Abstract
Background/Aims
Mini-probe endoscopic ultrasonography (mEUS) is a useful diagnostic tool for accurate assessment of tumor invasion. The aim of this study was to estimate the accuracy of mEUS in patients with early colorectal cancer (ECC).
Methods
Ninety lesions of ECC underwent mEUS for pre-treatment staging. We divided the lesions into either the mucosal group or the submucosal group according to the mEUS findings. The histological results of the specimens were compared with the mEUS findings.
Results
The overall accuracy for assessing the depth of tumor invasion (T stage) was 84.4% (76/90). The accuracy of mEUS was significantly lower for submucosal lesions compared to mucosal lesions (p=0.003) and it was lower for large tumors (≥2 cm) (p=0.034). The odds ratios of large tumors and submucosal tumors affecting the accuracy of T staging were 3.46 (95% confidence interval [CI], 1.05 to 11.39) and 6.25 (95% CI, 1.85 to 25.14), respectively. When submucosal tumors were combined with large size, the odds ratio was 14.67 (95% CI, 1.46 to 146.96).
Conclusions
The overall accuracy of T stage determination with mEUS was considerably high in patients with ECC; however, the accuracy decreased when tumor size was >2 cm or the tumor had invaded the submucosal layer.
Keywords: Colorectal neoplasms, Endosonography
INTRODUCTION
Colorectal cancer is one of the most common malignancies worldwide. Current studies have shown that colorectal cancer is on the rise, especially in Africa and Asia, including Korea.1-3 One possible explanation for this current trend may be the increased use of colonoscopy. The early diagnosis of colorectal cancer is feasible and various treatment methods have been developed. Multiple treatment options are available to patients with early colorectal cancer (ECC), including radical or laparoscopic surgery, transanal endoscopic microsurgery, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD).4 Endoscopic treatment for ECC is considered appropriate only when the invasion of the submucosal layer is <1,000 µm.5 Therefore, accurate assessment of tumor invasion (T stage) is essential when making therapeutic decisions regarding patients with ECC.
Endoscopic ultrasonography (EUS) is one of the most reliable assessment techniques in the preoperative assessment of T stage of gastrointestinal tract cancer. EUS is better than magnifying colonoscopy and is comparable to narrow-band imaging with magnification in determining tumor invasion of ECC.6-10 The pooled sensitivity and specificity in a meta-analysis of the use of EUS in determining T1 stage rectal cancer were 87.8% and 98.3%, respectively, and the accuracy of EUS for the T1 stage was lower than that for the advanced T stages (T3 or T4).11 However, maneuvering in the proximal part of the colon is difficult in conventional EUS.
The mini-probe EUS (mEUS) can be easily introduced through the biopsy channel of the endoscope and this technique has many benefits compared to conventional EUS.4 However, the accuracy of mEUS in identifying the T1 stage of colorectal cancer is variable, ranging from 67% to 100%.9,10,12 In addition, studies which focus solely on the accuracy of diagnosis of submucosal lesions are limited. Therefore, we investigated the performance of mEUS in T1 staging of mucosal and submucosal lesions. In addition, we estimated the factors that influence the accuracy in diagnosing the T1 stage of ECC.
MATERIALS AND METHODS
1. Materials
A mEUS was performed on 90 lesions in 86 patients with suspected T1 stage colorectal cancer at the Inje University Seoul Paik Hospital between March 2003 and June 2010. Among 86 patients, 82 had a single lesion and four patients had two lesions, making up a total of 90 lesions. The patients consisted of 62 men (72.1%) and 24 women (27.9%) with a mean age of 62.7 years (range, 35 to 85 years). The tumors were primarily located in the rectum (39/90, 43.3%) and sigmoid colon (30/90, 33.3%). Patients who were diagnosed with adenocarcinoma on histology were included in the study. The usefulness of mEUS in ECC treatment plans was investigated through a retrospective review of patients' medical records. The Institutional Review Board of Inje University Seoul Paik Hospital approved this study.
2. Methods
1) mEUS technique
All examinations were conducted using a 20 MHz mini-probe with a diameter of 6F (Olympus UM-3R-3; Olympus, Tokyo, Japan). Two specialists performed the procedures and one specialist reviewed all the mEUS findings retrospectively. All patients underwent examinations in a conventional manner. Colonic preparation was performed with 2 to 4 L of hypertonic polyethylene glycol before the examination. A sedative agent was used (midazolam; 3 to 5 mg intravenously) when requested by the patient. After a lesion was diagnosed via colonoscopy (Olympus CF-Q260; Olympus), mEUS was performed to identify the depth of invasion. Acoustic coupling with the colonic wall was obtained by instilling deaerated water in the colonic lumen. Based on the mEUS results, the patient underwent endoscopic or surgical resection.
2) Staging of colorectal cancer
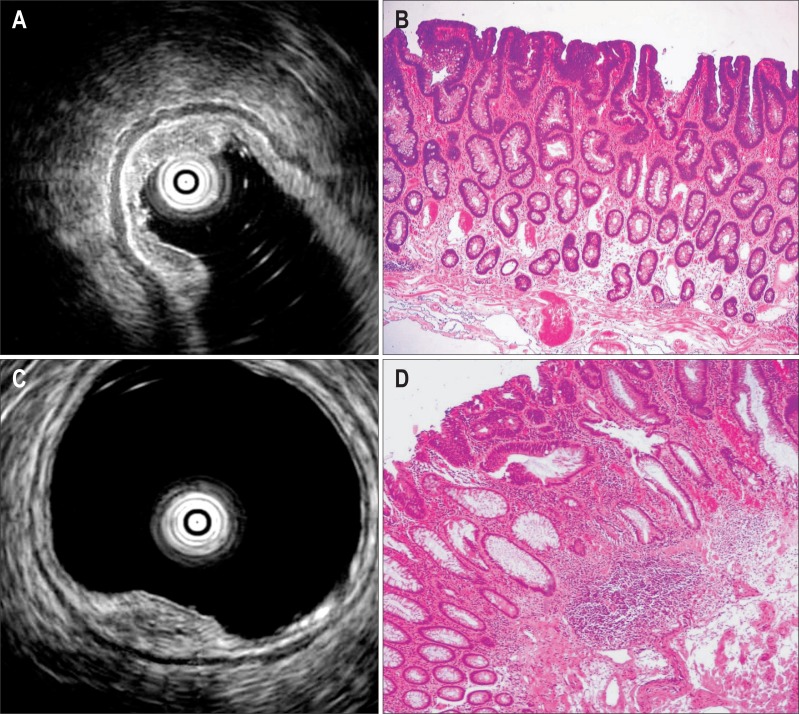
Tumor size and depth of invasion were assessed ultrasonographically and identified by the prefix "u," while the histopathology of the resected specimens was identified by the prefix "p" (Fig. 1). The depth of tumor invasion was categorized according to the TNM classification of malignant tumors. T1 stage was defined as a tumor that was confined to the submucosal layer with or without lymph node invasion. Tumors involving the mucosa, but not the submucosal layer, were classified as T1m. Tumors limited to the submucosal layer and not involving the muscularis propria were classified as T1sm. T2, T3, and T4 cancers were not included in the present study. In submucosal lesions, when invasion of tumor exceeded 1,000 µm, endoscopic treatment was followed by surgery. Tumor characteristics such as location (rectum or other parts of the colon), size (≥2 or <2 cm), tumor shape (sessile/flat or pedunculated), lymphovascular invasion (positive or negative), and tumor differentiation (well or poorly differentiated) were also evaluated.
Fig. 1.
Mini-probe endoscopic ultrasonography (EUS) and corresponding histopathologic findings. Mini-probe EUS (uT1m) (A) and histopathologic image (pT1m) (B) demonstrated that the tumor was confined to the mucosal layer (H&E stain, ×200). In contrast, mini-probe EUS (uT1sm) (C) and histopathologic image (pT1sm) (D) demonstrated that the tumor penetrated into the submucosal layer (H&E stain, ×200).
m, mucosa; sm, submucosa.
3) Statistical analysis
The overall accuracy, accuracy within each group, and mEUS sensitivity and specificity were calculated. The patient baseline characteristics and endoscopic findings were compared using Pearson's chi-square test, Fisher's exact test, or Student's t-test. The effects of location, size, tumor shape, lymphovascular invasion, and tumor differentiation were evaluated using Pearson's chi-square test or Fisher's exact test. The odds ratios (ORs) of large tumors and submucosal lesions affecting the accuracy of T staging were measured using logistic regression. Two-tailed p-values <0.05 were considered statistically significant.
RESULTS
1. Demographic and endoscopic characteristics
Sixty-four (71.1%) and 26 (28.9%) of the 90 lesions were identified as uT1m and uT1sm, respectively. No significant differences were found with respect to gender, age, or tumor location between the two groups. The mean size of the tumors tended to be larger in submucosal group (2.10±0.84 cm) compared to mucosal group (1.68±0.67 cm), although the difference was not statistically significant (p=0.064). With respect to mucosal group, 29.7% (19/64) were pedunculated-type tumors, while only 1 (3.8% [1/26]) submucosal lesion was a pedunculated-type (p=0.008) (Table 1).
Table 1.
Baseline Characteristics of Subjects

Data are presented as number (%) or mean±SD.
uT1m, endoscopic ultrasonography T1 mucosa; uT1sm, endoscopic ultrasonography T1 submucosa.
2. Staging accuracy and outcomes
The overall accuracy for depth of tumor invasion (T stage) was 84.4% (76/90) and the accuracy was significantly lower in submucosal group than in mucosal group (65.4% vs 92.2%; p=0.003). Among the 64 cases of uT1m, 61 cases (95.3%) underwent endoscopic treatment such as EMR (54 cases) or ESD (7 cases), and three cases (4.7%) received surgical therapy initially. Through histopathologic analysis of the resected specimens, 59 cases (92.2%) were correctly diagnosed as pT1m, while five cases (7.8%) were proved as having pT1sm. Two cases received endoscopic treatment followed by surgery because the depth of invasion of the carcinoma exceeded 1,000 µm of submucosa. On the other hand, among the 26 cases of uT1sm, 19 cases (73.1%) underwent surgery. Seven cases received endoscopic therapy initially because they had high risk factors such as old age or comorbidities for surgical complications. Among them, one case (14.3%) underwent additional surgery because the tumor had invaded beyond the submucosal layer by over 1,000 µm. As a result, 20 cases (76.9%) underwent surgery. On pathologic exam, only 17 of 26 lesions (65.4%) were correctly diagnosed as pT1sm (Table 2). In four cases, the involved layer was the mucosa (pT1m), and in five cases, the muscularis propria was also invaded, indicating underestimation of the depth of invasion with mEUS. The sensitivity and specificity of mEUS were 93.7% (95% confidence interval [CI], 83.7 to 97.9) and 81.5% (95% CI, 61.3 to 93.0) in T1m, and 77.3% (95% CI, 54.2 to 91.3) and 86.8% (95% CI, 75.9 to 93.4) in T1sm, respectively. Underestimation and overestimation occurred in 11.1% (10/90) and 4.4% (4/90) of the cases, respectively. Of 14 cases who showed discrepancy between mEUS and histopathologic results, nine had tumors >2 cm in size and nine had submucosal lesions. Eight lesions had submucosal involvement and a size >2 cm.
Table 2.
Correlation between Endoscopic Ultrasonography (uT) and Histopathology (pT)
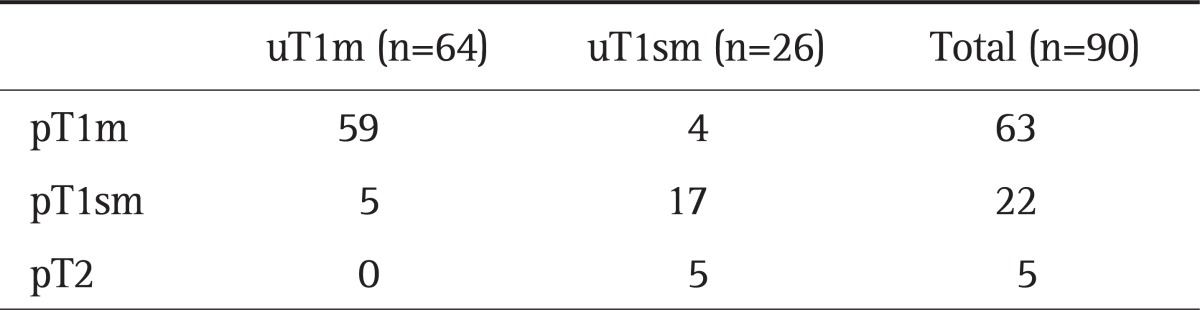
Data are presented as number.
m, mucosa; sm, submucosa.
3. Factors that influenced accuracy
We analyzed the factors that influenced the overall accuracy and group accuracy of mEUS when predicting T stage. There were no correlations between location (rectum and colon), tumor shape (pedunculated or sessile/flat), tumor differentiation, or lymphovascular invasion and accuracy. However, patients with large tumors had a lower overall accuracy than patients with small tumors (≥2 cm vs <2 cm; p=0.034), especially when the tumor involved the submucosal layer (p=0.014) (Table 3). The ORs of large tumors and submucosal tumors affecting the accuracy of T stage when using mEUS were 3.46 (95% CI, 1.05 to 11.39) and 6.25 (95% CI, 1.85 to 25.14), respectively. When submucosal tumors were combined with large tumors, the OR was 14.67 (95% CI, 1.46 to 146.96) (Table 4).
Table 3.
Comparison of the Mini-Probe Endoscopic Ultrasonograpy Accuracy According to the Tumor Characteristics
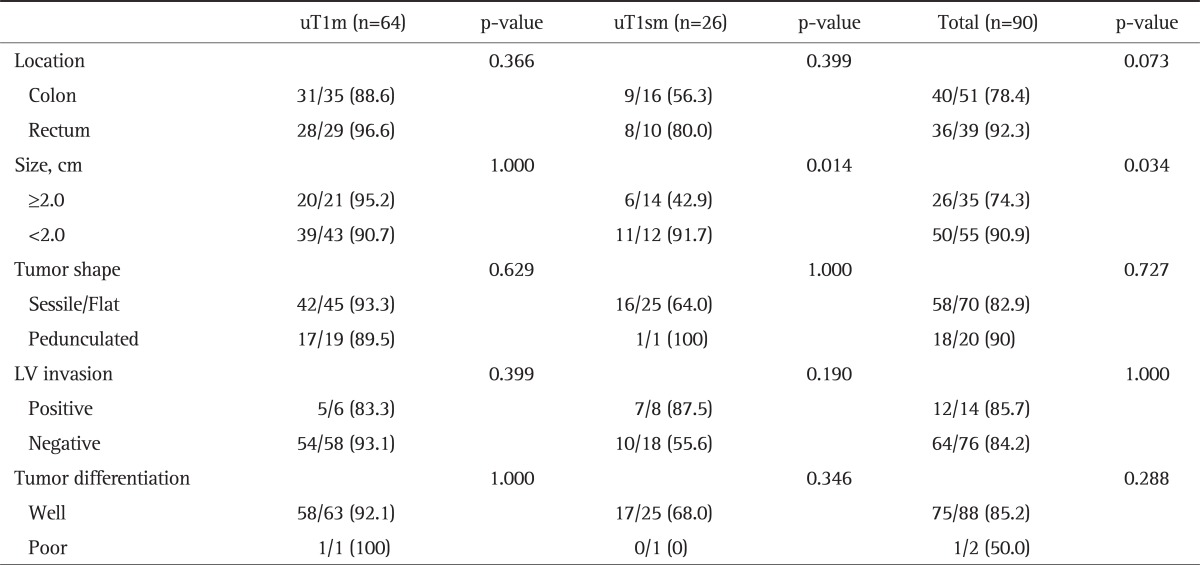
Data are presented as number (%).
LV, lymphovascular; uT1m, endoscopic ultrasonography T1 mucosa; uT1sm, endoscopic ultrasonography T1 submucosa.
Table 4.
Odds Ratio for the Effects of Tumor Size and the Submucosal Lesions on Affecting the Accuracy Rates of Mini-Probe Endoscopic Ultrasonograpy
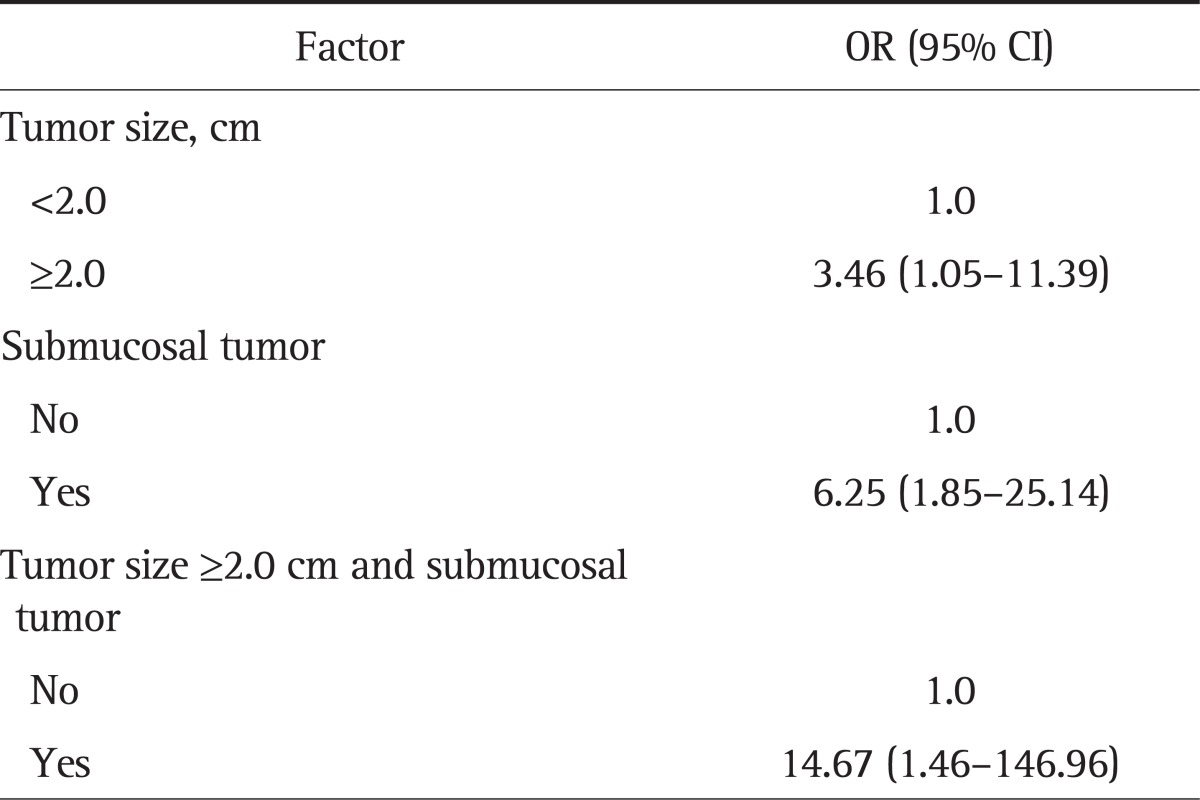
OR, odds ratio; CI, confidence interval.
DISCUSSION
Preoperative evaluation is critical for estimating patient prognosis and determining the appropriate treatment, including whether to perform endoscopic or laparoscopic surgery or not.4,13-16 EUS is one of the most sensitive techniques available for colorectal cancer staging, and as such, has become a standard technique. This approach is superior to computed tomography (CT) in the assessment of tumor invasion (T stage) and lymph node involvement (N stage).17,18 Compared to magnetic resonance imaging (MRI), EUS is more accurate in determining T stage, and is comparable to MRI in evaluating N stage.19-23
Conventional EUS does have some limitations. The equipment is difficult to be maneuvered in the proximal part of the colon and it cannot be passed through narrow segments because of the rigid and large diameter tip.24 In contrast to conventional EUS, mEUS has many benefits. First, it can be easily introduced through the endoscope biopsy channel during a routine colonoscopy without causing additional patient discomfort.4,9 Second, mEUS typically has no problems passing through stenotic lesions9 and it can evaluate colonic lesions located on the right side of the colon.10,12 Third, mEUS provides high-resolution images of the intestinal wall layers resulting in clearer images of superficial carcinoma invasion.4 However, despite these benefits, mEUS has some limitations. For example, mEUS is not suitable for the evaluation of regional lymph node invasion, and mEUS cannot accurately differentiate between stages T3 and T4 because mEUS typically uses high frequency ultrasound, which limits the depth of penetration. In addition, according to previous studies, the accuracy of mEUS may decrease with increasing tumor size, advanced tumor stage, pedunculated-type tumors, villous lesions, and rectal tumors.4,13,25 Results can also be influenced by inadequate contact between the tumor and the probe due to air, stool, or irregular tumor surfaces, anatomic defects from previous biopsies or polypectomy, and peritumoral inflammation.
In the current study, we evaluated the accuracy of mEUS in T1 staging, which was performed as part of the planning of the treatment of ECC. The N stage was evaluated with CT scanning and all patients were confirmed to have no lymph node enlargement. We analyzed 64 and 26 cases with mucosal and submucosal lesions, respectively, to estimate the accuracy of mEUS T staging. Previous studies have reported that the accuracy of mEUS in evaluating the depth of colorectal tumor invasion was 76% to 96% for the T1 to T4 stages.9,10,12,15 More specifically, its accuracy in identifying the T1 stage of colorectal cancer in these studies varied from 67% to 100%.9,10,12 In our study, the overall accuracy of T staging was 84.4%, which is compatible with the findings in previous reports. Of interest, the accuracy in evaluating submucosal lesions (65.4%) was significantly lower than that for mucosal lesions (92.2%, p=0.003). We reasoned that the depth of invasion of lesions located in the submucosal layer may be difficult to be accurately predicted because the 20-MHz mEUS has poor penetration. In fact, there are only a few studies that focus on the accuracy of mEUS in evaluating submucosal ECCs.9,13 Harada et al.13 reported that the accuracy of the mini-probe in categorizing submucosal invasion into three subclasses (SM1, SM2, and SM3) was 37.1% in 35 patients. However, the accuracy of mEUS in differentiating between tumors of SM1 subclass or lower (M and SM1) and tumors of SM2 class or higher (SM2, SM3, muscularis propria, and serosa) was 85.7% (30/35). In the current study, we demonstrated that large tumor size decreased the accuracy of T staging by mEUS, which is consistent with the findings of other studies.4,25 Interestingly, in cases in which the tumor had invaded the submucosa and tumor size was >2 cm, the OR was 14.67 (95% CI, 1.46 to 146.96), suggesting that the accuracy of mEUS had dramatically decreased. Therefore, we suggest that extra caution should be taken when performing mEUS to predict the T stage in submucosal tumors that are >2 cm in size. Several studies have suggested that the accuracy of mEUS was lower in pedunculated-type tumors, villous lesions or tumors located in the rectum.13,25 However, in our study, the shape, location, and histopathological findings such as tumor differentiation or lymphovascular invasion had no effects on the accuracy of T staging by mEUS.
There were several limitations in this study. First, this study was conducted retrospectively, and the treatment strategy was not strictly followed. Although the mEUS findings suggested involvement of the submucosal layer in 26 cases, seven of these 26 cases underwent endoscopic treatment as the initial therapy due to the high risks of operation in these patients. Second, interobserver variability might have been an issue because two specialists were involved in carrying out the mEUS procedures. However, they were all experts and had >5 years experience with mEUS. Additionally, we reviewed all records of mEUS procedures without knowledge of the pathologic findings. The third limitation was that the submucosal population was relatively small, and as a result, we could not subdivide it into classes.
In conclusion, mEUS is an effective, convenient and accurate modality in identifying the T stage of ECC. However, we found that mEUS was less accurate in determining the T stage in submucosal lesions or large tumors. In addition, accuracy rates dropped significantly in submucosal lesions that are >2 cm in size. Therefore, special precautions should be taken when interpreting mEUS results, especially in the cases of large submucosal lesions.
ACKNOWLEDGEMENTS
This study was supported by a grant of Inje University College of Medicine (2012).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.El-Tawil AM. Colorectal cancer and pollution. World J Gastroenterol. 2010;16:3475–3477. doi: 10.3748/wjg.v16.i28.3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdulkareem FB, Abudu EK, Awolola NA, et al. Colorectal carcinoma in Lagos and Sagamu, Southwest Nigeria: a histopathological review. World J Gastroenterol. 2008;14:6531–6535. doi: 10.3748/wjg.14.6531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung KW, Park S, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010;25:1113–1121. doi: 10.3346/jkms.2010.25.8.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunerbein M, Handke T, Ulmer C, Schlag PM. Impact of miniprobe ultrasonography on planning of minimally invasive surgery for gastric and colonic tumors. Surg Endosc. 2004;18:601–605. doi: 10.1007/s00464-003-8925-z. [DOI] [PubMed] [Google Scholar]
- 5.Ikehara H, Saito Y, Matsuda T, Uraoka T, Murakami Y. Diagnosis of depth of invasion for early colorectal cancer using magnifying colonoscopy. J Gastroenterol Hepatol. 2010;25:905–912. doi: 10.1111/j.1440-1746.2010.06275.x. [DOI] [PubMed] [Google Scholar]
- 6.Hurlstone DP, Brown S, Cross SS, Shorthouse AJ, Sanders DS. High magnification chromoscopic colonoscopy or high frequency 20 MHz mini probe endoscopic ultrasound staging for early colorectal neoplasia: a comparative prospective analysis. Gut. 2005;54:1585–1589. doi: 10.1136/gut.2005.069849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsumoto T, Hizawa K, Esaki M, et al. Comparison of EUS and magnifying colonoscopy for assessment of small colorectal cancers. Gastrointest Endosc. 2002;56:354–360. doi: 10.1016/s0016-5107(02)70038-2. [DOI] [PubMed] [Google Scholar]
- 8.Fukuzawa M, Saito Y, Matsuda T, Uraoka T, Itoi T, Moriyasu F. Effectiveness of narrow-band imaging magnification for invasion depth in early colorectal cancer. World J Gastroenterol. 2010;16:1727–1734. doi: 10.3748/wjg.v16.i14.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunerbein M, Totkas S, Ghadimi BM, Schlag PM. Preoperative evaluation of colorectal neoplasms by colonoscopic miniprobe ultrasonography. Ann Surg. 2000;232:46–50. doi: 10.1097/00000658-200007000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurlstone DP, Brown S, Cross SS, Shorthouse AJ, Sanders DS. Endoscopic ultrasound miniprobe staging of colorectal cancer: can management be modified? Endoscopy. 2005;37:710–714. doi: 10.1055/s-2005-870142. [DOI] [PubMed] [Google Scholar]
- 11.Puli SR, Bechtold ML, Reddy JB, Choudhary A, Antillon MR, Brugge WR. How good is endoscopic ultrasound in differentiating various T stages of rectal cancer? Meta-analysis and systematic review. Ann Surg Oncol. 2009;16:254–265. doi: 10.1245/s10434-008-0231-5. [DOI] [PubMed] [Google Scholar]
- 12.Stergiou N, Haji-Kermani N, Schneider C, Menke D, Köckerling F, Wehrmann T. Staging of colonic neoplasms by colonoscopic miniprobe ultrasonography. Int J Colorectal Dis. 2003;18:445–449. doi: 10.1007/s00384-003-0506-z. [DOI] [PubMed] [Google Scholar]
- 13.Harada N, Hamada S, Kubo H, et al. Preoperative evaluation of submucosal invasive colorectal cancer using a 15-MHz ultrasound miniprobe. Endoscopy. 2001;33:237–240. doi: 10.1055/s-2001-12798. [DOI] [PubMed] [Google Scholar]
- 14.Waxman I, Saitoh Y. Clinical outcome of endoscopic mucosal resection for superficial GI lesions and the role of high-frequency US probe sonography in an American population. Gastrointest Endosc. 2000;52:322–327. doi: 10.1067/mge.2000.105723. [DOI] [PubMed] [Google Scholar]
- 15.Saitoh Y, Obara T, Einami K, et al. Efficacy of high-frequency ultrasound probes for the preoperative staging of invasion depth in flat and depressed colorectal tumors. Gastrointest Endosc. 1996;44:34–39. doi: 10.1016/s0016-5107(96)70226-2. [DOI] [PubMed] [Google Scholar]
- 16.Hartley JE, Mehigan BJ, MacDonald AW, Lee PW, Monson JR. Patterns of recurrence and survival after laparoscopic and conventional resections for colorectal carcinoma. Ann Surg. 2000;232:181–186. doi: 10.1097/00000658-200008000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rifkin MD, Ehrlich SM, Marks G. Staging of rectal carcinoma: prospective comparison of endorectal US and CT. Radiology. 1989;170:319–322. doi: 10.1148/radiology.170.2.2643135. [DOI] [PubMed] [Google Scholar]
- 18.Beynon J, Mortensen NJ, Foy DM, Channer JL, Virjee J, Goddard P. Pre-operative assessment of local invasion in rectal cancer: digital examination, endoluminal sonography or computed tomography? Br J Surg. 1986;73:1015–1017. doi: 10.1002/bjs.1800731228. [DOI] [PubMed] [Google Scholar]
- 19.Kim NK, Kim MJ, Yun SH, Sohn SK, Min JS. Comparative study of transrectal ultrasonography, pelvic computerized tomography, and magnetic resonance imaging in preoperative staging of rectal cancer. Dis Colon Rectum. 1999;42:770–775. doi: 10.1007/BF02236933. [DOI] [PubMed] [Google Scholar]
- 20.Bianchi PP, Ceriani C, Rottoli M, et al. Endoscopic ultrasonography and magnetic resonance in preoperative staging of rectal cancer: comparison with histologic findings. J Gastrointest Surg. 2005;9:1222–1227. doi: 10.1016/j.gassur.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Bianchi P, Ceriani C, Palmisano A, et al. A prospective comparison of endorectal ultrasound and pelvic magnetic resonance in the preoperative staging of rectal cancer. Ann Ital Chir. 2006;77:41–46. [PubMed] [Google Scholar]
- 22.Harewood GC, Wiersema MJ, Nelson H, et al. A prospective, blinded assessment of the impact of preoperative staging on the management of rectal cancer. Gastroenterology. 2002;123:24–32. doi: 10.1053/gast.2002.34163. [DOI] [PubMed] [Google Scholar]
- 23.Herzog U, von Flüe M, Tondelli P, Schuppisser JP. How accurate is endorectal ultrasound in the preoperative staging of rectal cancer? Dis Colon Rectum. 1993;36:127–134. doi: 10.1007/BF02051167. [DOI] [PubMed] [Google Scholar]
- 24.Kuntz C, Kienle P, Buhl K, Glaser F, Herfarth C. Flexible endoscopic ultrasonography of colonic tumors: indications and results. Endoscopy. 1997;29:865–870. doi: 10.1055/s-2007-1004323. [DOI] [PubMed] [Google Scholar]
- 25.Konishi K, Akita Y, Kaneko K, et al. Evaluation of endoscopic ultrasonography in colorectal villous lesions. Int J Colorectal Dis. 2003;18:19–24. doi: 10.1007/s00384-002-0423-6. [DOI] [PubMed] [Google Scholar]