Abstract
Arteriovenous malformations (AVMs) of the jaws are relatively rare, with fewer than 200 cases reported in the literature. Their real importance lies in their potential to result in exsanguination, which usually follows an unrelated treatment, such as tooth extraction, surgical intervention, puncture wound or blunt injury in involved areas, with the dentist unaware of the existence of the AVM. The present case illustrates an AVM in an 18-year-old female with swelling on the right side of the face. This case report is unique because although there was no history of bleeding episodes, thorough examination and investigation diagnosed it as high-flow vascular malformation. We ascertain the importance of dentists' awareness of the fatal outcome of these lesions and emphasize that, prior to performing any procedure, necessary investigations should always be done.
Keywords: arteriovenous malformations, exsanguination, varix, embolization
Introduction
Before the 1980s, vascular lesions were referred to as haemangiomas. Mullikin and Glowacki,1 in 1982, classified vascular lesions into haemangiomas and vascular malformation based on endothelial characteristics. Vascular malformations can be categorized into low-flow lesions (capillary malformations, lymphatic malformations and venous malformations) and high-flow lesions [arteriovenous malformations (AVMs) and arteriovenous fistulae], according to blood flow characteristics.1
The two categories of vascular lesions have fundamentally different aetiologies and clinical presentations. Haemangiomas are vascular tumours demonstrating endothelial hyperplasia that enlarges by rapid cellular proliferation.2 They appear in numerous soft-tissue locations within the oral cavity, with the lips, buccal mucosa and tongue being the most common sites, while the skeleton is rarely involved. Vascular malformations are structural malformations with a normal rate of endothelial cell turnover, which are present at birth and are relatively static in nature, changing in size when they sustain trauma, infection or endocrine changes.3
Haemangiomas are caused by a failure of differentiation in the early stages of embryogenesis. Vascular malformations, on the other hand, are caused by a disturbance in the late stages of angiogenesis (truncal stage) and result in the persistence of arteriovenous anastomoses present during embryonic life.4 The shunt from a high-pressure to a low-pressure compartment can produce a pulsating mass and a characteristic bruit. The veins emerging from the shunt become dilated and thickened (arterializations), and increased flow rate accounts for the observed dilatation of the arteries.5 True involution never occurs in vascular malformations. Unlike haemangiomas, they are associated with skeletal abnormalities in 34% of cases.3
Case report
An 18-year-old female patient reported with a complaint of swelling on the right side of the face for 1 year and pain in right lower back teeth for 6 months. History revealed that the swelling was noticed by the patient's mother and her neighbours 1 year previously and there was no change in the size of the swelling. Pain started 6 months previously; it was intermittent and dull, radiating to the right pre-auricular area. She consulted a local doctor regarding the pain and took medication but the pain did not subside. The patient also had paraesthesia of the right side of the lower lip for 6 months. Family and medical history were non-contributory.
On extra-oral examination, facial asymmetry was observed owing to a swelling on the right side of the mandible. Clinical examination revealed diffuse swelling of 10 × 7 cm on the right side of body and on the angle of the mandible. The swelling extended anteroposteriorly 4 cm away from the angle of the mouth to 2 cm crossing the angle of the mandible, and superioinferiorly from the alatragus line to 3 cm crossing the inferior border of the mandible. Deviation of the mandible, to the right side was appreciated. On inspection, surface texture of the swelling was normal and visible pulsations were seen. On palpation, the temperature was raised and the swelling was non-tender and soft in consistency; compressible, palpable thrill was also noted. On auscultation, bruit was heard over the swelling. No secondary changes were observed (Figure 1). On intra-oral examination, Grade II mobility was observed in teeth 46 and 47 and dental caries in relation to tooth 47.
Figure 1.

Extra-oral view with swelling on right side of angle of mandible
A provisional diagnosis of vascular malformation was given based on visible pulsations, palpable thrill and bruit. A differential diagnosis of venous malformation, lymphatic malformation and AVM was given.
Intra-oral periapical radiograph showed loss of lamina dura and root resorption of teeth 46 and 47. The periapical region of teeth 46, 47 and 48 showed a moth-eaten appearance with multiple pin-point punched-out lytic lesions, erasing inferior alveolar canal borders (Figure 2).
Figure 2.

Intra-oral periapical radiograph—multiple pin-point punched-out lytic lesions with loss of trabeculation in teeth 46, 47 and 48 and root resorption of teeth 46 and 47
Panoramic radiograph showed extensive radiolucency in the posterior mandible causing destruction of the posterior border of the ascending ramus and condyle of the mandible. The panoramic radiograph also showed loss of trabeculation in the posterior body of the mandible with multiple punched-out lytic lesions (Figure 3).
Figure 3.

Panoramic radiograph—radiolucency in the posterior body of the mandible with destruction of the posterior border of the ascending ramus and condyle of the mandible
Colour Doppler revealed large draining veins, and feeding artery from the facial artery was noted. Fistulous communications with arteriovenous shunts revealed mixing of blood and a spectral study showed very high velocity of 320 cm s–1, suggesting arteriovenous shunting (Figure 4).
Figure 4.

Colour Doppler—arteriovenous shunts showing mixing of blood and very high velocity of 320 cm s–1
CT revealed an irregular expansile osteolytic destructive lesion involving the ramus and condyle of the right mandible. There is disruption of cortex overlying the mandible. A large soft-tissue density lesion with attenuation values of 40–45 HU was seen at the angle of the mandible and was infiltrating the parotid gland (Figures 5 and 6).
Figure 5.
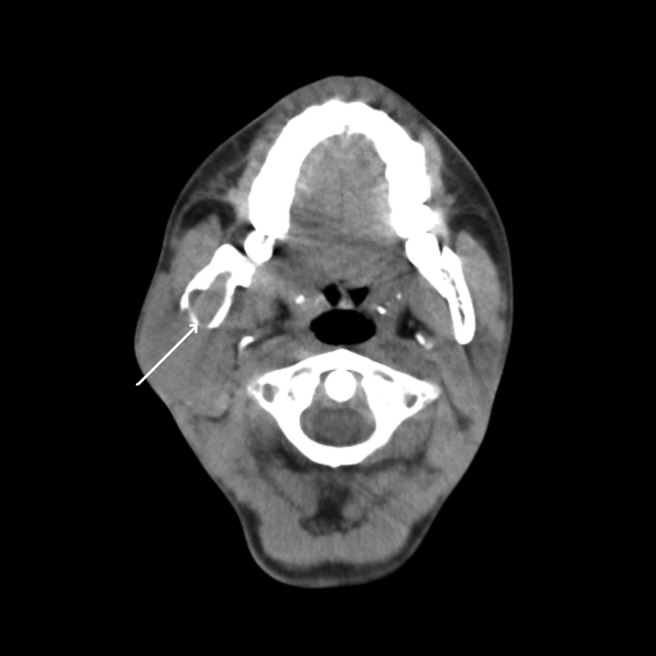
CT—axial soft-tissue algorithm showing expansion of the ramus and the condyle with cortical breach
Figure 6.

CT—axial bone algorithm showing an expansile osteolytic lesion involving the ramus and the condyle of the mandible on the right side with cortical destruction and surrounding soft-tissue component (arrow)
MRI revealed a large isointense soft-tissue lesion lateral to the ramus of the mandible and involving the parotid gland contiguously. The cortex of the mandible appeared interrupted with areas of destruction. MRI also revealed multiple serpentine flow voids in the right parotid, ramus and condyle, which were suggestive of high-flow vascular malformation (Figure 7).
Figure 7.

MRI—T1 axial fat saturated—multiple flow voids (arrows) in the right parotid and ramus region with loss of signal intensity
MR angiography (MRA) showed a large feeding artery from the ipsilateral facial artery and early opacification of the draining veins, which were grossly enlarged, and all the veins were draining to the internal jugular vein. MRA also confirmed a vascular nature with multiple tortuous vessels and suggested large AVM in the right parotid, ramus and condyle of the mandible (Figure 8).
Figure 8.

MR angiography—enlarged ipsilateral external carotid artery branches and internal jugular vein
Discussion
Vascular malformations are extremely common lesions, accounting for approximately 7% of all benign tumours. Although the head and neck constitute less than 14% of the total surface area of the body, approximately 50% of all vascular malformations occur in this region.6
AVMs are the most common high-flow lesions, frequently identified in the limbs, head, neck and lungs. However, lesions of the oral and maxillofacial regions are very rare. AVMs have been reported in the maxilla, but at half the frequency of AVMs in the mandible.7 AVMs of the jaws are relatively rare, with fewer than 200 cases reported in the literature.8
AVMs usually appear in adolescence but has an age range of 3 months to 74 years. Some authors noted predominance in females (female-to-male ratio, 2:1) while others have reported equal prevalence among males and females.4 Kohout et al9 studied 81 patients over a period of 20 years and found that 55 AVMs (69%) were in the middle of the face, 11 (14%) in the upper third and 14 (17%) in the lower third of the face.
Some cases of AVMs of the jaws are seen as painless, slow-growing soft-tissue enlargement with an audible bruit or palpable thrill, mucous membrane or cutaneous pigment changes, gingival bleeding and mobile tooth. Other patients are asymptomatic or may just have a loose tooth.8 However, when it involves the jaws, it is potentially life threatening because of uncontrollable massive haemorrhage during tooth extraction. The most frequent objective sign of an intra-osseous AVM is recurrent spontaneous bleeding from the gingival region. Other symptoms suggestive of AVM include gingival discolouration, hyperthermia over the lesion and a subjective feeling of pulsation in the presence of bruits.10
Radiographically, vascular malformations of the jaws have been referred to as the “great radiologic imitators”11 and can look like any lesion ranging from a cyst to a malignancy. AVMs show different signs because of their different locations, their extent and whether or not they have soft-tissue extension.3 In the mandible, vascular malformation produces a poorly defined, radiolucent image, often with the appearance of honeycomb or soap bubbles, with small, rounded and irregular lacunae or a punched-out area.7 AVMs most commonly appear as multilocular radiolucencies in panoramic examinations owing to an enlarged, pulsating inferior dental vein, sometimes owing to a dilated tortuous inferior dental artery.12
Thus, a large number of tumours, both benign and malignant, should be considered in the differential diagnosis. Of the benign lesions, squamous cysts are the most frequent. Less common lesions include non-epithelial cysts (also known as haemorrhagic or traumatic bone cysts), fibrous dysplasia, fibroma, myxoma, neurofibroma, eosinophilic granuloma and aneurysmal bone cysts.13 The other multilocular lesions, tumours and conditions which can be included in the list of differential diagnoses are ameloblastoma, central giant cell granuloma and odontogenic myxoma.14 Other features which are suggestive of a blood vessel tumour include widening of the marrow spaces, enlargement of the mandibular canal and the presence of clusters of small rounded or tubular bone defects with sclerotic margins confirming the shape of blood vessels.13
In the AVMs of the mandible without any involvement of soft tissue, the cortex of osteolytic radiolucency was intact and no septum was apparent in most of the cases, which could be helpful when differentiating it from ameloblastoma and other malignant lesions of the mandible, as they often have a perforated cortex. AVMs of the mandible can also be differentiated from dentigerous cysts because of the lack of a discrete margin and a sclerotic rim. The coexistence of a pulsatile soft-tissue mass and intraosseous changes on radiography warrants a high index of suspicion for the presence of an AVM of the jaws and raises little problem for the diagnosis.8
Because it most commonly appears as a multilocular radiolucency, other radiographic aids such as CT, MRI and digital subtraction angiography (DSA) are thought to obtain an accurate diagnosis of AVM.
Recently, digitalized equipment for Doppler sonography allows non-invasive depiction of small vessels concomitantly with the surrounding morphological features of anatomic structures. It also enables measurement of velocity of blood flow and resistance of the vessels. Thus, ultrasonography using colour Doppler flow analysis can confirm fast-flow anomalies.15 Normal arterial velocity is 80 cm s–1 and normal venous is 30 cm s–1; in our case it was 320 cm s–1, which is very high.
CT scan with high resolution proved to be very useful. In a study by Fan et al,8 the CT scan features of AVMs in the jaws included osteolytic expansion of the jaw (cavity-like change), expanded marrow spaces and obliteration of trabeculae. These findings are similar to our case. CT before and after intravenous administration of contrast medium has been the main imaging diagnostic procedure for a long time, being able to identify both haemangiomas and other vascular anomalies. However, it is important to remember that the ionizing radiation used with CT, particularly in studies with multiphasic protocols, may produce a great exposure to the subjects and that the majority of cases involve young patients.6
Although angiography is necessary to delineate the feeding arteries and draining veins and permits the therapeutic management of some lesions (embolization), it is a very invasive technique. Moreover, therapeutic actions during the diagnostic procedure are rarely possible, especially in cases of large vascular malformations when extensive collateral vascularization is present, providing little effective treatment.6 Although contrast angiography is a reliable method, it is associated with considerable morbidity. MRA of the head and neck offers great promise as a non-invasive method of studying vascular abnormalities and has excellent correlation with the conventional method.16
MRI can be used as an excellent technique in the diagnosis of vascular malformations, either by itself or before angiography with embolization. It offers a good depiction of vascular structures, permitting the differentiation between high-flow and low-flow lesions. High-flow lesions show typical signal flow voids both in T1 weighted and T2 weighted sequences with the appearance of serpentine images. In our case, MRI was able to identify the kind of flow (high-flow lesion) as well as the origin of the vessels. Low-flow lesions also appear as meandering structures characterized by low signal in spin echo T1 sequences, but with moderate and homogeneous signal in T2 images. Multiplanar images provide the depiction of the whole course of abnormal vessels and, with the advent of MRA techniques, the origin of the anomalous branches; they also provide adequate pre-therapeutic planning when the possibilities of embolization is considered.6 On MRI flow voids, hypointense signal intensity on T1 weighted and T2 weighted images and the breaks in hyperintense signal intensity of marrow are pathognomic signs for the AVMs of the jaws.8
On time-resolved MR projection angiography (MRPA), the time between the early arterial phase and enhancement of the malformation could be used to distinguish high- and low-flow lesions. High-flow AVMs showed early intense enhancement. Venous malformations were either not visible on MRPA or showed late enhancement of veins.17
The varix is a pool of blood with high pressure supplied by many fine arterial branches. The varix causes intra-osseous lytic changes, resorption of tooth roots and mobile teeth. When the mobile tooth is extracted or a new tooth is erupted into the varix, brisk bleeding of the varix may happen. The goal of any treatment should be to eliminate the existence of the varix.18
Management of vascular lesions is guided by location, flow characteristics, symptoms, functional disability and cosmetic deformity.19 Smith et al20 reported that the treatment of choice is wide local excision, but in some cases pre-operative embolization may be helpful. Better understanding of the pathophysiology of mandibular AVMs and development of endovascular techniques has altered treatment strategies.21 A multidisciplinary team approach is required in the assessment and treatment of these lesions and involves pre-operative angiography with superselective embolization, followed by resection of the lesion, ideally within 72 h.22
Conclusion
AVMs fail to show a characteristic picture on plain-film radiography. A review of fatal outcomes shows that most exsanguinations are from dental extractions, tooth eruption, incision of a cyst or ameloblastoma, with the dentist being unaware of the existence of AVMs. Although AVM is rare, the operator must always consider it and should add image inspection with new imaging modalities to thoroughly investigate the existence of potential lesions if doubtful conventional radiographic findings are observed, even in the absence of remarkable clinical signs. Consequently, further imaging tests such as CT, MRI and DSA may become essential and intraosseous AVMs should always be included in the differential diagnosis of multilocular radiolucent jaw lesions.
References
- 1.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial eharacteristics. Plas Reconstr Surg 1982;69:412–422 [DOI] [PubMed] [Google Scholar]
- 2.Dodson TB. Symposium on the diagnosis and treatment of vascular lesions. AAOMS 87th Annual Meeting; 20–24 September 2005; Boston, MA. Boston, MA: AAOMS, 2005 [Google Scholar]
- 3.Abramowicz S, Marshall CJ, Dolwick MF, Cohen D. Vascular malformation of the temporomandibular joint: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:203–206. [DOI] [PubMed] [Google Scholar]
- 4.Noreau G, Landry PE, Morais D. Arteriovenous malformation of the mandible: review of literature and case history. J Can Dent Assoc 2001;67:646–651 [PubMed] [Google Scholar]
- 5.Zachariades N, Mezitis M, Rallis G, Panoussis P, Machera H, Velmachou K. Vascular malformation in a 3 ½ year old child. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:271–273 [DOI] [PubMed] [Google Scholar]
- 6.Cappabianca S, Vecchio WD, Giudice A, Colella G. Vascular malformations of the tongue: MRI findings on three cases. Dentomaxillofac Radiol 2006;35:205–208 [DOI] [PubMed] [Google Scholar]
- 7.Wakoh M, Harada T, Yamamoto K, Hashimoto S, Noma H, Kaneko Y. Three-dimensional volumetric visualization of arteriovenous malformation of the maxilla. Dentomaxillofac Radiol 2003;32:63–66 [DOI] [PubMed] [Google Scholar]
- 8.Fan X, Qiu W, Zhang Z, Mao Q. Comparative study of clinical manifestation, plain-film radiography, and computed tomography scan in arteriovenous malformations of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:503–509 [DOI] [PubMed] [Google Scholar]
- 9.Kohout MP, Hansen M, Pribaz JJ, Mulliken JB. Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg 1998;102:643–654 [DOI] [PubMed] [Google Scholar]
- 10.Kawano K, Mizukl H, Mori H, Yanagisawa S. Mandibular arteriovenous malformation treated by transvenous coil embolization: a long–term follow up with a special reference to bone regeneration. J Oral Maxillofac Surg 2001;59:326–330 [DOI] [PubMed] [Google Scholar]
- 11.Wood NK, Goaz PW. Differential diagnosis of oral and maxillofacial lesions. 5th edn. St Louis, MO: Mosby; 1997 [Google Scholar]
- 12.Benndorf G, Kim DM, Menneking H, Klein M. Endovascular management of a mandibular arteriovenous malformation in a patient with severe hemophilia A. Am J Neuroradiol 2004;25:614–617 [PMC free article] [PubMed] [Google Scholar]
- 13.Banna M. Intra-osseous vascular malformation of the mandible. Br J Radiol 1978;51:738–741 [DOI] [PubMed] [Google Scholar]
- 14.Mohammadi H, Said-Al-Naief NAH, Heffez LB. Arteriovenous malformation of the mandible. Report of a case with a note on the differential diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:286–289 [DOI] [PubMed] [Google Scholar]
- 15.Ariji Y, Kimura Y, Gotoh M, Sakuma S, Zhao Y, Ariji E. Blood flow in and around the masseter muscle: normal and pathologic features demonstrated by color Doppler sonography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:472–482 [DOI] [PubMed] [Google Scholar]
- 16.Sreevathsa MR, Lalitha RM, Prasad K. Arteriovenous malformations of the head and neck: experience with magnetic resonance angiography and therapeutic embolization. Br J Oral Maxillofac Surg 2003;41:75–77 [DOI] [PubMed] [Google Scholar]
- 17.Ziyeh S, Schumacher M, Strecker R, Roseller J, Hochmuth A, Klisch J. Head and neck vascular malformations: time resolved MR projection angiography. Neuroradiology 2003;45:681–686 [DOI] [PubMed] [Google Scholar]
- 18.Fan X, Zhang Z, Zhang C, Tang Y, Hu Y, Mao Q, et al. Direct-puncture embolization of intraosseous arterio-venous malformation of jaws. J Oral Maxillofac Surg 2002;60:890–896 [DOI] [PubMed] [Google Scholar]
- 19.Patel SB, Desai A, Desai S, Vias RR, Soni HC. Case report: vascular lesions of face. Ind J Radiol Imaging 2003;13:257–260 [Google Scholar]
- 20.Smith WP, Prince S, Phelan S. The role of imaging and surgery in the management of vascular tumours of the masseter muscle. J Oral Maxillofac Surg 2005;63:1746–1752 [DOI] [PubMed] [Google Scholar]
- 21.Gluncic V, Reid RR, Baroody FM, Gottlieb LJ, Ansari SA. Hemostasis and obliteration of mandibular arteriovenous malformation through direct hydroxyapatite cement injection into the molar cavity. J Neurointerv Surg 2011;3:92–94 [DOI] [PubMed] [Google Scholar]
- 22.Erdmann MWH, Jackson JE, Davies DM, Allison DJ. Multidisciplinary approach to the management of head and neck arteriovenous malformations. Ann R Coll Surg Engl 1995;77:53–59 [PMC free article] [PubMed] [Google Scholar]


