Abstract
Background
Palliative care clinical and educational programs are expanding to meet the needs of seriously ill patients and their families. Multiple reports call for an enhanced palliative care evidence base.
Objective
To examine current National Institutes of Health (NIH) funding of palliative medicine research and changes since our 2008 report.1
Methods
We sought to identify NIH funding of palliative medicine from 2006 to 2010 in two stages. First, we searched the NIH grants database RePorter2 for grants with key words “palliative care,” “end-of-life care,” “hospice,” and “end of life.” Second, we identified palliative care researchers likely to have secured NIH funding using three strategies: (1) We abstracted the first and last authors' names from original investigations published in major palliative medicine journals from 2008 to 2010; (2) we abstracted these names from a PubMed generated list of all original articles published in major medicine, nursing, and subspecialty journals using the above key words Medical Subject Headings (MESH) terms “palliative care,” “end-of-life care,” “hospice,” and “end of life;” and (3) we identified editorial board members of palliative medicine journals and key members of palliative medicine research initiatives. We crossmatched the pooled names against NIH grants funded from 2006 to 2010.
Results
The NIH RePorter search yielded 653 grants and the author search identified an additional 352 grants. Compared to 2001 to 2005, 589 (240%) more grants were NIH funded. The 391 grants categorized as relevant to palliative medicine represented 294 unique PIs, an increase of 185 (269%) NIH funded palliative medicine researchers. The NIH supported 21% of the 1253 original palliative medicine research articles identified. Compared to 2001 to 2005, the percentage of grants funded by institutes other than the National Cancer Institute (NCI), the National Institute for Nursing Research (NINR), and the National Institute of Aging (NIA) increased from 15% to 20% of all grants.
Conclusions
When compared to 2001–2005, more palliative medicine investigators received NIH funding; and research funding has improved. Nevertheless, additional initiatives to further support palliative care research are needed.
Introduction
The development of the specialty of palliative medicine has been a critical step in addressing the unmet needs of patients with serious illness and their families. The growth of this field has been remarkable. There has been an increase from 658 hospital palliative care teams (24.5%) to 1568 (63.0%)—a steady 138.3% increase from 2000 to 2009.3 Nevertheless, the field continues to face some sizeable challenges if care for seriously ill patients and their families is to improve. Specifically, federal funding to palliative medicine researchers is critical to support improvements in the evidence base for seriously ill patients and their families.
Our prior report about the state of palliative care funding reported inadequacies in both the number of studies published and, more significantly, in the number of studies supported by federal dollars. Over the five-year period 2001 to 2005, we identified only 388 original palliative medicine research manuscripts published in palliative medicine, general medicine, or relevant subspecialty journals. Whereas 279 (71.9%) manuscripts were supported by external funding, the majority of studies were supported by foundation grants (51%) and only a minority (31%) reported any National Institutes of Health (NIH) funding. Three NIH institutes, National Cancer Institute (NCI); National Institute for Nursing Research (NINR); and National Institute of Aging (NIA) funded 85% of all awards identified. Fewer than 1% of all funded grants by the National Cancer Institute; the National Heart, Lung and Blood Institute; the National Institute on Diabetes, Digestives and Kidney Diseases; and the National Institute on Aging were awarded to investigators performing palliative medicine research. Finally, 109 principal investigators (PIs) accounted for the 418 funded NIH awards, a mean of 3.8 grants/investigator.
Since our 2008 report, a number of national initiatives have been undertaken to stimulate and support new federally funded palliative care research. Examples of such initiatives include the development of the National Palliative Care Research Center (www.NPCRC.org); targeted funding of palliative care research by the American Cancer Society,4 the largest funder of research outside of NIH and VA; the development of the NINR funded Palliative Care Research Cooperative (www.palliativecareresearch.org/PCRC/Home.html); support for early stage investigators by the leading nursing and physician professional organizations, the American Academy of Hospice and Palliative Medicine (AAHPM) and the Hospice and Palliative Nursing Association (HPNA); the growth and expansion of palliative medicine departments and divisions within academic medical centers; and new funding initiatives in palliative care research from NINR.5 Finally, the major journals in palliative medicine have undergone significant growth, providing an important venue for the publication of palliative care research findings.
Given the changes outlined above, we performed the following study to examine NIH funding for published palliative medicine research from 2006 to 2010, to update our prior work and to help support and guide NIH funding priorities in this area.
Methods
We conducted a two-stage process to identify NIH funding related to palliative care from 2006 to 2010. First, we searched the NIH RePorter grants database for all grants with the key words “palliative care,” “end-of-life care,” “hospice,” and “end of life.” RePorter2 is an electronic tool that allows users to search a repository of NIH funded research projects and access publications and patents resulting from NIH fundings. Second, we supplemented this initial search by identifying palliative care researchers likely to have secured NIH funding. Potential NIH fundees were identified as follows. First, we abstracted the first and last authors' names from all original investigations published in major palliative medicine journals from 2008 to 2010. We reviewed all articles published in the major palliative medicine journals (Journal of Palliative Medicine, Journal of Pain and Symptom Management, Palliative Medicine, Palliative and Supportive Care, and Journal of Hospice and Palliative Nursing). Second, we searched PubMed using the key MESH terms “palliative care,” “end-of-life care,” “hospice,” and “end of life” and abstracted the first and last authors' names from all articles published in major adult internal medicine journals (Annals of Internal Medicine, New England Journal of Medicine, British Medical Journal, Lancet, Archives of Internal Medicine, and American Journal of Medicine) and relevant high-impact subspecialty journals, representing care of patients with serious illness (Journal of Clinical Oncology, Journal of the American Geriatrics Society, Journal of General Internal Medicine, Journals of Gerontology, American Journal of Respiratory and Critical Care Medicine, Critical Care Medicine, Thorax, Circulation, Circulation Research, and Journal of the American College of Cardiology). Finally, we identified all editorial board members of palliative medicine journals, National Palliative Care Research Center grantees and committee members, and the American Cancer Society's Palliative Care Initiative grantees and committee members.
In order to examine NIH funding in palliative medicine research, we compiled this list of U.S. palliative medicine researchers and then crossmatched this list against all funded NIH research projects from 2006 to 2010. We used the NIH ExPorter system6 to download all project data from the fiscal years 2006 to 2010. ExPorter makes downloadable versions of the data accessed through the Reporter interface available to the public. The resulting list of 839 names was crossmatched with the list of PIs from NIH ExPorter project data from 2006 to 2010. Subsequently, we generated a list of grants awarded to the palliative medicine researchers. From the NIH annual project data reports we abstracted the PI's name, the grant number, the grant title, the PI's institution, administering institute, activity code, the dollar value for each grant (when available), and the start date and end date of the grant.
The two authors (LPG, RSM) independently hand reviewed all the identified grants for relevance to palliative medicine, as determined by the National Consensus Project for Quality Palliative Medicine.7 Of the 653 grants identified in the NIH Reporter key word search, the authors (LPG and RSM) agreed that 331 of the grants were relevant to palliative medicine, with 100% agreement. Of the 533 grants identified in the author search for NIH grants determined to be relevant to palliative medicine, the authors agreed that 218 were relevant to palliative medicine, with 100% agreement.
Of the 218 grants from the author search for NIH grants, 126 were unique grants, of which 77 were also identified in the NIH RePorter search. Overall, from the search by author name, 49 additional unique grants were identified and 29 unique investigators, which were not identified in the NIH Reporter key word search.
Finally, the 391 unique grants categorized as relevant to palliative medicine were further categorized independently by each author (LPG and RSM) into one of the following ten categories: (1) studies focused on pain and physical symptom management and quality of life, (2) studies examining psychological, spiritual, and emotional symptoms, (3) studies focused on instrument development and measurement, (4) health services research evaluating systems of care, (5) decision making and communication studies, (6) studies focused on education and training in palliative medicine, (7) studied focused on caregivers and families, (8) pediatrics studies, (9) career development awards, and (10) other. The authors agreed on the categories for 375 of 391 NIH grants. For the 16 on which the authors disagreed (4%), grant topics were discussed until consensus was reached.
Results
We identified 653 grants from our initial NIH RePorter search and 533 grants from the author search, of which 179 were also identified in the NIH RePorter search, for a total of 1007 unique grants. Of these, we identified 391 grants relevant to palliative medicine awarded to 294 unique principal investigators (mean of 1.33 grants per investigator). Of the 1253 original research articles identified, 21% were supported by NIH funding. Overall, grants from 2006 to 2010 related to palliative care research comprised 0.2% of total grants awarded by NIH.
We identified 1253 original palliative medicine research manuscripts published by U.S. authors from 2008 to 2010. Of these, 1095 papers (87%) were published in palliative medicine journals and 158 (13%) in general medicine and relevant subspecialty journals.
Types of grants
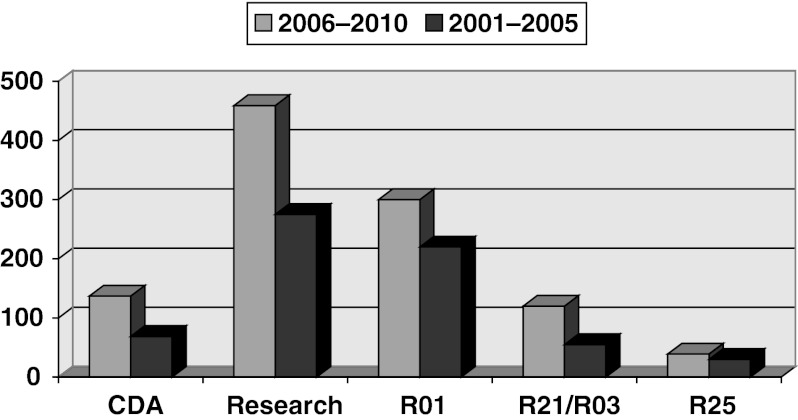
Of the awards identified, 52 (13%) were career development awards—24 to junior investigators and 16 to midcareer/senior investigators. Research awards accounted for 258 (66%), of which 119 (46%) were R01s, 74 (29%) were R21s and R03s, 30 (12%) were R25 education awards, and 35 (14%) represented other funding mechanisms (see table). The data on budgets was incomplete, but the total dollars awarded to each grant type was <0.1% of the total budget for each grant type.
Table 1.
NIH Funded Palliative Care Research by Institute, 2006–2010, N Grants (%)
| Institute | All institutes | Junior CDA (K01, K08, K23, K22, K99) | Mid-Senior CDA (K05, K24, K02) | K07 | K23 | K24 | R21/R03 | R01 | R25 |
|---|---|---|---|---|---|---|---|---|---|
| Institute totals | 391 | 24 | 16 | 12 | 16 | 11 | 74 | 119 | 30 |
| NIA | 71 (18.2) | 15 (62.5) | 7 (43.8) | 3 (25) | 11 (68.8) | 5 (45.5) | 9 (12.2) | 20 (16.8) | 0 |
| NCI | 125 (32.0) | 2 (8.3) | 5 (31.3) | 9 (75) | 1 (6.3) | 2 (18.2) | 22 (29.7) | 36 (30.3) | 30 (100) |
| NHLBI | 5 (1.3) | 0 | 2 (12.5) | 0 | 0 | 2 (18.2) | 0 | 2 (1.7) | 0 |
| NCCAM | 5 (1.3) | 0 | 1 (6.3) | 0 | 0 | 1 (9.1) | 2 (2.7) | 2 (1.7) | 0 |
| NIMH | 6 (1.5) | 2 (8.3) | 1 (6.3) | 0 | 2 (12.5) | 1 (9.1) | 0 | 0 | 0 |
| NINR | 123 (31.5) | 0 | 0 | 0 | 0 | 0 | 3 (4.1) | 46 (38.7) | 0 |
| NIDDK | 1 (0.3) | 0 | 0 | 0 | 0 | 0 | 1 (1.4) | 0 | 0 |
| NCRR | 9 (2.3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 46 (11.8) | 5 (20.1) | 0 | 0 | 2 (12.5) | 0 | 37 (50) | 13 (10.9) | 0 |
CDA, career development award.
Research area
Of 391 NIH grants, 77 (19.7%) focused on pain, nonpain symptoms, and quality of life; 39 (10.0%) supported education and training in palliative medicine; 52 (13.3%) funded decision making and communication studies; 24 (6.1%) funded studies examining psychological, spiritual, and emotional symptoms; 71 (18.2%) funded health services research evaluating systems of care, 11 (2.8%) funded studies related to measurements or instrument development, 33 (8.4%) funded studies related to caregivers and families of seriously ill patients; 25 (6.4%) funded pediatrics studies; and 7 (1.8%) funded other areas of research.
Funding institutes
Three NIH institutes, NCI, NINR, and NIA, funded 81.7% of all awards. Specifically, 125 (32%) were funded by NCI (0.4% of all NCI research grants awarded); 123 (31.5%) were funded by NINR (7.6% of all NINR grants); 71 (18.2%) were funded by NIA (0.8% of all NIA grants); 6 (1.5%) were funded by the National Institute of Mental Health (NIMH) (0.04% of all NIMH grants); and 66 (16.9%) were funded by fifteen other institutes/centers.
Discussion
This study updates our prior research examining NIH funding in palliative medicine.1 With significant growth of the field in the last five years, it is important to note the significant strides made by palliative medicine researchers in a challenging funding environment. These data demonstrate a significant increase in the number of palliative medicine investigators with NIH funding, a critical step necessary to enhance the evidence base of our field.
Highlighted differences between our last report and this update
Compared to 2001 to 2005, the combination of the NIH RePorter search from 2006 to 2010 and the author search from 2008 to 2010 resulted in 1007 unique grants. This represents an increase of 589 funded grants (240%) over the same five-year period. Furthermore, compared to 2001 to 2005, the identified 391 unique NIH grants relevant to palliative care, which were awarded to 294 investigators, represent an increase of 185 NIH funded researchers (269%). More importantly, compared to the period of 2001 to 2005, there has been an increase in NIH grants in both career development and research awards (see Figure 1). Whereas in 2001 to 2005, NCI, NINR, and NIA funded 85% of grants in palliative care research, these new data show funding by other institutes increased from 15% to 20% of all grants. Compared to our initial study examining palliative medicine research from 2001 to 2005, we found a broader research breadth with more distribution of grants across research areas and with a decrease in grants focused on pain, nonpain symptoms, and quality of life and an increase in grants focused on pediatrics, a newer area in great need of development and support (see Figure 2).
FIG. 1.
A comparison of NIH funding for palliative care research by grant type: 2001–2005 versus 2006–2010.
FIG. 2.
A comparison of NIH funding for palliative care research by research area: 2001–2005 versus 2006–2010.
Our updated results also demonstrate areas for improvement. From 2001 to 2005, fewer than 1% of all grants funded by the NCI; National Heart, Lung and Blood Institute; National Institute on Diabetes, Digestive and Kidney Diseases; and the NIA were awarded to investigators performing palliative medicine research. Our current study demonstrates that these data have not changed over 10 years, with <1% of all NIH research funding studies in palliative care and no notable changes in the percentage of palliative care grants funded across the three major funding institutes, NCI, NINR, and NIA.
What factors might have created these changes?
In our prior study we described multiple barriers to federal funding support for palliative medicine research. Many of the suggested initiatives have been undertaken in the last five years. These approaches include (1) continued private philanthropic foundation support; (2) focus on support to junior investigators; (3) development of collaborative palliative medicine research networks, as exemplified by the National Palliative Care Research Center (www.npcrc.org); and (4) increase in NIH funding for palliative medicine research.
A reflection of the successful efforts to promote palliative medicine research can be seen in the rising impact factors of major palliative medicine journals. The impact factor is a measure reflecting the average number of citations to articles published in science journals. For example, the impact factor for the Journal of Palliative Medicine was 1.909 in 2008 and rose to 2.245 in 2010, an 18% increase.8 Similarly, Palliative Medicine's impact factor,1.874 in 2008, increased to 2.515 in 2010, a 34% increase in two years. In sum, the three major palliative care research journals, Journal of Palliative Medicine, Palliative Medicine, and the Journal of Pain and Symptom Management, all have impact factors ranging from 2.2 for the newest journal to 2.6 for the most mature journal.
Limitations
This study has several limitations that should be noted. First, our study was designed specifically to identify palliative medicine studies and researchers and thus did not include studies in related areas that might have implications for palliative medicine research (e.g., treatments of chemotherapy induced nausea, interventions to improve postoperative pain). These criteria potentially excluded relevant research in related areas. Second, we focused specifically on studies in adult internal medicine, such that we may have underreported funding in pediatrics, psychiatry, surgery, neurology, and anesthesiology. Thirdly, because we identified researchers from published manuscripts, it is possible that we did not identify funding for junior investigators who have not yet published their results. We suspect, however, that the number of such researchers is small. Finally, the decreased number of grants identified in this study, when compared to our prior study, can be partly explained by our more rigorous evaluation of both investigators and grants as relevant to palliative medicine. Specifically, for this study, we utilized a key word search in the NIH RePorter database which allowed for a more targeted search. Because the NIH RePorter database was not available at the time of our prior study of NIH funding from 2001 to 2005, we may have included grants with less relevance to palliative medicine. And therefore we may not have included as many grants with less relevance to palliative medicine.
Conclusions
In conclusion, despite increasing number of authors with NIH funded grants, when compared to our findings from 2001 to 2005, the overall number of grants in the field of palliative medicine remains low, and in turn, federal funding for palliative medicine research remains inadequate. Critically needed are focused efforts to ensure the development of an appropriate evidence base for palliative medicine. These efforts should included staffing relevant NIH study sections with permanent members with appropriate expertise in palliative care, earmarked funds for palliative research across major NIH institutes, and ongoing and increased investments by private foundations to support pilot work and junior and career development awards for junior and midcareer researchers to continue the development of the needed critical mass of palliative care researchers.
Acknowledgments and Funding Support
Dr. Gelfman was supported by a T32 (T32HP10262), a National Palliative Care Research Center (NPCRC) Junior Faculty Career Development Award, an R03 (R03 AG042344-01), and Mount Sinai School of Medicine's Older American Independence Center (1P30AG28741-01) Research Career Development Core support. Dr. Morrison is the recipient of a Mid-Career Investigator Award in Patient-Oriented Research from the National Institute on Aging (K24 AG022345).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Gelfman LP. Morrison RS. Research funding for palliative medicine. J Palliat Med. 2008;11:36–43. doi: 10.1089/jpm.2006.0231. [DOI] [PubMed] [Google Scholar]
- 2.Research Porfolio Online Reporting Tools (RePORT): projectreporter.nih.gov/reporter.cfm . [Jul 11;2012 ].
- 3.Morrison RS. Maroney-Galin C. Kralovec PD. Meier DE. The growth of palliative care programs in United States hospitals. J Palliat Med. 2005;8(6):1127–1134. doi: 10.1089/jpm.2005.8.1127. [DOI] [PubMed] [Google Scholar]
- 4.Society AC. RFA: Pilot and Exploratory Projects in Palliative Care of Cancer Patients and Their Families. 2012. www.cancer.org/Research/ResearchProgramsFunding/FundingOpportunities/IndexofGrants/NewInitiatives/rfa-pilot-and-exploratory-projects-in-palliative-care-of-cancer-patients-and-their-families. [Jul 11;2012 ]. www.cancer.org/Research/ResearchProgramsFunding/FundingOpportunities/IndexofGrants/NewInitiatives/rfa-pilot-and-exploratory-projects-in-palliative-care-of-cancer-patients-and-their-families
- 5.Research NIoN: Palliative Care Brochure. www.ninr.nih.gov/NewsAndInformation/NINRPublications/Palliative+Care+Brochure. [Jul 11;2012 ]. www.ninr.nih.gov/NewsAndInformation/NINRPublications/Palliative+Care+Brochure
- 6.Health NIo: ExPORTER. exporter.nih.gov/ [Aug;2012 ]. exporter.nih.gov/
- 7.New York: 2004. National Consensus Project for Quality Palliative Care: Clinical Practice Researchers Guidelines for Quality Palliative Care. [DOI] [PubMed] [Google Scholar]
- 8.San-Miguel MT. Centeno C. Carvajal A. Ponz M. In which journals do active researchers of palliative care publish their articles? J Palliat Med. 2011;14(1):4–5. doi: 10.1089/jpm.2010.0310. [DOI] [PubMed] [Google Scholar]