Abstract
Concern over consistency and completeness of surgical site infection (SSI) surveillance has increased due to public reporting of hospital SSI rates and imminent non-payment rules for hospitals that do not meet national benchmarks. 1 Already, hospitals no longer receive additional payment from the Centers for Medicare & Medicaid Services (CMS) for certain infections following coronary artery bypass graft (CABG) surgery, orthopedic procedures, and bariatric surgery.2
One major concern is incomplete and differential post-discharge surveillance. At present, substantial variation exists in how and whether hospitals identify SSI events after the hospitalization in which the surgery occurred. Parameters used for SSI surveillance such as the duration of the window of time that surveillance takes place following the surgical procedure can impact the completeness of surveillance data. Determination of the optimal surveillance time period involves balancing the potential increased case ascertainment associated with a longer follow-up period with the increased resources that would be required. Currently, the time window for identifying potentially preventable SSIs related to events at the time of surgery is not fully standardized. The Centers for Disease Control and Prevention (CDC) National Healthcare Surveillance Network (NHSN) requires a 365-day postoperative surveillance period for procedures involving implants and a 30-day period for non-implant procedures. 3 In contrast, the National Surgical Quality Improvement Program (NSQIP) and the Society of Thoracic Surgeons (STS) systems employ 30-day post-operative surveillance regardless of implant. As consensus builds towards national quality measures for hospital-specific SSI rates, it will be important to assess the frequency of events beyond the 30-day post-surgical window that may quantify the value of various durations of surveillance, and ultimately inform the choice of specific outcome measures.
We evaluated the fraction of deep and organ/space SSIs detected beyond 30 days following CABG, orthopedic procedures, and mastectomy with implant surgical procedures to inform whether a longer SSI surveillance time period identifies sufficient additional SSI cases to warrant additional surveillance resources.
SSIs were identified as part of retrospective cohort studies at five hospitals following total hip replacements (THRs) and total knee replacements (TKRs) performed from January 1, 2007 – December 31, 2007.4 SSIs with onset of infection within 365 days of surgery were identified by: a) routine surveillance by hospital infection prevention programs, which was not standardized and commonly involved a combination of review of microbiology records and evaluation of readmissions or reoperations that came to attention, and b) cases flagged by a previously-validated algorithm involving antibiotic data, administrative diagnostic codes, and readmission criteria.5
Previously-identified post-CABG SSIs were identified from a 2005 retrospective cohort study of Medicare beneficiaries undergoing CABG in US hospitals ranked in the top and bottom deciles based upon case mix–adjusted probabilities of an SSI-related claim code within 60 days of surgery. The Romano score was used for case mix adjustment, and was demonstrated as a significant predictor of SSI. 6 Randomly selected medical records were reviewed for SSI.
Lastly, we evaluated previously identified SSI cases following mastectomy procedures involving implantation of prosthetic material from an academic medical center (August 2005–December 2007). Data were collected from the surgical admission, readmissions and clinic visits within one year of surgery. 7
All SSIs were limited to those involving deep incisional (DI) or organ/space (OS) infections. Time from surgery to SSI onset was calculated for all SSIs and grouped into ≤30 days and 31–60 days for CABG, while TKR, THR and mastectomy procedures included additional groupings of 61–90 days, and 91–365 days.
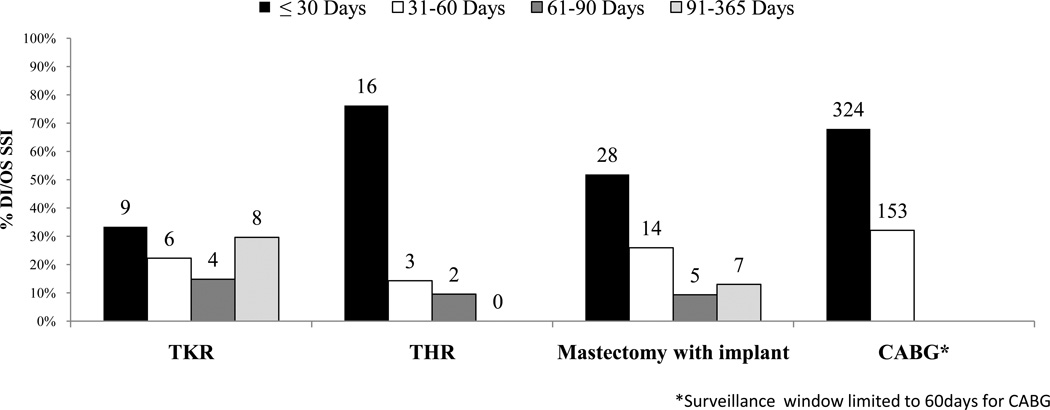
We identified 27 SSIs following 1,666 TKRs, 21 SSIs following 1,691 THRs, 477 SSI following 23,376 CABGs, and 54 SSIs following 327 mastectomies with implants (Figure 1). Based upon these identified SSIs, TKR required 60 days to identify the majority of cases.8 By 90 days post-procedure, 100% of known DI/OS SSIs were identified for THR, 70% of DI/OS SSIs for TKR, and 87% of DI/OS SSIs for mastectomy with implants. Limiting post-operative SSI surveillance to 30-days would lead to under-reporting of approximately one quarter to two thirds of DI/OS SSIs across the four procedures surveyed. Confining post-operative SSI surveillance to 60 days, as was done for all CABG procedures, results in detection of the vast majority of DI/OS SSIs following THR and mastectomy-plus-implant procedures, but only half of DI/OS SSIs following TKR. In contrast, a 90-day window detected most DI/OS SSIs across these three procedures. A limitation of all SSI estimates across THR, TKR and mastectomy-plus-implant procedures was that follow-up was confined to the hospital where the index procedure was performed. Therefore, results represent minimum estimates of infection since post-discharge outpatient events and SSIs identified at other hospitals were not captured. In contrast, the use of insurer claims to identify CABG SSIs regardless of the location of medical care would allow for more confidence that all medically attended DI/OS infections were captured.6
Figure 1.
Distribution of time to onset of Deep-incisional (DI) and Organ space (OS) surgical site infections (SSIs) following total knee replacement (TKR), total hip replacement (THR), mastectomy with implant reconstruction, and coronary artery bypass grafting (CABG) surgeries. Duration of post-procedure follow-up for DI/OS SSI was 365 days for TKR, THR and Mastectomy with implant, and 60 days for CABG.
Impending CMS SSI surveillance measures for mandatory reporting should consider including DI/OS SSI surveillance periods for TKR, THR, CABG and mastectomy-plus-implant procedures beyond 30 days. Nevertheless, additional research is needed to assess whether resources to extend surveillance out to 365 days post-procedures is prudent given limited resources, the fact that most DI/OS SSIs are captured within 90 days, and the uncertainty whether SSIs occurring that long after surgery are in fact due to preventable issues at the time of the operation.
Regardless of which duration of post-discharge surveillance is selected, assurance that hospitals are conducting post-discharge surveillance using standardized methods is necessary for inter-hospital comparison. Training and validation to ensure similarly comprehensive SSI capture across hospitals is critical for valid public reporting used to determine Medicare payment. In addition, comparison and improvement of existing case mix adjustors should be performed to properly account for different patient population risks for SSI. Early successful explorations into the use of large networks of claims-based databases appear promising in this regard since both case mix adjustment and claims-based algorithms to trigger chart review have been shown to be superior to routine surveillance performed by hospital infection prevention programs for SSI detection and can be used to standardize post-discharge SSI surveillance. 6, 9, 10
Acknowledgments
This study was funded by the CDC Prevention Epicenters Programs U01CI000344 (Platt) and U01CI0000333 (Fraser), and National Institutes of Health career development awards to MAO (K01AI065808) and VJF (K24AI067794).
Footnotes
All authors report no conflicts of interest relevant to this article.
References
- 1.Rosenthal MB. Nonpayment for performance? Medicare's new reimbursement rule. N Engl J Med. 2007 Oct 18;357(16):1573–1575. doi: 10.1056/NEJMp078184. [DOI] [PubMed] [Google Scholar]
- 2.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2008 rates. Fed Regist. 2007 Aug 22;72(162):47129–48175. [PubMed] [Google Scholar]
- 3.Horan TC, Andrus M, Dudeck M. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Yokoe D. Multicenter Evaluation of Enhanced Methods for Surgical Site Infection Surveillance Following Total Hip and Total Knee Arthroplasty. Presented at the Fifth Decennial International Conference on Healthcare-Associated Infections; April 2010; Atlanta, GA. [Google Scholar]
- 5.Bolon MK, Hooper D, Stevenson KB, et al. Improved surveillance for surgical site infections after orthopedic implantation procedures: extending applications for automated data. Clin Infect Dis. 2009;48:1223–1229. doi: 10.1086/597584. [DOI] [PubMed] [Google Scholar]
- 6.Huang SS, Placzek H, Livingston J, et al. Use of Medicare Claims to Rank Hospitals by Surgical Site Infection Risk following Coronary Artery Bypass Graft Surgery. Infect Control Hosp Epidemiol. 2011;32(8):775–783. doi: 10.1086/660874. [DOI] [PubMed] [Google Scholar]
- 7.Olsen M, Ball K, Fraser V. Risk of Surgical Site Infection due to Chemotherapy and Radiotherapy in Patients Undergoing Mastectomy. Presented at the Fifth Decennial International Conference on Healthcare-Associated Infections; April 2010; Atlanta, GA. [Google Scholar]
- 8.Sohoo NF, Zingmond DS, Lieberman JR, Ko CY. Optimal timeframe for reporting short-term complication rates after total knee arthroplasty. J Arthroplasty. 2006;21(5):705–711. doi: 10.1016/j.arth.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Yokoe DS, Noskin GA, Cunningham SM, et al. Enhanced identification of postoperative infections among inpatients. Emerg Infect Dis. 2004;10(11):1924–1930. doi: 10.3201/eid1011.040572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang SS, Livingston JM, Rawson NS, et al. Developing algorithms for healthcare insurers to systematically monitor surgical site infection rates. BMC Med Res Methodol. 2007;7:20. doi: 10.1186/1471-2288-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]