Abstract
Patient-centered care requires pediatricians to address parents’ health concerns, but their willingness to solicit parental concerns may be limited by uncertainty about which topics will be raised. We conducted surveys of parents to identify current health-related issues of concern.
Methods
Participants rated 30 items as health problems for children in their community (large, medium, small, or no problem) and volunteered concerns for their own children.
Results
1,119 parents completed the survey. Allergies (69%), lack of exercise (68%), asthma (65%), attention deficit hyperactivity disorder (65%), Internet safety (63%), obesity (59%), smoking (58%), and bullying (57%) were identified as important problems (large or medium), with variation among demographic subgroups. Concerns for their own children included healthy nutrition, obesity, and lack of exercise, healthy growth and development, safety and injury prevention, and mental health issues.
Conclusion
Parents’ health concerns for children are varied and may differ from those routinely addressed during well-child care.
Keywords: Health needs assessment, practice-based research network, well-child care
INTRODUCTION
Parents regard their pediatrician as a trusted source of health information and rely on them to provide advice on raising children.1, 2 Health information and advice is often provided within the context of well childcare, a cornerstone of pediatric care. Topics selected for discussion at a well-child visit are guided by the Bright Futures Guidelines for health supervision visits published by the American Academy of Pediatrics (AAP).3 The list of potential topics has lengthened over time and is described as “overwhelming” by community pediatricians.4, 5 In addition to traditional topics like healthy growth and development and prevention of injuries, pediatricians are asked to address “new morbidities” such as obesity, behavior disorders, depression, adolescent risky behaviors, and violence.6, 7 Gaps between what is recommended to be included in well-child care and what parents report is provided have been identified with over half of parents reporting one or more unmet need for guidance or education.8
Parents often have concerns about psychosocial issues but are unlikely to raise them during the office visit.2, 9, 10 Recognizing this, the Bright Futures Guidelines promote solicitation of parental concerns at every well-child visit to keep the visit patient-centered.3, 11 This more tailored approach to well-child care is supported by pediatricians, although it creates a tension between addressing parents’ concerns and covering the recommended visit content.5 Implementation of this approach to care requires a change from the more traditional visit format that is still encouraged by the templates included in electronic medical records where the pediatrician determines the topics for discussion and asks most of the questions.10.
Practitioners’ willingness to ask open-ended questions to solicit parental concerns as well as their ability to provide effective management may be limited by their uncertainty about which topics are likely to be raised by the parent, their concern they may not have the knowledge to adequately respond, and a paucity of research evidence to guide care.10, 12, 13 Knowledge of common parental concerns could guide implementation of patient-centered care. We conducted surveys of parents to identify current health-related issues of concern in our community. Our goal was to alert local pediatricians about common parental concerns so they could be prepared to address them.
METHODS
We developed and implemented a survey to assess parents’ health concerns for children and adolescents in their community and parents’ concerns for their own children. The study was approved by the Washington University Human Research Protection Office.
Survey Tools
The survey was developed by the authors, based in part on the University of Michigan C. S. Mott Children’s Hospital National Poll on Children’s Health (http://www.med.umich.edu/mott/npch/about/index.htm). This web-based survey measures national opinion and priorities regarding major healthcare issues and trends for U.S. children using a representative national sample of about 2,000 U.S. households.
We modified this 20-item instrument (with permission) to reflect local concerns, adding 10 items to the list of possible health problems nominated by local experts and community pediatricians after reviewing the original survey. These included allergies (including food allergies), diabetes, HIV/AIDS, lead poisoning, marijuana use, overuse of antibiotics, poverty, risks associated with immunization shots, sport- and play-related injuries, and swine flu. We also modified the wording of 8 items for clarity: environmental pollution, heavy drinking of alcohol, illegal drug use, lack of exercise, motor vehicle accidents, neighborhood safety (including assaults and homicides), obesity, sexually transmitted infections other than HIV/AIDs (Chlamydia, gonorrhea, etc.). Respondents used a 4-point categorical scale to indicate how much of a problem (large, medium, small, or not a problem) they felt each item on the 30-item list was for children and adolescents in their community. Items rated as a large or medium problem were considered an important problem.
In addition, parents identified the top three health concerns for their own children by age group (<2 years old, 2 to 5 years old, 6–11 years old, 12 to 17 years old) by responding to an open-ended question (e.g., What are the top three health concerns for your own children under 2 years old?). The final parent survey had a reading level of 6.3.
The survey also collected demographic information and was paper-based, self-administered, anonymous, and took about 10 minutes to complete.
Study Participants
Parents (or legal guardians) attending the office of a pediatrician in our practice-based research network (PBRN), Washington University Pediatric and Adolescent Ambulatory Research Consortium (WU PAARC) when a research assistant (RA) was present were eligible to participate in the study. Parents were approached by the RA in the waiting room and invited to participate. Parents were not approached if they were immediately called to see the physician, were preoccupied with an administrative task, or if the RA was busy with another parent. Unaccompanied minors and pregnant women with no children were ineligible as were parents who could not speak English or had previously completed the survey. Most parents finished the survey prior to seeing the physician. Of 31 participants who did not have enough time to complete the survey in the office, 13 returned the completed survey in the provided stamped, addressed envelope.
Statistical Analysis
Descriptive statistics are reported for respondents and for demographic subgroups, defined after comparing the distribution of responses. These groups included African American vs. all other races; Medicaid vs. work-related insurance; less than a bachelors degree vs. a bachelors degree or higher educational attainment; and family income < $60,000/year vs. ≥ $60,000/year. Meaningful differences in important problems between subgroups were defined as differences of at least 20%. Parents response to the open ended questions were coded by two of the authors (EL and JG). Potential categories were identified from review of the survey responses and the Bright Futures Guidelines. Nine discrete categories were identified and parents’ responses were coded by consensus. The categories included: mental health (eg, self esteem, behavioral problems, bullying, depression, suicide); food/activity (eg, healthy nutrition, obesity, eating disorders, lack of exercise); environment (eg, environmental pollution, lead, food safety, poverty); risky behaviors (eg, alcohol, smoking, illicit drug use, STDs, teen pregnancy); safety (eg, accidents, car and pedestrian safety, sport-related injuries, neighborhood safety, internet safety); development (eg, normal growth and development, social health, healthy sexuality); parenting (eg, sleep problems, education); oral health (eg, thumb sucking, oral hygiene) and diseases (all diseases mentioned specifically eg, acute infectious diseases, allergies, asthma, ADHD). Summary statistics are presented as means and standard deviations or medians and ranges for continuous variables, and percentages for categorical variables. We used the Pearson Chi-square or Fisher’s exact test to compare responses among subgroups. A probability of p < 0.05 (two-tailed) was used to establish statistical significance. All statistical analyses were done using SAS 9.2 (SAS Institute Inc., Cary N.C.)
RESULTS
Study Participants
In-office recruitment for the parent survey occurred in 12 practices (Figure 1). The RA was at each practice for a median of 3.9 days (range 3.5–4.5 days) from June 8, 2009 to September 4, 2009. Of 1,278 eligible parents, 1,119 (88%) completed the survey with a median of 93 surveys completed at each practice (range: 40 to 170). Respondents were from throughout the St. Louis metropolitan area: 85% were the child’s mother, 24% were African American, 60% had a college degree or higher, and 22% used Medicaid insurance for their child (Table 1). The non-completion rate for each item in the survey ranged from 2% to 6% (median 4%).
Figure 1.
Subject recruitment.
Table 1.
Characteristics of the 1,119 study participants*
| Characteristic | % |
|---|---|
|
| |
| Female gender (n=1,077) | 88% |
| Racial group (n=1,052) | |
| White | 72% |
| Black | 24% |
| Asian | 2% |
| Other | 2% |
| Hispanic (n=1,056) | 2% |
| Educational level (n=1,074) | |
| Grades 1 through 8 | 0.4% |
| High school, no diploma | 4% |
| High school graduate or GED | 14% |
| College – no degree | 20% |
| Associates degree or equivalent | 10% |
| Bachelors degree | 29% |
| Post graduate or professional degree | 21% |
| Health insurance (n=1,056) | |
| Work-related insurance | 72% |
| Medicaid | 22% |
| Self-pay | 4% |
| Other | 2% |
| Two-parent family (n=1,074) | 79% |
| Family income/year (n=996) | |
| < $30,000 | 20% |
| $30,000 – < $60,000 | 21% |
| $60,000 to < $100,000 | 26% |
| $100,000 or more | 33% |
When data are missing, n is provided.
Percentages may not sum to 100% due to rounding
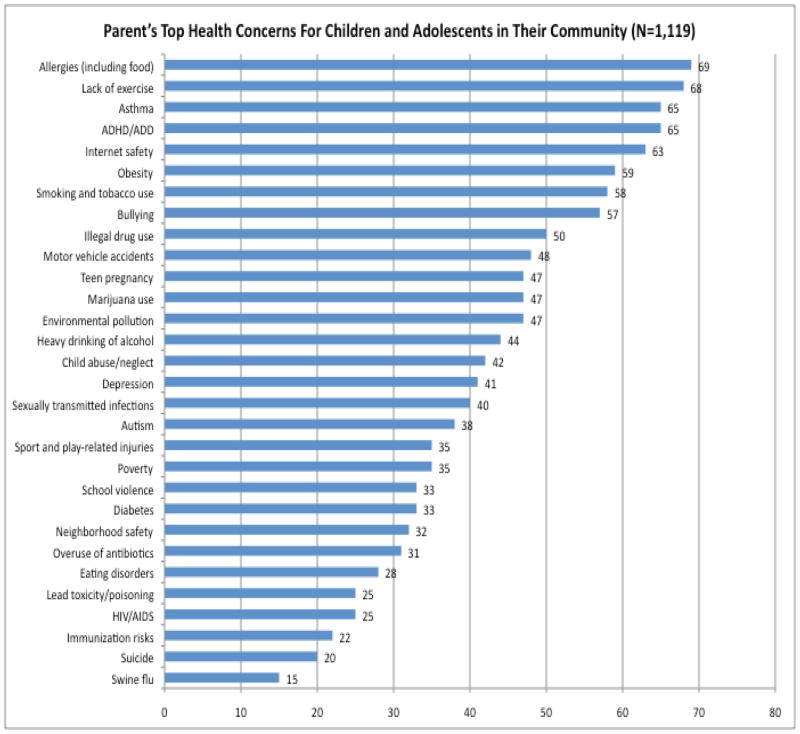
Health problems identified for children and adolescents in the community
Parents’ assessment of the magnitude of 30 health problems for children and adolescents in the community where they lived is presented in Figure 2 and Appendix A. Items identified as important problems (those most frequently identified as a large or medium problem) were: allergies (69%), lack of exercise (68%), asthma (65%), attention deficit hyperactivity disorder (ADHD) (65%), internet safety (63%), obesity (59%), smoking and tobacco use (58%), and bullying (57%).
Figure 2.
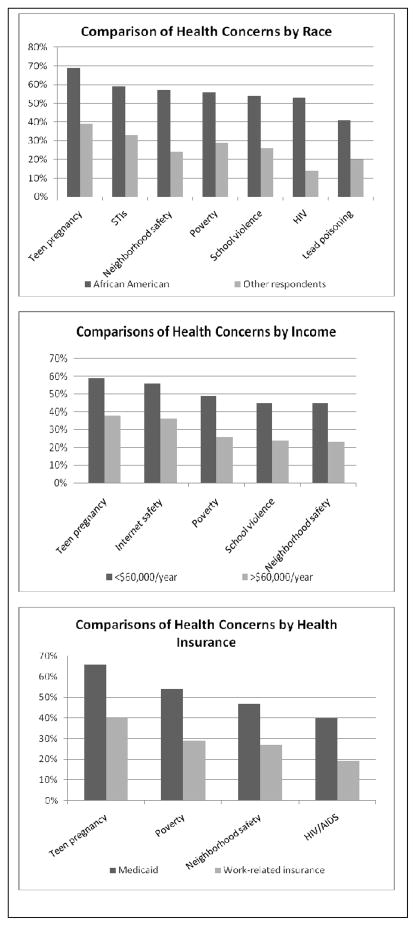
Demographic subgroups varied considerably in the frequency that an item was selected as an important problem (Figure 3). In the univariate analyses, there was > 20% difference between the following subgroup comparisons (all p<0.001); African American parents were more likely than other parents to identify HIV, neighborhood safety, teen pregnancy, school violence, poverty, sexually transmitted infections (other than HIV), and lead poisoning; Parents earning < $60,000/year were more likely than other parents to identify poverty, neighborhood safety, school violence, internet safety, and teen pregnancy; Parents using Medicaid insurance for their child were more likely than other parents to identify teen pregnancy, poverty, HIV/AIDS, and neighborhood safety.
Figure 3.
Comparison of important health concerns by sociodemographic factors
Health concerns for their own children
Parents’ health concerns for their own children varied considerably by age group (Table 2). Across all age groups many parents had concerns for their child’s mental health, healthy nutrition, healthy growth and development, and safety. Many parents were also concerned about specific diseases, most often allergies, asthma, acute infectious diseases and ADHD. Concerns about mental health increased with the child’s age. Parents of 2 to 5 year olds were concerned about behavior problems (2.9%), parents of 6 to 11 year olds concerned about bullying (10%), and parents of 12 to 17 year olds concerned about depression (10.7%). The frequency of parental concern about obesity and lack of exercise increased across the age groups, whereas more parents of young children were concerned about environmental pollution. Few parents identified Internet safety as a concern (4.6% of parents of 5 to 11 year olds, and 6.0% of 11 to 17 year olds), and few parents were concerned about risky behaviors in their adolescent children (13.7% illicit drug use, 11.8% alcohol use, 6% STDs, 4.9% teen pregnancy, 3.2% tobacco use).
Table 2.
Most frequently selected health concerns parents reported for their own children by age group.*
| Parental Concerns | < 2 Years (n=452) | 2 to 5 years (n=518) | 6 to 11 years (n=589) | 12 to 17 years (n=533) |
|---|---|---|---|---|
| Diseases | 99.8% | 86.7% acute | 81.5% | 42.8% |
| Most commonly named diseases (% all parents in agegroup) | Acute infectious diseases (23%) | Allergies (26%) | Allergies (22%) | Allergies (9%) |
| Allergies (22%) | Asthma (19%) | Asthma (15%) | Asthma (8%) | |
| Asthma (15%) | Acute infectious diseases (13%) | ADHD (14%) | ADHD (6%) | |
| Mental health | 2.7% | 9.8% | 23.6% | 23.8% |
| Food/activity | 14.2% | 23.0% | 34.8% | 37.7% |
| Healthy nutrition | 11.1% | 13.3% | 13.1% | 11.4% |
| Obesity | 2.4% | 6.0% | 11.5% | 13.1% |
| Lack of exercise | 0.7% | 3.7% | 9.2% | 10.7% |
| Environment | 9.3% | 5.6% | 3.1% | 2.3% |
| Risky behaviors | 0 | 0 | 3.8% | 44.3% |
| Safety | 13.1% | 19.1% | 22.4% | 33.6% |
| Development | 13.3% | 10.2% | 7.8% | 12.0% |
| Parenting | 3.8% | 3.1% | 2.4% | 3% |
| Oral health | 1.8% | 1.7% | 0.8% | 0.8% |
Abbreviations: ADHD Attention deficit hyperactivity disorder
Parents could provide up to 3 responses
DISCUSSION
We asked almost 1,200 parents from various demographic groups about their health concerns for children. We found considerable variation for the items parents identified as important health problems for children in their community and as concerns for their own children. These findings support the need for health care providers to ask each parent to identify their specific concerns in order to promote a more patient-centered approach to well child care.3 Although strongly recommended in the Bright Futures Guidelines, a recent study found clinicians did not ask open-ended questions to solicit parental concerns in almost 25% of well-child visits.14 Expanding the scope of the well child visit with a more patient-centered approach may improve the effectiveness and efficiency of these visits.14, 15
Parents are more likely to follow advice from their pediatrician than advice from other sources.1, 16 In order to provide the most relevant and helpful advice, pediatricians must both be aware of parents’ concerns and be prepared to address them. Our findings suggest that pediatricians need to be prepared to adequately address psychosocial concerns that reflect recent social and environmental changes such as obesity, lack of physical exercise, depression, violence and Internet safety,17 problems identified as significant causes of morbidity by many parents in this study. Although they are common, psychosocial concerns are unlikely to be raised by the parent during an office visit,2, 9, 18 and are less likely than traditional topics to be raised by the pediatrician especially if time is short.10, 14, 17, 19 A parent questionnaire could be used to alert parents that their pediatrician can provide help with psychosocial issues, and to identify any issues that are a particular concern,3 but pediatricians may need additional education and an established referral process to feel comfortable dealing with behavioral, developmental or psychological issues.19
Our findings also suggest that parents may fail to identify significant health risks for their own children. Some items commonly identified as an important problem for children in the community were not reported as concerns for their own children. For example, there was a six-fold decrease in the frequency that parents identified Internet safety and lack of physical exercise as a concern for their children compared to being a concern for children in the community. A detailed enquiry by the pediatrician may be needed to ascertain if physical activity is adequate and Internet access is being monitored. Similarly, there was a three-fold decrease in the frequency that parents identified risky behaviors such as alcohol, tobacco and drug use and unsafe sexual activity as concerns for their own adolescent children compared with being a concern for adolescents in their community. Pediatricians could help parents to guide their teen to make healthy choices by raising these issues for discussion at an earlier age, but may need additional training to enhance their comfort and effectiveness for discussing these issues with parents and adolescent patients.20–22
Items identified as important problems for children in the community may represent unmet need and opportunities to improve care. The significant morbidity associated with asthma and allergies identified as important problems by parents in this study could be reduced by increased use of effective, safe treatments that are readily available.23 Establishing a therapeutic partnership by inviting parents to share their specific concerns is a strategy supported by national guidelines and by community pediatricians5 and may increase treatment effectiveness. Meeting the needs of disadvantaged families may be more difficult for providers. Mothers from disadvantaged groups in this study identified neighborhood safety and violence at school as important problems for children in their community. Language barriers, low health literacy, and problems with provider-patient communication may make it difficult for these mothers to raise their concerns with the provider.24 Providers too may be reluctant to raise these issues due to lack of training and time pressures.25 Although pediatricians cannot alleviate these problems, they could enlist the help of community agencies to provide needed services and advocate for safe environments for their patients.7, 26
Limitations
Limitations to our findings must be noted. While the practices used for the survey represented all socio-demographic groups in the St Louis area, the concerns identified in this survey may still be local. For example, the prevalence of asthma and allergy is high in the St. Louis area.27 Findings may also have been influenced by the seasonality of the survey (the summer months). However, our survey could easily be replicated to identify local concerns.
CONCLUSION
Concerns and problems identified by parents may differ from those routinely addressed at well child visits. Health problems and concerns for children identified by parents are varied and are likely to change over time, influenced by social changes, the emergence of new health threats, and the media. Variations in parents’ concerns support the need for the health care provider to ask the parent to identify their specific concerns during each visit. Identifying common parental concerns can inform the primary care provider about topics they need to be prepared to discuss at well child visits and identify issues that may need a more detailed enquiry. Common concerns may reflect unmet needs and help to guide development of targeted interventions and policies to improve health.
What’s New.
Parents’ health concerns for children are varied and reflect some contemporary issues such as obesity, Internet safety, and bullying. Parents’ concerns may differ from those of their pediatrician and issues routinely addressed in well child visits.
Acknowledgments
We thank all of the health care providers and parents at the following practices who participated in our study: Children’s Clinic, Crystal City Pediatrics, Esse Health – Creve Coeur, Esse Health – Florissant, Esse Health – Watson, Fenton Pediatrics, Forest Park Pediatrics, Health Care for Kids, Robert H. Strashun, M.D., Tots Thru Teens Pediatrics, Southwest Pediatrics, and St. Louis Pediatric Practitioners
We would also like to thank the staff of the C.S. Mott Children’s Hospital National Poll on Children’s Health for sharing their original survey instrument.
ABBREVIATIONS
- AAP
American Academy of Pediatrics
- ADHD
Attention deficit hyperactivity disorder
- AIDS
Acquired immune deficiency syndrome
- HIV
Human immunodeficiency virus
- NCRR
National Center for Research Resources
- NIH
National Institutes of Health
- PBRN
Practice based research network
- RA
Research assistant
- SD
Standard deviation
- STD
Sexually Transmitted Disease
- WU PAARC
Washington University Pediatric and Adolescent Ambulatory Research Consortium
APPENDIX A
Parents’ assessment of the magnitude of the problems caused by various health issues for children and adolescents in their community (n=1119).
| Important problem (large and medium) | Large problem | Medium problem | Small problem | Not a problem | N | |
|---|---|---|---|---|---|---|
| Allergies (including food allergies) | 69% | 31% | 38% | 20% | 11% | 1100 |
| Lack of exercise | 68% | 35% | 33% | 18% | 14% | 1091 |
| Asthma | 65% | 31% | 34% | 21% | 14% | 1093 |
| ADHD | 65% | 28% | 36% | 19% | 17% | 1086 |
| Internet safety | 63% | 29% | 34% | 22% | 15% | 1081 |
| Obesity | 59% | 28% | 31% | 23% | 18% | 1088 |
| Smoking/tobacco use | 58% | 28% | 30% | 26% | 17% | 1087 |
| Bullying | 57% | 26% | 31% | 25% | 18% | 1079 |
| Illegal drug use | 49% | 21% | 28% | 27% | 24% | 1078 |
| Motor vehicle accidents | 48% | 16% | 32% | 34% | 18% | 1070 |
| Environmental pollution | 47% | 20% | 27% | 31% | 22% | 1080 |
| Teen pregnancy | 47% | 21% | 26% | 30% | 23% | 1076 |
| Marijuana use | 47% | 23% | 24% | 29% | 24% | 1067 |
| Heavy drinking of alcohol | 45% | 17% | 28% | 28% | 28% | 1082 |
| Child abuse and neglect | 43% | 19% | 24% | 29% | 29% | 1078 |
| Depression | 41% | 15% | 26% | 33% | 26% | 1073 |
| STDs other than HIV/AIDs (Chlamydia, gonorrhea, etc.) | 40% | 19% | 21% | 30% | 30% | 1059 |
| Autism | 38% | 13% | 25% | 35% | 27% | 1076 |
| Poverty | 36% | 17% | 19% | 33% | 32% | 1060 |
| Sport/play-related injuries | 35% | 8% | 27% | 44% | 22% | 1066 |
| Diabetes | 33% | 12% | 21% | 37% | 30% | 1070 |
| School violence | 33% | 12% | 21% | 38% | 29% | 1077 |
| Neighborhood safety (including assaults and homicides) | 32% | 15% | 17% | 34% | 34% | 1085 |
| Overuse of antibiotics | 31% | 10% | 21% | 33% | 36% | 1048 |
| Eating disorders (like anorexia and bulimia) | 28% | 9% | 19% | 38% | 35% | 1065 |
| Lead toxicity/poisoning | 25% | 9% | 16% | 35% | 40% | 1066 |
| HIV/AIDS | 25% | 13% | 12% | 34% | 42% | 1063 |
| Risks associated with immunization shots | 21% | 6% | 15% | 35% | 44% | 1069 |
| Suicide | 21% | 7% | 14% | 39% | 40% | 1062 |
| Swine flu | 15% | 5% | 10% | 35% | 51% | 1069 |
Percentages may not sum to 100% due to rounding.
ADHD, Attention deficit hyperactivity disorder; STD, sexually transmitted disease; HIV, Human immunodeficiency virus; AIDS, Acquired immune deficiency syndrome.
Footnotes
Conflict of Interest: This publication was made possible by Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the author and do not necessarily represent the official view of NCRR or NIH. The sponsors had no involvement in study design, collection, analysis, interpretation of the data, the writing of the report or the decision to submit the paper for publication.
References
- 1.Moseley KL, Freed GL, Goold SD. Which sources of child health advice do parents follow? Clin Pediatr (Phila) 2011 Jan;50(1):50–56. doi: 10.1177/0009922810379905. [DOI] [PubMed] [Google Scholar]
- 2.Young KT, Davis K, Schoen C, Parker S. Listening to parents. A national survey of parents with young children. Arch Pediatr Adolesc Med. 1998 Mar;152(3):255–262. [PubMed] [Google Scholar]
- 3.Bright Futures: Guidelines for Health Supervision for Infants, Children, and Adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 4.Belamarich PF, Gandica R, Stein RE, Racine AD. Drowning in a sea of advice: pediatricians and American Academy of Pediatrics policy statements. Pediatrics. 2006 Oct;118(4):e964–978. doi: 10.1542/peds.2006-0652. [DOI] [PubMed] [Google Scholar]
- 5.Tanner JL, Stein MT, Olson LM, Frintner MP, Radecki L. Reflections on well-child care practice: a national study of pediatric clinicians. Pediatrics. 2009 Sep;124(3):849–857. doi: 10.1542/peds.2008-2351. [DOI] [PubMed] [Google Scholar]
- 6.Kelleher KJ, McInerny TK, Gardner WP, Childs GE, Wasserman RC. Increasing identification of psychosocial problems: 1979–1996. Pediatrics. 2000 Jun;105(6):1313–1321. doi: 10.1542/peds.105.6.1313. [DOI] [PubMed] [Google Scholar]
- 7.Satcher D, Kaczorowski J, Topa D. The expanding role of the pediatrician in improving child health in the 21st century. Pediatrics. 2005 Apr;115(4 Suppl):1124–1128. doi: 10.1542/peds.2004-2825C. [DOI] [PubMed] [Google Scholar]
- 8.Bethell C, Reuland CH, Halfon N, Schor EL. Measuring the quality of preventive and developmental services for young children: national estimates and patterns of clinicians’ performance. Pediatrics. 2004 Jun;113(6 Suppl):1973–1983. [PubMed] [Google Scholar]
- 9.Hickson GB, Altemeier WA, O’Connor S. Concerns of mothers seeking care in private pediatric offices: opportunities for expanding services. Pediatrics. 1983 Nov;72(5):619–624. [PubMed] [Google Scholar]
- 10.Cheng TL, DeWitt TG, Savageau JA, O’Connor KG. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999 Jun;153(6):629–635. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 11.Glascoe FP, Dworkin PH. The role of parents in the detection of developmental and behavioral problems. Pediatrics. 1995 Jun;95(6):829–836. [PubMed] [Google Scholar]
- 12.Bethell C, Peck C, Schor E. Assessing health system provision of well-child care: The Promoting Healthy Development Survey. Pediatrics. 2001 May;107(5):1084–1094. doi: 10.1542/peds.107.5.1084. [DOI] [PubMed] [Google Scholar]
- 13.Moyer VA, Butler M. Gaps in the evidence for well-child care: a challenge to our profession. Pediatrics. 2004 Dec;114(6):1511–1521. doi: 10.1542/peds.2004-1076. [DOI] [PubMed] [Google Scholar]
- 14.Norlin C, Crawford MA, Bell CT, Sheng X, Stein MT. Delivery of well-child care: a look inside the door. Acad Pediatr. 2011 Jan-Feb;11(1):18–26. doi: 10.1016/j.acap.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Barkin SL, Scheindlin B, Brown C, Ip E, Finch S, Wasserman RC. Anticipatory guidance topics: are more better? Ambul Pediatr. 2005 Nov-Dec;5(6):372–376. doi: 10.1367/A04-2131R1.1. [DOI] [PubMed] [Google Scholar]
- 16.D’Alessandro DM, Kreiter CD, Kinzer SL, Peterson MW. A randomized controlled trial of an information prescription for pediatric patient education on the Internet. Arch Pediatr Adolesc Med. 2004 Sep;158(9):857–862. doi: 10.1001/archpedi.158.9.857. [DOI] [PubMed] [Google Scholar]
- 17.Halfon N, Stevens GD, Larson K, Olson LM. Duration of a well-child visit: association with content, family-centeredness, and satisfaction. Pediatrics. 2011 Oct;128(4):657–664. doi: 10.1542/peds.2011-0586. [DOI] [PubMed] [Google Scholar]
- 18.Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. 1. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968 Nov;42(5):855–871. [PubMed] [Google Scholar]
- 19.Committee on Psychosocial Aspects of C Family H American Academy of Pediatrics. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Committee on Psychosocial Aspects of Child and Family Health. Pediatrics. 2001 Nov;108(5):1227–1230. doi: 10.1542/peds.108.5.1227. [DOI] [PubMed] [Google Scholar]
- 20.Lafferty WE, Downey L, Holan CM, et al. Provision of sexual health services to adolescent enrollees in Medicaid managed care. Am J Public Health. 2002 Nov;92(11):1779–1783. doi: 10.2105/ajph.92.11.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Millstein SG, Marcell AV. Screening and counseling for adolescent alcohol use among primary care physicians in the United States. Pediatrics. 2003 Jan;111(1):114–122. doi: 10.1542/peds.111.1.114. [DOI] [PubMed] [Google Scholar]
- 22.Tanski SE, Klein JD, Winickoff JP, Auinger P, Weitzman M. Tobacco counseling at well-child and tobacco-influenced illness visits: opportunities for improvement. Pediatrics. 2003 Feb;111(2):E162–167. doi: 10.1542/peds.111.2.e162. [DOI] [PubMed] [Google Scholar]
- 23.National Institutes of Health. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007 Nov;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 24.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999 Aug 11;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 25.Erickson MJ, Hill TD, Siegel RM. Barriers to domestic violence screening in the pediatric setting. Pediatrics. 2001 Jul;108(1):98–102. doi: 10.1542/peds.108.1.98. [DOI] [PubMed] [Google Scholar]
- 26.Schor EL. Rethinking well-child care. Pediatrics. 2004 Jul;114(1):210–216. doi: 10.1542/peds.114.1.210. [DOI] [PubMed] [Google Scholar]
- 27.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. Natl Health Stat Report. 2011 Jan 12;(32):1–14. [PubMed] [Google Scholar]