Abstract
Despite the notion that increases in functioning should be associated with increases in life satisfaction in schizophrenia, research has often found no association between the two. Dual change models of global and domain-specific life satisfaction and functioning were examined in 145 individuals with schizophrenia receiving community-based services over 12 months. Functioning and satisfaction were measured using the Role Functioning Scale and Satisfaction with Life Scale. Data were analyzed using latent growth curve modeling. Improvement in global life satisfaction was associated with improvement in overall functioning over time. Satisfaction with living situation also improved as independent functioning improved. Work satisfaction did not improve as work functioning improved. Although social functioning improved, satisfaction with social relationships did not. The link between overall functioning and global life satisfaction provides support for a recovery-based orientation to community based psychosocial rehabilitation services. When examining sub-domains, the link between outcomes and subjective experience suggests a more complex picture than previously found. These findings are crucial to interventions and programs aimed at improving functioning and the subjective experiences of consumers recovering from mental illness. Interventions that show improvements in functional outcomes can assume that they will show concurrent improvements in global life satisfaction as well and in satisfaction with independent living. Interventions geared toward improving social functioning will need to consider the complexity of social relationships and how they affect satisfaction associated with personal relationships. Interventions geared towards improving work functioning will need to consider how the quality and level of work affect satisfaction with employment.
Keywords: Severe mental illness, Schizophrenia, Functioning, Life satisfaction
1. Introduction
Psychosocial functioning and satisfaction with life are widely recognized as important treatment goals and components of recovery in people with severe mental illness (SMI) (Lasalvia et al., 2005; Xie et al., 2005; Bellack, 2006; Yanos and Moos, 2007). While alleviating psychiatric symptoms remains a primary treatment outcome, broadening treatment goals to encompass psychosocial functioning and life satisfaction incorporates multiple stakeholder perspectives on mental health recovery (Resnick et al., 2004; Lasalvia et al., 2005).
Further, it has been argued that psychosocial functioning is a more accurate benchmark to measure treatment outcomes and recovery than clinical outcomes for individuals with SMI (Liberman et al., 2002) and has been widely used to measure outcomes in SMIs like schizophrenia (Brekke et al., 2002; Peer et al., 2007).
Numerous studies have underlined the importance of subjective quality of life as a treatment outcome for individuals with schizophrenia (Bobes and García-Portilla, 2006). As an indicator of subjective quality of life, studies assessing changes in life satisfaction in treatment have reported mixed findings. While some studies reported a significant improvement in life satisfaction levels (Stein and Test, 1982; Rosenheck et al., 1998), other studies reported marginal to no improvement (Tempier et al., 1997; Brekke et al., 1999). Part of this discrepancy may be due to various demographic and clinical factors that affect life satisfaction including age, gender, illness insight, depression, and psychotic symptoms (Karow and Pajonk, 2006; Zissi and Barry, 2006). Another explanation for these divergent findings concerns treating life satisfaction as a global construct. Most measures assessing life satisfaction use global scores or include multiple domains of life satisfaction (i.e., social/family relationships, work, independent living) but use a composite score for analysis. However, improvements in one domain may not necessarily relate to improvements in other domains, as has been found for functional outcomes (Brekke and Long, 2000). Life satisfaction in different domains may change at different rates or times. Consequently, treating life satisfaction as a unidimensional construct measured by global or composite scores may result in the failure to capture important changes in levels of life satisfaction.
Concerning life satisfaction and functioning, there is an underlying assumption that psychosocial interventions improving consumer functioning will also improve life satisfaction. Some studies have found a positive relationship between life satisfaction and social or work functioning (Kemmler et al., 1997; Mueser et al., 1997; Bradshaw and Brekke, 1999). However, the relationship between objective indicators of functioning and subjective indicators of life satisfaction is complex. Perceptions of satisfaction with life may be affected by an appraisal process that includes re-evaluating expectations and aspirations as functioning changes (Zissi and Barry, 2006) thus accounting for studies that find no relationships between the two (Arns and Linney, 1995; Narvaez et al., 2008). Additionally, most studies examining the association between functioning and life satisfaction are cross sectional and may not fully capture the dynamic covarying changes occurring between functioning and life satisfaction over time.
One longitudinal study examined the relationship between specific objective indicators of functioning and specific subjective quality of life domains (Heider et al., 2007). A relationship was found between daily activities, family relations, social relations over a two-year period and corresponding subjective quality of life domains. However, the extent to which specific functioning domains and specific quality of life domains changed together over time was not examined. To address this gap, we sought to build upon the Heider et al. (2007) study in three ways. First, we examined concurrent changes in overall functioning and global life satisfaction for individuals with schizophrenia receiving psychosocial rehabilitation services that target functional improvement. Second, we examined concurrent changes in specific domains of functioning and corresponding life satisfaction domains using distinct measures of functioning and life satisfaction. Finally, we used latent curve modeling which allowed us to analyze covarying change between these variables over time. From previous analyses on this sample we knew that global and domain-specific functioning would improve over time (Brekke et al., 2007), and we expected that there would be improvement in global satisfaction and specific satisfaction domains over time. Specifically, we hypothesized that (1) overall functioning and global life satisfaction would improve together over time, and (2) domain-specific functioning and corresponding domain-specific life satisfaction would improve together over time.
2. Methods
2.1. Participants
Participants were 145 individuals recruited upon admission from four community-based psychosocial rehabilitation programs in Los Angeles, California. In previous studies, the program sites have yielded significant improvements in functional outcomes for individuals with SMI (Bae et al., 2004; Brekke et al., 2007). Participants enrolled in the study met the following criteria for study admission: 1) 18–60 years old and a resident of Los Angeles for at least 3 months prior to study admission, 2) diagnosis of schizophrenia or schizoaffective disorder, and 3) no diagnosis of organic brain disorder, mental retardation, nor a primary diagnosis of substance dependence. Diagnoses were obtained from a DSM-IV checklist, clinical case records and collateral reports from program clinicians and on-site psychiatrists (Brekke et al., 2005; Nakagami et al., 2008). Previous studies conducting structured diagnostic interviews at the program sites have demonstrated very low rates of inaccurate diagnosis for schizophrenia spectrum diagnoses (Bae et al., 2004). In this prospective follow-along design, data were collected from participants at baseline, 6 and 12 months after study admission. Study procedures were conducted with the approval of University of Southern California Institutional Review Board.
2.2. Measures
2.2.1. Satisfaction with Life Scale
The Satisfaction with Life Scale (SWL; Stein and Test, 1980) is an 18-item self-report survey that measures life satisfaction globally and in four domains: living situation, work, social life, and self/present life. Each item is rated on a 5-point Likert-scale from ‘not at all satisfied’ to ‘satisfied a great deal’. The 18-item version of the SWL has excellent construct validity (Test et al., 2005) and is supported in literature as an appropriate measure to assess changes over time in satisfaction with life for individuals with schizophrenia (Lee et al., 2010).
2.2.2. Role Functioning Scale
Our functional outcome measure is the Role Functioning Scale (RFS) (McPheeters, 1984; Goodman et al., 1993; Green and Jerrell, 1994; Wieduwilt and Jerrell, 1998). Its usefulness as a measure of functional change for this population has been detailed (Wieduwilt and Jerrell, 1998). Interviewer ratings of work, independent living, and social functioning from the RFS were used for this study in accordance with procedures reported previously (Brekke et al., 1993; Nakagami et al., 2008). In our protocols the RFS showed high inter-rater reliability with intraclass correlation coefficients ranging from 0.75 to 0.98 (mean of 0.89) for the three RFS domains. Similar to other functional measures, it captures both the quantity and quality of community-based functioning in each domain by providing anchored ratings. The ratings (from 1 to 7) indicate increasing levels of productive activity and independence, with 1 indicating severe dysfunction, and 7 indicating optimal community functioning. For example, in the work domain a rating of 1 indicates an inability to work or no attempts to work; a rating of 4 indicates marginal productivity such as sheltered work or minimal independent work; and a rating of 7 indicates optimal work performance. For this study, individual items as well as a global score (i.e. the sum of the three items) were used. While this scale rates multiple domains, it does so with a single item in each domain, which increases its efficiency. Other functional scales in SMI use multiple items for each domain which can increase their comprehensiveness but reduce their efficiency.
2.3. Analysis
Data analysis was conducted using latent growth curve modeling (Kline, 2005; Bollen and Curran, 2006). First, a latent growth curve model was used to analyze changes in functioning, whereby, three repeated measured functioning scores are represented by two latent growth factors: the intercept (representing initial level of functioning) and the slope (representing change in functioning) (Kline, 2005). A significant slope indicates significant change in functioning over time. Similarly, a latent growth curve model was used to analyze changes in life satisfaction.
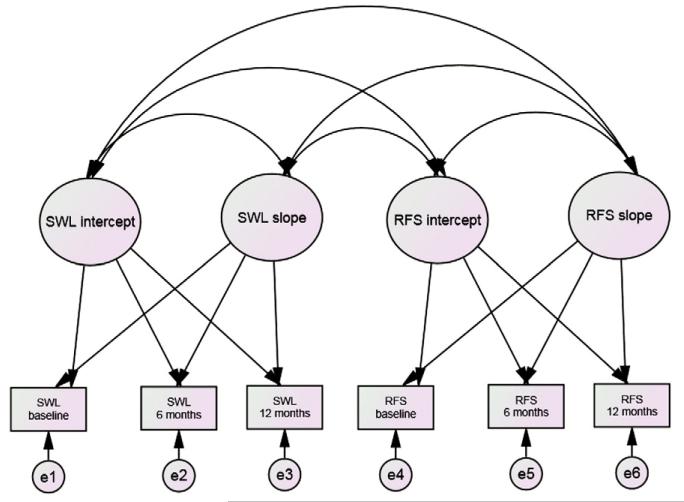
Second, a bivariate latent growth curve model was used to conduct a dynamic latent covariate analysis of functioning and life satisfaction. This allows each construct to have a separate trajectory, but enables testing of covariance of those changes over time (Curran and Willoughby, 2003). In this model, we allowed the change slope of functioning to covary with the change slope of life satisfaction. We called this a dual change model of functioning and life satisfaction (Fig. 1). Dual change models were used to test for covarying changes in (1) overall functioning and global life satisfaction (2) functioning in social relationships and satisfaction with social life (3) functioning in independent living and satisfaction with living situation and (4) work functioning and satisfaction with work.
Fig. 1.
A dual change model of life satisfaction and functioning.
Two criteria were used to determine if significant change occurred over time in all latent growth curve models: model fit and parameter estimates of the change slope. First, model fits were examined using the following indices: Chi-square, Comparative Fit Index (CFI;Bentler, 1990), Tucker-Lewis Index (TLI; Tucker and Lewis, 1973), and Root Mean Square Error of Approximation (RMSEA; Steiger, 1990). A nonsignificant Chi-square indicates a good model fit. For CFI and TLI, a value above .90 indicates an acceptable model fit (Hu and Bentler, 1999). A RMSEA value between .05 and .08 indicates a reasonable fit while values below .05 indicate a close fit to the data (Browne and Cudeck, 1993). When linear models did not show a good fit to the data according to these fit statistics, a nonlinear model was tested. While a linear model explains change over time in the form of a straight line, a non-linear model represents a curvilinear change. For the linear models, factor loadings for the change slope were specified as 0, 6, and 12 to represent baseline, 6-months and 12-months respectively. For the non-linear models, factor loadings for the change slope were specified as 0 and 1 to represent baseline and 12-months (1 year), respectively. The 6-month factor loading was allowed to vary. Second, parameter estimates for the change slopes were examined.
In order to conclude that there was significant dual change occurring over time we required that there be both acceptable model fit and significant change parameter estimates. All analyses were conducted using Amos-17 (Arbuckle, 2009).
3. Results
Table 1 summarizes the demographic and clinical characteristics of the participants. Participants are over 65% male, over 50% are racial/ethnic minorities, and they are largely anti-psychotic medication users with symptom levels that are comparable to other outpatient samples (Brekke et al., 1997; Heinrichs and Zakzanis, 1998).
Table 1.
Demographic and clinical characteristics (n = 145).
| Variable | % | Mean | SD |
|---|---|---|---|
| Gender | |||
| Females | 31.7% | ||
| Males | 68.3% | ||
| Ethnicity | |||
| Euro American | 44.1% | ||
| African American | 38.6% | ||
| Latino | 11% | ||
| Asian | 3.5% | ||
| Other | 2.8% | ||
| Age | 37.91 | 9.16 | |
| Length of illness (years) | 13.68 | 9.98 | |
| BPRSa | 39.22 | 10.42 | |
| # of days on medicationb | 144.49 | 65.27 | |
| 180 days on medication | 68.8% | ||
BPRS = Brief Psychiatric Rating Scale.
In past 180 days.
3.1. Attrition analysis
The total sample size was 145 at baseline, 119 at 6 months, and 106 at 12 months. A series of one-sample t-tests was done on the sociodemographic variables (age, gender, ethnicity length of illness, symptoms, and medication usage) of participants at baseline and 12 months. The baseline and 12-month samples were not found to be statistically significantly different on these baseline variables (p>.05) suggesting no attrition bias on those variables.
3.2. Change in life satisfaction over 12 months
Table 2 shows means and standard deviations of life satisfaction domains at baseline, 6, and 12 months. Overall, we found that global life satisfaction fit a linear model of change (χ2=1.600, df=1, p=0.206, CFI=.992, TLI=.951, RMSEA=.065). A latent growth model of change in subdomains of SWL was examined. Two subdomains of life satisfaction fit the data well. Living situation (χ2=.847, df=1, p=.357, CFI=1.000, TLI=1.041, RMSEA=.000) fit a nonlinear model of change and work fit a linear model of change (χ2=.001, df=1, p=0.969, CFI=1.000, TLI=1.000, RMSEA=.000). Parameter estimates for overall life satisfaction (ß=.161, z=1.710, p=.043), satisfaction with living situation (ß=1.01, z=2.863, p=.002) and satisfaction with work (ß=.025, z=1.741, p=.041) showed a significant change over time. Satisfaction with social relationships did not meet both criteria of model fit and significant parameter estimates for change over time.
Table 2.
Means and standard deviations of functioning and life satisfaction domains at each time point.
| Variable | Baseline | 6 months | 12 months |
|---|---|---|---|
| Independent living functioninga | 3.30 (1.70) | 4.03 (1.76) | 4.16 (1.90) |
| Work functioninga | 1.99 (1.53) | 2.66 (1.88) | 2.58 (1.97) |
| Social functioninga | 2.96 (1.55) | 3.01 (1.69) | 3.37 (1.99) |
| Global functioningb | 8.25 (3.46) | 9.69 (4.17) | 10.10 (4.71) |
| Satisfaction with living situationc | 12.64 (3.23) | 13.58 (3.38) | 13.48 (3.31) |
| Satisfaction with workd | 5.81 (1.80) | 5.97 (1.77) | 6.06 (1.51) |
| Satisfaction with social relationshipse | 18.14 (4.77) | 18.40 (5.09) | 18.37 (4.58) |
| Global satisfactionf | 53.98 (11.60) | 56.25 (12.02) | 55.83 (10.99) |
Measured by RFS subscale: ranges from 1 to 7.
Measured by RFS total score: ranges from 3 to 21.
Measured by SWL living situation subscale: ranges from 4 to 20.
Measured by SWL work subscale: ranges from 2 to 10.
Measured by SWL social relationships subscale: ranges from 6 to 30.
Measured by SWL total scale score: ranges from 18 to 90.
While the statistically significant changes at the global and domain levels are numerically small, the changes in work and global satisfaction scores represent an average change from ‘very little’ satisfaction to ‘average’ satisfaction. To gauge the meaningfulness of these quantitative changes we also used a method outlined by Wieduwilt and Jerrell (1998) for calculating a reliable change index, in which we found that over 58% of our sample showed ‘true improvement’ when analyzing the total SWL score.
3.3. Change in psychosocial functioning over 12 months
Table 2 shows means and standard deviations of functioning domains at baseline, 6, and 12 months. The analysis showed good model fits and significant change over time in all objective indicators of functioning. A linear change model for overall functioning fit the data well (χ2=.954, df=1, p=0.329, CFI=1.000, TLI=1.000, RMSEA=.000). A nonlinear model of change showed an acceptable fit to the data for the three subdomains of functioning: independent living (χ2=1.851, df=1, p=.174, CFI=.992, TLI=.950, RMSEA=.077); social functioning (χ2=1.259, df=1, p=.262, CFI=.997, TLI=.985, RMSEA=.042); and work functioning (χ2=1.463, df=1, p=.226, CFI=.997, TLI=.981, RMSEA=.057). Significant change over time was seen in overall functioning (ß=.161, z=5.455, p<.001), independent living (ß=.845, z=5.542, p<.001), social functioning (ß=.429, z=2.484, p=.006), and work functioning (ß=.684, z=3.880, p<.001).
Using the reliable change index (Wieduwilt and Jerrell, 1998) we found that over 45% of our sample showed ‘true clinical change’ when analyzing the total RFS score. The scale anchors provide another gauge of meaningfulness. For example, the data on work functioning would suggest that our sample generally moves from a baseline average score of 2 with the top of the first S.D. at 3.5, to an average score at 12 months of nearly a 3, with the top of the first S.D. at 4.5. When using the RFS anchors, the baseline score reflects “occasional attempts at productivity unsuccessful” up to “limited productivity in structured setting”. At 12 months the score anchors reflect “limited productivity in structured setting” up to “productive in sheltered or minimally productive in independent settings”.
3.4. Dual change models of functioning and life satisfaction
In order to conclude that there was significant dual change occurring over time we required that there be both acceptable model fit and significant change parameter estimates. These two conditions were met for global satisfaction with life and overall functioning (χ2=6.21, df=7, p=0.52, CFI=1.00, TLI=1.00, RMSEA=0.00), and for satisfaction with living situation and functioning in independent living (χ2=2.955, df=7, p=.889, CFI=1.000, TLI=1.061, RMSEA=.000). Change parameter estimates (slopes and correlations between slopes) for overall life satisfaction and overall functioning were significant also indicating that these two domains improved together over time (Table 3). The same held for satisfaction with living situation and independent living functioning (Table 3). Satisfaction with work and work functioning showed a reasonable fit to the data (χ2=11.413, df=7, p=.122, CFI=.971, TLI=.912, RMSEA=.066); however, satisfaction with work did not improve as work functioning improved over time (Table 3). Finally, because satisfaction with social life did not improve over time, a dual change model including social functioning and satisfaction with social life was not tested.
Table 3.
Change slope estimates for dual change models.
| Corresponding domains | ß | z | Correlation between slopes |
|---|---|---|---|
| SWL total and RFS total | 0.13** | 3.82 | .63 |
| SWL living situation and RFS independent living |
2.30** | 3.63 | .61 |
| SWL work and RFS work | .02 | .82 | .19 |
Note: SWL = Satisfaction with Life Scale; RFS = Role Functioning Scale.
p<.01.
4. Discussion
There is limited literature on how satisfaction with life and psychosocial functioning are related over time for individuals with schizophrenia. This study examined the degree to which changes in functioning and life satisfaction were linked for individuals with schizophrenia receiving community-based psychosocial rehabilitation. These linkages underlie assumptions of psychosocial rehabilitation and recovery oriented treatment methods.
Our results demonstrated the association between changes in the subjective experience of global life satisfaction and changes in overall functioning. This is significant in that it shows at the global level that increases in psychosocial functioning will be accompanied by improvements in life satisfaction. In addition, we found that covarying changes in life satisfaction and functioning varied according to specific domains. Specifically, satisfaction with living situation and functioning in independent living were found to increase together over time. Work satisfaction did not significantly improve as work functioning improved. Although social functioning improved, satisfaction with social relationships did not improve over time.
Given that many individuals with schizophrenia receiving community-based psychosocial rehabilitation enter treatment with housing needs and limited skills in independent living, it is not surprising that our sample showed improvement in independent living and satisfaction with living situation. Assisting consumers in finding stable, suitable housing and increasing skills to live independently are among the primary goals of rehabilitation programs and key components in recovery from mental illness (Liberman, 2008). This finding also supports the literature on Assertive Community Treatment that shows that improvement in housing has a significant impact on life satisfaction (Bond et al., 2001).
While significant increases in psychosocial functioning domains have been reported in studies of individuals with schizophrenia receiving psychosocial rehabilitation services, we found that those expected improvements in functioning were not reflected in all corresponding areas of life satisfaction. Our results indicated that although social functioning improved, satisfaction with social relationships did not significantly improve over time. Considering consumers with schizophrenia tend to suffer decreased capacity to experience pleasure in social interaction (Blanchard et al., 2001), these results are not surprising. This is possibly related to the complex, multi-dimensional nature of social relationships. The RFS social functioning domain did not provide enough information about the relative importance consumers place on different dimensions of social relationships. The SWL social relationship domain does include specific items about satisfaction with the frequency and quality of contact with opposite sex, the number of and closeness to friends, quality of family relationship, and leisure activities. However, these items were used as unweighted composite scores and hence, are limited in providing information about changes in specific areas of satisfaction with social relationships as it relates to changes in social functioning.
In addition, other variables such as neurocognition, social cognition, affective state, illness insight, and innate personality traits may mediate or moderate the relationship between functioning and life satisfaction in individuals with schizophrenia (Brekke et al., 2001). Furthermore, psychotic symptoms and depressed mood have both been associated with lower satisfaction with life and may partially explain the lower levels of satisfaction with social relationships found in our sample (Brekke et al., 1993; Blanchard et al., 2001; Huppert et al., 2001; Reine et al., 2003).
From the provider’s and client’s point of view, work is also seen as a critical step in the recovery process (Provencher et al., 2002). However, our results indicated that participants were not satisfied with an increase in work functioning. This may be related to factors not captured in changes in work functioning including work-related stress or the low level and quality of work experiences available to individuals with schizophrenia (Becker et al., 1998; Koletsi et al., 2009). Other studies have shown that individuals with schizophrenia report high levels of satisfaction when placed in employment opportunities that match their work preferences (Mueser et al., 2001), but this effect might also be transient and time limited (Torrey et al., 2000).
This study has implications for mental health practice and research. Covarying change between psychosocial functioning and life satisfaction can inform interventions and programs aimed not only at improving functioning but also the subjective experiences of consumers recovering from mental illness. Furthermore, interventions aimed at improving overall and independent functioning can assume that they will show change in overall life satisfaction and satisfaction with living situation respectively. Services targeting social functioning may need to focus on the specific aspects of social relationships that concern consumers the most to provide individually tailored intervention. Services designed to improve work functioning will also need to consider other factors that influence satisfaction with work such as symptomatology, quality of work placements, and increased support to cope with work-related stress.
This study has a several limitations. First, our study represents an outpatient sample of individuals with schizophrenia that are higher functioning and treatment seeking, which may not generalize to other clinic populations. Second, the sample size is small for the statistical method used. Third, more time point observations could have more adequately captured the relationship between life satisfaction and functioning over time. Finally, although we only talked about dual change in the context of whole group, there is heterogeneity within the group in terms of their changes in the level of psychosocial functioning and life satisfaction. Identifying subgroup differences would be beneficial in providing more finely tuned interventions.
Future studies should examine the factors influencing the dual change process. This includes examining global factors such as neurocognition and symptom levels that may influence evaluation of satisfaction in any of the domains. In addition, specific factors related to satisfaction in specific domains, such as work-related factors, should be considered. Understanding the mechanisms that influence the dual change process of functioning and life satisfaction will contribute to increasing the effectiveness of interventions that promote recovery for individuals with schizophrenia. Finally, outcome research should examine global functioning and satisfaction indicators, but also specific domains so that the full picture of functioning and life satisfaction can be understood.
Acknowledgments
This work was supported by an NIMH grant R-01 MH53282: Predicting Psychosocial Rehabilitation Service Outcomes (J. Brekke, PI).
Role of funding source
Funded by National Institute of Mental Health R-01 MH 53282: Predicting Psychosocial Rehabilitation Service Outcomes awarded to J. Brekke.
Footnotes
Contributors
Melissa Edmondson: Conceptualized the paper, literature review, wrote sections of the introduction, edited introduction, wrote methods; edited results and wrote discussion sections, edited manuscript drafts.
Rohini Pahwa: Conceptualized the paper, literature review, wrote sections of the introduction; conducted the analysis; wrote results; helped write discussion sections.
Karen Kyeunghae Lee: Conceptualized the paper, literature review, wrote sections of the introduction; helped write discussion section.
Maanse Hoe: Statistical consulting, edited methods and results section.
John Brekke: Conducted and supervised the study as PI, conceptualized and helped write paper, did final over-all editing.
Conflict of interest
Melissa Edmondson: No actual or potential conflict of interest.
Rohini Pahwa: No actual or potential conflict of interest.
Karen Lee: No actual or potential conflict of interest.
Maanse Hoe: No actual or potential conflict of interest.
John Brekke: No actual or potential conflict of interest.
References
- Arbuckle JL. Amos 17 User’s Guide. Small Waters; Chicago, IL: 2009. [Google Scholar]
- Arns PG, Linney JA. Relating functional skills of severely mentally ill clients to subjective and societal benefits. Psychiatr. Serv. 1995;46:260–265. doi: 10.1176/ps.46.3.260. [DOI] [PubMed] [Google Scholar]
- Bae SW, Brekke JS, Bola JR. Ethnicity and treatment outcomes in schizophrenia: a longitudinal study of community-based psychosocial rehabilitation interventions. J. Nerv. Ment. Dis. 2004;192:623–628. doi: 10.1097/01.nmd.0000140035.36075.7f. [DOI] [PubMed] [Google Scholar]
- Becker DR, Drake RE, Bond GR, Xie H, Dain BJ, Harrison K. Job terminations among persons with severe mental illness participating in supported employment. Community Ment. Health J. 1998;34:71–81. doi: 10.1023/a:1018716313218. [DOI] [PubMed] [Google Scholar]
- Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr. Bull. 2006;32:432–442. doi: 10.1093/schbul/sbj044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychol. Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Horan WP, Brown SA. Diagnostic differences in social anhedonia: a longitudinal study of schizophrenia and major depressive disorder. J. Abnorm. Psychol. 2001;110:363–371. doi: 10.1037//0021-843x.110.3.363. [DOI] [PubMed] [Google Scholar]
- Bobes J, García-Portilla MP. Quality of life in schizophrenia. In: Katschnig H, Freeman H, Sartorius N, editors. Quality of Life in Mental Disorders. 2nd ed. John Wiley & Sons Ltd.; New York: 2006. pp. 153–167. [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Approach. Wiley; Hoboken, N.J.: 2006. [Google Scholar]
- Bond GR, Drake RE, Mueser KT, Latimer E. Assertive community treatment for people with severe mental illness: critical ingredients and impact on clients. Dis. Manag. Health Outcomes. 2001;9:141–159. [Google Scholar]
- Bradshaw W, Brekke J. Subjective experience in schizophrenia: factors influencing self esteem, satisfaction with life, and subjective distress. Am. J. Orthopsychiatry. 1999;69:254–260. doi: 10.1037/h0080427. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Long JD. Community-based psychosocial rehabilitation and prospective change in functional, clinical, and subjective experience variables in schizophrenia. Schizophr. Bull. 2000;26(3):667–680. doi: 10.1093/oxfordjournals.schbul.a033485. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Levine S, Wolkon G, Sobel G, Slade B. Psychosocial functioning and subjective experience in schizophrenia. Schizophr. Bull. 1993;19:599–608. doi: 10.1093/schbul/19.3.599. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Long JD, Nesbitt N, Sobel E. The impact of service characteristics on functional outcomes from community support programs for persons with schizophrenia: a growth curve analysis. J. Consult. Clin. Psychol. 1997;65(3):464–475. doi: 10.1037//0022-006x.65.3.464. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Ansel M, Long J, Slade E, Weinstein M. Intensity and continuity of services and functional outcomes in the rehabilitation of persons with schizophrenia. Psychiatr. Serv. 1999;50:248–256. doi: 10.1176/ps.50.2.248. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Kohrt B, Green MF. Neuropsychological functioning as a moderator of the relationship between psychosocial functioning and the subjective experience of self and life in schizophrenia. Schizophr. Bull. 2001;27(4):697–708. doi: 10.1093/oxfordjournals.schbul.a006908. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Long JD, Kay DD. The structure and invariance of a model of social functioning in schizophrenia. J. Nerv. Ment. Dis. 2002;190(2):63–72. doi: 10.1097/00005053-200202000-00001. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Kay DD, Lee KL, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr. Res. 2005;80:213–225. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Hoe M, Long J, Green MF. How neurocognition and social cognition influence functional change during community-based psychosocial rehabilitation for individuals with schizophrenia. Schizophr. Bull. 2007;33:1247–1256. doi: 10.1093/schbul/sbl072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Browne MW, Cudeck R, Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage; Newbury Park, CA: 1993. pp. 154–162. [Google Scholar]
- Curran PJ, Willoughby MT. Implications of latent trajectory models for the study of developmental psychopathology. Dev. Psychopathol. 2003;15:581–612. doi: 10.1017/s0954579403000300. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: the role functioning scale. Community Ment. Health J. 1993;29:119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- Green RS, Jerrell JM. The generalizability of brief ratings of psychosocial functioning. Eval. Program Plann. 1994;17:141–151. [Google Scholar]
- Heider D, Angermeyer MC, Winkler I, Schomerus G, Bebbington PE, Brugha T, Azorin JM, Toumi M. A prospective study of quality of life in schizophrenia in three European countries. Schizophr. Res. 2007;93:194–202. doi: 10.1016/j.schres.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–445. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6:1–55. [Google Scholar]
- Huppert JD, Weiss KA, Lim R, Pratt S, Smith TE. Quality of life in schizophrenia: contributions of anxiety and depression. Schizophr. Res. 2001;51:171–180. doi: 10.1016/s0920-9964(99)00151-6. [DOI] [PubMed] [Google Scholar]
- Karow A, Pajonk FG. Insight and quality of life in schizophrenia: recent findings and treatment implications. Curr. Opin. Psychiatry. 2006;19:637–641. doi: 10.1097/01.yco.0000245754.21621.c9. [DOI] [PubMed] [Google Scholar]
- Kemmler G, Holzner B, Neudorfer C, Meisue U, Hinterhuber H. General life satisfaction and domain-specific quality of life in chronic schizophrenic patients. Qual. Life Res. 1997;6:265–273. doi: 10.1023/a:1026466906643. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed. Guilford Press; New York: 2005. [Google Scholar]
- Koletsi M, Niersman A, van Busschback JT, Catty J, Becker T, Burns T, Fioritti A, Kalkan R, Lauber C, Rossler W, Tomov T, Wierma D. Working with mental health problems: clients experiences of IPC, vocational rehabilitation and employment. Soc. Psychiat. Epidemiol. 2009;44:961–970. doi: 10.1007/s00127-009-0017-5. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Bonetto C, Malchiodi F, Salvi G, Parabiaghi A, Tansella M, Ruggeri M. Listening to patients’ needs to improve their subjective quality of life. Psychol. Med. 2005;35:1655–1665. doi: 10.1017/S0033291705005611. [DOI] [PubMed] [Google Scholar]
- Lee KK, Brekke JB, Yamada AM, Cho CP. Longitudinal invariance of the satisfaction with life scale for individuals with schizophrenia. Res. Soc. Work. Pract. 2010;20:234–241. [Google Scholar]
- Liberman PL. Recovery from Disability: Manual of Psychiatric Rehabilitation. American Psychiatric Publishing Inc.; Arlington, VA: 2008. [Google Scholar]
- Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int. Rev. Psychiatry. 2002;14:256–272. [Google Scholar]
- McPheeters HL. Statewide mental health outcome evaluation: a perspective of two southern states. Community Ment. Health J. 1984;20:44–55. doi: 10.1007/BF00754103. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Becker DR, Torrey WC, Haiyi X, Bond GR, Drake RE, Bradley DJ. Work and nonvocational domains of functioning in persons with severe mental illness: a longitudinal analysis. J. Nerv. Ment. Dis. 1997;185:419–426. doi: 10.1097/00005053-199707000-00001. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Becker DR, Wolfe R. Supported employment, job preferences, job tenure and satisfaction. J. Ment. Health. 2001;10(4):411–417. [Google Scholar]
- Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizophr. Res. 2008;105:95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Narvaez JM, Twamley EW, McKibbin CL, Heaton RK, Patterson TL. Subjective and objective quality of life in schizophrenia. Schizophr. Res. 2008;98:201–208. doi: 10.1016/j.schres.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peer JE, Kupper Z, Long JD, Brekke JS, Spaulding WD. Identifying mechanisms of treatment effects and recovery in rehabilitation of schizophrenia: longitudinal analytic methods. Clin. Psychol. Rev. 2007;27(6):696–714. doi: 10.1016/j.cpr.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Provencher HL, Gregg R, Mead S, Mueser KT. The role of work in the recovery of persons with psychiatric disabilities. Psychiatr. Rehabil. J. 2002;26:132–144. doi: 10.2975/26.2002.132.144. [DOI] [PubMed] [Google Scholar]
- Reine G, Lançon C, Di Tucci S, Sapin C, Auquier P. Depression and subjective quality of life in chronic phase schizophrenic patients. Acta Psychiatr. Scand. 2003;108(4):297–303. doi: 10.1034/j.1600-0447.2003.00132.x. [DOI] [PubMed] [Google Scholar]
- Resnick SG, Rosenheck RA, Lehman AF. An exploratory analysis of correlates of recovery. Psychiatr. Serv. 2004;55:540–547. doi: 10.1176/appi.ps.55.5.540. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Tekell J, Peters J, Cramer J, Foutana A, Xu W, Thomas J, Henderson W, Charney D. Does participation in psychosocial treatment augment the benefit of clozapine? Arch. Gen. Psychiatry. 1998;55:618–625. doi: 10.1001/archpsyc.55.7.618. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivar. Behav. Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Stein LI, Test MA. Alternative to mental hospital treatment, I: Conceptual model, treatment, program and clinical evaluation. Arch. Gen. Psychiatry. 1980;37:392–397. doi: 10.1001/archpsyc.1980.01780170034003. [DOI] [PubMed] [Google Scholar]
- Stein LI, Test MA. Community treatment of the young adult patient. New Dir. Ment. Health Serv. 1982;14:57–67. [Google Scholar]
- Tempier R, Mercier C, Leouffre P, Caron J. Quality of life and social integration of severely mentally ill patients: a longitudinal study. J. Psychiatry Neurosci. 1997;22(4):249–255. [PMC free article] [PubMed] [Google Scholar]
- Test MA, Greenberg JS, Long JD, Brekke JS, Burke SS. Construct validity of a measure of subjective satisfaction with life of adult with serious mental illness. Psychiatr. Serv. 2005;56:292–300. doi: 10.1176/appi.ps.56.3.292. [DOI] [PubMed] [Google Scholar]
- Torrey WC, Mueser KT, McHugo GH, Drake RE. Self-esteem as an outcome measure in studies of vocational rehabilitation for adults with severe mental illness. Psychiatr. Serv. 2000;51:229–233. doi: 10.1176/appi.ps.51.2.229. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Wieduwilt KM, Jerrell JM. Measuring the sensitivity to change of the role functioning scale through the utilization of the RCID index. Int. J. Methods Psychiatr. Res. 1998;7:163–170. [Google Scholar]
- Xie H, McHugo GJ, Helmstetter BS, Drake RE. Three-year recovery outcomes for long-term patients with co-occurring schizophrenic and substance use disorders. Schizophr. Res. 2005;75:337–348. doi: 10.1016/j.schres.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Yanos PT, Moos RH. Determinants of functioning and well-being among individuals with schizophrenia: an integrated model. Clin. Psychol. Rev. 2007;27:58–77. doi: 10.1016/j.cpr.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zissi A, Barry MM. Well-being and life satisfaction as components of quality of life in mental disorders. In: Katschnig H, Freeman H, Sartorius N, editors. Quality of Life in Mental Disorders. 2nd ed. John Wiley & Sons Ltd.; New York: 2006. pp. 33–44. [Google Scholar]