Abstract
Objectives
Position stability of the abutment should be investigated in four implant systems with a conical implant–abutment connection.
Materials and methods
Previously developed formulas and an established experimental setup were used to determine the position stability of the abutment in the four implant systems with a conical implant–abutment connection and different positional index designs: The theoretical rotational freedom was calculated by using the dimensions of one randomly selected implant per system for approximated geometric models. Experimentally, the rotation, the vertical displacement, and canting moments of the abutment after multiple repositioning and hand tightening of the abutment screw were investigated.
Results
The experimental rotation and vertical displacement differed between the implant systems tested. The analytical and experimental results for the rotation of the abutment clearly deviated in the three implant systems.
Conclusions
Malpositioning of the abutment was possible in all the implant systems tested. Deviating theoretical and experimental results suggest high manufacturing tolerances during fabrication of the implant components.
Clinical relevance
Position stability of the abutment is essential for precisely fitting implant-supported superstructures.
Keywords: Rotational freedom, Vertical displacement, Conical, Positional index, Hexagon, Cam–groove design
Introduction
Mechanical complications still exist in implant dentistry including fractures or mobility of the superstructure and the abutment screw [1, 2]. These complications have a multifactorial etiology [3–5]. Current studies indicate that position stability of the implant–abutment connection (IAC) is a decisive factor for prosthesis misfit [6, 7] and mechanical complications [8]. Position stability of the implant–abutment connection is essential, since multiple repositioning of the implant components is necessary during fabrication of the superstructure by the dental technician and the dentist [9, 10].
Rotational position stability of IACs with different positional index designs has been investigated [11–16]. The results indicate that the rotational freedom of different positional indices of the second and third generation is similar to that of hexagonal indices of the first generation [16]. Theoretical calculations show that the position stability depends on the geometric design of the index and the manufacturing tolerances [14, 15].
Conical connections were developed to achieve a friction-based fit of the implant components [16–20]. Little has been published about the repositioning accuracy of the abutment in conical implant–abutment connections [16, 21].
In the present study, position stability of the abutment in various implant systems with a conical implant–abutment connection was examined in vitro, and its rotational freedom was theoretically calculated. Working hypotheses were that the theoretical optimal result for the rotational freedom of the index corresponds to the findings of the experiment and that the experimental results do not differ between the implant systems tested.
Materials and methods
The position stability of different implant systems with a conical implant–abutment connection was investigated: Nobel Active (S1), Bone Level (S2), Ankylos C/X (S3), and Conelog (S4) (Table 1, Fig. 1). Seven implants and rotation-safe abutments of each implant system were purchased regularly. To allow comparability of the results, implants with similar diameters were ordered (Table 1).
Table 1.
Specifications of the implants and abutments used
| System | Ident. | Article no. | Lot no. | Ident. | Mat | Article no. | Lot no. | Manufacturer |
|---|---|---|---|---|---|---|---|---|
| Nobel Active (S1) | Internal RP, 4.3 × 11.5 mm | 34132 | 707722 | Esthetic abutment | Ti | 34199 | 708540 | Nobel Biocare AB, SE-40226 Göteborg, Sweden |
| 696896 | 708540 | |||||||
| 696896 | 708540 | |||||||
| 707023 | 708540 | |||||||
| 707023 | 708540 | |||||||
| 707023 | 708540 | |||||||
| 707023 | 708540 | |||||||
| Bone Level (S2) | Bone Level, 4.1 RC SLActive, 12 mm | 021.4112 | K6756 | Universal abutment | Ti | 022.2104 | X3223 | Institut Straumann AG, CH-4002 Basel, Switzerland |
| F7007 | R8701 | |||||||
| F7007 | R8701 | |||||||
| F7007 | R8701 | |||||||
| F7007 | R8701 | |||||||
| F7007 | R8701 | |||||||
| F7007 | R8701 | |||||||
| Ankylos (S3) | C/X Implant, B14∅4.5/L14 | 170556/31010440 | 0020039200 | Regular/X abutment GH3.0/A0 | Ti | 31024130 | 20035835 | FRIADENT GmbH, 68229 Mannheim, Germany |
| 0020034919 | 20035835 | |||||||
| 0020034919 | 20035835 | |||||||
| 0020039201 | 20035835 | |||||||
| 0020039201 | 20035835 | |||||||
| 0020038909 | 20035835 | |||||||
| 0020038909 | 20035835 | |||||||
| Conelog (S4) | Screw-Line ConeLog Implant Promote plus ∅4.3 L11 | E-C1062.4311 | 0000029157 | Universal abutment | Ti | C2211.4300 | 0000028679 | Camlog Biotechnologies AG, CH-4053 Basel, Switzerland |
| 0010024599 | 0010027056 | |||||||
| 0010024599 | 0010027056 | |||||||
| 0010024599 | 0010027056 | |||||||
| 0010024599 | 0010027056 | |||||||
| 0010024599 | 0010027056 | |||||||
| 0010024599 | 0010027056 |
Fig. 1.
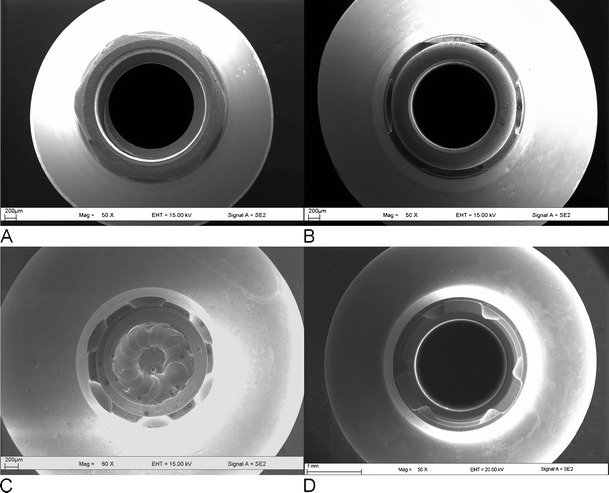
Abutments showing the positional index designs. a S1: Nobel Active. Conical implant–abutment connection with a cone angle of 12° and an internal hexagonal positional index. b S2: Bone Level. Conical implant–abutment connection with a cone angle of 15° and cams and grooves. c S3: Ankylos C/X. Conical implant–abutment connection with a cone angle of 5.7° and six cams and grooves. d S4: Conelog. Conical implant–abutment connection with a cone angle of 7.5°and three cams and grooves
Theoretical calculation
Calculation of the rotational freedom of the abutment
The measured dimensions of the positional index of one randomly selected implant and abutment per system (Table 1) [15] were used to calculate the maximum rotational freedom of the positional index designs by utilizing previously developed closed-form formulas for approximated geometric models [14, 15]. The clearance between implant and abutment was set at 20 μm according to the previous investigation [15].
Experimental investigation
Experimental setup
An established experimental setup [16] was used. The six implants of each system were fixated in prefabricated stainless steel models that were manufactured to imitate a clinical situation. The implants were fixated in angulations of 0° (implants 1 and 6), 5° (implants 2 and 5), and 15° (implants 3 and 4).
Experiment
The experiment was performed as described with the exception that two test persons having different implantological skills dis- and reassembled the implant–abutment test body complexes 20 times each by hand tightening the screw [16]. The test persons were specified as Pe1 (=person with implantological skills) and Pe2 (=person without implantological skills).
Statistical analysis
The mean and standard deviation of the experimental values were calculated. Since the mean and median were skewed, the median and quartiles were used for the analysis. The maximum bidirectional displacement was expressed by the maximum range of deviation (most positive value + most negative value).
A two-factorial nonparametric analysis for repeated measurements [22] was used to analyze the influence of the implant system and the test person on the outcomes. The implant system was set as a whole-plot factor and the test person as a split-plot factor.
Statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA) and SAS 9.1 (SAS Institute Inc., Cary, NC, USA). A P value <0.05 was considered statistically significant.
Results
Theoretical calculation
Rotation of the abutment
Hexagonal positional index design
Using the formula for polygonal positional index designs, a rotational freedom of 3.1° results for S1 (Table 2).
Table 2.
Values inserted into the previously developed formulas to calculate the rotational freedom of the positional index for the implant systems used
| Polygon | R (mm), width across vertices | n, number of vertices | C (mm), clearance between implant and abutment | α (°), rotational freedom |
|---|---|---|---|---|
| S1 | 1.52 | 6 | 0.02 | 3.1 |
| Cam–groove | R (mm), distance of contact point to rotational axis | δ (°), angle between R and implant wall | C (mm), clearance between implant and abutment | α (°), rotational freedom |
| S2 | 1.35 | 2.0 | 0.02 | 1.7 |
| S3 | 1.00 | 29.5 | 0.02 | 2.6 |
| S4 | 1.15 | 18.1 | 0.02 | 2.1 |
Cam–groove design
The maximum rotational freedom of the systems having a cam–groove connection design was calculated using a universal equation. A theoretical rotational freedom of 1.7° results for S2, of 2.6° for S3, and of 2.1° for S4 (Table 2).
Experimental investigation
Rotation of the abutment
The median rotation of S1 (hexagon) was 1.19° (0.39°, 2.11 °), and the maximum range of rotational movement of the abutment was 7.27°. S2 (cam–groove) showed a similar median rotational displacement of 1.09° (0.79°, 1.39°) with a smaller maximum range of 4.29°. The system S3 (cam–groove) displayed a median rotation of 0.82° (0.33°, 1.95°) showing a maximum range of 6.22°. S4 (cam–groove) showed a median rotation value of 0.25° (0.15°, 0.34°) and a maximum range of 2.14°. The minimal and maximal values for each implant system and test person are shown in Table 3. Rotational displacements of the abutments tested differed significantly between the implant systems (P < 0.001) with S4 showing significantly lower rotational freedom than S1, S2, and S3 (all P < 0.001). S1, S2, and S3 were not different (S1 vs. S2, P = 0.718; S1 vs. S3, P = 0.273; S2 vs. S3, P = 0.423). The test person did influence the outcome (P < 0.001).
Table 3.
Minimal (min) and maximal (max) experimental rotational and vertical displacement measurement values for each implant system and test person
| System/implant | Person 1 | Person 2 | ||
|---|---|---|---|---|
| Rotation | ||||
| Min (°) | Max (°) | Min (°) | Max (°) | |
| S1 | 0.07 | 3.95 | <0.01 | 3.23 |
| 1 | 0.14 | 3.41 | 0.02 | 2.59 |
| 2 | 0.07 | 3.37 | <0.01 | 1.31 |
| 3 | 0.86 | 3.88 | 0.01 | 1.03 |
| 4 | 0.13 | 2.29 | 0.01 | 3.23 |
| 5 | 1.15 | 3.95 | 0.04 | 0.69 |
| 6 | 0.60 | 3.28 | 0.04 | 0.63 |
| S2 | 0.38 | 2.58 | 0.04 | 2.50 |
| 1 | 0.55 | 1.30 | 0.22 | 1.40 |
| 2 | 0.38 | 1.22 | 0.25 | 1.24 |
| 3 | 0.44 | 2.58 | 0.25 | 2.50 |
| 4 | 1.00 | 1.89 | 0.14 | 1.89 |
| 5 | 1.25 | 1.48 | 0.41 | 1.62 |
| 6 | 0.61 | 2.00 | 0.04 | 1.39 |
| S3 | 0.13 | 3.84 | 0.02 | 4.20 |
| 1 | 0.87 | 3.56 | 0.02 | 1.05 |
| 2 | 1.24 | 3.42 | 0.04 | 4.10 |
| 3 | 0.51 | 3.84 | 0.29 | 4.20 |
| 4 | 1.53 | 3.23 | 0.05 | 0.76 |
| 5 | 0.14 | 1.73 | 0.14 | 1.55 |
| 6 | 0.13 | 3.15 | 0.20 | 1.49 |
| S4 | <0.01 | 1.30 | <0.01 | 1.72 |
| 1 | 0.07 | 0.88 | <0.01 | 0.88 |
| 2 | <0.01 | 1.28 | 0.05 | 0.93 |
| 3 | <0.01 | 1.21 | <0.01 | 0.77 |
| 4 | 0.01 | 1.17 | <0.01 | 0.39 |
| 5 | 0.02 | 0.89 | <0.01 | 0.28 |
| 6 | 0.04 | 1.30 | <0.01 | 1.72 |
| Vertical displacement | ||||
| Min (μm) | Max (μm) | Min (μm) | Max (μm) | |
| S1 | <1 | 21 | <1 | 14 |
| 1 | <1 | 13 | <1 | 12 |
| 2 | <1 | 12 | <1 | 14 |
| 3 | <1 | 19 | <1 | 8 |
| 4 | <1 | 21 | <1 | 10 |
| 5 | <1 | 11 | <1 | 7 |
| 6 | <1 | 7 | <1 | 9 |
| S2 | <1 | 8 | <1 | 8 |
| 1 | <1 | 6 | <1 | 5 |
| 2 | <1 | 5 | <1 | 5 |
| 3 | <1 | 8 | <1 | 7 |
| 4 | <1 | 8 | <1 | 8 |
| 5 | <1 | 6 | <1 | 6 |
| 6 | <1 | 6 | <1 | 6 |
| S3 | <1 | 11 | <1 | 7 |
| 1 | <1 | 7 | <1 | 7 |
| 2 | <1 | 9 | <1 | 7 |
| 3 | <1 | 5 | <1 | 4 |
| 4 | <1 | 4 | <1 | 2 |
| 5 | <1 | 11 | <1 | 5 |
| 6 | <1 | 6 | <1 | 3 |
| S4 | <1 | 25 | <1 | 17 |
| 1 | <1 | 10 | <1 | 9 |
| 2 | <1 | 9 | <1 | 7 |
| 3 | <1 | 6 | <1 | 14 |
| 4 | <1 | 25 | <1 | 17 |
| 5 | <1 | 13 | <1 | 10 |
| 6 | <1 | 10 | <1 | 11 |
Vertical displacement of the abutment
S1 (cone angle, 12°) showed a median deviation of 3 μm (3 μm, 5 μm) with a maximum range of 39 μm. S2 (cone angle, 15°) and S3 (cone angle, 5.7°) showed a similar median vertical displacement with S2, 2 μm (2, 3 μm) and S3, 2 μm (1, 3 μm). Also, the maximum range of vertical displacement was similar: S2, 16 μm and S3, 18 μm. S4 (cone angle, 7.5°) displayed a median vertical deviation of 4 μm (3, 5 μm) with a maximum range of 41 μm. The vertical deviation of the abutment depended on the implant system (P = 0.001) (Table 3). The values for S1 vs. S4 and S2 vs. S3 comparing the extent of the vertical deviation did not differ significantly (S1 vs. S4, 0.476; S2 vs. S3, P = 0.886). Significant differences were observed for S1 vs. S2 (P = 0.002), S1 vs. S3 (P = 0.001), S2 vs. S4 (P < 0.001), and S3 vs. S4 (P < 0.001). The outcome differed significantly between Pe1 and Pe2 (P < 0.001).
Canting moments of the abutment
The median changes in position were 0.09° (0.04°, 0.18°) for S1, 0.05° (0.03°, 0.08°) for S2, 0.02° (0.01°, 0.11°) for S3, and 0.05° (0.04°, 0.05°) for S4. The maximum range of canting moments was 1.20° (S1), 0.46° (S2), 0.79° (S3), and 0.38° (S4). Position stability related to the canting of the abutment did not differ between the four systems (P = 0.167). Significant differences between the results of the two test persons were observed (P < 0.001).
Discussion
The results of the present study show that repositioning of the abutment in all the four implant systems with an internal conical implant–abutment connection varies.
The analytical maximum rotational freedom based on equal clearance values (manufacturing tolerance) varies (1.7°–2.6°) in the cam–groove group (S2–S4); this is due to the geometric variation of R and δ. Cam–groove butt joint connections with a greater R show less rotational freedom [15]. This can be related to the limited sizing inside the implant when the index is placed more apical in conical connections in contrast to the sizing of the index in butt joint connections. As described previously, polygonal antirotational indices show higher rotational freedom than cam–groove connections due to the unfavorable features of their geometric design.
When analyzing the experimental rotational displacement of the abutment, significant differences between the implant systems were observed: The measured values of the Conelog system were significantly different to all other systems tested whereas Nobel Active, Bone Level, and Ankylos C/X showed similar values. Comparing the results to the outcome of a previous experimental study, the maximum rotational displacement of Nobel Active (hexagon) in the experiment is higher than the results for polygonal indices [16] and hexagonal indices in other studies [12, 13, 23]. Internal hexagonal indices such as Nobel Active show less rotational position stability than external indices again due to their smaller sizing (radius of index from rotational axis) [12, 16]. The investigated cam–groove connection designs show an increased rotational displacement in comparison to the Camlog system of the previous study [16] with Bone Level and Ankylos C/X clearly deviating.
In 1996, Binon declared that a possible rotational movement of the abutment of less than 5° assures screw joint stability of the implant–abutment complex in systems with an external hexagonal connection [11]. Further guidelines were not found. The Conelog system meets this standard; the Bone Level system barely meets this requirement. The two other implant systems (Nobel Active and Ankylos C/X) showed higher rotation values. Whether these findings compromise the stability of the conical screw joint needs to be determined; they definitely influence the fit of the superstructure [6], and a passive fit cannot be achieved.
The analytical approach of the present study aimed to show the rotational freedom of different geometric designs under idealized conditions, while the experimental part shows the possible reproducibility of the abutment position after physical repositioning. The experimental rotational freedom of the implant systems does not reflect the possible rotational freedom from the left to the right horizontal stop; if this was simulated, it would probably lead to higher rotational values. Shape irregularities (e.g., flattening of the vertices in polygons) may also influence the outcome. Manufacturing tolerances during fabrication of the implant components have a major influence on the rotational freedom in all index designs [14, 15]. Relating the theoretical findings to the experimental results shows that the rotational freedom of Nobel Active, Bone Level, and Ankylos C/X is approximately twice as large as calculated by the analytical approach. This suggests high manufacturing tolerances irrespective of the geometric design of the index. For the Conelog system, high-precision manufacturing can be assumed as the theoretical and experimental results were similar.
Canting moments of the abutment were not different between the four implant systems. They were of minimal extent as observed in the previous study [16].
Investigating the vertical displacement of the abutment after multiple repositioning and hand tightening resulted in significant differences between the systems, with Nobel Active and Conelog showing a different behavior from Bone Level and Ankylos C/X. Although the median values were similar, the maximum range of values clearly deviated. Nobel Active and Conelog displayed a higher vertical displacement of the abutment comparable to the systems with a conical connection design (Straumann Tissue Level and Astra Tech) from a former study [15]. For Bone Level and Ankylos C/X, a reduced vertical displacement of the abutment was observed. Still, their extent of vertical displacement is higher than in butt joint connections [16, 24, 25]. A vertical displacement is natural in conical connections and essential for a friction fit. The vertical position of the abutment is not only influenced by the cone angle, as the systems with the most acute (Ankylos C/X) and most obtuse (Bone Level) angle show comparable results. Other factors including the manufacturing tolerances (Semper et al., unpublished observation) and the torque value applied [21] may be of importance for the present results. The present approach is based on hand tightening of the screw, as suggested by the manufacturers until definitive seating of the abutment. Investigations showed that there is a wide variability of torque values when the abutment screw is manually tightened [26, 27]. Achieving predictable and repeatable torque values using hand tightening seems to be impossible. Therefore, the vertical position of the abutment in conical implant–abutment connections can vary between repeated screw tightening. Further studies should be performed using a torque wrench to investigate the final positioning of the abutment.
Conclusion
Malpositioning of the abutment was possible in all systems with a conical implant–abutment connection tested. The experimental rotational freedom and the vertical displacement of the abutment differed between the implant systems. In three implant systems, the theoretical rotational freedom clearly deviated from the experimental results suggesting high manufacturing tolerances diminishing position stability of the abutment.
Acknowledgments
The authors thank Dipl.-Ing. E. Trostmann and Dipl.-Math. G. Siebert. The present study was funded by the Camlog Foundation and Institut Straumann AG.
Conflict of interest
K. Nelson is a consultant to Camlog Biotechnologies AG.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1.Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- 2.Bozini T, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5years. Int J Oral Maxillofac Implants. 2011;26:304–318. [PubMed] [Google Scholar]
- 3.Davis DM, Packer ME, Watson RM. Maintenance requirements of implant-supported fixed prostheses opposed by implant-supported fixed prostheses, natural teeth, or complete dentures: a 5-year retrospective study. Int J Prosthodont. 2003;16:521–523. [PubMed] [Google Scholar]
- 4.Nedir R, Bischof M, Szmukler-Moncler S, Belser UC, Samson J. Prosthetic complications with dental implants: from an up-to-8-year experience in private practice. Int J Oral Maxillofac Implants. 2006;21:919–928. [PubMed] [Google Scholar]
- 5.Stimmelmayr M, Erdelt K, Güth JF, Happe A, Beuer F (2011) Evaluation of impression accuracy for a four-implant mandibular model—a digital approach. Clin Oral Investig Oct 19. doi:10.1007/s00784-011-0622-z [DOI] [PubMed]
- 6.Semper W, Kraft S, Mehrhof J, Nelson K. Impact of abutment rotation and angulation on marginal fit: theoretical considerations. Int J Oral Maxillofac Implants. 2010;25:752–758. [PubMed] [Google Scholar]
- 7.Barbosa GA, das Neves FD, de Mattos Mda G, Rodrigues RC, Ribeiro RF. Implant/abutment vertical misfit of one-piece cast frameworks made with different materials. Braz Dent J. 2010;21:515–519. doi: 10.1590/S0103-64402010000600006. [DOI] [PubMed] [Google Scholar]
- 8.Theoharidou A, Petridis HP, Tzannas K, Garefis P. Abutment screw loosening in single-implant restorations: a systematic review. Int J Oral Maxillofac Implants. 2008;23:681–690. [PubMed] [Google Scholar]
- 9.Gallucci GO, Bernard JP, Belser UC. Treatment of completely edentulous patients with fixed implant-supported restorations: three consecutive cases of simultaneous immediate loading in both maxilla and mandible. Int J Periodontics Restorative Dent. 2005;25:27–37. [PubMed] [Google Scholar]
- 10.Nelson K, Hildebrand D, Mehrhof J. Fabrication of a fixed retrievable implant-supported prosthesis based on electroforming: a technical report. J Prosthodont. 2008;17:591–595. doi: 10.1111/j.1532-849X.2008.00345.x. [DOI] [PubMed] [Google Scholar]
- 11.Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996;9:149–160. [PubMed] [Google Scholar]
- 12.de Barros Carrilho GP, Dias RP, Elias CN. Comparison of external and internal hex implants' rotational freedom: a pilot study. Int J Prosthodont. 2005;18:165–166. [PubMed] [Google Scholar]
- 13.Vigolo P, Fonzi F, Majzoub Z, Cordioli G. An in vitro evaluation of titanium, zirconia, and alumina procera abutments with hexagonal connection. Int J Oral Maxillofac Implants. 2006;21:575–580. [PubMed] [Google Scholar]
- 14.Semper W, Kraft S, Krüger T, Nelson K. Theoretical considerations: implant positional index design. J Dent Res. 2009;88:725–730. doi: 10.1177/0022034509341172. [DOI] [PubMed] [Google Scholar]
- 15.Semper W, Kraft S, Krüger T, Nelson K. Theoretical optimum of implant positional index design. J Dent Res. 2009;88:731–735. doi: 10.1177/0022034509341243. [DOI] [PubMed] [Google Scholar]
- 16.Semper W, Heberer S, Mehrhof J, Schink T, Nelson K. Effects of repeated manual disassembly and reassembly on the positional stability of various implant-abutment complexes: an experimental study. Int J Oral Maxillofac Implants. 2010;25:86–94. [PubMed] [Google Scholar]
- 17.Sutter F, Weber HP, Sorensen J, Belser U. The new restorative concept of the ITI Dental Implant System: design and engineering. Int J Periodontics Restorative Dent. 1993;13:409–431. [Google Scholar]
- 18.Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000;15:519–526. [PubMed] [Google Scholar]
- 19.Harder S, Dimaczek B, Açil Y, Terheyden H, Freitag-Wolf S, Kern M. Molecular leakage at implant-abutment connection—in vitro investigation of tightness of internal conical implant-abutment connections against endotoxin penetration. Clin Oral Investig. 2010;14:427–32. doi: 10.1007/s00784-009-0317-x. [DOI] [PubMed] [Google Scholar]
- 20.Harder S, Quabius ES, Ossenkop L, Kern M (2011) Assessment of lipopolysaccharide microleakage at conical implant-abutment connections. Clin Oral Investig Dec 2. doi:10.1007/s00784-011-0646-4 [DOI] [PubMed]
- 21.Dailey B, Jordan L, Blind O, Tavernier B. Axial displacement of abutments into implants and implant replicas, with the tapered cone-screw internal connection, as a function of tightening torque. Int J Oral Maxillofac Implants. 2009;24:251–256. [PubMed] [Google Scholar]
- 22.Brunner E, Domhof S, Langer F. Nonparametric analysis of longitudinal data in factorial experiments. New York: Wiley; 2002. [Google Scholar]
- 23.Lang LA, Wang RF, May KB. The influence of abutment screw tightening on screw joint configuration. J Prosthet Dent. 2002;87:74–79. doi: 10.1067/mpr.2002.121488. [DOI] [PubMed] [Google Scholar]
- 24.Jansen VK, Conrads G, Richter EJ. Microbial leakage and marginal fit of the implant-abutment interface. Int J Oral Maxillofac Implants. 1997;12:527–540. [PubMed] [Google Scholar]
- 25.Tsuge T, Hagiwara Y, Matsumura H. Marginal fit and microgaps of implant-abutment interface with internal anti-rotation configuration. Dent Mater J. 2008;27:29–34. doi: 10.4012/dmj.27.29. [DOI] [PubMed] [Google Scholar]
- 26.Goheen KL, Vermilyea SG, Vossoughi J, Agar JR. Torque generated by handheld screwdrivers and mechanical torquing devices for osseointegrated implants. Int J Oral Maxillofac Implants. 1994;9:149–155. [PubMed] [Google Scholar]
- 27.Hill EE, Phillips SM, Breeding LC. Implant abutment screw torque generated by general dentists using a hand driver in a limited access space simulating the mouth. J Oral Implantol. 2007;33:277–279. doi: 10.1563/1548-1336(2007)33[277:IASTGB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]


