Abstract
AIM: To evaluate the effectiveness of a short-type single-balloon-enteroscope (SBE) for endoscopic retrograde cholangiopancreatography (ERCP) in patients with a reconstructed intestine.
METHODS: Short-type SBE was developed to perform ERCP in postoperative patients with a reconstructed intestine. Short-type SBE is a direct-viewing endoscope with the following specifications: working length, 1520 mm; total length, 1840 mm; channel diameter, 3.2 mm. In addition, short-type SBE has a water-jet channel. The study group comprised 22 patients who underwent 31 sessions of short-type SBE-assisted ERCP from June 2011 through May 2012. Reconstruction was performed by Billroth-II (B-II) gastrectomy in 6 patients (8 sessions), Roux-en-Y (R-Y) gastrectomy in 14 patients (21 sessions), and R-Y hepaticojejunostomy in 2 patients (2 sessions). We retrospectively studied the rate of reaching the blind end (papilla of Vater or choledochojejunal anastomosis), mean time required to reach the blind end, diagnostic success rate (defined as the rate of successfully imaging the bile and pancreatic ducts), therapeutic success rate (defined as the rate of successfully completing endoscopic treatment), mean procedure time, and complications.
RESULTS: Among the 31 sessions of ERCP, the rate of reaching the blind end was 88% in B-II gastrectomy, 91% in R-Y gastrectomy, and 100% in R-Y hepaticojejunostomy. The mean time required to reach the papilla was 18.3 min in B-II gastrectomy, 21.1 min in R-Y gastrectomy, and 32.5 min in R-Y hepaticojejunostomy. The diagnostic success rates in all patients and those with an intact papilla were respectively 86% and 86% in B-II gastrectomy, 90% and 87% in R-Y gastrectomy, and 100% in R-Y hepaticojejunostomy. The therapeutic success rates in all patients and those with an intact papilla were respectively 100% and 100% in B-II gastrectomy, 94% and 92% in R-Y gastrectomy, and 100% in R-Y hepaticojejunostomy. Because the channel diameter was 3.2 mm, stone extraction could be performed with a wire-guided basket in 12 sessions, and wire-guided intraductal ultrasonography could be performed in 8 sessions. As for complications, hyperamylasemia (defined as a rise in serum amylase levels to more than 3 times the upper limit of normal) occurred in 1 patient (7 sessions) with a B-II gastrectomy and 4 patients (19 sessions) with an R-Y gastrectomy. After ERCP in patients with an R-Y gastrectomy, 2 patients (19 sessions) had pancreatitis, 1 patient (21 sessions) had gastrointestinal perforation, and 1 patient (19 sessions) had papillary bleeding. Pancreatitis and bleeding were both mild. Gastrointestinal perforation improved after conservative treatment.
CONCLUSION: Short-type SBE is effective for ERCP in patients with a reconstructed intestine and allows most conventional ERCP devices to be used.
Keywords: Endoscopic retrograde cholangiopancreatography, Single-balloon-enteroscope, Short type, Billroth-II gastrectomy, Roux-en-Y gastrectomy
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is often difficult to perform in postoperative patients with a reconstructed intestine because of altered anatomical features. However, the advent of balloon enteroscopy has improved the outcome of ERCP in patients with a reconstructed intestine, and many recent studies have found this procedure to be useful[1-20]. However, during ERCP, several problems remain to be solved. For example, these scopes do not have a lifting device, and the narrow channel diameter precludes the use of wire-guided devices. Moreover, the development of special devices is required because a single balloon enteroscope (SBE) has a long working length. Therefore, the development of a balloon endoscope with a short working length and a large working channel is eagerly anticipated[9]. The development of short-type double balloon enteroscopy (DBE) (models EC-450B15 and EI-530B, Fujifilm, Osaka, Japan) allowed many ERCP devices to be used. However, because the channel diameter of most conventional balloon enteroscopy is 2.8 mm, wire-guided devices cannot be used. We describe our experience with 22 postoperative patients with a reconstructed intestine who underwent ERCP (31 sessions) using a short-type SBE that was specifically developed for ERCP (model SIF-Y0004; Olympus Medical Systems, Tokyo, Japan). To the best of our knowledge, this is the first report to describe ERCP performed with this SBE.
MATERIALS AND METHODS
Patients
From June 2011 to May 2012, 37 sessions of short-type SBE-assisted ERCP were performed in 28 postoperative patients who had a reconstructed intestine in our hospital. Six patients were excluded from the study because the passage of the scope to the blind end (papilla of Vater or choledochojejunal anastomosis) was precluded by proximal narrowing or occlusion of the intestine caused by tumor invasion. The remaining 22 patients (31 sessions) were studied. Reconstruction was performed by Billroth II (B-II) gastrectomy in six patients (eight sessions), Roux-en-Y (R-Y) gastrectomy in 14 (21 sessions), and R-Y hepaticojejunostomy in two (two sessions). B-II gastrectomy was performed only in patients with a long afferent loop or Braun’s anastomosis in whom a direct-viewing multipurpose endoscope could not reach the blind end. Table 1 shows the detailed demographic characteristics of the patients.
Table 1.
Baseline characteristics of the patients n (%)
| Billroth-II gastrectomy | Roux-en-Y gastrectomy | Roux-en-Y hepatico-jejunostomy | Total No. of SIF-Y0004-assisted ERCP | |
| (n = 8) | (n = 21) | (n = 2) | (n = 31) | |
| Age1, mean (range), yr | 75.4 (62-82) | 71.3 (50-85) | 65 (65) | 72.0 (50-85) |
| Sex2: | ||||
| Male | 5 (83) | 13 (93) | 2 (100) | 20 (91) |
| Female | 1 (17) | 1 (7) | 0 (0) | 2 (9) |
| Reasons for surgery1 | ||||
| Gastric ulcer | 2 (25) | 0 (0) | 0 (0) | 2 (6.5) |
| Duodenum ulcer | 2 (25) | 2 (9.5) | 0 (0) | 4 (13) |
| Carcinoma of the stomach | 4 (50) | 19 (90.5) | 0 (0) | 23 (74) |
| Carcinoma of the pancreas | 0 (0) | 0 (0) | 2 (100) | 2 (6.5) |
| Reasons for ERCP1 | ||||
| AOSC (due to CBD stone) | 1 (12.5) | 1 (5) | 0 (0) | 2 (6.5) |
| Carcinoma of the pancreas | 2 (25) | 0 (0) | 0 (0) | 2 (6.5) |
| Carcinoma of the gallbladder | 1 (12.5) | 0 (0) | 0 (0) | 1 (3.3) |
| CBD stone | 3 (37.5) | 14 (66) | 2 (100) | 19 (61) |
| IPMN | 0 (0) | 1 (5) | 0 (0) | 1 (3.3) |
| IPNB suspected | 0 (0) | 1 (5) | 0 (0) | 1 (3.3) |
| Metastasis of L/N in porta hepatis | 1 (12.5) | 4 (19) | 0 (0) | 5 (16) |
No. of procedures;
No. of patients. AOSC: Acute obstructive suppurative cholangitis; CBD: Common bile duct; IPMN: Intraductal papillary mucinous neoplasm; IPNB: Intraductal papillary neoplasm of the bile duct; ERCP: Endoscopic retrograde cholangiopancreatography.
Endoscope and ERCP Instruments
The SIF-Y0004 is a direct-viewing endoscope with the following specifications: angle of view, 120°; bending section, up 180°, down 180°, right 160°, and left 160°; working length, 1520 mm; total length, 1840 mm; outer diameter of distal end, 9.2 mm; outer diameter of insertion end, 9.2 mm; and working channel diameter, 3.2 mm. The SIF-Y0004 has a water-jet channel.
A sliding tube with a working length of 880 mm was used. The specifications of the SIF-Y0004 are compared with those of a conventional SBE (SIF-Q260; Olympus Medical Systems, Tokyo, Japan) in Table 2 and Figure 1.
Table 2.
Specifications of two types of single-balloon endoscopes
| SIF-Y0004 | SIF-Q260 | |
| Direction of view | Forward viewing | Forward viewing |
| Angle of view | 120° | 140° |
| Outer diameter (mm) | ||
| Distal end | 9.2 | 9.2 |
| Insertion end | 9.2 | 9.2 |
| Bending section | ||
| Up/down | 180°/180° | 180°/180° |
| Right/left | 160°/160° | 160°/160° |
| Working length (mm) | 1520 | 2000 |
| Total length (mm) | 1840 | 2345 |
| Working channel diameter (mm) | 3.2 | 2.8 |
| Water-jet channel | Yes | No |
Figure 1.
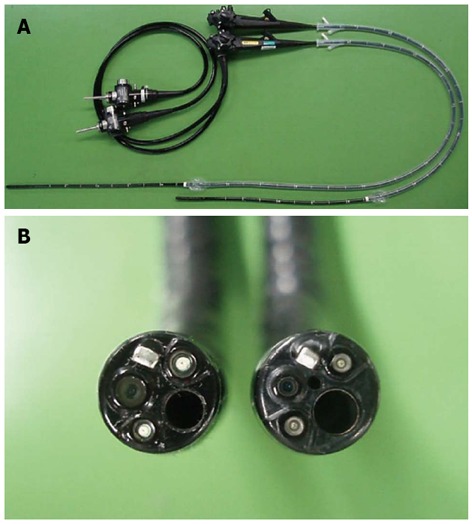
Comparison of two types of single-balloon endoscopes. A: Comparison of working lengths of two types of single balloon endoscopes (SBEs). Left: SIF-Q260 (working length 2000 mm); Right: SIF-Y0004 (working length 1520 mm); B: Comparison of working channel diameters of two types of SBE. Left: SIF-Q260 (working channel diameter 2.8 mm); Right: SIF-Y0004 (working channel diameter 3.2 mm and water-jet channel).
For biliary cannulation and injection of contrast media, a conventional ERCP catheter (PR-4Q-1; Olympus Medical Systems, Tokyo, Japan) and a bending cannula (PR-233Q; Olympus Medical Systems) were used. If cannulation was difficult to perform with a catheter alone, a 0.035-inch guide wire (RF-GA35403; Radifocus®, Terumo Corporation, Tokyo, Japan) was used. For stent placement and insertion of guide-wire instruments, a 0.035-inch JagwireTM (Boston Scientific; Natick, MA, United States) and a 0.025-inch disposable VisiglideTM guide wire (G-240-2545A, Olympus Medical Systems, Japan) were mainly used.
Endoscopic papillary balloon dilation was done using a Quantum TTC® Biliary Balloon Dilator (QBD-8X3, Cook Medical, Bloomington, IN, United States) and a CRETM Balloon Dilation Catheter (Boston Scientific), measuring 10 to 15 mm, was used to perform endoscopic papillary large balloon dilation. Lithotripsy was performed with the following retrieval baskets: models FG-V435P (Flower Basket V®, Olympus Medical Systems), FG-V436P (Tetra Catch V®, Olympus Medical Systems), and EBL-15-200 (Escort II Extraction Balloon, Cook Medical).
Intraductal ultrasonography was carried out with a miniature ultrasound probe (UM-G20-29R, Olympus Medical Systems), inserted using a guide wire. As for stents, a 7-French pigtail plastic stent (PBD-203 series, Olympus Medical Systems) and metallic WallFlexTM Biliary RX Fully Covered and RX Partially Covered Stents Systems (Boston Scientific) were used.
Methods
Many studies have reported that balloon enteroscopy-assisted ERCP is therapeutically useful; however, a system for this procedure is not commercially available. We explained to patients that treatment outcomes and the incidence of complications have not been reported, and received written informed consent from all patients. Patients were sedated with pethidine (50 mg) and midazolam (3 to 10 mg), and vital signs were intermittently monitored during all procedures. Propofol was used if necessary. The same operator performed all examinations from the time of endoscope insertion to treatment. The endoscope was inserted with the patient in the prone position, and abdominal compression was applied manually if a scope was technically difficult to insert deeply. Butylscopolamine (20 to 40 mg) or glucagon (1 to 2 mg) was administered as an antispasmodic. Three very experienced endoscopists (with experience in > 1200 sessions of ERCP) conducted the examinations. After ERCP, all patients received nafamostat mesilate (10 mg) to prevent pancreatitis, with the exception of those in whom the drug was contraindicated because of allergies or other reasons.
We retrospectively studied the rate of reaching the blind end, time required to reach the papilla, diagnostic success rate, therapeutic success rate, procedure time, and complications according to the reconstruction method. The diagnostic success rate was defined as the rate of successfully imaging of the bile and pancreatic ducts. The therapeutic success rate was defined as the rate of successfully completing the endoscopic treatment. The procedure time was defined as the interval from the start of cannulation to removal of the endoscope. Pancreatitis and bleeding occurring after ERCP were evaluated according to the 1991 Consensus Guidelines (Cotton Classification)[21]. Hyperamylasemia was defined as a rise in serum amylase levels to more than three times the upper limit of normal. In our hospital, we routinely measure serum amylase 3 h after the completion of ERCP, as well as the next morning. In patients in whom the blind end was not reached, SBE-assisted ERCP was not attempted a second time, except if the patient strongly requested to undergo the procedure again. If SBE-assisted ERCP was unsuccessful, open surgery or percutaneous cholangioscopy was performed.
RESULTS
Rate of reaching the blind end (papilla of Vater or choledochojejunal anastomosis)
The rate of reaching the blind end was 88% (7/8) in patients with a B-II gastrectomy, 91% (19/21) in those with a R-Y gastrectomy, and 100% (2/2) in those with a R-Y hepaticojejunostomy (Table 3).
Table 3.
Summary of results n (%)
| Billroth-II gastrectomy (n = 8) | Roux-en-Y gastrectomy (n = 21) | Roux-en-Y Hepatico-jejunostomy (n = 2) | Total No. of SIF-Y0004-assisted ERCP (n = 31) | |
| Reaching the blind end | 7 (88) | 19 (91) | 2 (100) | 28 (90) |
| Mean time (min) to reach the blind end (range) | 18.3 (5-37) | 21.1 (10-37) | 32.5 (32-33) | 21.2 (5-37) |
| Diagnostic success | ||||
| Total | 6 (86) | 17 (90) | 2 (100) | 25 (89) |
| Intact papilla | 6 (86) | 13 (87) | - | 19 (86) |
| Therapeutic intervention required | ||||
| Total | 5 (83) | 16 (94) | 2 (100) | 23 (92) |
| Intact papilla | 5 (83) | 12 (92) | - | 17 (89) |
| Therapeutic success | ||||
| Total | 5 (100) | 15 (94) | 2 (100) | 22 (96) |
| Intact papilla | 5 (100) | 11 (92) | - | 16 (94) |
| Mean procedure time (min) (range) | 35.4 (7-65) | 43.3 (12-125) | 46.5 (26-41) | 40.2 (7-125) |
ERCP: Endoscopic retrograde cholangiopancreatography.
Mean time required to reach the blind end
The mean time required to reach the blind end was 18.3 min (range, 5 to 37 min) in B-II gastrectomy, 21.1 min (range, 10 to 37 min) in R-Y gastrectomy, and 32.5 min (range, 32 to 33 min) in R-Y hepaticojejunostomy (Table 3).
Diagnostic success rates
The diagnostic success rate was 86% (6/7) in B-II gastrectomy, 90% (17/19) in R-Y gastrectomy, and 100% (2/2) in R-Y hepaticojejunostomy. All the patients with a B-II gastrectomy and 15 (80%) of the 19 patients with an R-Y gastrectomy had an intact papilla. The diagnostic success rate among patients with an intact papilla was 86% (6/7) in B-II gastrectomy and 87% (13/15) in R-Y gastrectomy (Table 3).
Therapeutic success rate
The therapeutic success rate was 100% (5/5) in B-II gastrectomy, 94% (15/16) in R-Y gastrectomy, and 100% (2/2) in R-Y hepaticojejunostomy. Among patients with an intact papilla, the therapeutic success rate was 100% (5/5) in B-II gastrectomy and 92% (11/12) in R-Y gastrectomy (Table 3).
Treatment procedures
The channel diameter of 3.2 mm allowed 12 sessions of stone extraction with a wire-guided basket, and eight sessions of wire-guided intraductal ultrasonography to be performed (Figures 2, 3). Residual stones could thus be confirmed, and biliary strictures evaluated. All treatment procedures are summarized in Table 4.
Figure 2.
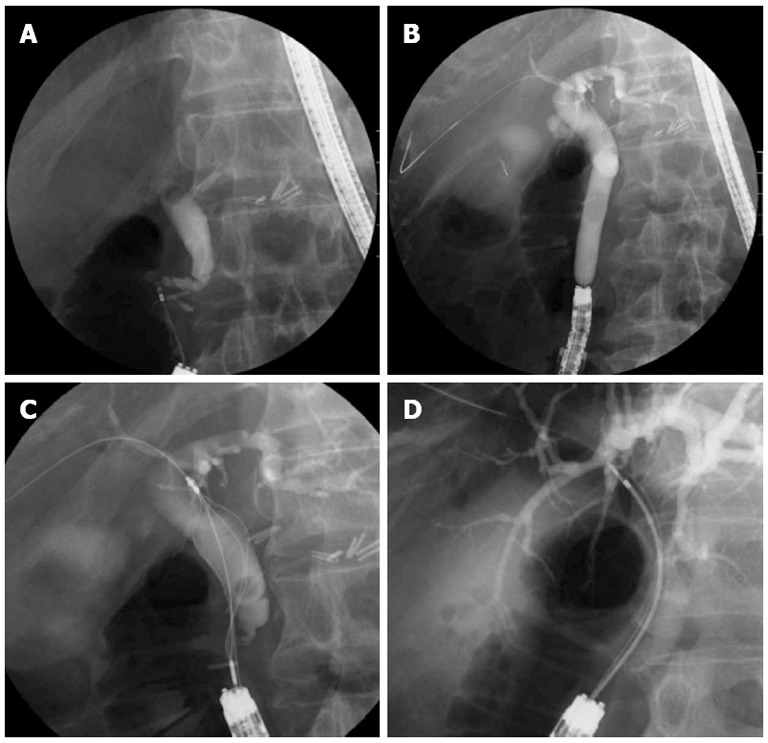
Therapeutic intervention. A: Cholangiogram showing a bile duct stone; B: Radiographic image showing papillary dilation using a large balloon catheter; C: Radiographic image showing wire-guided 4-wire retrieval basket; D: Radiographic image showing wire-guided intraductal ultrasonography.
Figure 3.
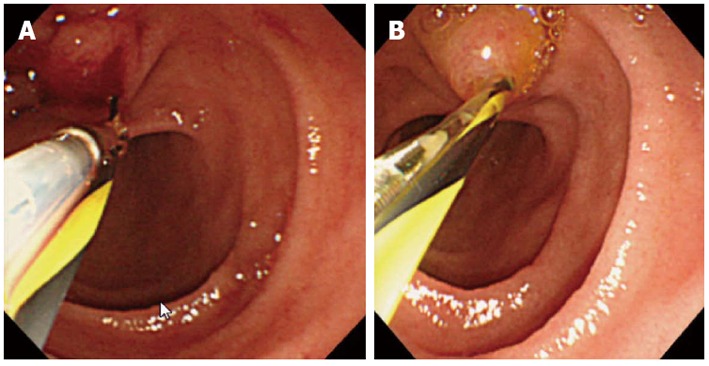
Wire-guided devices. A: A wire-guided 4-wire retrieval basket was inserted; B: A wire-guided intraductal ultrasonography was inserted.
Table 4.
Treatment procedures
| Billroth-II gastrectomy | Roux-en-Y gastrectomy | Roux-en-Y Hepatico-jejunostomy | Total No. of SIF-Y0004-assisted ERCP | |
| EST | 0 | 3 | 0 | 3 |
| EPBD | 2 | 5 | 0 | 7 |
| EPLBD | 1 | 4 | 1 | 6 |
| EBD | ||||
| Plastic stent | 1 | 3 | 0 | 4 |
| Metallic stent | 2 | 2 | 0 | 4 |
| Stone extraction | ||||
| Wire-guided basket | 1 | 9 | 2 | 12 |
| Balloon catheter | 0 | 1 | 0 | 1 |
| Wire-guided IDUS | 1 | 7 | 0 | 8 |
EBD: Endoscopic biliary drainage; EPBD: Endoscopic papillary balloon dilation; EPLBD: Endoscopic papillary large balloon dilation; EST: Endoscopic sphincterotomy; IDUS: Intraductal ultrasonography; ERCP: Endoscopic retrograde cholangiopancreatography.
Mean procedure time
The mean procedure time was 35.4 min (range, 7 to 65 min) in B-II gastrectomy, 43.3 minutes (range, 12 to 125 min) in R-Y gastrectomy, and 29.5 min (range, 26 to 33 min) in R-Y hepaticojejunostomy (Table 3).
Complications
Hyperamylasemia, pancreatitis, and gastrointestinal perforation were the main complications encountered (Table 5) Pancreatitis and bleeding were both mild. Gastrointestinal perforation improved after conservative treatment.
Table 5.
Complications n (%)
| Complications | Billroth-II gastrectomy (n = 8) | Roux-en-Y gastrectomy (n = 21) | Roux-en-Y Hepatico-jejunostomy (n = 2) | Total No. of SIF-Y0004-assisted ERCP (n = 31) |
| Hyperamylasemia1 | ||||
| Total | 1 (14.3) | 4 (21.1) | - | 5 (19.2) |
| Intact papilla | 1 (14.3) | 3 (20) | - | 4 (18.2) |
| Pancreatitis2 | ||||
| Total | 0 (0) | 2 (10.5) | - | 2 (7.7) |
| Intact papilla | 0 (0) | 2 (13.3) | - | 2 (9.1) |
| Perforation of digestive tract | 0 (0) | 1 (4.8) | 0 (0) | 1 (3.2) |
| Bleeding of papilla2 | 0 (0) | 1 (5.3) | 0 (0) | 1 (3.4) |
Hyperamylasemia: More than 3 times the upper limit of normal;
According to Cotton’s criteria. ERCP: Endoscopic retrograde cholangiopancreatography.
DISCUSSION
When performing ERCP in postoperative patients with a reconstructed intestine, whether the scope can reach the papilla or choledochojejunal anastomosis is an important concern. However, recent studies have reported that the blind end is reached in more than 80% of patients[3-5,9-15,17]. After reaching the blind end, imaging and treatment of the papilla or biliary anastomosis become the most important issues. In particular, the outcomes of ERCP in patients with an intact papilla differ substantially among hospitals and remain far from satisfactory. Shimatani et al[12] reported that the diagnostic success rate of DBE-assisted ERCP exceeded 90% in patients with an intact papilla, as compared with 25% to 80% in general[8,9,11]. In several small studies, the diagnostic success rate of SBE-assisted ERCP in patients with an intact papilla ranged from 25% to 80%[1,4,5]. In our study, the diagnostic success rate was 86%, indicating relatively good results. As for the relative advantages and disadvantages of SBE and DBE, May et al[22] reported that setting up a DBE system requires 15.2 min, whereas Kawamura et al[23] showed that an SBE system could be set up within 5 min because it is simpler. A DBE system requires two balloons; therefore, the technique is complex, and the balloon at the distal end may interfere with passage of the scope through the intestine. However, one study reported that a DBE is easier to pass through an intestine with sharp angles than an SBE[24].
Although several studies have compared SBE-assisted ERCP with DBE-assisted ERCP, and such a comparison would be challenging, these procedures are reported to be similarly clinically useful[1,11,18-20].
The SIF-Q260, a conventional SBE, has a working length of 2000 mm and a channel diameter of 2.8 mm. Therefore, most conventional ERCP devices cannot be used, and the types of devices that could be used are limited. A short-type DBE has a working length of 1520 mm and a channel diameter of 2.8 mm, making passage of devices through the forceps channel difficult. Itoi et al[3] replaced an SBE with a conventional forward-viewing endoscope after reaching the papilla. We have used this technique in several patients in our hospital. However, even if the papilla is reached, some patients have severe bowel adhesion associated with complex loops that are difficult to resolve. Replacement of the scope is therefore not necessarily successful.
In this study, we used an SIF-Y0004, a new enteroscope that was developed to perform ERCP in postoperative patients with a reconstructed intestine. This enteroscope has a working length of 1520 mm and a channel diameter of 3.2 mm, allowing most conventional ERCP devices to be employed. In our hospital, the use of the SIF-Y0004 permitted the delivery of 8.5-French or smaller devices. The SIF-Y0004 also allowed the use of wire-guided devices that could not be passed through enteroscopy with a 2.8 mm channel diameter, as well as the insertion of a 7-French stent after the placement of two guide wires. A decreased rate of reaching the blind end was an important concern, because the SIF-Y0004 has a shorter effective length than a conventional SBE. However, the rate of reaching the blind end in our study was 90%, which was similar to that of ERCP performed with a SIF-Q260 in our hospital (89%).
The SIF-Y0004 permitted the use of devices that could not be used with the SIF-Q260. Compared with a short-type DBE, more devices and diagnostic instruments could be used with SIF-Y0004. Conventional models have a channel diameter of 2.8 mm; therefore, ERCP for stone extraction requires free-hand cannulation and the use of a 4-wire retrieval basket. However, the SIF-Y0004 allowed wire-guided devices to be used for stone extraction; successfully accomplished in 12 patients in our study. In addition, this new SBE allowed wire-guided intraductal ultrasonography to be easily performed to confirm residual stones.
The incidence of complications after ERCP in patients with a reconstructed intestine has been reported to be 0% to 11% for perforation, 0% to 20% for pancreatitis, and 0% to 32% for bleeding, and differed considerably among hospitals[1-5,8,9,12-16]. Many patients who underwent ERCP in our hospital had undergone gastrectomy and had an intact papilla; therefore, cannulation was expected to be difficult, potentially leading to a high incidence of pancreatitis. However, the incidence of pancreatitis in this study was 7.7%, which is not particularly higher compared with previous reports. Further studies of larger numbers of patients are required because our study group was small.
The patient with gastrointestinal perforation had duodenal ulcer postoperatively and had undergone abdominal surgery three times. The initial procedure was Roux-en-Y reconstruction after distal gastrectomy, and a duodenum-transverse colon fistula developed. Subsequently, abdominal surgery was performed twice to repair the fistula site. Marked adhesion was found in the horizontal portion of the duodenum. Although a defect apparently caused by a stone in the bile duct was found on endoscopic retrograde cholangiography, the scope was retracted during the examination and did not reach the blind end. The scope was inserted several times, but the results were the same. Lithotripsy was therefore not performed, and the examination was terminated. After endoscopy, the patient had abdominal pain and increased amylase levels. Post-ERCP pancreatitis was suspected. Enhanced computed tomography showed a small amount of free air around the horizontal portion of the duodenum, and perforation was diagnosed. There were no symptoms of peritoneal irritation. Computed tomography performed 5 d after surgery showed disappearance of the free air. As for the common bile duct stones, there was no dilation of the bile duct, and a percutaneous approach was precluded. We therefore recommended open surgery. However, ERCP with the SIF-Y0004 was repeated after 10 d at the strong request of the patient. Lithotripsy was successfully performed without perforation.
In the patient with papillary bleeding, melena occurred 12 h after endoscopic papillary large balloon dilatation. The hemoglobin level decreased by 2 g/dL. Bleeding from the papilla was suspected, and endoscopic examination with the SIF-Y0004 showed blood clots at and around the papilla. There was no active bleeding from the papilla. The examination was completed without any treatment. Subsequently, there was no melena or progression of anemia. Hemostasis was achieved spontaneously, with no need for blood transfusion.
The present study was small. The SIF-Y0004 has a channel diameter of 3.2 mm, currently the largest available among balloon endoscopes, and a short working length. The water-jet channel of this model helps to maintain a field of view during scope insertion and treatment. It will be particularly useful in the presence of bleeding.
Further studies in larger numbers of patients are needed to confirm our results. However, in postoperative patients with a reconstructed intestine who underwent ERCP, the rate of the reaching the blind end with the SIF-Y0004 was similar to that with the SIF-Q260. This new model SBE permitted the use of most ERCP devices. Our results suggest that the SIF-Y0004 enables high-quality diagnosis and treatment to be provided reliably.
ACKNOWLEDGMENTS
The authors thank Olympus Medical Systems (Tokyo, Japan) for providing the prototype instruments used in the study.
COMMENTS
Background
Endoscopic retrograde cholangiopancreatography (ERCP) with duodenal scope or conventional forward viewing endoscope for reconstructed intestine (Billroth-II reconstruction, Roux-en-Y reconstruction) has often been described as unsatisfactory because of altered anatomical features. Balloon enteroscopy has improved the outcomes of ERCP in patients with a reconstructed intestine.
Research frontiers
Balloon enteroscopy has improved the outcomes of ERCP in patients with a reconstructed intestine. These patients may avoid the need for surgical treatment in case of biliopancreatic problems.
Innovations and breakthroughs
Balloon-enteroscope assisted-ERCP is an important endoscopic breakthrough for the therapeutic management of the conventionally inaccessible biliopancreatic ducts. However, several problems remain to be solved. For example, wire-guided devices cannot be used because these scopes have a narrow channel diameter, 2.8 mm. In this study, the authors used a newly designed short-type single balloon enteroscope (SBE) that was developed to perform ERCP in postoperative patients with a reconstructed intestine. This short-type SBE has a working length of 1520 mm, and a channel diameter of 3.2 mm, allowing most conventional ERCP devices to be employed. Among all balloon enteroscopy, these specifications are limited to this scope. As for treatment, this scope permitted the use of devices that could not be used with conventional SBE. Compared with a short-type double balloon enteroscopy, more devices and diagnostic instruments could be used with this scope. Conventional models have a channel diameter of 2.8 mm; therefore, ERCP for stone extraction requires free-hand cannulation. However, this scope allowed wire-guided devices to be used for stone extraction. In addition, this scope allowed wire-guided intraductal ultrasonography to be easily performed to confirm residual stones.
Applications
This study suggests that short-type SBE enables high-quality diagnosis and treatment to be provided reliably.
Terminology
Billroth-II reconstruction is a surgical technique in gastrectomy. Roux-en-Y reconstruction of the small intestine is a frequently performed surgical technique in gastrointestinal surgery, hepatobiliary and pancreatic surgery. The location of the Vater’s papilla and choledochojejunal anastomosis of the most patients who are underwent these operation are differed from normal position that was accessible with conventional endoscope.
Peer review
The authors investigated the efficacy of new short-type SBE for ERCP in patients with altered gastrointestinal anatomy, and concluded that short-type SBE is effective for ERCP in patients with a reconstructed intestine. This study clearly shows the efficacy of short-type SBE as a clinical trial.
Footnotes
Supported by A Prototype Single Balloon Enteroscope from Olympus Medical Systems, Tokyo, Japan
P- Reviewer Murata A S- Editor Song XX L- Editor Stewart GJ E- Editor Zhang DN
References
- 1.Neumann H, Fry LC, Meyer F, Malfertheiner P, Monkemuller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion. 2009;80:52–57. doi: 10.1159/000216351. [DOI] [PubMed] [Google Scholar]
- 2.Dellon ES, Kohn GP, Morgan DR, Grimm IS. Endoscopic retrograde cholangiopancreatography with single-balloon enteroscopy is feasible in patients with a prior Roux-en-Y anastomosis. Dig Dis Sci. 2009;54:1798–1803. doi: 10.1007/s10620-008-0538-x. [DOI] [PubMed] [Google Scholar]
- 3.Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video) Am J Gastroenterol. 2010;105:93–99. doi: 10.1038/ajg.2009.559. [DOI] [PubMed] [Google Scholar]
- 4.Saleem A, Baron TH, Gostout CJ, Topazian MD, Levy MJ, Petersen BT, Wong Kee Song LM. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy. 2010;42:656–660. doi: 10.1055/s-0030-1255557. [DOI] [PubMed] [Google Scholar]
- 5.Wang AY, Sauer BG, Behm BW, Ramanath M, Cox DG, Ellen KL, Shami VM, Kahaleh M. Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointest Endosc. 2010;71:641–649. doi: 10.1016/j.gie.2009.10.051. [DOI] [PubMed] [Google Scholar]
- 6.Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608–1610. doi: 10.1002/lt.20623. [DOI] [PubMed] [Google Scholar]
- 7.Moreels TG, Roth B, Vandervliet EJ, Parizel PM, Dutré J, Pelckmans PA. The use of the double-balloon enteroscope for endoscopic retrograde cholangiopancreatography and biliary stent placement after Roux-en-Y hepaticojejunostomy. Endoscopy. 2007;39 Suppl 1:E196–197. doi: 10.1055/s-2007-966410. [DOI] [PubMed] [Google Scholar]
- 8.Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038–1041. doi: 10.1016/j.gie.2007.06.056. [DOI] [PubMed] [Google Scholar]
- 9.Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068–1071. doi: 10.1055/s-2007-966841. [DOI] [PubMed] [Google Scholar]
- 10.Mönkemüller K, Bellutti M, Neumann H, Malfertheiner P. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc. 2008;67:992–996. doi: 10.1016/j.gie.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 11.Chu YC, Yang CC, Yeh YH, Chen CH, Yueh SK. Double-balloon enteroscopy application in biliary tract disease-its therapeutic and diagnostic functions. Gastrointest Endosc. 2008;68:585–591. doi: 10.1016/j.gie.2008.03.1083. [DOI] [PubMed] [Google Scholar]
- 12.Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849–854. doi: 10.1055/s-0029-1215108. [DOI] [PubMed] [Google Scholar]
- 13.Parlak E, Ciçek B, Dişibeyaz S, Cengiz C, Yurdakul M, Akdoğan M, Kiliç MZ, Saşmaz N, Cumhur T, Sahin B. Endoscopic retrograde cholangiography by double balloon enteroscopy in patients with Roux-en-Y hepaticojejunostomy. Surg Endosc. 2010;24:466–470. doi: 10.1007/s00464-009-0591-3. [DOI] [PubMed] [Google Scholar]
- 14.Iwamoto S, Ryozawa S, Yamamoto H, Taba K, Ishigaki N, Harano M, Iwano H, Sakaida I. Double balloon endoscope facilitates endoscopic retrograde cholangiopancreatography in roux-en-y anastomosis patients. Dig Endosc. 2010;22:64–68. doi: 10.1111/j.1443-1661.2009.00920.x. [DOI] [PubMed] [Google Scholar]
- 15.Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Fukuzawa K, Moriyasu F, et al. Long- and short-type double-balloon enteroscopy-assisted therapeutic ERCP for intact papilla in patients with a Roux-en-Y anastomosis. Surg Endosc. 2011;25:713–721. doi: 10.1007/s00464-010-1226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raithel M, Dormann H, Naegel A, Boxberger F, Hahn EG, Neurath MF, Maiss J. Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol. 2011;17:2302–2314. doi: 10.3748/wjg.v17.i18.2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho S, Kamalaporn P, Kandel G, Kortan P, Marcon N, May G. 'Short' double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol. 2011;25:615–619. doi: 10.1155/2011/354546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreels TG, Pelckmans PA. Comparison between double-balloon and single-balloon enteroscopy in therapeutic ERC after Roux-en-Y entero-enteric anastomosis. World J Gastrointest Endosc. 2010;2:314–317. doi: 10.4253/wjge.v2.i9.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mönkemüller K, Fry LC, Neumann H, Malfertheiner P. Single Balloon Enteroscopy (SBE) Versus Double Balloon (DBE) ERCP in Patients with Roux-en-Y Anastomosis. Gastrointest Endosc. 2009;69:AB139. doi: 10.1055/s-2007-966949. [DOI] [PubMed] [Google Scholar]
- 20.Shah RJ, Smolkin M, Ross AS, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, H Al-Lehibi A, Hardy A, Morgan DR, Sethi A, Stevens PD, Akerman PA, Thakkar SJ, Yen RD, Brauer BC. A Multi-Center, U.S. Experience of Single Balloon, Double Balloon, and Rotational Overtube Enteroscopy-Assisted ERCP in Long Limb Surgical Bypass Patients. Gastrointest Endosc. 2010;71:AB134–5. [Google Scholar]
- 21.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 22.May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc. 2005;62:62–70. doi: 10.1016/s0016-5107(05)01586-5. [DOI] [PubMed] [Google Scholar]
- 23.Kawamura T, Yasuda K, Tanaka K, Uno K, Ueda M, Sanada K, Nakajima M. Clinical evaluation of a newly developed single-balloon enteroscope. Gastrointest Endosc. 2008;68:1112–1116. doi: 10.1016/j.gie.2008.03.1063. [DOI] [PubMed] [Google Scholar]
- 24.Tsujikawa T, Saitoh Y, Andoh A, Imaeda H, Hata K, Minematsu H, Senoh K, Hayafuji K, Ogawa A, Nakahara T, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: preliminary experiences. Endoscopy. 2008;40:11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]


