Abstract
Objective
To investigate the frequency and characteristics of the mandibular accessory buccal foramen (ABF) with CT.
Methods
A retrospective study was carried out using the CT records of 504 patients referred to the Erciyes University Medical School (Kayseri, Turkey) between 2007 and 2010. Presence, location, diameter, area and number of ABFs and their continuity with mandibular canal and distance to the mental foramen were evaluated using axial, sagittal and three-dimensional CT images. Statistical analysis was performed using SPSS® v. 15 (SPSS Inc., Chicago, IL), and t-tests were used for statistical analysis.
Results
14 ABFs were observed in 10 (2%) of 504 patients. The frequency of ABFs was found to be 2.6% in males and 1% in females. The mean distance between the ABF and the mental foramen was 5.0 mm [standard deviation (SD) ± 2.48]. The mean long axis of the ABFs was 1.4 mm (SD ± 0.4) and the mean area of them was 1.5 mm2 (SD ± 0.8). The mean area of the mental foramen on the side with the ABF was 4.1 mm2 (SD ± 2.71).
Conclusions
This study presents a relatively lower frequency of ABFs than that in the literature. These foramina could have more complex neurovascular structures than was previously thought. Thus, in special cases where a direct surgical exploration during the planned surgery is not indicated, CT or cone beam CT examination to determine the possible presence of ABFs may be indicated.
Keywords: accessory mental foramen, buccal foramen, mental foramen, computed tomography
Introduction
The mental nerve is a somatic afferent sensory nerve of the mandibular nerve that emerges from the mental foramen and which presents as a single circular, or elliptical, bilateral radiolucent area in the premolar region.1-3 On the perimandibular surface, accessory foramina smaller than the mental foramen have been frequently reported in the literature.3-5 The evaluations of accessory foramina that relate to the mandibular canal are clinically important in endodontic treatments and surgical procedures such as dental implant insertion, implant-related bone grafting, genioplasty and mandibular anterior segmented osteotomy.4-8
Recently, some studies investigating the presence of small foramina in the perimandibular region have been carried out.4,5,7,8 In CT-based studies, Naitoh et al5 and Katakami et al7 classified accessory foramina according to their continuity with the mandibular canal. According to these reports, an accessory foramen showing a connection with the mandibular canal was defined as accessory mental foramen (AMF), and an accessory foramen showing no connection with the mandibular canal was defined as a nutrient foramen.5,7 However, in a cadaveric study, Fuakami et al9 stated that neurovascularization of these foramina is more complex than was previously thought. Thus, in that report, all the detected accessory foramina on the buccal mandibular surface were defined as accessory buccal foramina (ABFs), regardless of location and course.
ABFs are rarely observed with conventional radiography techniques, such as periapical and panoramic radiographs, because the long axis of an ABF is generally less than 1.5 mm, and it is difficult to recognize this structure with two-dimensional techniques.7,9-11 Three-dimensional (3D) evaluation with CT and cone beam CT (CBCT) could demonstrate the presence and course of ABFs. The detection of ABFs may reduce the rates of haemorrhage, post-operative pain and paralysis in surgical procedures.5
In the present study, we aimed to investigate the frequency and characteristics of ABFs using CT images.
Material and methods
A retrospective study was performed using the CT records of 504 patients referred to the Erciyes University Medical School, Kayseri, Turkey, from 2007 to 2010. All records were selected from a Turkish population from the Cappadocia region of Turkey. CT images had been taken because of the patients' previous medical problems. The exposure factors and slice thickness (0.625–1.25 mm) varied according to the requirement of each individual, and images were taken by a radiology technician with a CT machine (LightSpeed™; GE Medical Systems, Milwaukee, WI). Reformat images were generated in a PACS (Picture Archiving and Communication Systems) unit and evaluated using InfinittTM software v. 3.0.8.1 (Infinitt Medical Imaging and Archive System, Seoul, Republic of Korea). All CT images were examined by two oral radiologists (YS with 11 years of experience and HS with 4 years of experience in CT).
A buccal foramen, except for the mental foramen, was identified as ABF regardless of location and course. Images were examined in axial and sagittal planes and 3D reformats. Each ABF was investigated with regards to its continuity with the mandibular canal (Figures 1 and 2). The relative location of the ABF in relation to the mental foramen was marked according to the illustration in Figure 3. The distance between the centre of the ABF and the mental foramen was measured in the sagittal CT images (Figure 4). In addition, the long (a) and short (b) axes of each ABF and mental foramen on the side with the ABF were measured (Figure 5) to calculate the elliptical area using the following formula:
 |
(1) |
Figure 1.
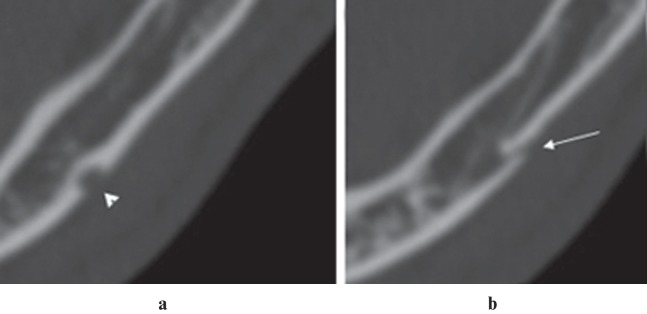
Axial CT images of an accessory buccal foramen (ABF) on the left side (Patient 9). (a) Arrowhead shows the mental foramen and (b) arrow shows the ABF has a connection with the mandibular canal
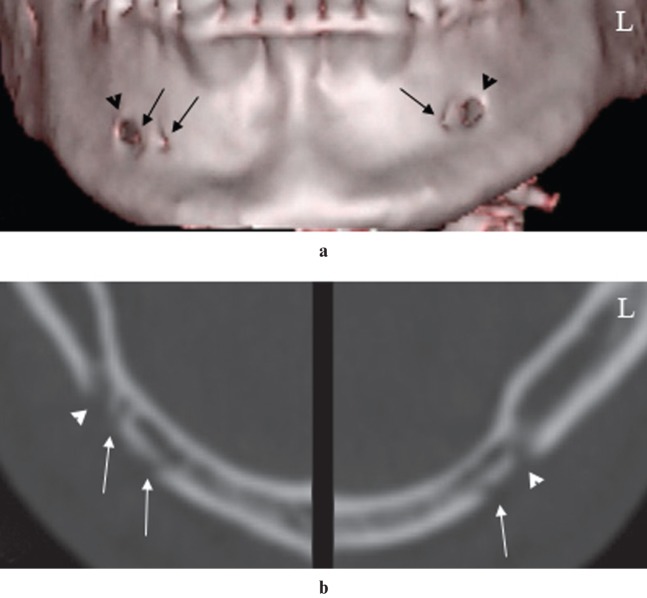
Figure 2.
Three-dimensional reconstruction (a) and axial CT images (b) of an accessory buccal foramen (ABF) on the right side (Patient 6). Images show the mental foramen (arrowheads) and that the ABF (arrows) has a connection with the anterior loop of the mental nerve
Figure 3.
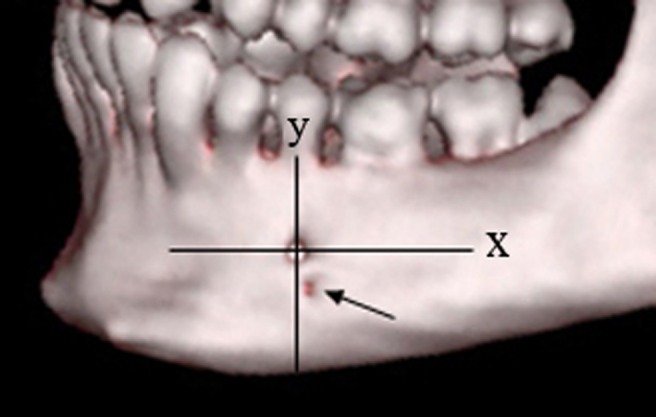
Three-dimensional reconstruction shows the location of the accessory buccal foramen (ABF). The origin was defined as the centre of the mental foramen. The x-axis was parallel to the occlusal plane and the arrow shows the ABF
Figure 4.
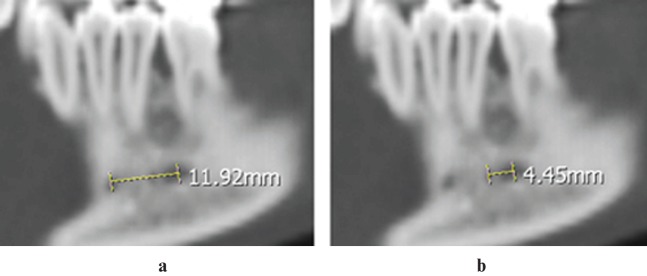
Longitudinal CT images of the buccal surface show two accessory buccal foramina on the right side (Patient 5). The distances between the centre of the mental foramen and the farther accessory buccal foramen (ABF) (a), and between the centre of mental foramen and the nearby ABF (b) are shown
Figure 5.
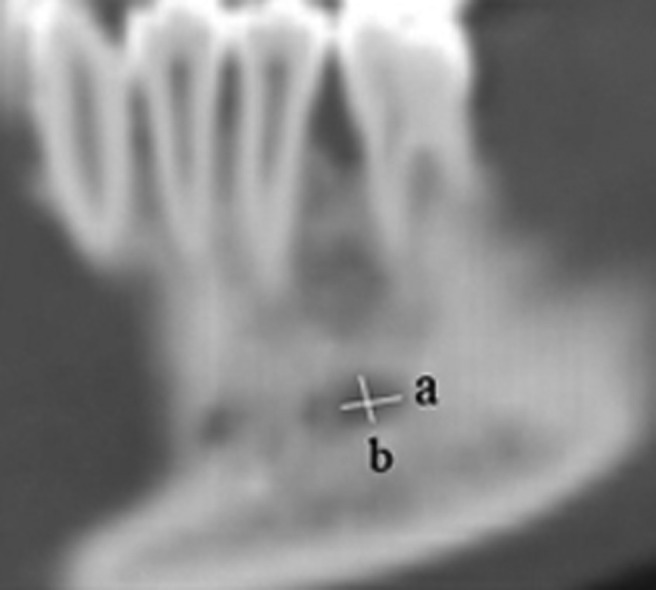
Longitudinal CT image of the buccal surface and measurement of axes of a foramen. The long (a) and short (b) axes of a foramen were measured
Statistical analysis
Statistical evaluation of the data was carried out using SPSS® v. 15.0 (SPSS Inc., Chicago, IL). The differences between categorical variables were analysed using t-tests. p<0.05 was considered to be statistically significant.
Results
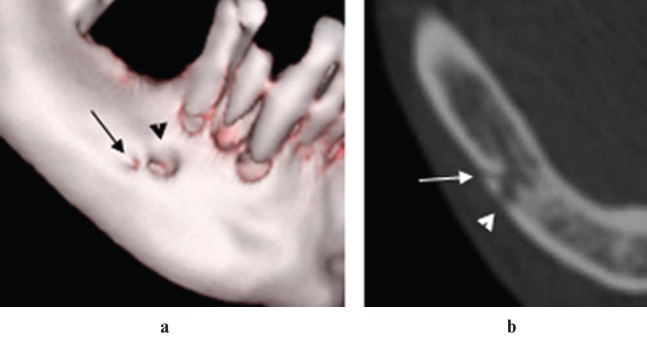
A total of 504 CT images obtained between 2007 and 2011 were evaluated. Of these patients, 307 (60.9%) were male and 197 (39.1%) were female. The mean age of the patients was 39.73 ± 15.88 years and there was no statistically significant difference in mean age between males (40.8 ± 16.7 years) and females (38.1 ± 14.9 years) (p = 0.458). 14 ABFs were detected in 10 (2%, 8 males and 2 females) of the 504 patients. The frequency of ABFs was found to be 2.6% in males and 1% in females. There was no statistically significant difference in males and females (p = 0.327). Of the cases of ABF, three were bilateral and seven were unilateral: three were on the right and four were on the left side. No statistically significant differences were found between either the right- and left-sided ABFs or between female and male patients (p > 0.05). In addition, three ABFs were detected on the right side of Patient 5 (Figure 6). Also, there was no statistically significant difference in mean age between patients with ABFs (39.73 ± 15.8 years) and those without (39.73 ± 15.8 years) (p > 0.05). The mean distance between the ABF and the mental foramen was 5.0 mm (SD ± 2.48 mm). The mean area of the 14 ABFs was 1.5 mm2 (SD ± 0.8 mm2). The mean area of the mental foramen on the side with the ABF was 4.1 mm2 (SD ± 2.7 mm2). Also, the proportion of the area of the ABF to the area of the mental foramen on the same side ranged from 5.6% to 92.9% (mean 50.3%, SD ± 27%) (Table 1).
Figure 6.
Three-dimensional reconstruction (a) and axial CT images (b) of the bilateral accessory buccal foramen (ABF) (Patient 5). Arrowheads show the mental foramen and arrows show the ABF
Table 1. Characteristics of accessory buccal foramina (ABFs) and mental foramina (MFs) on the side with ABFs.
| Axis of foramen (mm) |
|||||||||
| ABF |
MF |
Area of foramen (mm2) |
|||||||
| Number of ABF | Location | Distance to MF (mm) | Long | Short | Long | Short | ABF | MF | Proportion of the area of ABF/MF (%) |
| 1 | ID | 5.3 | 1.7 | 1.5 | 2.1 | 2 | 2 | 3.2 | 62.5 |
| 2 | SD | 2.9 | 1.2 | 0.9 | 1.2 | 1.2 | 0.8 | 1.1 | 72.7 |
| 3 | IM | 7.4 | 1.2 | 1.1 | 1.8 | 1.7 | 1.1 | 2.4 | 45.8 |
| 4 | M | 2.9 | 1.3 | 1.2 | 1.4 | 1.2 | 1.2 | 1.3 | 92.3 |
| 5 | IM | 4.5 | 1.7 | 1.6 | 4 | 2.4 | 2.1 | 7.7 | 27.3 |
| 6 | IM | 11.9 | 2.3 | 2.1 | 4 | 2.4 | 3.7 | 7.7 | 48 |
| 7 | IM | 5.6 | 1.6 | 1.5 | 3.5 | 2.3 | 1.8 | 6.2 | 29 |
| 8 | ID | 5.6 | 1.1 | 1 | 4 | 3 | 0.9 | 9.2 | 9.8 |
| 9 | SD | 4.2 | 1.4 | 1.2 | 1.5 | 1.2 | 1.3 | 1.4 | 92.9 |
| 10 | SD | 3.5 | 1.2 | 1.2 | 1.4 | 1.4 | 1.1 | 1.6 | 68.8 |
| 11 | ID | 3.2 | 0.7 | 0.6 | 2.9 | 2.4 | 0.3 | 5.5 | 5.6 |
| 12 | SM | 3.6 | 1.6 | 1.5 | 1.9 | 1.8 | 1.9 | 2.6 | 73.1 |
| 13 | ID | 3.4 | 1.4 | 1.4 | 2.4 | 2.3 | 1.6 | 4.3 | 37.2 |
| 14 | ID | 6.1 | 1.4 | 1.3 | 2.6 | 1.8 | 1.4 | 3.6 | 38.9 |
ID, inferodistal; IM, inferomesial; M, mesial; SD, superodistal; SM, superomesial.
The locations of the ABFs in relation to the mental foramina are illustrated in Figure 7. Most of the ABFs (5, 35.8%) were located in the inferodistal region and the fewest (1, 7.1%) were located in the superomesial and mesial regions (Table 1). Furthermore, 8 of the 14 ABFs had continuity with the mandibular canal. Two ABFs had a connection with the anterior loop of the mental foramen (Figure 2) and six ABFs had a direct connection with the mandibular canal at the posterior of the mental foramen.
Figure 7.
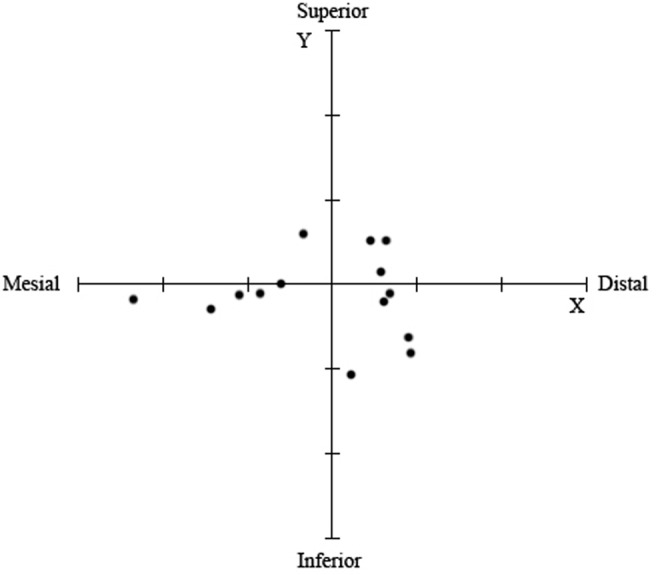
Locations of the accessory mental foramina. The confluence of the axis, defined as the centre of the mental foramen and the x-axis, is parallel to the occlusal plane. Equal lines on the x- and y-axis correspond to 5 mm
Discussion
An accessory foramen located in the region surrounding the mental foramen and showing a connection with the mandibular canal is defined as AMF and is believed to relate to the mental nerve. On the other hand, an accessory foramen showing no connection with the mandibular canal is defined as a nutrient foramen, which nourishes the bone with arterial structures.5,7 Ichikawa12 reported that the submental, lower lip, buccal arteries and branches of the facial artery enter into the mandibular cancellous bone through the nutrient foramina. However, a clear distinction between AMF and the nutrient foramen has not been identified or supported in previous reports. In a cadaveric study, Fuakami et al9 reported some remarkable findings: (a) a branch of the facial artery coursed beside the mandible and re-entered through an ABF which showed a connection with the mandibular canal; and (b) a branch of the mental nerve re-entered the mandible through an ABF which showed no connection to the mandibular canal. Therefore, neurovascularization of these foramina may be more complex than was previously thought, and we also called the accessory foramina found in the present study “accessory buccal foramina” regardless of location and course.
The reported frequency of ABFs has been reported to range widely from 1.4% to 30%.13-17 However, the frequency of ABFs was found to be 4%, 7.7% and 10.7% in CT-based studies performed in the last 3 years.5,11,18 In the present study, 14 ABFs were detected in 10 of the 504 patients, and the frequency rate was found to be 2%, which is lower than that generally reported in the literature. There was no statistically significant difference in males and females and no significant gender differences were observed in the present and previous studies.
The mean long axis of the ABF ranged from 1.3 mm to 1.9 mm in previous CT-based studies.5,7,11 In accordance with previous studies, the mean long axis was found to be 1.4 mm (SD ± 0.4 mm) in this study. The mean area of the ABFs was found to be 1.7 mm2 and 1.5 mm2 in different studies performed by Naitoh et al.5,18 Similar to those studies, we found a mean diameter of 1.5 mm2 (SD ± 0.8 mm2). Also, Naitoh et al5 reported that the distance between the mental foramen and the ABF ranged from 4.5 mm to 9.6 mm, with a mean of 6.3 mm. In the present study, the distance between the mental foramen and the ABF ranged from 2.9 mm to 11.9 mm, with a mean of 5 mm (SD ± 2.5 mm).
The location of the ABF in relation to the mental foramen has been demonstrated by Katakami et al7 and Naitoh et al.5 Both studies reported that the majority of ABFs were located in the distal region of mental foramen. Only 1 of 17 and 3 of 15 ABFs, respectively, were located at the mesial region in the reports by Katakami et al7 and Naitoh et al.5. However, the mesial-to-distal ratio (mesial 6, distal 8 ABFs) in the present study was close. According to the comparison of the inferior and superior regions, the majority of ABFs were located in the inferior region in previous studies as well as in our study.5,7
The courses of the ABFs were also examined with radiographic findings. 8 of the 14 ABFs had continuity with the mandibular canal and 5 did not. As a point of interest, a branch of the mental nerve most likely re-entered the mandible through an ABF and continued to the median region in Patient 4 (Figure 8). However, these radiographic findings could not provide conclusive information about the neurovascular structures of the ABFs in our study. Thus, in a cadaveric study, Fuakami et al9 reported the following possibilities with regard to the neurovascularization of the ABF: it may be due to (a) a branch of an artery which enters the mandible, or (b) a branch of the mental nerve which re-enters the mandible and (c) a branch of the mental nerve which exits the mandible. As a result, radiographic findings of the relation between the ABF and the mandibular canal cannot confirm the neurovascular structures of an accessory foramen.
Figure 8.
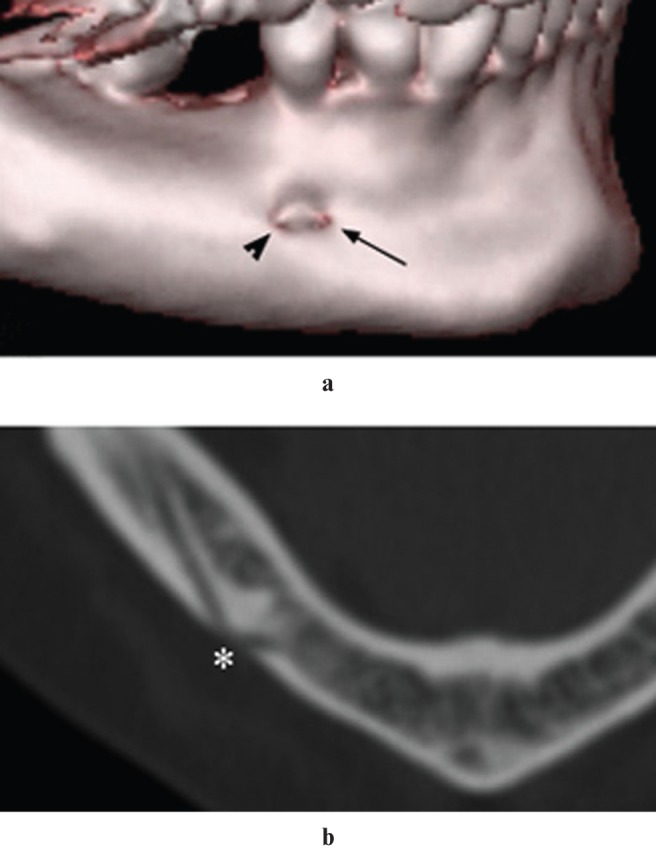
Three-dimensional reconstructions (a) of an accessory buccal foramen (ABF) on the right side (Patient 4). Arrowhead shows the mental foramen and arrow shows the ABF. Axial CT image (b) shows the junction point (asterisk) of the mental foramen and ABF
Dentists routinely use panoramic radiographs in dental examinations. These radiographs are generally sufficient for general dental practices, and ABFs in many surgical procedures can be found by appropriate surgical approaches.18 However, application of tomographic techniques can reduce risk factors and provide considerable information before surgical procedures involving the perimandibular region or other important anatomical structures. In recent years, CBCT applications have become widespread. Thus, in order to avoid excessive radiation, clinicians should prefer CBCT to other tomographic techniques. From among different imaging modalities of tomography, we consider that 3D reformat is the best way to observe the presence of ABF and its location in relation to the mental foramen. However, axial, sagittal and cross-sectional slices are more functional regarding the detection of the course of ABF.
In conclusion, this study presents a relatively low frequency rate of ABFs than that in the literature. However, the presence and location of ABFs and their neurovascular structures are important during surgical procedures involving the area surrounding the mental foramen. The presence of an arterial branch or accessory mental nerve in the buccal perimandibular region should be considered. This approach may reduce the risk of paralysis, haemorrhage and post-operative pain in this region.
References
- 1.De Andrade E, Otomo-Corgel J, Pucher J, Ranganath KA, St George N., Jr The intraosseous course of the mandibular incisive nerve in the mandibular symphysis. Int J Periodontics Dent 2001;21:591–597 [PubMed] [Google Scholar]
- 2.Hu KS, Yun HS, Hur MS, Kwon HJ, Abe S, Kim HJ. Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg 2007;65:2288–2294 [DOI] [PubMed] [Google Scholar]
- 3.Neves FS, Torres MGG, Oliveira C, Campos PSF, Crusoe-Rebello L. Lingual accessory mental foramen: a report of an extremely rare anatomical variation. J Oral Science 2010;52:501–503 [DOI] [PubMed] [Google Scholar]
- 4.Kaufman E, Serman NJ, Wang PD. Bilateral mandibular accessory foramina and canals: a case report and review of the literature. Dentomaxillofac Radiol 2000;29:170–175 [DOI] [PubMed] [Google Scholar]
- 5.Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:289–294 [DOI] [PubMed] [Google Scholar]
- 6.Sutton RN. The practical significance of mandibular accessory foramina. Aust Dent J 1974;19:167–173 [DOI] [PubMed] [Google Scholar]
- 7.Katakami K, Mishima A, Shiozaki K, Shimoda S, Hamada Y, Kobayashi K. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. J Endod 2008;34:1441–1445 [DOI] [PubMed] [Google Scholar]
- 8.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:25–31 [DOI] [PubMed] [Google Scholar]
- 9.Fuakami K, Shiozaki K, Mishima A, Shimoda S, Hamada Y, Kobayashi K. Detection of buccal perimandibular neurovascularisation associated with accessory foramina using limited cone-beam computed tomography and gross anatomy. Surg Radiol Anat 2011;33:141–146 [DOI] [PubMed] [Google Scholar]
- 10.Toh H, Kodama J, Yanagisako M, Ohmori T. Anatomical study of the accessory mental foramen and the distribution of its nerve. Okajimas Folia Anat Jpn 1992;69:85–88 [DOI] [PubMed] [Google Scholar]
- 11.Haktanir A, Ilgaz K, Turhan-Haktanir N. Evaluation of mental foramina in adult living crania with MDCT. Surg Radiol Anat 2010;32:351–356 [DOI] [PubMed] [Google Scholar]
- 12.Ichikawa K. Nutrient artery in Japanese prenatal mandible. Shikagakuho 1961;61:481–511 [Google Scholar]
- 13.Agthong S, Huanmanop T, Chentanez V. Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg 2005;63:800–804 [DOI] [PubMed] [Google Scholar]
- 14.Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Acta Anat 1986;126:21–28 [DOI] [PubMed] [Google Scholar]
- 15.Hanihara T, Ishida H. Frequency variations of discrete cranial traits in major human populations. IV. Vessel and nerve related variations. J Anat 2001;199:273–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sawyer DR, Kiely ML, Pyle MA. The frequency of accessory mental foramina in four ethnic groups. Arch Oral Biol 1998;43:417–420 [DOI] [PubMed] [Google Scholar]
- 17.Shankland WE., 2nd The position of the mental foramen in Asian Indians. J Oral Implantol 1994;20:118–123 [PubMed] [Google Scholar]
- 18.Naitoh M, Yoshida K, Nakahara K, Gotoh K, Ariji E. Demonstration of the accessory mental foramen using rotational panoramic radiography compared with cone-beam computed tomography. Clin Oral Implants Res 2011:22: 1415–1419 [DOI] [PubMed] [Google Scholar]