Abstract
Adverse effects to antipsychotics are varied, frequently intolerable, often serious and sometimes fatal in clinical practice. Seizures are one of these adverse effects. Almost all first and second generation antipsychotics elicit dose-dependent lowering of seizure threshold, indicating increased seizure risk at higher drug dosages. The adverse event of zotepine induced seizure is published in few case reports. We report the occurrence of myoclonic seizure progressing to generalized tonic-clonic seizures with zotepine along with clear temporal association of dose dependent modulation evident in this case.
KEY WORDS: Adverse effect, convulsive seizure, treatment resistant schizophrenia, zotepine
Introduction
Schizophrenia is prevalent among people with epilepsy and vice-a-versa. The reported rates range from 4% to 18%, with highest prevalence observed in people with temporal lobe seizures.[1] Antipsychotic-induced seizures appear to be relatively uncommon in patients lacking risk factors, however, they have been found to induce electroencephalographic (EEG) abnormalities resembling seizure activities at rate that far exceeds the frequency of actual antipsychotic induced seizures.[2] The majority of antipsychotics can reduce the seizure threshold and the risk is dose related. Zotepine (2-Chloro-11-(2-dimethyl-aminoethoxy) dibenzo [b, f] thiepin) is an atypical antipsychotic with molecular weight of 331.86, structurally similar to the phenothiazines and clozapine.[3] It has been found to be effective in management of both positive and negative symptoms of schizophrenia with beneficial effect on cognitive symptoms and its efficacy has been demonstrated in few open label clinical trials including treatment resistant schizophrenia.[4] The fatal adverse events observed with zotepine were neuroleptic malignant syndrome, abnormal ECG, paralytic ileus, and convulsive seizure (s).[5] Zotepine induced seizure has been only published in few case reports and discrete occasional observational studies[6] and none so far from India. We report myoclonic seizure progressing to generalized tonic-clonic seizures with clear temporal association of dose dependent modulation occurring with zotepine.
Case Report
A 22-year-old, right handed male with premorbid schizoid traits without significant past or family history of mental illness presented with an insidious onset, gradually progressive continuous course of four years duration of disabling symptoms characterized by delusion of control, delusion of persecution, auditory hallucinations (commenting and commanding type), anger outbursts and violent behaviour, mannerism, regressed behaviour, social withdrawal, poor personal care, decreased sleep, and appetite associated with severe socio-occupational dysfunction. There was no history of other Schneiderian First Rank Symptoms, substance use or abuse, suicidal attempt or ideations, affective symptoms, head injury, learning disability, epilepsy or neurodegenerative disorder. He was treated with adequate trial of trifluperazine, chlorpromazine, risperidone, olanzapine and aripiprazole since last three years with electroconvulsive therapy cycles (12 effective ECT's). Clozapine could not be built-up because he had persistent history of development of agranulocytosis even with 25 mg initiation (Total Leukocyte count was 2500/cc mm) and associated anemia (Hemoglobin 7.2 gm%). He was prescribed zotepine 50 mg per day, which was gradually increased every week by 50 mg, till 350 mg per day. His liver function tests were monitored for transaminase levels and were found to be within normal limits. He showed moderate improvement in the psychotic symptoms by week 8 (PANSS score in all three dimensions showed significant change from baseline by week 8). The dose was raised from 300 to 350 mg per day (in view of residual auditory hallucinations and off and on anger outbursts against parents). On 49th day on zotepine he developed paroxysms of sudden, brief and jerky muscle contractions involving right more than left upper extremities followed by tonic contraction of muscles throughout the body that typically continued for 20-30 seconds followed by clonic phase which had lasted for about a minute. He was found to be in a state of flaccid, unresponsiveness with stridorous breathing and involuntary passage of urine. He was given injection diazepam slow intravenous drip and his airway was secured. The EEG showed paroxysms of repetitive, generalized high amplitude discharges associated with muscle artefact followed by slow spikes [Figure 1]. The dose of zotepine was reduced to 300 mg per day. For the next week he remained seizure free and the EEG was showed residual epileptiform activity. However he began complaining of hearing of third person voices; which were not present with higher dose of zotepine. He was re-hospitalized for a brief duration and the dose of zotepine was again increased to 350 mg/day, four hours later patient again suffered another episode of myoclonic jerks; followed by tonic-clonic convulsions and post-ictal confusion. The EEG concomitantly showed generalized, transient, repetitive paroxysms of high amplitude spikes and polyspikes followed by slow waves. The dose of zotepine was reduced to 300 mg per day and clobazam 20 mg per day was added. Distraction techniques along with cognitive remediation were taught to patient to deal with intractable auditory hallucination. Patient has been seizure free since last four months and clinically better in both positive and negative symptoms.
Figure 1.
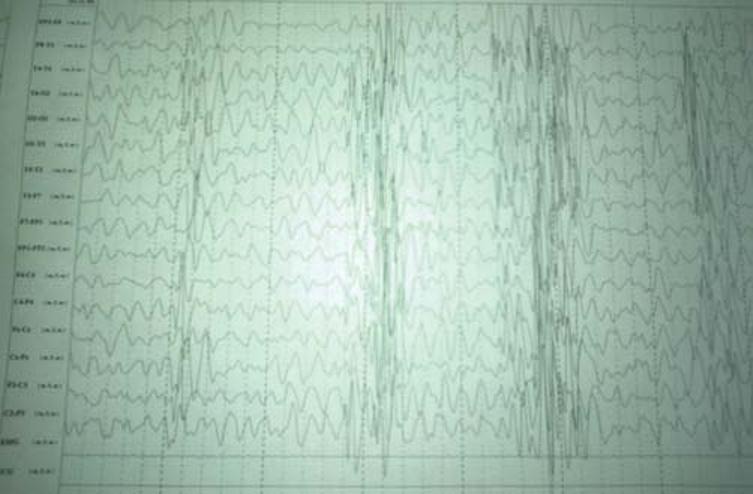
EEG showing repetitive, generalized paroxysms of high amplitude discharges followed by slow wave pattern associated with muscle artifact suggesting myoclonic type of epileptiform discharges
Discussion
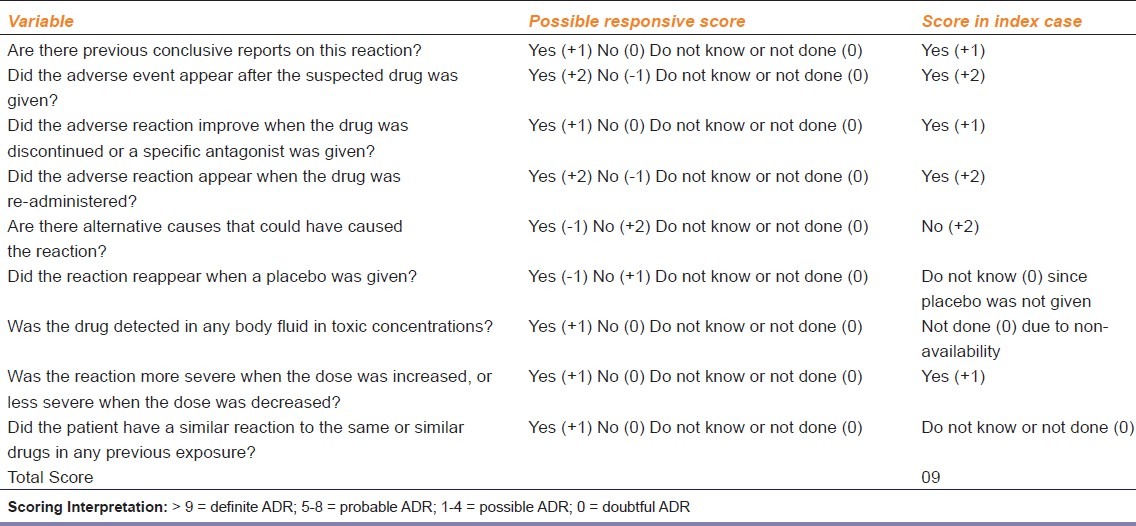
Convulsions are a well-known with antipsychotic drugs. The incidence of first unprovoked seizure with antipsychotics is estimated to be 0.073% to 0.086% almost similar to that of the general population 0.037% and as general rule, the more sedating the antipsychotic, the more likely it is to induce seizures.[6] Seizures were reported most commonly with clozapine, followed by chlorpromazine and Olanzapine, while quetiapine was least likely to cause convulsion[7,8] Data on zotepine induced seizure is scarce and mostly reported from Japan and European countries where it has been in use for almost two decades. In their landmark observational study Hori et al.,[9] evaluated 129 schizophrenic patient who were receiving zotepine and found that 22 (17.1% incidence) of them had developed grand mal seizures. No other seizure type was reported with zotepine so far. Thus the index case is the first to reflect an additional myoclonic type of seizures with zotepine with subsequent progression to generalized tonic-clonic seizures clearly related to escalation of the dose. The seizure in our patient improved when the dose was decreased from 350 mg/day to 300 mg/day and reappeared again within 72 hrs when zotepine was increased to 350 mg/ day suggesting a temporal association. There was no apparent alternate cause other than increase in the dose of zotepine that could have caused the seizure as his repeat liver function tests including serum ammonia level were also normal. Further, the epileptiform activity was confirmed on EEG (as shown in figure 1). On Naranjo Adverse Drug Reaction Probability Scale, the total score was 9 out of 13 [Table 1] which reflects the ‘definite causal association’[10]
Table 1.
Naranjo Causality Scale[9]
This is in conformity with the study by Hori et al., who reported that zotepine induced seizure(s) were closely related to the dosage (above 325 mg/day) and the duration of use zotepine (mean duration is 48.1 days). Appropriate investigations ruled out any organic cause of the convulsions and zotepine was successfully continued (300 md/day) together with clobazam (20 mg/day). By the time the treatment was stabilized, the patient had not experienced any convulsions in the last 9 months. These findings suggest that zotepine-induced seizures were phenomenologically identical to those occurring in juvenile myoclonic epilepsy and were classified as generalized epileptic seizures. We tentatively conclude that generalized myoclonic epileptic seizures may be induced by zotepine. They can be successfully treated and gradual dose titration can reduce the likelihood of further episodes of seizures. Also concomitant use of a suitable mood stabilizer or anti-epileptic medication can improve the outcome of treatment-resistant schizophrenia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Gaitatzis A, Carroll K, Majeed A, Sander WJ. The epidemiology of the comorbidity of epilepsy in the general population. Epilepsia. 2004;45:1613–22. doi: 10.1111/j.0013-9580.2004.17504.x. [DOI] [PubMed] [Google Scholar]
- 2.Alldredge BK. Seizure risk associated with psychotropic drugs: clinical and pharmacokinetic considerations. Neurology. 1999;53(Suppl 5):68–75. [PubMed] [Google Scholar]
- 3.Cooper SJ, Butler A, Tweed J, Welch C, Raniwalla J. Zotepine in the prevention of recurrence: A randomised, double-blind, placebo-controlled study for chronic schizophrenia. Psychopharmacology. 2000;150:237–43. doi: 10.1007/s002130000452. [DOI] [PubMed] [Google Scholar]
- 4.Hashimoto K, Sudo T, Hirano M, Motomura H, Tagawa K, Nashiro S, et al. Efficacy and safety of zotepine for patients with treatment-resistant schizophrenia. Schizophr Res. 2006;87:332–3. doi: 10.1016/j.schres.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 5.Kondo T, Otani K, Ishida M, Tanaka O, Kaneko S, Fukushima Y, et al. Adverse effects of zotepine and their relationship to serum concentrations of the drug and prolactin. Ther Drug Monit. 1994;16:120–4. doi: 10.1097/00007691-199404000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Lee KC, Finley PR, Alldredge BK. Risk of seizures associated with psychotropic medications: emphasis on new drugs and new findings. Expert Opin Drug Saf. 2003;2:233–47. doi: 10.1517/14740338.2.3.233. [DOI] [PubMed] [Google Scholar]
- 7.Devinsky O, Honigfeld G, Patin J. Clozapine-related seizures. Neurology. 1991;41:369–71. doi: 10.1212/wnl.41.3.369. [DOI] [PubMed] [Google Scholar]
- 8.Pisani F, Oteri G, Cost C, Di Raimondo G, Di Perri R. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25:91–110. doi: 10.2165/00002018-200225020-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hori M, Suzuki T, Sasaki M, Shiraishi H, Koizumi J. Convulsive seizures in schizophrenic patients induced by zotepine administration. Jpn J Psychiatry Neurol. 1992;46:161–7. doi: 10.1111/j.1440-1819.1992.tb00829.x. [DOI] [PubMed] [Google Scholar]
- 10.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]


