Abstract
Parapharyngeal space tumors are rare, accounting for 0.5% of head and neck neoplasms. Most of them are benign and originate in the salivary glands, especially the pleomorphic adenoma. We presented a 47-year-old male with parotid tail pleomorphic adenoma extending to the parapharyngeal space. The patient applied to our clinic with the complaints of a painless mass on his neck and in his mouth for three months. After fine needle aspiration biopsy the mass was diagnosed as pleomorphic adenoma. The patient hospitalized and operated in our clinic. As we see in literature review parapharyngeal space tumors are rare and most of them are pleomorphic adenomas arising from deep lobe of the parotid gland and extend into the PPS.
Keywords: Parapharyngeal space tumors, Parotid tail pleomorphic adenoma, Intraoral surgical approach
Introduction
Parapharyngeal space tumors are rare, accounting for 0.5% of head and neck neoplasms. Most of these tumors (70%–80%) are benign and 40–50% of these originate in the salivary glands, particularly the pleomorphic adenoma (1). Pleomorphic adenoma in the parapharyngeal space (PPS) can develop de novo or may arise from deep lobe of the parotid gland and extend into the PPS (2). Management of these tumors represents a challenge to surgeons because of vital neurovascular structures (3).
The incidence of salivary gland tumors is approximately 3% of all head and neck cancers (4). The salivary gland tumors are most commonly seen in parotid gland; 50–74% of all parotid lesions are benign pleomorphic adenomas (5).
Case Report
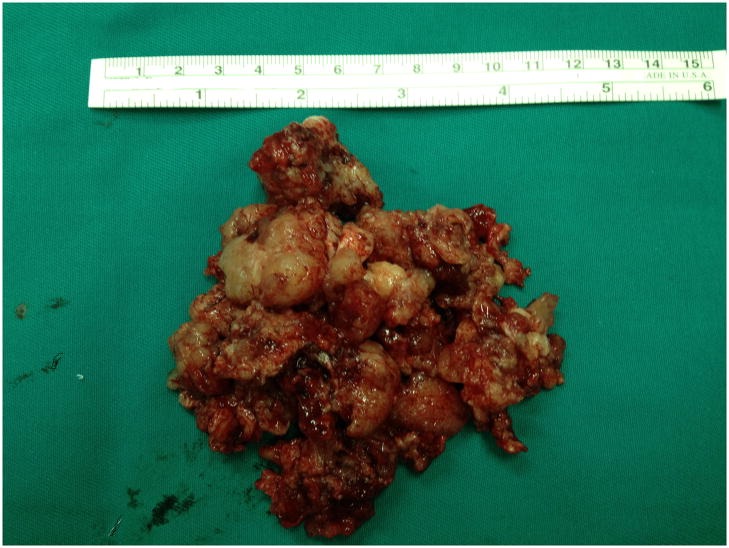
A 47-year-old male came to our clinic with the complaints of a painless mass on his neck and in his mouth for three months (fig. 1). This mass had begun to grow for last twenty days and the patient had difficulty in swallowing and even talking. In clinical examination there was a mass just behind the right tonsil and the tonsil was pushed medially. In laryngeal and nasopharyngeal endoscopic examination there was not any pathology detected except right parapharyngeal place. The routine laboratory tests were in normal range.
Figure 1.
The preoperative view of the mass from oral cavity.
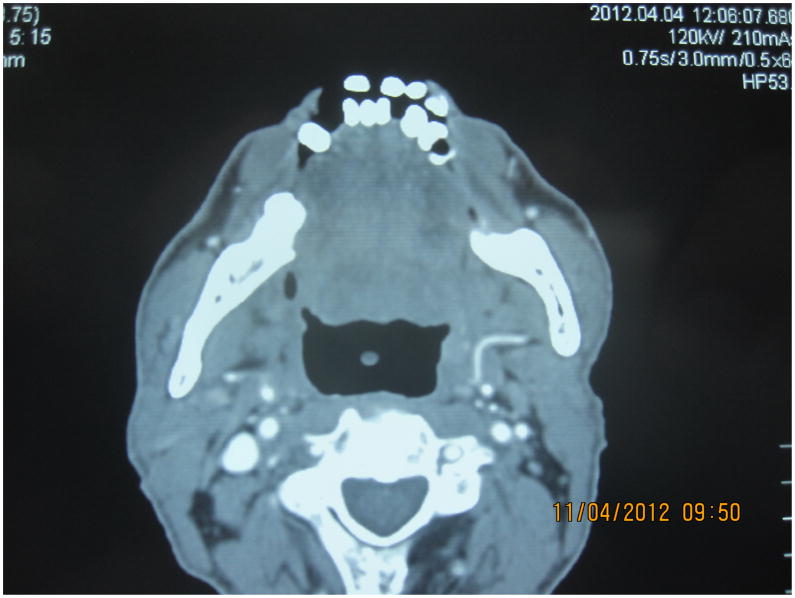
He had an ultrasound imaging with him performed in another clinic and there was a solid mass about 76×55 mm in diameter in right jugulodigastric place. We took a cervical computed tomography (CT) with contrast and in CT scan a non-homogenously contrast enhancing mass was reported beginning from nasopharynx extending to the hyoid bone level, obliterating the right rosenmüller fossa, torus tubarius and eustachian tube and narrowing the air passage. The mass had cystic-necrotic fields and was 4×6×8 cm in diameter. The right submandibular gland was deplaced inferiorly due to the mass (fig. 2). Cervical CT anjiography was applied to understand the relation of the mass with vascular structures and its result reported that the right jugular vein was displaced posteriorly by the mass.
Figure 2.
Cervical CT scan with contrast in axial plane, showing the mass narrowing the air passage.
Fine needle aspiration biopsy was performed to the patient and the result was compatible with pleomorphic adenoma.
The patient was taken to surgery and firstly right tonsillectomy was done. The encapsulated mass was seen and dissected from surrounding structures by intraoral way (fig. 3). The mass was extending towards the parotid tail and the tail was the source of it. Therefore the mass was excised totally together with the parotid tail (fig. 4). The patient was discharged from the hospital after one week. After two months we performed a maxillofacial computed tomography with contrast for control and there was not seen any mass in that region (fig. 5).
Figure 3.

Intraoperative view of the mass with intraoral approach.
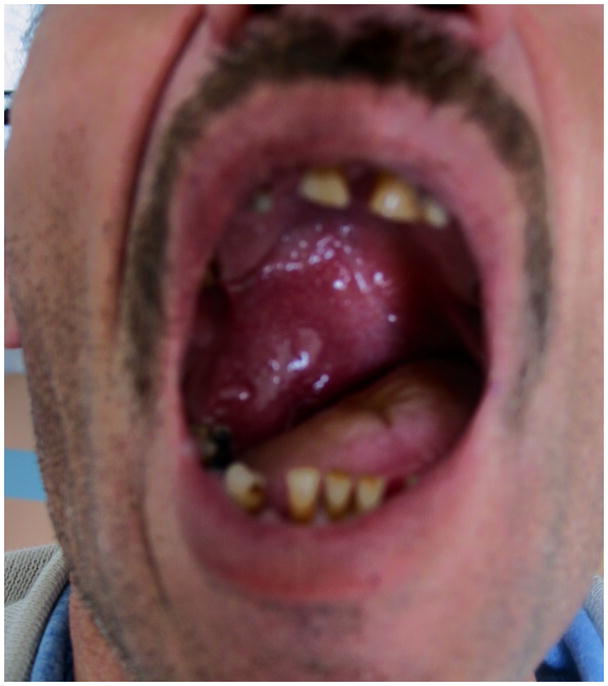
Figure 4.
Macroscopic view of the mass.
Figure 5.
Postoperative maxillofacial CT scan with contrast in axial plane showing a normal anatomy without any mass.
Discussion
PPS is situated laterally with respect to the nasopharynx and in front of the cervical column showing the shape of an inverted pyramid located behind the skull base whose apex defines the joint between the posterior belly of the digastric muscle and the greater cornu of the hyoid bone. The styloid process and the associated musculature are also located there, and other structures are the carotid and jugular vessels; cranial nerves V, VII, IX, X, and XII; the deep lobe of the parotid gland; and some lymph nodes (3).
Pleomorphic adenoma (PA) is the most common tumor of the parotid gland. It is a benign, slowly growing tumor. The treatment of PA is surgical excision. Because of its pseudocapsule and fingerlike projections, failure to resect some normal surrounding parotid tissue with the tumor usually results in a high recurrence rate (20%–45%) (6). Pleomorphic adenoma is classified by the World Health Organization as a benign neoplasm of the salivary glands characterized by cellular and architectural pleomorphism (7). The microscopic analysis revealed epithelial and myoepithelial elements immersed in a mucoid, myxoid, or chondroid matrix. Fibrous capsule can be presented (8).
PAs are found rarely in the PPS and thus both diagnosis and surgical management are difficult. Most of these tumors remain silent for a long time since they grow slowly, and do not show symptoms even if tumors are in contact, or displace, vital structures located in the PPS (9). Among benign PPS tumors, the pleomorphic adenoma, originating either from the parotid gland or from some aberrant minor salivary gland, is the most represented entity, accounting for approximately 40% of all benign PPS lesions and 63% of all parotid gland tumors (10,11).
Most of the benign tumors of the salivary gland in the oral cavity present as a painless submucosal swelling, those from the parapharyngeal space may also show additional symptoms, like otalgia, neuralgia, foreign body sensation in the throat, difficulty with swallowing, voice changes, trismus, otologic symptoms, obstruction of the Eustachian tube, 9th, 10th, or 11th cranial nerve deficits, and, rarely, obstructive sleep apnea. Submucosal swelling in the lateral pharyngeal wall with or without extension to retromandibular fossa or the submandibular trigone are the classical findings of benign parapharyngeal swellings (12–16). PPS is a difficult place to clinical examination as it is surrounded by the muscles of mastication, mandible, and parotid gland. Symptoms are usually noticed when the tumor is larger than 2.5–3 cm (1,17)
CT scan and MRI are important diagnostic tools in parapharyngeal space tumors. They are used to determine the extent of disease, local spread and also type of tumor. Contrast enhancement is seen in vascular and neurogenic tumors. Presence of intact fat plane helps in distinguishing benign tumors from malignant ones. A fine translucent line can distinguish the extension of tumors from the deep lobe of a parotid gland from tumor arising de novo in parapharyngeal space by representing the compressed layer of fibroadipose tissue between the tumor and deep lobe of parotid (18). In a study on 51 patients with a PPS neoplasm, both benign and malignant, the mass was able to be localized in 95% and 84% of patients with CT and MRI (11).
Fine needle aspiration cytology is the modality of choice for obtaining biopsy sample for diagnosis (2). In PPS tumors, 25% of intraoral FNA may not be diagnostic because of the lack of adequate cellular material. The positive predictive value to identify benign tumors is 90% when performing an ultrasound-guided FNA or CT but drops to 75% for malignant (19,20).
There are several surgical approaches to PPS tumors. External approaches such as; cervical-transparotid, transparotid, transcervical (via submandibular or transmandibular), via infratemporal fossa and intraoral approach (21,22). Though these tumors are apparently well encapsulated, it is necessary to resect an adequate margin of grossly normal surrounding tissue to be able to prevent local recurrence because these tumors have microscopic pseudopod-like extension into the surrounding tissue (18). In the usual cervical–transparotid approach to the PPS, a superficial parotidectomy with facial nerve dissection is performed to expose the underlying deep lobe together. The cervical incision makes it possible to access to the PPS compartment via the submandibular gland, which can be removed or displaced. In the long run, this procedure can cause a visible facial defect as a result of volume loss. We preferred intraoral approach because of the great benefit of having no aesthetic sequelae and minimal functional complications and the tumor was attainable from oral cavity (3,23,24).
The prognosis for PAs found in the PPS is good. According to some studies, the recurrence rate was 5%, which may be related to the fragmentation of the tumor or capsular damage when removed (19,25,26). When the pleomorphic adenoma shows recurrence, in addition to revision surgery radiotherapy is recommended to the patients with residual tumor, multinodular disease and known tumor spillage (27).
Conclusion
We report this case to emphasize that the masses around parapharyngeal spaces should be evaluated carefully, because they may be originated not only from this space but also from adjacent anatomical structures. As in our case an intraoral mass can rarely be derived from parotis gland. We also aimed to suggest an approach to parotid tail pleomorphic adenoma extending to the parapharyngeal space both in diagnosis and treatment.
Contributor Information
Kerem Polat, Cumhuriyet University School of Medicine, Department of Otolaryngology
Mansur Doğan, Cumhuriyet University School of Medicine, Department of Otolaryngology.
Salim Yüce, Cumhuriyet University School of Medicine, Department of Otolaryngology.
İsmail Önder Uysal, Cumhuriyet University School of Medicine, Department of Otolaryngology.
Suphi Müderris, Cumhuriyet University School of Medicine, Department of Otolaryngology.
References
- 1.Khafif A, Segev Y, Kaplan DM, Gil Z, Fliss D. Surgical management of parapharyngeal space tumours: a 10- year review. Otolaryngol Head Neck Surg. 2005;132:401–406. doi: 10.1016/j.otohns.2004.09.062. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Giurana J, Rodado C, Saez M, Bassas C. Giant parotid pleomorphic adenoma involving the parapharyngeal Space: report of a case. J Oral Maxillofac Surg. 2000;58:1184–1187. doi: 10.1053/joms.2000.9587. [DOI] [PubMed] [Google Scholar]
- 3.Zhi K, Ren W, Zhou H, Wen Y, Zhang Y. Management of parapharyngeal-space tumors. J Oral Maxillofac Surg. 2009;67:1239–1244. doi: 10.1016/j.joms.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Leegaard T, Lindeman H. Salivary gland tumors: clinical picture and treatment. Acta Otolayngol. 1970;263:155–159. [PubMed] [Google Scholar]
- 5.Redaelli de Zinis LO, Piccioni M, Antonelli AR, et al. Management and prognostic factors of recurrent pleomorphic adenoma of the parotid gland: personal experience and review of the literature. Eur Arch Otorhinolaryngol. 2008;265:447–452. doi: 10.1007/s00405-007-0502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suh MW, Kwon SK, Jung YH, Kwon TK, Kim HK, Sung MW. Clinical manifestations of recurrent parotid pleomorphic adenoma. Clin Exp Otorhinolaryngol. 2009;2:193–197. doi: 10.3342/ceo.2009.2.4.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes L, Eveson JW, Reichart P, et al., editors. Pathology and Genetics of Head and Neck Tumours. Lyon, France: IARC Press; 2005. World Health Organization Classification of Tumours. [Google Scholar]
- 8.Gnepp DR. Malignant mixed tumors of the salivary glands: a review. Pathol Annu. 1993;28:279–328. [PubMed] [Google Scholar]
- 9.Bozza F, Vigili MG, Ruscito P, Marzetti A, Marzetti F. Surgical management of parapharyngeal space tumours: results of 10-year follow-up. Acta Otorhinolaryngol Ital. 2009;29:10–15. [PMC free article] [PubMed] [Google Scholar]
- 10.Batsakis JG, Sneige N. Pathology consultation: parapharyngeal and retropharyngeal space diseases. Ann Otol Rhinol Laryngol. 1989;98:320–321. doi: 10.1177/000348948909800416. [DOI] [PubMed] [Google Scholar]
- 11.Miller FR, Wanamaker JR, Lavertu P, Wood BG. Magnetic resonance imaging and the management of parapharyngeal space tumours. Head Neck. 1988;18:67–77. doi: 10.1002/(SICI)1097-0347(199601/02)18:1<67::AID-HED9>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 12.Hughes KV, Oslen KD, McCaffery TV. Parapharyngeal space neoplasms. Head Neck. 1995;17:124–130. doi: 10.1002/hed.2880170209. [DOI] [PubMed] [Google Scholar]
- 13.Eveson JW, Cawson RA. Tumour of the minor (oropharyngeal) salivary gland: demographic study of 336 cases. J Oral Pathol. 1985;14:500–509. doi: 10.1111/j.1600-0714.1985.tb00522.x. [DOI] [PubMed] [Google Scholar]
- 14.Cohen MA. Pleomorphic adenoma of the cheek. Int J Oral maxillofac surg. 1986;15:777–779. doi: 10.1016/s0300-9785(86)80123-5. [DOI] [PubMed] [Google Scholar]
- 15.Giddings CE, Bray D, Rimmer J, Williamson P. Pleomorphic adenoma and severe obstructive sleep apnoea. J Laryngol Otol. 2005;119:226–229. doi: 10.1258/0022215053561602. [DOI] [PubMed] [Google Scholar]
- 16.Mendelsohn AH, Bhuta S, Calcaterra TC, Shih HB, Abemayor E, St John MA. Parapharyngeal space pleomorphic adenoma: a 30-year review. Laryngoscope. 2009;119:2170–2174. doi: 10.1002/lary.20496. [DOI] [PubMed] [Google Scholar]
- 17.Dimitrijevic MV, Jesic SD, Mikic AA, Arsovic NA, Tomanovic NR. Parapharyngeal space tumors: 61 case reviews. Int J Oral Maxillofac Surg. 2010;39:983–989. doi: 10.1016/j.ijom.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Work PW, Gates GA. Tumours of parapharyngeal space. Otolaryngol Clin N Am. 1969:479–514. [Google Scholar]
- 19.Papadogeorgakis N, Petsinis V, Goutzanis L, Kostakis G, Alexandridis C. Parapharyngeal space tumors: surgical approaches in a series of 13 cases. Int J Oral Maxillofac Surg. 2010;39:243–250. doi: 10.1016/j.ijom.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 20.Farrag TY, Lin FR, Koch WM, Califano JA, Cummings CW, Farinola MA, Tufano RP. The role of pre-operative CTguided FNAB for parapharyngeal space tumors. Otolaryngol Head Neck Surg. 2007;136:411–414. doi: 10.1016/j.otohns.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Ruiz-Laza L, Infante-Cossio P, Garcia-Perla A, Hernandez-Guisado JM, Gutierrez-Perez JL. Giant pleomorphic adenoma in the parapharyngeal space: report of 2 cases. J Oral Maxillofac Surg. 2006;64:519–523. doi: 10.1016/j.joms.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 22.Fernández-Ferro M, Fernández-Sanromán J, Costas-López A, Sandoval Gutiérrez J, López de Sánchez A. Surgical treatment of benign parapharyngeal space tumours. Presentation of two clinical cases and revision of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E61–E64. [PubMed] [Google Scholar]
- 23.Avitia S, Hamilton JS, Osborne RF. Deep-lobe parotid tumor presenting in the parapharyngeal space. Ear Nose Throat J. 2007;86:730–731. [PubMed] [Google Scholar]
- 24.Hussain A, Murray DP. Preservation of the superficial lobe for deep-lobe parotid tumors: a better aesthetic outcome. Ear Nose Throat J. 2005;84:518–524. [PubMed] [Google Scholar]
- 25.Malone JP, Agrawal A, Schuller DE. Safety and efficacy of transcervical resection of parapharyngeal space neoplasms. Ann Otol Rhinol Laryngol. 2001;110:1093–1098. doi: 10.1177/000348940111001202. [DOI] [PubMed] [Google Scholar]
- 26.Pang KP, Goh CH, Tan HM. Parapharyngeal space tumours: an 18 year review. J Laryngol Otol. 2002;116:170–175. doi: 10.1258/0022215021910447. [DOI] [PubMed] [Google Scholar]
- 27.Polat ş, Serin GM, Öztürk Ö, Üneri C. Pleomorphic adenomas recurrences within the parapharyngeal space. J Craniofac Surg. 2011 May;22(3):1124–8. doi: 10.1097/SCS.0b013e3182108f3b. [DOI] [PubMed] [Google Scholar]