osteoblast-specific marker) were decreased by both EDC and E2 (Figure 4E). The decrease in osteoclastogenesis, osteoblastogenesis, and osteoclast and osteoblast markers by EDC strongly suggests that this compound replicates the antiremodeling effect of estrogens.
Figure 4.
Osteoclastogenesis and the increase in bone remodeling are prevented by EDC. A, Number of TRAP+ cells generated from bone marrow cells, pooled from the femurs of 3 mice per group and plated in triplicate cultures with M-CSF and RANKL for 5 days. B, Cathepsin K and calcitonin receptor mRNA levels by quantitative PCR in vertebral bone and femoral shafts (n = 8 animals per group). C, CTx levels in serum collected immediately before euthanasia (n = 10 animals per group). D, Bone marrow cells described in A were plated in triplicate at a density of 2 × 106 cells/well. CFU-OBs were stained with von Kossa stain after 25 days to detect mineral. E, Osteocalcin (OCN) levels in serum collected immediately before euthanasia (n = 10 animals per group). Bars represent means and SD. *, P < .05 vs OVX, vehicle-treated by 1-way ANOVA. DC, empty dendrimer; veh, vehicle.
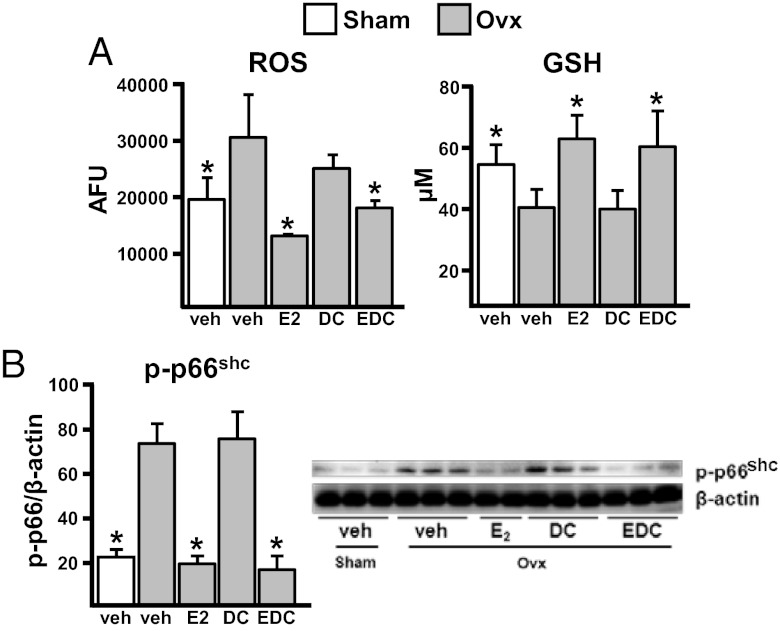
EDC prevents the OVX-induced increase in oxidative stress
In earlier in vitro studies, we had found that EDC exhibited antioxidant properties similar to those of E2 on osteoblasts (23). We, therefore, sought to determine whether EDC had similar antioxidant effects in vivo. Like E2, the EDC prevented the OVX-induced increase in ROS and the decrease in GSH levels in the bone marrow (Figure 5A and Supplemental Figure 5, A and B). In addition, EDC was as effective as E2 in preventing the OVX-induced increase in p66Shc phosphorylation in bone (Figure 5B and Supplemental Figure 5C).
Figure 5.
The OVX-induced increase in oxidative stress is attenuated by EDC. A, ROS levels and GSH activity in bone marrow cells from femurs (n = 4 animals/group). B, Phosphorylation of p66Shc determined by Western blot in vertebral bone lysates; each lane represents 1 animal (n = 2–3 animals per group). Bars represent means and SD. *, P < .05 vs OVX, vehicle-treated by 1-way ANOVA. DC, empty dendrimer; veh, vehicle; AFU, arbitrary fluorescent units.
Discussion
The results of this report indicate that the protective effect of estrogens against endocortical bone resorption does not require nuclear-initiated actions of ERα, because it can be reproduced by EDC, a compound that is incapable of stimulating the nuclear-initiated actions of the ERα. EDC, nonetheless, could not prevent the loss of cancellous bone caused by estrogen deficiency. Taken together with the evidence that deletion of ERα from osteoblast progenitors abrogates the increased endocortical resorption caused by OVX in the mouse (20), whereas osteoclast ERα deletion accounts for the protective effect of estrogens on the cancellous compartment (18, 19), the results of the present report support the contention that the protective effect of EDC against endocortical bone loss results from actions on osteoblast progenitors, not direct effects on osteoclasts. On the other hand, the effects of estrogens on the cancellous compartment must result from nuclear-initiated actions of ERα.
In previous in vitro work, we had found that EDC stimulates murine osteoclast apoptosis as effectively as E2 (18), suggesting that the proapoptotic effect of estrogens on osteoclasts results from DNA binding–independent actions of ERα. The inability of EDC to prevent the loss of cancellous bone caused by estrogen deficiency in vivo in the present study, however, argues against this mechanism and may reflect a true difference between the in vitro and the in vivo situation. That being said, it remains possible that the non-nuclear–initiated direct actions of estrogens have a relatively smaller impact compared with the nuclear-initiated estrogen actions in the cancellous vs the cortical compartment. The latter possibility is supported by evidence that direct or perhaps indirect effects of estrogens on other cell types, for example, B-lymphocytes, also contribute to the loss of bone caused by estrogen deficiency (44).
Both E2 and EDC attenuated the oxidative stress induced by OVX. In this and all our previous work, we have determined oxidative stress by quantifying ROS and GSH in the bone marrow and p66Shc activation in whole bone. Given the relative small number of osteoclasts, compared with the numbers of other hematopoietic cells in the marrow or relative to the numbers of osteoblasts and osteocytes in bone (10 and 100 times lower, respectively) (21), the contribution of osteoclasts to the overall oxidative stress is likely to be negligible. Nevertheless, in contrast to the case with estrogens or antioxidants (24, 26), the loss of cancellous bone by OVX in mice could not be prevented by EDC. Hence, the results of the present report suggest that because of its extranuclear-initiated actions, EDC is incapable of decreasing ROS in mature osteoclasts and the resulting increase in their rate of apoptosis. EDC, nonetheless, can reduce the generation of oxidative stress in other cell types and thereby indirectly affect osteoclastogenesis.
Aging of the skeleton is accompanied by decreased cancellous bone mass and increased formation of pores within cortical bone. Recent analysis of cortical bone loss with high-resolution peripheral CT of the radius and postmortem femurs of women aged between 50 and 80 years has revealed that most bone loss in old age is the result of increased intracortical porosity (45). This may account for a large portion of the increase in nonvertebral fractures after age 65 in humans. At this stage, it is difficult to judge whether a compound with protective effects on cortical, but not cancellous, bone and no effects on reproductive organs, such as EDC, would be useful in the management of osteoporosis in postmenopausal women, nor can one predict the dose of EDC that would be required for replacing the level of estrogens lost after menopause. Nonetheless, the results of the present report demonstrate that several effects of estrogens on bone, including their protective effect on cortical bone mass and their antioxidant properties (at least in most other cell types with the exception of mature osteoclasts), are indeed mediated by a mechanism distinct from their classic genotropic action on reproductive organs.
Acknowledgments
We thank C. O'Brien for critical reading of the manuscript, A. Warren and S. Berryhill for technical assistance, and L. Elrod for help with the preparation of the manuscript.
This work was supported by the National Institutes of Health (Grants P01 AG13918 [to S.C.M.], R01 AR56679 [to M.A.], F32 AR061956-02 [to S.M.B.], R37 DK015556 [to J.A.K.], and P50 AT006268 [to B.S.K.]); the Biomedical Laboratory Research and Development Service of the Veteran's Administration Office of Research and Development [Grants I01 BX001405 [to S.C.M.], I01 BX000514 [to R.L.J.], and I01 BX000436 [to R.S.W.]); and the University of Arkansas for Medical Sciences Translational Research Institute and Tobacco Settlement funds.
Disclosure Summary: S.C.M. and J.A.K. are members of the Scientific Advisory Board and hold stock in Radius Health, Inc., a biotech company developing treatments for osteoporosis. B.S.K., R.S.W., and R.L.J. hold stock in Radius Health, Inc. P.W.S. received research funding from Pfizer, Inc. The other authors have nothing to disclose.
Footnotes
- BMD
- bone mineral density
- CFU-OB
- colony-forming unit osteoblast
- CTx
- collagen type 1 cross-linked C-telopeptide
- DEXA
- dual-energy x-ray absorptiometry
- E2
- 17β-estradiol
- EDC
- 17β-estradiol dendrimer conjugate
- ER
- estrogen receptor
- GSH
- glutathione
- M-CSF
- macrophage colony-stimulating factor
- PAMAM
- poly(amido)amine
- RANKL
- receptor activator of nuclear factor-κb ligand
- ROS
- reactive oxygen species
- TRAP
- tartrate-resistant acid phosphatase.
References
- 1. Tsai MJ, O'Malley BW. Molecular mechanisms of action of steroid/thyroid receptor superfamily members. Annu Rev Biochem. 1994;86:451–486 [DOI] [PubMed] [Google Scholar]
- 2. Hammes SR, Levin ER. Minireview: recent advances in extranuclear steroid receptor actions. Endocrinology. 2011;152:4489–4495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kousteni S, Bellido T, Plotkin LI, et al. Nongenotropic, sex-nonspecific signaling through the estrogen or androgen receptors: dissociation from transcriptional activity. Cell. 2001;104:719–730 [PubMed] [Google Scholar]
- 4. Kousteni S, Han L, Chen J-R, et al. Kinase-mediated regulation of common transcription factors accounts for the bone-protective effects of sex steroids. J Clin Invest. 2003;111:1651–1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Madak-Erdogan Z, Kieser KJ, Kim SH, Komm B, Katzenellenbogen JA, Katzenellenbogen BS. Nuclear and extranuclear pathway inputs in the regulation of global gene expression by estrogen receptors. Mol Endocrinol. 2008;22:2116–2127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Manolagas SC, Kousteni S, Chen JR, Schuller M, Plotkin L, Bellido T. Kinase-mediated transcription, activators of nongenotropic estrogen-like signaling (ANGELS), and osteoporosis: a different perspective on the HRT dilemma. Kidney Int Suppl. 2004;91:S41–S49 [DOI] [PubMed] [Google Scholar]
- 7. Kousteni S, Chen JR, Bellido T, et al. Reversal of bone loss in mice by nongenotropic signaling of sex steroids. Science. 2002;298:843–846 [DOI] [PubMed] [Google Scholar]
- 8. Manolagas SC, Kousteni S. Perspective: nonreproductive sites of action of reproductive hormones. Endocrinology. 2001;142:2200–2204 [DOI] [PubMed] [Google Scholar]
- 9. Windahl SH, Galien R, Chiusaroli R, et al. Bone protection by estrenes occurs through non-tissue-selective activation of the androgen receptor. J Clin Invest. 2006;116:2500–2509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Manolagas SC, Jilka RL, Kousteni S, et al. Response to Windahl et al. J Clin Invest. 2006;116:2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Page ST, Marck BT, Tolliver JM, Matsumoto AM. Tissue selectivity of the anabolic steroid, 19-nor-4-androstenediol-3β,17β-diol in male Sprague Dawley rats: selective stimulation of muscle mass and bone mineral density relative to prostate mass. Endocrinology. 2008;149:1987–1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wessler S, Otto C, Wilck N, Stangl V, Fritzemeier KH. Identification of estrogen receptor ligands leading to activation of non-genomic signaling pathways while exhibiting only weak transcriptional activity. J Steroid Biochem Mol Biol. 2006;98:25–35 [DOI] [PubMed] [Google Scholar]
- 13. Otto C, Fuchs I, Altmann H, et al. In vivo characterization of estrogen receptor modulators with reduced genomic versus nongenomic activity in vitro. J Steroid Biochem Mol Biol. 2008;111:95–100 [DOI] [PubMed] [Google Scholar]
- 14. Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev. 2000;21:115–137 [DOI] [PubMed] [Google Scholar]
- 15. Manolagas SC. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev. 2010;31:266–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Riggs BL, Khosla S, Melton LJ., III Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23:279–302 [DOI] [PubMed] [Google Scholar]
- 17. Manolagas SC, Kousteni S, Jilka RL. Sex steroids and bone. Recent Prog Horm Res. 2002;57:385–409 [DOI] [PubMed] [Google Scholar]
- 18. Martin-Millan M, Almeida M, Ambrogini E, et al. The estrogen receptor alpha in osteoclasts mediates the protective effects of estrogens on cancellous but not cortical bone. Mol Endocrinol. 2010;24:323–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nakamura T, Imai Y, Matsumoto T, et al. Estrogen prevents bone loss via estrogen receptor alpha and induction of Fas ligand in osteoclasts. Cell. 2007;130:811–823 [DOI] [PubMed] [Google Scholar]
- 20. Almeida M, Iyer S, Martin-Millan M, et al. Estrogen receptor-alpha signaling in osteoblast progenitors stimulates cortical bone accrual. J Clin Invest. 2013;123:394–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Manolagas SC, Parfitt AM. What old means to bone. Trends Endocrinol Metab. 2010;21:369–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Almeida M, Han L, Martin-Millan M, et al. Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. J Biol Chem. 2007;282:27285–27297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Almeida M, Han L, Ambrogini E, Bartell SM, Manolagas SC. Oxidative stress stimulates apoptosis and activates NF-κB in osteoblastic cells via a PKCβ/p66shc signaling cascade: counter regulation by estrogens or androgens. Mol Endocrinol. 2010;24:2030–2037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lean JM, Davies JT, Fuller K, et al. A crucial role for thiol antioxidants in estrogen-deficiency bone loss. J Clin Invest. 2003;112:915–923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grassi F, Tell G, Robbie-Ryan M, et al. Oxidative stress causes bone loss in estrogen-deficient mice through enhanced bone marrow dendritic cell activation. Proc Natl Acad Sci USA. 2007;104:15087–15092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Almeida M, Martin-Millan M, Ambrogini E, et al. Estrogens attenuate oxidative stress, osteoblast differentiation and apoptosis by DNA binding-independent actions of the ERα. J Bone Miner Res. 2010;25:769–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harrington WR, Kim SH, Funk CC, et al. Estrogen dendrimer conjugates that preferentially activate extranuclear, nongenomic versus genomic pathways of estrogen action. Mol Endocrinol. 2006;20:491–502 [DOI] [PubMed] [Google Scholar]
- 28. Kim SH, Katzenellenbogen JA. Hormone-PAMAM dendrimer conjugates: polymer dynamics and tether structure affect ligand access to receptors. Angew Chem Int Ed Engl. 2006;45:7243–7248 [DOI] [PubMed] [Google Scholar]
- 29. Kukowska-Latallo JF, Candido KA, Cao Z, et al. Nanoparticle targeting of anticancer drug improves therapeutic response in animal model of human epithelial cancer. Cancer Res. 2005;65:5317–5324 [DOI] [PubMed] [Google Scholar]
- 30. Wu G, Barth RF, Yang W, Kawabata S, Zhang L, Green-Church K. Targeted delivery of methotrexate to epidermal growth factor receptor-positive brain tumors by means of cetuximab (IMC-C225) dendrimer bioconjugates. Mol Cancer Ther. 2006;5:52–59 [DOI] [PubMed] [Google Scholar]
- 31. Chambliss KL, Wu Q, Oltmann S, et al. Non-nuclear estrogen receptor alpha signaling promotes cardiovascular protection but not uterine or breast cancer growth in mice. J Clin Invest. 2010;120:2319–2330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. O'Brien CA, Jilka RL, Fu Q, Stewart S, Weinstein RS, Manolagas SC. IL-6 is not required for parathyroid hormone stimulation of RANKL expression, osteoclast formation, and bone loss in mice. Am J Physiol Endocrinol Metab. 2005;289:E784–E793 [DOI] [PubMed] [Google Scholar]
- 33. Jilka RL, Almeida M, Ambrogini E, Han L, Roberson PK, Weinstein RS, Manolagas SC. Decreased oxidative stress and greater bone anabolism in the aged, as compared to the young, murine skeleton by parathyroid hormone. Aging Cell. 2010;9:851–867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010;25:1468–1486 [DOI] [PubMed] [Google Scholar]
- 35. DiGregorio G, Yamamoto M, Ali A, Abe E, Roberson P, Manolagas SC, Jilka RL. Attenuation of the self-renewal of transit amplifying osteoblast progenitors in the murine bone marrow by 17β-estradiol. J Clin Invest. 2001;107:803–812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kuznetsov S, Robey PG. Species differences in growth requirements for bone marrow stromal fibroblast colony formation in vitro. Calcif Tissue Int. 1996;59:265–270 [DOI] [PubMed] [Google Scholar]
- 37. Almeida M, Han L, Bellido T, Manolagas SC, Kousteni S. Wnt proteins prevent apoptosis of both uncommitted osteoblast progenitors and differentiated osteoblasts by β-catenin-dependent and -independent signaling cascades involving Src/ERK and phosphatidylinositol 3-kinase/AKT. J Biol Chem. 2005;280:41342–41351 [DOI] [PubMed] [Google Scholar]
- 38. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods. 2001;25:402–408 [DOI] [PubMed] [Google Scholar]
- 39. Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;104:1363–1374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kousteni S, Almeida M, Han L, Bellido T, Jilka RL, Manolagas SC. Induction of osteoblast differentiation by selective activation of kinase-mediated actions of the estrogen receptor. Mol Cell Biol. 2007;27:1516–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Callewaert F, Sinnesael M, Gielen E, Boonen S, Vanderschueren D. Skeletal sexual dimorphism: relative contribution of sex steroids, GH-IGF1, and mechanical loading. J Endocrinol. 2010;207:127–134 [DOI] [PubMed] [Google Scholar]
- 42. Tobias JH, Chow J, Colston KW, Chambers TJ. High concentrations of 17β-estradiol stimulate trabecular bone formation in adult female rats. Endocrinology. 1991;128:408–412 [DOI] [PubMed] [Google Scholar]
- 43. Samuels A, Perry MJ, Goodship AE, Fraser WD, Tobias JH. Is high-dose estrogen-induced osteogenesis in the mouse mediated by an estrogen receptor? Bone. 2000;27:41–46 [DOI] [PubMed] [Google Scholar]
- 44. Onal M, Xiong J, Chen X, et al. Receptor activator of nuclear factor κB Ligand (RANKL) protein expression by B lymphocytes contributes to ovariectomy-induced bone loss. J Biol Chem. 2012;287:29851–29860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zebaze RM, Ghasem-Zadeh A, Bohte A, et al. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet. 2010;375:1729–1736 [DOI] [PubMed] [Google Scholar]