Abstract
Neutrophilic eccrine hidradenitis (NEH) is a distinctive dermatosis occurring in patients with malignancy or undergoing chemotherapy. This disorder is characterized by a neutrophilic infiltrate around the eccrine glands and secretory coils, and is associated with necrosis. It must be distinguished from infections, drug eruptions, malignancies or other forms of skin diseases. As it is a self-limiting condition, establishing the diagnosis will avoid unnecessary investigations and treatment. Here we report a case of NEH in a 40-year-old woman suspected to be due to carbamazepine.
KEY WORDS: Adverse cutaneous drug reaction, carbamazepine, neutrophilic eccrine hidradenitis
Introduction
Neutrophilic Eccrine Hidradenitis (NEH), first described by Harris et al in 1982,[1] is a self-limiting, reactive neutrophilic dermatosis primarily affecting the eccrine glands and occurs mostly in patients with malignancy or those undergoing chemotherapy. Malignancies associated with NEH include acute myeloid leukemia, acute myelomonocytic leukemia,[2] testicular carcinoma,[3] Hodgkin's and non-Hodgkin's lymphoma, and osteogenic sarcoma. The most commonly implicated drug is cytarabine followed by bleomycin, mitoxantrone, chlorambucil, zidovudine and acetaminophen.[4]
The clinical lesions are typically erythematous plaques, located on the extremities, trunk, face, and palms. A skin biopsy demonstrating typical pathologic changes of the eccrine glands is required to confirm a diagnosis of NEH. Here we describe a patient who developed neutrophilic eccrine hidradenitis (NEH) after receiving carbamazepine, an anti-epileptic drug.
Case Report
A 40-year-old woman was admitted in the medical ward with complaints of fever, puffiness of face, vomiting and skin rash since five days. She was a known case of epilepsy and was taking carbamazepine for the same for the past one month. A provisional diagnosis of carbamazepine syndrome was made and the patient was referred to the dermatology department.
General physical examination showed the patient to be febrile and her vital parameters were within normal limits. No other abnormalities were noted. The dermatological examination showed multiple dry, non scaly, discretely arranged, round to oval, bilaterally near symmetrical papules, nodules, vesicles and pustules over the forearms and hands [Figure 1]. Mild peeling of skin was seen over the abdomen, proximal upper and lower limbs. Mucosa, scalp, nails and genitalia were normal.
Figure 1.

Showing multiple papules, pustules over the forearms
Clinically, the differential diagnosis included toxic epidermal necrolysis, acute febrile neutrophilic dermatosis, bullous pemphigoid and DRESS syndrome. Extensive evaluation found no infectious focus. Complete blood count, biochemical parameters and urine analysis were normal. Nikolsky's sign and pathergy test were negative. Tzanck test was negative. A skin biopsy of the cutaneous lesions over the right forearm was performed. Histological features of the biopsy consisted of a neutrophilic infiltrate surrounding the eccrine glands and sparing the duct. There was a focal interface vacuolar dermatitis. An ill-defined collection of histiocytes, large and pleomorphic, and scattered lymphocytes could be observed within the dermis [Figure 2]. Special stains were negative. Based on the clinical and histological findings, a diagnosis of NEH secondary to carbamazepine was made. Opinion with an oncologist was sought and basic screening for malignancies did not reveal any evidence of malignancy. Oral corticosteroids were initiated in tapering doses. The fever subsided over the next three days and the skin lesions resolved gradually with post-inflammatory hyperpigmentation.
Figure 2.
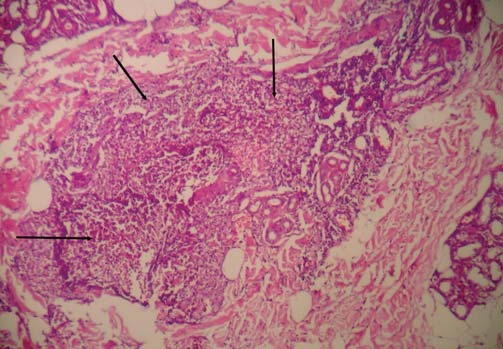
A low-power histopathological photograph showing neutrophilic infiltration (arrow) around eccrine glands with necrosis
In view of the condition starting a few weeks after initiation of carbamazepine, resolution on stopping carbamazepine, and response to steroids, a final diagnosis of NEH secondary to carbamazepine was made. Detailed history did not reveal any other drug being taken by the patient in the last six weeks. Causality assessment score was performed using Naranjo's algorithm and was scored 6 which suggested a probable relationship between the reaction and carbamazepine. Re-challenge to carbamazepine was not performed as the patient was put on a different class of anti-epileptic drugs.
Discussion
Neutrophilic eccrine hidradenitis (NEH) is a self-limiting dermatosis commonly associated with malignancies and chemotherapy. The exact etiology is not known. One hypothesis suggests that neutrophilic accumulation around the eccrine cells is either caused by local chemotactic factors or secondary to abnormal neutrophil function.[1] Another hypothesis proposes that NEH is actually a unique subtype of neutrophilic dermatosis in which antineoplastic chemotherapy induces the differentiation of myeloid leukemia blast cells into neutrophils. The leukemia blasts disappear from circulation as they develop mature morphology and differentiated functional characteristics, which allows margination, diapedesis, and accumulation in other tissues like eccrine glands.[5] Chemotherapeutic agents are excreted via the eccrine sweat glands and may cause a local irritant reaction.
To the best of our knowledge, this case report is the first instance of carbamazepine being considered as the causal drug for NEH. The differential diagnosis includes leukemia cutis, bullous pyoderma, pyoderma gangrenosum, erythema multiforme, Sweet's syndrome, drug hypersensitivity, and vasculitis. Among all of them, only NEH has a characteristic histological profile of pronounced neutrophilic infiltration of the lower dermis around the eccrine glands.[1] Establishing the diagnosis of NEH is important to avoid unnecessary and erroneous treatment for other conditions. A skin biopsy demonstrating neutrophilic infiltrate around the eccrine glands and coils and associated with necrosis helps confirm a diagnosis of NEH as done in our study.
Resolution of the condition is usually spontaneous following withdrawal of the drug, so no therapy is required. In severe cases, corticosteroids, dapsone and ibuprofen have been tried with varying success.[3] Recurrence following subsequent exposure to the offending drug is likely. A probable relationship between NEH and cabamazepine was suggested using Naranjo's algorithm, considering the temporal relationship between the condition and the drug and the resolution of symptoms after discontinuation of carbamazepine. We are reporting this case in view of the offending drug i.e. carbamazepine, which has not yet been reported in literature.
Acknowledgement
The authors acknowledge the contribution made by Dr. Ananya Chakraborty, Associate Professor, Vydehi Hospital, in helping score the causality assessment scale for this drug reaction.
Footnotes
Source of Support: Nil
Conflict of Interest: No
References
- 1.Harrist TJ, Fine JD, Berman RS, Murphy GF, Mihm MC., Jr Neutrophilic eccrine hidradenitis. A distinctive type of neutrophilic dermatosis associated with myelogenous leukemia and chemotherapy. Arch Dermatol. 1982;118:263–6. doi: 10.1001/archderm.118.4.263. [DOI] [PubMed] [Google Scholar]
- 2.Flynn TC, Harrist TJ, Murphy GF, Loss RW, Moschella SL. Neutrophilic eccrine hidradenitis: A distinctive rash associated with cytarabine therapy and acute leukemia. J Am Acad Dermatol. 1984;11:584–90. doi: 10.1016/s0190-9622(84)70210-6. [DOI] [PubMed] [Google Scholar]
- 3.Fitzpatrick JE, Bennion SD, Reed OM, Wilson T, Reddy VV, Golitz L. Neutrophilic eccrine hidradenitis associated with induction chemotherapy. J Cutan Pathol. 1987;14:272–8. doi: 10.1111/j.1600-0560.1987.tb00499.x. [DOI] [PubMed] [Google Scholar]
- 4.Beutner KR, Packman CH, Markowitch W. Neutrophilic eccrine hidradenitis associated with Hodgkin's disease and chemotherapy: A case report. Arch Dermatol. 1986;122:809–11. [PubMed] [Google Scholar]
- 5.Aractingi S, Mallet V, Pinquier L, Chosidow O, Vignon-Pennamen MD, Degos L, et al. Neutrophilic dermatoses during granulocytopenia. Arch Dermatol. 1995;131:1141–5. [PubMed] [Google Scholar]


