Abstract
Background
The provision of intrauterine devices (IUDs) immediately postabortion has the potential to decrease unintended pregnancy in the United States. Studies have demonstrated safety and efficacy; however, there are limited data about continuation, satisfaction, and bleeding patterns among women receiving immediate postabortion IUDs.
Study Design
We performed a retrospective cohort study of women undergoing immediate postabortion IUD insertion. Demographics and clinical data were collected from intake forms and procedure notes. We attempted to contact women by telephone to administer a short questionnaire to assess continuation, satisfaction, and bleeding patterns.
Results
We were able to contact 77 of 225 (34%). Women lost to follow-up were more likely to have higher parity or a pregnancy of greater gestational age at the time of abortion compared with women who were successfully contacted. Continuation and satisfaction rates were high (80.5% and 80.6%, respectively). Reported bleeding patterns with IUD use were similar to previously reported patterns.
Conclusion
Follow-up of women undergoing immediate postabortion IUD insertion is challenging. However, we found that women choosing immediate postabortion IUD had high rates of continuation and satisfaction.
Introduction
Unintended pregnancies account for nearly half of all pregnancies in the United States each year, and more than 40% of these end in induced abortion (Finer & Henshaw, 2006). The use of highly effective contraception decreases the incidence of unintended pregnancy. Immediate postabortion intrauterine device (IUD) insertion has been shown to decrease the rate of repeat abortion (Heikinheimo, Gissler, & Suhonen, 2008). A 2008 study showed that women who received immediate postabortion IUDs had a lower rate of repeat abortion (hazard ratio, 0.38; 95% confidence interval, 0.27–0.53; Goodman et al., 2008).
The safety and efficacy of IUDs, as well as high rates of satisfaction and continuation, have been clearly demonstrated. A 3-year study investigating continuation and acceptability of the levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena, Bayer HealthCare Pharmaceuticals, Wayne, NJ) found a continuation rate of 90% at 36 months with 77% of women reporting they were very satisfied with the method (Baldaszti, Wimmer-Puchinger, & Loschke, 2003). Twelve-month continuation and satisfaction data from the Contraceptive CHOICE Project, an observational cohort study designed to promote long-acting, reversible contraception, showed a 1-year continuation rate of 88% for LNG-IUS users and 84% for copper IUD (ParaGard, Barr Pharmaceuticals, Montvale, NJ) users. Satisfaction rates for all IUD users were greater than 80% (Peipert et al., 2011).
Multiple studies have demonstrated safety and efficacy of the IUD (Beatty & Blumenthal, 2009; Kulier, O’Brien, Helmerhorst, Usher-Patel, & D’Arcangues, 2007; O’Brien, Kulier, Helmerhorst, Usher-Patel, & d’Arcangues, 2008; Rivera & Best, 2002). Safety and efficacy also have been established in women undergoing immediate postabortion IUD insertion, with similarly low rates of perforation and pelvic inflammatory disease when compared with interval insertions (Grimes, Lopez, Schulz, & Stanwood, 2010). An increased rate of IUD expulsion has been reported with immediate postabortion insertion, which is associated with increasing gestational age at the time of the induced abortion (O’Brien et al., 2008). However, there are few studies evaluating long-term continuation and satisfaction with immediate postabortion IUD insertion. In part, this may be because of the challenges of recruiting abortion patients into research studies as well as successfully following patients postabortion (Madden & Westhoff, 2009). Stanek, Bednarek, Nichols, Jensen, & Edelman (2009) reported that, among women desiring an IUD for postabortion contraception, 67% preferred immediate postabortion insertion. They also reported that the additional visit required for an interval placement was the principal barrier to IUD insertion. Bednarek and colleagues (2011) showed that women who were randomized to immediate postaspiration insertion were more likely to both receive and continue IUD use.
We undertook this study to determine patient satisfaction, continuation, and bleeding profiles with postabortion IUD insertion using retrospective data collection. We also undertook this study to determine the feasibility of collecting such data on a population that has been shown in the past to be difficult to study.
Materials and Methods
We performed a retrospective cohort study of 225 women who underwent immediate postabortion IUD insertion after a first- or second-trimester surgical abortion between July 2007 and April 2008 at a single urban family planning clinic. This was the first 10 months that we offered immediate postabortion IUD insertion at this clinic site. Potential participants were not enrolled in a research study at the time of the IUD insertion, but were contacted retrospectively. After undergoing standard contraceptive counseling, women who desired an IUD could choose either the LNG-IUS or the copper IUD. During this period, financial assistance was available to help with the cost of the IUD.
Each patient was counseled about her contraceptive options before the abortion as part of standard clinic protocol. The risks, benefits, and side effects of each type of contraception were discussed. First-trimester surgical abortions were performed with manual or electric aspiration according to physician preference. Second-trimester abortions were performed by dilation and evacuation. Misoprostol or osmotic dilators were used for cervical ripening according to physician preference. Laboratory testing for Chlamydia trachomatis and Neisseria gonorrhoeae was performed on urine samples by nucleic acid amplification.
Women eligible for this study were aged 18 to 45 years, undergoing a surgical abortion in the first or second trimester, and receiving an immediate postabortion insertion of the LNG-IUS or the copper IUD. We reviewed all charts from this time period to identify eligible women. Women were only considered eligible if their intake form indicated a willingness to be contacted at a later date. Demographics and clinical data were extracted from the questionnaire and procedure notes, respectively. We made a minimum of three attempts by telephone to contact each woman. If more than one telephone number was provided, three attempts were made to each number. Phone calls were placed at least once during three different time windows: Daytime, evenings, and weekends. All phone calls were made from an unlisted telephone number preventing identification by caller ID.
We administered a short questionnaire to the women we contacted asking about continued IUD use and satisfaction with the IUD if she reported continued use. Satisfaction was reported on a 5-point Likert scale. Reported values of 1 and 2 were coded as not satisfied, a value of 3 was considered neutral, and values of 4 and 5 were considered satisfied. Satisfaction was also ascertained by asking women if they would recommend the method to a friend. We assessed side effects associated with the IUD in several ways. The presence of irregular bleeding was assessed with participant report (yes/no) and further quantified with average number of bleeding/spotting days per month. Change in menstrual flow (lighter, heavier, no change) or pain with menses (improved, worse, no change) were also documented. Last, we asked whether the patient had been diagnosed with an infection since insertion, and if so, what infection was also noted. Those participants who were no longer using the IUD were asked if they were using another method of contraception, and if so, which method. All questionnaires were administered by a single member of the research team.
Statistical Methods
We performed Fischer’s exact, chi-square, or Student’s t-tests to identify demographic differences between the women we successfully contacted and those we were unable to contact. The median gestational age (approximated in weeks at the time of induced abortion) and the median duration of IUD use were analyzed using the median two-sample test. All statistical analysis was performed using Stata 10 (StataCorp LP, College Station, TX). Approval was obtained from the Human Research Protection Office at Washington University in Saint Louis for this study.
Results
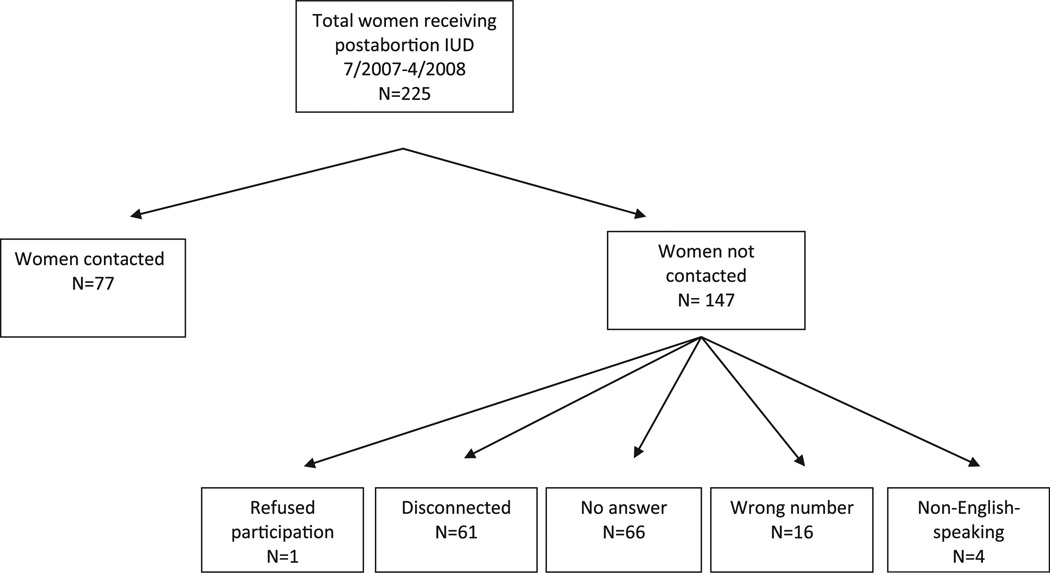
We were able to reach 77 of 225 potential participants (34%) with multiple attempts (Figure 1) at telephone contact. Of the 147 women whom we were unable to contact, 61 (41.2%) had a disconnected telephone number, 66 (44.6%) did not answer any of the telephone calls despite having a working number, 16 (10.8%) had provided incorrect telephone numbers in the medical record, and four (2.7%) were non-English-speaking. One woman refused to participate.
Figure 1.
Postabortion IUD follow-up contact rates.
In comparing the demographic and behavioral characteristics of contacted women with those we were unable to contact, there were no differences in age, race, educational level, marital status, history of prior abortion, type of IUD, or presence of gonorrhea or chlamydia infection in the two groups (Tables 1 and 2). Women successfully contacted were more likely to have two or fewer children (89.6% vs. 72.3%; p < .01), and be at an earlier gestational age at the time of their abortion (61.6 vs. 71.2 days; p < .01). The median duration of time from postabortion IUD insertion to telephone contact was 9 months (range, 6–17). Overall, 80.5% (62/77) of those contacted reported continued use of IUD at follow-up and 80.6% (50/62) reported being satisfied or very satisfied (values of 4 or 5) with the IUD.
Table 1.
Demographics
| Total (n = 225) | Contacted (n = 77) | Not Contacted (n = 148) | p-Value | |
|---|---|---|---|---|
| Age, mean (SD) | 26.3 (6.1) | 27.2 (7.1) | 25.8 (5.6) | .11 |
| Race, n (%) | .15 | |||
| Black | 90 (40.7) | 25 (33.8) | 65 (44.2) | |
| White | 120 (54.3) | 43 (58.1) | 77 (52.4) | |
| Other | 11 (5.0) | 6 (8.1) | 5 (3.4) | |
| Missing | 4 | 3 | 1 | |
| Education, n (%) | .33 | |||
| <12th grade | 45 (21.3) | 13 (17.6) | 32 (23.4) | |
| ≥ 12th grade | 166 (78.7) | 61 (82.4) | 105 (76.6) | |
| Missing | 14 | 3 | 11 | |
| Marital status, n (%) | .30 | |||
| Never married | 142 (64.5) | 44 (57.9) | 98 (68.1) | |
| Married | 42 (19.1) | 18 (23.7) | 24 (16.7) | |
| Divorced/separated | 36 (16.4) | 14 (18.4) | 22 (15.3) | |
| Missing | 5 | 1 | 4 | |
| Employed, n (%) | .20 | |||
| Yes | 128 (63.7) | 44 (62.0) | 84 (64.6) | |
| No | 52 (25.9) | 16 (22.5) | 36 (27.7) | |
| Student | 21 (10.4) | 11 (15.5) | 10 (7.7) | |
| Missing | 24 | 6 | 18 | |
| Gravidity, n (%) | .07 | |||
| 1–2 | 71 (31.6) | 28 (36.4) | 43 (29.1) | |
| 3–5 | 112 (49.8) | 41 (53.2) | 71 (48.0) | |
| ≥ 6 | 42 (18.7) | 8 (10.4) | 34 (23.0) | |
| Parity, n (%) | .01 | |||
| 0 | 37 (16.4) | 14 (18.2) | 23 (15.5) | |
| 1–2 | 139 (61.8) | 55 (71.4) | 84 (56.8) | |
| 3 | 49 (21.8) | 8 (10.4) | 41 (27.7) | |
| History of abortions, n (%) | .30 | |||
| No | 109 (48.4) | 41 (53.2) | 68 (45.9) | |
| Yes | 116 (51.6) | 36 (46.8) | 80 (54.1) | |
| Estimated gestational age in weeks, median (range) | 9 (4–20) | 8 (5–19) | 9 (4–20) | <.01 |
| Sexually transmitted infection at time of insertion, n (%) | .84* | |||
| None | 118 (91.5) | 46 (93.9) | 72 (90.0) | |
| CT positive | 10 (7.8) | 3 (6.1) | 7 (8.8) | |
| GC positive | 1 (0.8) | 0 (0.0) | 1 (1.3) | |
| Missing, n (%) | 96 | 28 | 68 | |
| Type of IUD, n (%) | .85 | |||
| LNG-IUS | 153 (68.0) | 53 (68.8) | 100 (67.6) | |
| Copper IUD | 72 (32.0) | 24 (31.2) | 48 (32.4) |
Abbreviations: IUC, intrauterine contraception; IUD, intrauterine device; LNG-IUS, levonorgestrel-releasing intrauterine system.
Fisher’s exact test.
Table 2.
Characteristics of the Contacted Participants Stratified by IUC Type (n = 77)
| Total (n = 77) |
LNG-IUS (n = 53) |
Copper-IUD (n = 24) |
p-Value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| IUD in place | .77* | ||||||
| No | 15 | 19.5 | 11 | 20.8 | 4 | 16.7 | |
| Yes | 62 | 80.5 | 42 | 79.2 | 20 | 83.3 | |
| Satisfaction among continuous user | .99* | ||||||
| Not satisfied (1–2) | 2 | 3.2 | 2 | 4.8 | 0 | 0 | |
| Neutral (3) | 10 | 16.1 | 7 | 16.7 | 3 | 15.0 | |
| Satisfied (4–5) | 50 | 80.6 | 33 | 78.7 | 17 | 85.0 | |
| Irregular bleeding | .37 | ||||||
| No | 35 | 46.7 | 22 | 43.1 | 13 | 54.2 | |
| Yes | 40 | 53.3 | 29 | 56.9 | 11 | 45.8 | |
| Missing | 2 | 2 | 0 | ||||
| Menses comparison | <.01* | ||||||
| Lighter | 40 | 53.3 | 39 | 76.5 | 1 | 4.2 | |
| Heavier | 18 | 24.0 | 2 | 3.9 | 16 | 66.7 | |
| Same | 17 | 22.7 | 10 | 19.6 | 7 | 29.2 | |
| Missing | 2 | 2 | 0 | ||||
| Period pain | .05* | ||||||
| More | 25 | 33.3 | 14 | 27.5 | 11 | 45.8 | |
| Less | 27 | 36.0 | 23 | 45.1 | 4 | 16.7 | |
| Same | 23 | 30.7 | 14 | 27.5 | 9 | 37.5 | |
| Missing | 2 | 2 | 0 | ||||
| Infection | .53* | ||||||
| No | 75 | 97.4 | 52 | 98.1 | 23 | 95.8 | |
| Yes | 2 | 2.6 | 1 | 1.9 | 1 | 4.2 | |
| Expulsions | .99* | ||||||
| No | 73 | 94.8 | 50 | 94.3 | 23 | 95.8 | |
| Yes | 4 | 5.2 | 3 | 5.6 | 1 | 4.2 | |
Abbreviations: IUC, intrauterine contraception; IUD, intrauterine device; LNG-IUS, levonorgestrel-releasing intrauterine system.
Fisher’s exact test.
Continuation did not differ between the LNG-IUS and the copper IUD; 79.2% of LNG-IUS users (n = 53) and 83.3% of copper IUD users (n = 24) were still using their method (p = .77). Rates of satisfaction among women continuing their IUD were similar among participants in each group (78.7% LNG-IUS and 85.0% copper IUD; p = .99).
The presence of irregular bleeding did not differ between groups with 29 out of 53 (56.9%) in the LNG-IUS and 11 of 24 (45.8%) in the copper IUD responding affirmatively (p = .37). However, the perception of menstrual flow and dysmenorrhea differed when participants compared their current bleeding pattern with their pre-IUD pattern. Predictably, LNG-IUS users were more likely to report lighter menses (39/53; 76.5%) compared with just 1 of 24 (4.2%) copper IUD users (p < .01). Twenty-three of 53 LNG-IUS users (45.1%) reported less painful menses compared with 4 of 24 copper IUD users (16.7%; p = .05). By contrast, 66.7% (16/24) copper IUD users reported heavier menses compared with 3.9% (2/53) LNG-IUS users (p < .01). Similarly, 45.8% (11/24) of copper IUD users reported more painful menses as compared with 27.5% (14/53) of LNG-IUS users (p = .05). There were no differences in the rate of self-reported expulsion between the two IUDs; three expulsions (5.6%) occurred in LNG-IUS users and one (4.2%) in copper IUD users (p = .63). Last, there was no difference in reported pelvic infections with one infection reported in each group (p = .53).
Discussion
Our findings support prior studies that show high rates of continuation and satisfaction with immediate postabortion IUD insertion. Drey and colleagues (2000) also found high rates of continuation and satisfaction among women who had undergone immediate postabortion IUD insertion; 74.2% women reported continuing the IUD and 93.8% of those women reported being satisfied. However, the mean time to follow-up in this study was only 8 weeks. Although our study had low follow-up rates, it does add to these findings and shows high rates of continuation among women contacted with a longer mean follow-up time of 9 months.
Women who were contacted were more likely to have fewer children and present for their abortion at an earlier gestational age. This may reflect increasing stigma associated with abortion at advancing gestational ages. It may also be attributed to the increased level of stress and more chaotic schedules that women with more children have.
Although bleeding patterns reported by the LNG-IUS and copper IUD users reflected the expected changes reported in other studies, one limitation of our study is the wide range of follow-up time. Altered bleeding patterns within the first few months of use are common but are generally self-limited and resolve by 6 months. As in all retrospective data collection, the potential for recall bias also exists. The median follow-up time was similar in both the LNG-IUS and copper IUD groups minimizing the potential for differential recall bias between the two. However, given the wide range of follow-up, particularly those at the later end, the potential for misinformation exists.
The major limitation of this study was our low rate of follow-up (34%), which may limit the validity of our results. When we began the study, we did not know if telephone contact was feasible in this population. Of the 147 women who were unable to be reached, 77 had a disconnected or incorrect number.
Women undergoing immediate postabortion insertion in this analysis were not enrolled in a research study at the time of their insertion; however, they had indicated a willingness to be contacted in the future. It is likely that follow-up rates would have been higher among women who had previously agreed to participate in a research study. However, our attempt to include all women receiving an immediate postabortion IUD better reflects the real population of women choosing this method, and the difficulty we experienced in contacting this population further underscores their need for immediate and highly effective postabortion contraception.
Low rates of follow-up in women undergoing abortion have been previously described. Grossman, Ellertson, Grimes, & Walker (2004) reported postabortion follow-up rates varying from 35% to 60%. Additionally, Drey and associates (2009) were only able to contact 51% of the women in their clinic population who had undergone an immediate postabortion insertion. Madden & Westhoff (2009) found that only 64% of patients returned as scheduled for postabortion follow-up. Low rates of postabortion follow-up means that the opportunity for contraceptive provision may be missed if delayed until the follow-up visit. Stanwood, Grimes, & Schulz (2001) reported that 40% of women who intended to have a delayed IUD insertion after an induced abortion did not follow-up. Similarly, a recent study looking at the barriers to IUD placement after abortion found that only 26% of women intending delayed postabortion IUD placement had actually received their IUD by 6 weeks (Stanek et al., 2009). Similar findings were reported by Fox and co-workers (2011), who found that only 23% of patients who intended to return for an interval IUD insertion actually received their contraceptive device, compared with 96% of women choosing immediate postabortion insertion.
Although our low follow-up rates are not a new problem, our study again demonstrates the challenges of conducting clinical research in this population of women. Our retrospective approach included all women undergoing a post-abortion IUD insertion and is more likely to provide a sample that represents the true population. However, as demonstrated in our study, it is also an approach that makes follow-up difficult. Although prospective recruitment allows for collection of important follow-up information, it may introduce selection bias and fail to recruit a number of women who are concerned about confidentiality and participating in a study.
In summary, women presenting for abortion are a challenging population to study and often go to extremes to preserve their anonymity. Delayed insertion coupled with low rates of follow-up likely result in missed opportunities for effective contraception. Immediate postabortion IUD placement increases the number of women who receive this highly effective method of contraception and, therefore, has the potential to significantly decrease repeat unintended pregnancy and abortion. Abortion and childbirth are considered the times when women are the most motivated to initiate contraception. Transitioning women directly from pregnancy to long-acting, reversible contraceptive methods at these times is critical. In 2009, the Institute of Medicine declared increasing long-acting, reversible contraception among its highest priority in comparative effectiveness research. This is consistent with the American College of Obstetricians and Gynecologists Committee on Gynecologic Practice Opinion, published in 2009, which suggested that the high rates of unintended pregnancy may be a direct consequence of low use of long-acting reversible contraceptives (ACOG, 2009). Expanding access to immediate postabortion IUDs should be a priority to help decrease unintended pregnancy in the United States.
Acknowledgments
The contents of this articles are solely the responsibility of the authors and do not necessarily represent the official view of NICHD.
Supported in part by award number K12HD001459 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD).
Biographies
Colleen McNicholas, DO, is a Clinical Fellow in Family Planning at Washington University in St. Louis, Obstetrics and Gynecology. Her specialties are family planning and contraception.
Taylor Hotchkiss, MD, practices at Shoreline OB/GYN in New London, Connecticut.
Tessa Madden, MD, MPH, is an Assistant Professor of Obstetrics Gynecology at the Washington University in St. Louis and specialized in family planning and contraception.
Qiuhong Zhao, MS, is a biostatistician at Washington University in St. Louis.
Jenifer Allsworth, PhD, is an Assistant Professor at Washington University in St. Louis and specializes in epidemiology and sexually transmitted infections.
Jeffrey F. Peipert, MD, PhD, is the Robert J. Terry Professor of Obstetrics and Gynecology, the Vice Chair of Clinical Research, and the OB/GYN Residency Program Director. He specializes in epidemiology and contraception.
References
- ACOG. Committee Opinion no. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstetrics and Gynecology. 2009;114:1434–1438. doi: 10.1097/AOG.0b013e3181c6f965. [DOI] [PubMed] [Google Scholar]
- Baldaszti E, Wimmer-Puchinger B, Loschke K. Acceptability of the long-term contraceptive levonorgestrel-releasing intrauterine system (Mirena): A 3-year follow-up study. Contraception. 2003;67:87–91. doi: 10.1016/s0010-7824(02)00482-1. [DOI] [PubMed] [Google Scholar]
- Beatty MN, Blumenthal PD. The levonorgestrel-releasing intrauterine system: Safety, efficacy, and patient acceptability. Therapeutics and Clinical Risk Management. 2009;5:561–574. doi: 10.2147/tcrm.s5624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednarek PH, Creinin MD, Reeves MF, Cwiak C, Espey E, Jensen JT. Immediate versus delayed IUD insertion after uterine aspiration. New England Journal of Medicine. 2011;364:2208–2217. doi: 10.1056/NEJMoa1011600. [DOI] [PubMed] [Google Scholar]
- Drey EA, Reeves MF, Ogawa DD, Sokoloff A, Darney PD, Steinauer JE. Insertion of intrauterine contraceptives immediately following first- and second-trimester abortions. Contraception. 2009;79:397–402. doi: 10.1016/j.contraception.2008.11.019. [DOI] [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Fox MC, Oat-Judge J, Severson K, Jamshidi RM, Singh RH, McDonald-Mosley R, et al. Immediate placement of intrauterine devices after first and second trimester pregnancy termination. Contraception. 2011;83:34–40. doi: 10.1016/j.contraception.2010.06.018. [DOI] [PubMed] [Google Scholar]
- Goodman S, Hendlish SK, Benedict C, Reeves MF, Pera-Floyd M, Foster-Rosales A. Increasing intrauterine contraception use by reducing barriers to post-abortal and interval insertion. Contraception. 2008;78:136–142. doi: 10.1016/j.contraception.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Grimes DA, Lopez LM, Schulz KF, Stanwood NL. Immediate postabortal insertion of intrauterine devices. Cochrane Database of Systematic Reviews. 2010;6:CD001777. doi: 10.1002/14651858.CD001777.pub3. [DOI] [PubMed] [Google Scholar]
- Grossman D, Ellertson C, Grimes DA, Walker D. Routine follow-up visits after first-trimester induced abortion. Obstetrics and Gynecology. 2004;103:738–745. doi: 10.1097/01.AOG.0000115511.14004.19. [DOI] [PubMed] [Google Scholar]
- Heikinheimo O, Gissler M, Suhonen S. Age, parity, history of abortion and contraceptive choices affect the risk of repeat abortion. Contraception. 2008;78:149–154. doi: 10.1016/j.contraception.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Kulier R, O’Brien PA, Helmerhorst FM, Usher-Patel M, D’Arcangues C. Copper containing, framed intra-uterine devices for contraception. Cochrane Database of Systematic Reviews. 2007:CD005347. doi: 10.1002/14651858.CD005347.pub3. [DOI] [PubMed] [Google Scholar]
- Madden T, Westhoff C. Rates of follow-up and repeat pregnancy in the 12 months after first-trimester induced abortion. Obstetrics and Gynecology. 2009;113:663–668. doi: 10.1097/AOG.0b013e318195dd1e. [DOI] [PubMed] [Google Scholar]
- O’Brien PA, Kulier R, Helmerhorst FM, Usher-Patel M, d’Arcangues C. Copper-containing, framed intrauterine devices for contraception: A systematic review of randomized controlled trials. Contraception. 2008;77:318–327. doi: 10.1016/j.contraception.2007.12.011. [DOI] [PubMed] [Google Scholar]
- Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, et al. Continuation and satisfaction of reversible contraception. Obstetrics and Gynecology. 2011;117:1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera R, Best K. Current opinion: Consensus statement on intrauterine contraception. Contraception. 2002;65:385–388. doi: 10.1016/s0010-7824(02)00304-9. [DOI] [PubMed] [Google Scholar]
- Stanek AM, Bednarek PH, Nichols MD, Jensen JT, Edelman AB. Barriers associated with the failure to return for intrauterine device insertion following first-trimester abortion. Contraception. 2009;79:216–220. doi: 10.1016/j.contraception.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Stanwood NL, Grimes DA, Schulz KF. Insertion of an intrauterine contraceptive device after induced or spontaneous abortion: A review of the evidence. British Journal of Obstetrics and Gynaecology. 2001;108:1168–1173. doi: 10.1111/j.1471-0528.2003.00264.x. [DOI] [PubMed] [Google Scholar]