Abstract
Objective
In the context of an increasing correctional population and corresponding rates of mental illness and substance abuse among this population, this study focuses on describing the predictors of substance abuse service utilization for ex-inmates with dual disorders. Our aim is to assess the likelihood and characteristics of ex-inmates with mental disorders who access substance abuse treatment services within two years of correctional release.
Methods
Using merged administrative data on all ex-inmates with open mental health cases released from Massachusetts Department of Corrections and two County Houses of Corrections from 2007 to 2009 (N=2,280) and substance abuse treatment outcome data through 2011, we analyze the influence of demographics, behavioral and mental disorders, and criminal justice variables on entry into substance abuse treatment within 24 months post release. We also describe primary drug use and services utilized for all the ex-inmates who accessed substance abuse services (N=1,383). Regression techniques were used to analyze the probability of utilizing substance abuse treatment services by various demographic, behavioral, and criminal involvement characteristics.
Results
The prevalence of a history of substance use disorders is high in this population (69%; n = 1,285). Subsequently, at 24 months post release 61% (n = 1,383) of ex-inmates with open mental health cases utilized substance abuse treatment services. This group was disproportionately female, with a preincarceration history of substance abuse, an increased number of previous incarcerations, and more likely released under correctional supervision.
Conclusions
Substance abuse is a chronic relapsing disorder and dual diagnosis is common among individuals with mental disorders involved with the criminal justice system. Their service needs and contacts across substance abuse, mental health, and criminal justice systems highlight individuals caught up in the institutional circuit. Study results point to the need for expanded and targeted dual diagnosis treatment approaches and relapse prevention for ex-inmates with mental disorders post correctional release.
Keywords: mental illness, mental disorder, substance abuse, criminal justice, dual diagnosis, history of substance abuse services, substance abuse treatment services, ex-inmates
The high prevalence of substance use and abuse among persons affected by mental illness has long been noted (Drake & Wallach, 1989). It is also well established that persons with mental illness have higher arrest rates than demographically similar members of the general population (Fisher et al., 2011); half of all prisoners have some form of mental disorder (James & Glaze, 2006) and Steadman and colleagues (2009) examined prevalence rates of serious mental illness among jail inmates and found a 15% rate among males and twice that among females (30%). Nationally, 83% of inmates with mental health diagnoses are dually diagnosed (Bureau of Justice Statistics, 2001). Hartwell (2004) reports that 70% of individuals with serious mental illness incarcerated in Massachusetts' prisons and houses of correction have substance abuse histories. At entry into the criminal justice system, individuals with co-occurring mental health and substance abuse problems (dual diagnosis) are at increased risk for involvement with formal agents of social control due to the proliferation of pathways to the criminal justice system, such as drug-related and drug-defined offenses (Swartz & Lurigio, 2007). Upon leaving the criminal justice system, the majority of individuals with mental disorders who are released also have a substance use disorder, resulting in correctional and community treatment imperatives for this population.
Individuals with mental illness are more likely to report being under the influence of drugs or alcohol when committing criminal offenses (McGillivray & Moore, 2001). Substance use is also a mediating factor for individuals with serious mental illness committing both violent and non-violent crimes (Swartz & Lurigio, 2007). Furthermore, ex-inmates with a history of dual diagnosis are more likely to recidivate than ex-inmates with mental illness alone (Hartwell, 2004). Clark and colleagues (1999) found a higher likelihood of rearrest and reincarceration among ex-inmates with dual diagnosis than the general population of ex-inmates. Evidence also suggests that inmates with serious mental illness are more likely than the general inmate population to have had previous incarcerations (Baillargeon et al., 2009).
Still, the presence of a mental disorder alone does not predict a higher likelihood of rearrest after release, and rates of rearrest and types of arrest do not differ significantly between ex-inmates with mental illness and the general population of ex-inmates (Feder, 1991; Jacoby & Kozie-Peak, 1997; Harris & Koepsell, 1998; Lovell, Gagliardi, & Peterson, 2002; Theurer & Lovell, 2008). However, the presence of both mental illness and substance use disorders changes the reinstitutionalization or recidivism dynamic and forces individuals to continue churning across the institutional circuit (Wiseman, 1970; Hopper, Jost, Welber & Haugland, 1997; Corporation for Supportive Housing, 2009). For instance, Baillargeon and colleagues (2009) found that dual diagnosis increased the risk of rearrest for both technical violations and new criminal offenses for individuals paroled at release. The synergy between mental illnesses and substance abuse that drives this increased risk is underscored by the observation that parolees with either substance abuse or major psychotic illness alone were not at an elevated risk (Baillargeon et al., 2009). These studies suggest that substance abuse treatment for ex-inmates with dual diagnosis at correctional release might play a critical role in reducing the risk of further offending.
Despite the importance of substance abuse in the criminal justice involvement of persons with serious mental illnesses and, presumably, of addressing this problem, it is surprising that there have been no studies examining the characteristics and probability of ex-inmates with dual diagnosis utilizing substance abuse treatment once released to the community. Existing studies focus on prison-based residential treatment (Wexler, 2003) or post-release services in general via case management (Godley, et al., 2003). Therapeutic communities in prison are an evidence based best practice for treating substance abuse disorders (Wexler, 2003). Unfortunately, there has been little replication of these programs across institutions or continuity of care across systems at the transitional time of release (Jennings, 2009). One report (Mallik-Kane & Visher, 2008) describes the significant titration of substance abuse services post-release among ex-inmates in general in the short term. At eight to ten months after release, however, there is some evidence that individuals with mental health issues are more likely to have received substance abuse treatment services than have other ex-inmates likely due to their engagement with treatment services in general (Mallik-Kane& Visher, 2008).
Similarly, treatment utilization studies among individuals with dual diagnosis are also rare, and there are conflicting views about the patterns of seeking treatment and treatment utilization. For example, on the one hand, Green (2006) found that females are more likely than males to face multiple barriers to accessing substance abuse treatment and are less likely to seek treatment. On the other hand, Drapsalski and her colleagues (2011) found that the current research about gender differences among individuals with dual diagnosis and their treatment seeking patterns and motivation to change is limited. Their research shows that females have to overcome many barriers to seek treatment, but once they do, show greater readiness to cease abusing substances. They also found that individuals with severe mental health problems are more motivated to enter substance abuse treatment regardless of gender. Similarly in regards to race and ethnicity, Acevedo and colleagues (2012) found that there are significant racial differences in initiation of seeking treatment and engagement in substance abuse treatment. They found that African Americans are the least likely to initiate treatment and that more attention needs to be given to this issue. Green and Drake (2011) argue that although dual diagnosis is likely to occur in individuals across all social strata, disadvantaged ethnic groups are significantly more likely to be affected and to have contact with the criminal justice system. In general, more studies are needed to examine the utilization and treatment seeking patterns among individuals with dual diagnosis and the important factors that may influence their decisions to seek treatment especially among individuals involved in the criminal justice system.
Integrated treatment programs for individuals with dual diagnosis, involved with the criminal justice system, and residing in the community, continue to be regarded as specialty services (Osher, 2008). Programs such as Co-occurring Disorders Court, which diverts individuals from incarceration (Kleinpeter, 2008), and community-based programming such as Forensic Assertive Community Treatment; Forensic Intensive Case Management; Integrated Dual Diagnosis Treatment; Maintaining Independence and Sobriety through Systems Integration, Outreach, and Networking; Project Link; and Critical Time Intervention show considerable promise in terms of their aims and structures. However, they currently lack a true evidence base and are subsequently not widespread (Smelson, Sawh, Kane, Kuhn, & Ziedonis, 2011; Jennings, 2009; Draine & Herman, 2007; Morrissey, Meyer, & Cuddeback, 2007; Lamberti et al., 2001). Given this chasm between available, appropriate, integrated programming, our limited knowledge of substance abuse treatment service utilization, and the prevalence of ex-inmates released from corrections with dual diagnosis, this paper seeks to inform our understanding of ex-inmates with dual diagnosis by describing post release substance abuse service utilization and predictors/characteristics of individuals accessing treatment within a standard time period post release to improve system responsiveness and effective interventions. Specifically the analysis will examine: (1) the basic characteristics of ex-inmates with dual diagnosis; (2) the relationship between the major independent variables and service utilization; and (3) the factors that affect the probability of utilizing substance abuse services within a standard two-year time period post release. The analysis further provides post release service system implications related to treatment type and primary drug of choice among the individuals who utilized treatment within 24 months (n=1,383).
METHODS
Sample and Sources of Data
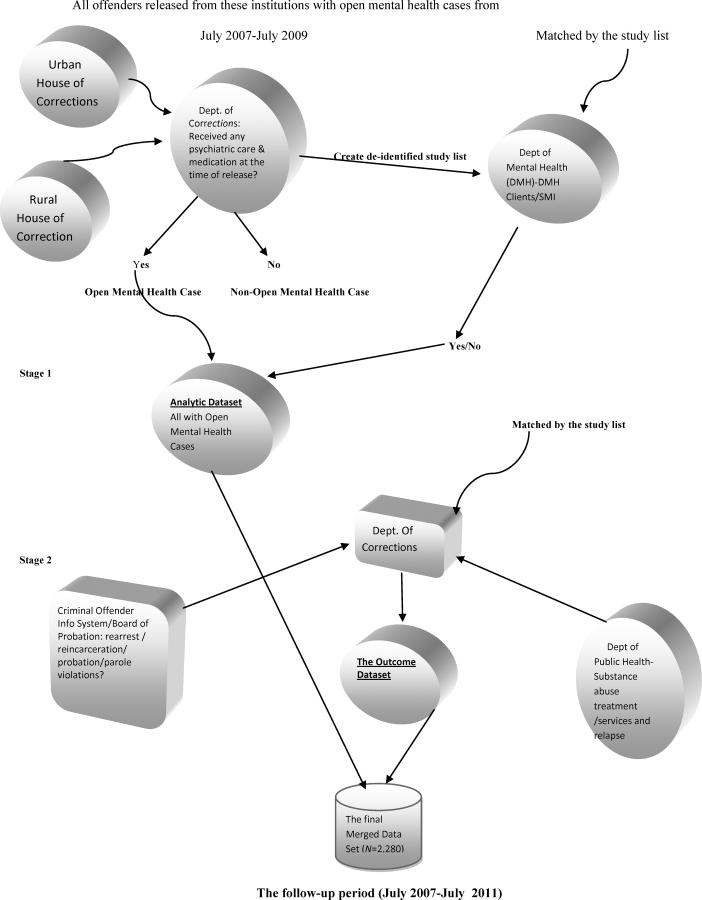
Study participants were identified using merged administrative data on all individuals with open mental health cases released from all 16 Massachusetts Department of Correction (DOC) facilities and two County Houses of Corrections from 2007 to 2009 under a Memorandum of Understanding with the Department of Correction and the Department of Mental Health.1 We focused on individuals who, while incarcerated, had open mental health cases, arguably a broad-based definition that subsumes a broad spectrum of individuals and clinical features. Individuals with open mental health cases receive psychiatric care and medications while incarcerated. Within that group is a subset of persons with serious mental illnesses having more severe Axis I diagnoses, lengthier duration of illnesses, and higher levels of dysfunction which makes them, in some cases, eligible for services provided by the Massachusetts Department of Mental Health (see Figure 1).
Figure 1.
Data Sources and Merging Process
A total of 2,280 individuals who had open mental health cases were released during our observation period, comprising 16% of the 14,642 individuals released from the Department of Corrections and two County Houses of Correction over the two year period spanning July 2007 to July 2009. The group of individuals with serious mental illness eligible for Department of Mental Health services included 138 people (6% of those with open mental health cases and less than 1% of all releases). In addition, more than two thirds (69%) had a history of substance abuse recorded on their correctional records (n=1,285; see Table 1). Overall, 85% (n=1,948) of individuals in our sample accessed substance abuse services either prior to or after correctional custody. Secondary data on substance abuse treatment utilization post release were integrated through August 2011 under the same Memorandum of Understanding with the Department of Public Health Bureau of Substance Abuse Services.2
Table 1.
Description of Participants upon Post-Correctional Release (N=2,280)
| Demographics & Other Factors | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 1472 | 64.6 |
| Female | 808 | 35.4 |
| Age Groups (n=2,279) | ||
| 18–25 | 334 | 14.7 |
| 26–35 | 794 | 34.8 |
| 36–45 | 751 | 33.0 |
| 46+ | 400 | 17.6 |
| Race /Ethnicity | ||
| White | 1348 | 59.1 |
| Black | 424 | 18.6 |
| Hispanic | 487 | 21.4 |
| Other | 21 | 0.9 |
| Education (n=1,998) | ||
| < High School | 854 | 42.7 |
| High School/GED | 1025 | 51.3 |
| Higher Education | 119 | 6.0 |
| Primary Mental Health Disorder (n=1,788) | ||
| Mood Disorder | 763 | 42.7 |
| Thought Disorder | 283 | 15.8 |
| Personality Disorder | 43 | 2.4 |
| Anxiety Disorder | 232 | 13.0 |
| Posttraumatic Stress Disorder | 298 | 16.7 |
| Substance Abuse | 112 | 6.3 |
| Other | 57 | 3.2 |
| Substance Abuse History (n=1,871) | ||
| Yes | 1285 | 68.7 |
| No | 586 | 31.3 |
| Most Recent Criminal Charge (n=2,276) | ||
| Person Offenses | 859 | 37.7 |
| Sexual Offenses | 66 | 2.9 |
| Property | 425 | 18.7 |
| Drug Offense | 656 | 24.8 |
| Other | 361 | 15.9 |
| Juvenile Record (n=2,278) | ||
| Yes | 1035 | 45.5 |
| No | 1243 | 54.6 |
| Post-Release Supervision (n=1,882) | ||
| No Legal Supervision | 813 | 43.2 |
| Had Legal Supervision (e.g. parole and probation) | 1069 | 56.8 |
| Correctional Setting | ||
| State Prison System | 1438 | 63.1 |
| County House of Corrections | 842 | 46.9 |
| Entered into Treatment within 24 mos. of Release | ||
| Yes | 1383 | 60.7 |
| No | 897 | 39.3 |
| Previous Incarcerations | Mean | SD |
| 6.20 | 6.79 |
Data
The dataset used in this study was built in two stages (see Figure 1). The first stage entailed merging data on all releases from 2007 through 2009 (N=14,642). Once this was completed a study identification code list was created and kept at the Department of Correction. This dataset was then shared with the Department of Mental Health to identify their clients with serious mental illness. Department of Mental Health client data were incorporated and the dataset was stripped of identifiers (which would have constituted protected health information) and sent back to the Department of Correction, where only those with open mental health cases were retained in the file and the remainder of the variables were populated. This dataset functioned as the final analytic dataset (N=2,280).
The second stage included the creation of the outcome dataset, which entailed sharing the study identification code list, including client identifiers stripped of other information such as private health information, with the Department of Public Health. The Department of Public Health provided quarterly outcome data on Bureau of Substance Abuse Service treatment utilization. Quarterly, and at the end of the study period, the Department of Public Health stripped the outcome dataset of identifying information (except for the study code) and returned the data on an encrypted disc to be uploaded to the main dataset at the Department of Correction where the analytic and outcome datasets were merged using study identifiers. The Department of Correction provided rearraignment and reincarceration information for each individual, which a research assistant uploaded into the dataset on a quarterly basis.
Human Subjects Review
The study was approved by institutional review boards at University of Massachusetts Boston, Lowell, and Worcester campuses, the Department of Public Health, and the Department of Mental Health in full conformance with the Declaration of Helsinki. Additionally, a research review process and authorization was granted by the Department of Correction and the Massachusetts Criminal History Systems Board (currently the Criminal Justice Information System).
Measures and Analysis
Our dependent variable, accessing substance abuse treatment within 24 months of release was based on treatment admission dates (month and year) and was captured continuously over the course of the entire study period (39 months from 2007 through 2011). We recoded each episode of treatment into categories of within 6-months, 12-months, and 24-months of release to examine rearrest, reincarceration, and treatment service utilization outcomes across standard periods for individuals post release. However, here we elected to limit our observation to within 24 months for purposes of our regression analysis to also assure that all individuals in the dataset had a standard, fairly lengthy observation period to better understand the predictors of accessing substance abuse treatment services post-correctional release. All analyses were conducted using SPSS software version 18.
Most of our variables are either multiple categorical or binary with the exception of education, previous number of incarnations, and age group (which is ordinal). Three major types of variables are included in our analysis: (a) demographic variables, including gender, age, race, and education; (b) behavioral health related variables, including mental health/primary disorder and substance abuse history; and (c) measures of past and current criminal justice involvement, including most recent serious criminal charge, juvenile record, previous incarcerations, post-release supervision (probation and/or parole), and correctional setting (state prison, county house of correction). In addition, we also examine primary drug use and the substance abuse services the ex-inmates utilized post release. The categories of primary drug use include alcohol, hypnotics, cocaine/crack, opium derivatives, and marijuana. The “other” category includes methamphetamine and over-the-counter drugs. Hypnotics include barbiturates, phencyclidine/PCP, hallucinogens and club drugs. Opium derivatives include heroin, non-prescription methadone, oxycodone, and other opiates. Treatment type was coded as “residential” (including family housing, recovery homes, therapeutic communities, transitional housing, and social modeling homes); “detox services” (such as acute treatment and clinical stabilization); “legal mandates” (including drunk driving mandates, probation and reentry resource centers, parole, court orders and drug court); “outpatient” (such as day treatment, counseling, recovery support, street outreach, and transitional support); “opioid treatment” (including methadone and office-based opioid treatment); and “other” (treatment such as acupuncture).
Our analyses began with a univariate analysis to describe the basic characteristics of the sample as shown in Tables 1 and 2. Second, a binary analysis method was used, as shown in Table 3, which examined the relationship between our major independent variables and the dependent variable (accessing substance abuse treatment by 24 months) for individuals with a substance abuse history (n=1,285). Table 4 displays the relationship between substance abuse treatment utilization and time in three time frames: within 6 months, 12 months, and 24 months. Finally, multivariate logistic regression was used to assess the effects of major independent variables on entry into treatment within 24 months. One of the major challenges in secondary data collection and analysis is that administrative data collected across various agencies and facilities may result in missing values. We addressed this issue by making clear in our tables and results the total number of missing values within each variable.
Table 2.
Primary Drug Use and Substance Abuse Service Type at First Admission Post Release (n=1,383).
| n | Percentage | |
|---|---|---|
| 1383 | 60.6 | |
| Primary Drug Use | ||
| Alcohol | 371 | 26.8 |
| Hypnotics | 16 | 1.2 |
| Cocaine/Crack | 224 | 16.9 |
| Opium Derivatives | 634 | 45.8 |
| Marijuana | 94 | 6.8 |
| Other | 34 | 2.5 |
| Substance Abuse Service Type | ||
| Residential | 242 | 17.4 |
| Detox Services | 381 | 27.5 |
| Legal Mandate | 375 | 27.1 |
| Outpatient | 281 | 20.3 |
| Opioid Treatment | 86 | 6.2 |
| Other | 18 | 1.3 |
Table 3.
Relationship between Predictor Variables and Substance Abuse Treatment Access by 24 Months among Individuals with a Substance Abuse History (n=1,285)
| Accessed Treatment within 24 Months | |||||
|---|---|---|---|---|---|
| n | Percentage | χ 2 | df | p | |
| Gender | 10.17 | 1 | <.001*** | ||
| Male (n=1,013) | 616 | 60.8 | |||
| Female (n=272) | 194 | 71.3 | |||
| Age Groups | 3.34 | 3 | .34 | ||
| 18–25 (n=173) | 107 | 61.8 | |||
| 26–35 (n=456) | 292 | 64.2 | |||
| 36–45(n=419) | 272 | 54.9 | |||
| 46+ (n=237) | 138 | 58.2 | |||
| Race/Ethnicity1 | 12.74 | 3 | .005** | ||
| White (n=737) | 494 | 67.0 | |||
| Black (n=230) | 129 | 56.1 | |||
| Hispanic (n=311) | 182 | 58.5 | |||
| Other (n=7) | 5 | 71.4 | |||
| Education | 1.76 | 2 | .414 | ||
| < High School (n=513) | 328 | 63.9 | |||
| HS/GED (n=604) | 390 | 64.6 | |||
| Higher Education (n=49) | 27 | 55.1 | |||
| Primary Mental Disorder | 13.19 | 6 | .04* | ||
| Mood Disorder (n=488) | 311 | 63.7 | |||
| Thought Disorder (n=214) | 113 | 52.8 | |||
| Personality Disorder (n=31) | 22 | 71.0 | |||
| Anxiety Disorder (n=135) | 91 | 67.4 | |||
| PTSD (n=169) | 111 | 65.7 | |||
| Substance Abuse (n=28) | 20 | 71.4 | |||
| Other (n=39) | 26 | 66.7 | |||
| Most Recent Primary Criminal Charge | 8.14 | 4 | .086 | ||
| Person Offenses (n=517) | 332 | 64.2 | |||
| Sexual Offenses (n=32) | 13 | 40.6 | |||
| Property Offenses (n=224) | 147 | 65.6 | |||
| Drug Offenses (n=333) | 208 | 62.5 | |||
| Other (n=178) | 109 | 61.2 | |||
| Juvenile Record | .59 | 1 | .45 | ||
| Yes (n=627) | 402 | 64.1 | |||
| No (n=656) | 407 | 62.0 | |||
| Post-Release Supervision | 8.66 | 1 | .003** | ||
| Legal Supervision (n=597) | 401 | 67.2 | |||
| No Legal Supervision (n=497) | 291 | 58.6 | |||
| Correctional Setting | 7.27 | 1 | .007** | ||
| State Prison system (n=712) | 472 | 66.3 | |||
| County House of Corrections (n=573) | 338 | 59.0 | |||
| Primary Drugs | 2.22 | 5 | .69 | ||
| Alcohol (n=224) | 215 | 96.0 | |||
| Cocaine/Crack (n=136) | 132 | 97.1 | |||
| Opium Derivatives (n=388) | 375 | 96.6 | |||
| Marijuana (n=62) | 58 | 93.5 | |||
| Hypnotics/Other (n=12) | 12 | 100.0 | |||
| Substance Abuse Service Type | 13.13 | 5 | .02* | ||
| Residential (n=133) | 133 | 100.0 | |||
| Detox Services (n=254) | 241 | 94.9 | |||
| Legal Mandate (n=223) | 219 | 98.2 | |||
| Outpatient (n=170) | 161 | 94.7 | |||
| Opioid Treatment (n=51) | 47 | 92.2 | |||
| Other Drugs (n=7) | 7 | 100 | |||
Note.
Some variables do not add up to 1,285 due to missing values.
Because the “other” category had such a small n, we ran the analyses with and without this category. The results were essentially the same, so the category was retained.
p<.001;
p<.01;
p<.05
Table 4.
Substance Abuse Treatment Access within 6 Months/12 Months /24 Months (n=1,383)
| n | Percent | Cumulative Percent | χ 2 | df | p | |
|---|---|---|---|---|---|---|
| 602.0 | 1 | <.001** | ||||
| 7 | * | |||||
| Accessed Treatment Months 1–6 | 1062 | 76.8 | ||||
| Total at 6 months | 1062 | 76.8 | ||||
| Accessed Treatment Months 7–12 | 159 | 11.5 | ||||
| Total at 12 months | 1221 | 88.3 | ||||
| Accessed Treatment Months 13–24 | 162 | 11.7 | ||||
| Total at 24 months | 1383 | 100 |
RESULTS
Table 1 describes the sample of individuals with open mental health cases (N=2,280). The table indicates where there are missing values in each variable sequence as well as percents adjusting for missing values.
The sample is more than two-thirds male (n=1,472; 65%) and white (n=1,348; 59%). About half of the sample is high school educated (n=1,025; 51%). As the data indicate, the sample exhibits variation with respect to the nature of the most recent charge, but person-related charges including assault/robbery are the most common. More than half were released under some form of correctional supervision (n=1,069; 57%). The mean number of previous incarcerations was about 6 (SD=6.79), with a range of 0 to 70 previous incarcerations. Mood disorders including major depression are the most prevalent mental health/primary disorder at more than double the prevalence of other disorders (n=763, 43%). The high prevalence of substance abuse history (n=1,285, 69%) is consistent with prevalence rates found in the cited literature (Bureau of Justice Statistics, 2001; Hartwell, 2004). Our goal was to link these characteristics with the likelihood of utilizing substance abuse treatment services in a standard time period.
Nearly two-thirds of the sample accessed substance abuse treatment services by 24 months post release (61%; n=1,383) with an additional 45 individuals utilizing services outside our two-year time frame, up to 39 months post release. Table 2 provides more descriptive data on primary drug use and service type for the group accessing services within 24 months post release (n=1,383). There is a striking prevalence of depressant use (alcohol and opium derivatives including heroin, non-prescription methadone, oxycodone and other opiates). In fact, nearly half of the primary drug use reported (46%; n=634) at first admission post-release falls into the opiate abuse category. Additionally, more than a quarter (28%; n=381) of these individuals were coming to treatment for detoxification services (acute treatment, clinical stabilization), and another quarter were mandated to treatment post release (27%; n=375).
Table 3 shows the relationships between our predictor variables and the dependent variable (substance abuse treatment by 24 months; n=1,383) for individuals with a substance abuse history (n=1,285). The table lists all predictors variables including basic demographic variables, mental health and behavioral disorders, crime and correctional characteristics, primary types of drugs, and types of substance services received. Among these variables, only three were statistically significant beyond the .01 level, gender, correctional setting at release, and post-release supervision. Although a p value of .05 is a commonly accepted standard to determine statistical significance, we have a relatively large sample and have therefore decided to adopt a more rigorous standard to focus on those variables with p values less than .01 to avoid potential Type I errors. Using this standard, being female (χ2=12.17, df=1, p<.001), released from a longer term sentence in a state prison (χ2=7.37, df.=1, p<.01), and/or under some form of post-release/correctional supervision (χ2=8.66, df=1, p<.01) were the predominant correlates of individuals with substance abuse histories accessing substance abuse services within 24 months of release. Nevertheless, it remains important to balance statistical significance and practical social significance. With this in mind, we also indicate the variables that are significant at .05 level.
Table 4 displays the distribution patterns of substance abuse treatment use within three time frames: 6 months, 12 months, and 24 months. As shown, 1,062 (76.7%) individuals utilized services within the first 6 months after their release. From month seven to twelve, 159 more additional individuals accessed treatment, and from thirteen to twenty-four months, 162 more individuals accessed treatment. The majority of ex-inmates utilized treatment within the first six months of release and this relationship was significant (χ2=602.27, df.=1, p<.001). Many of these individuals were likely complying with a post-release and/or a legally mandated treatment plan (n=379; 27%), and the vast majority were parolees (n=305; 22% of individuals utilizing treatment). All parolees in Massachusetts are currently mandated to meet with substance abuse coordinators to create reentry plans within a couple days of release. Smaller numbers of individuals (n=47; 3%) were recorded as accessing reentry resource centers as their first service type at substance abuse treatment admission when released from county houses of corrections. Finally, a handful of individuals were court ordered to treatment via court petitions or due to convictions for driving under the influence (n=23; less than 1%). While legally mandated treatment may partially explain the peak in treatment in the early months after release, detoxification and stabilization services were in equally high demand suggesting high relapse rates soon after release.
Assessing probability of substance abuse treatment entry
Our next task involved modeling the probability of entry into substance abuse treatment post release (Table 5). In this analysis we used our entire sample of individuals with open mental health cases who accessed substance abuse treatment including persons who were not identified as having a history of substance abuse. This approach was taken based on the literature documenting extremely high levels of risk for engaging in substance abuse among persons with mental disorders residing in the community (Alverson, Alverson & Drake, 2001; Drake, Bartels, Teague, Noordsy, & Clark, 1993). We thus assumed that persons with substance abuse histories, as well as those without, were at risk for engaging in substance abuse and in potential need of treatment at some point post release. Of the 1,383 individuals who accessed treatment, 183 individuals had missing data on key variables. Thus, only 1,200 individuals were included in this analysis.
Table 5.
Logistic regression of effects of demographic, behavioral health, criminal history, and correctional factors on entry into substance abuse treatment within 24 months post release (n=1,200).1
| B | SE | Exp(B) | 95% CI | |
|---|---|---|---|---|
| Gender (Male) | −.61** | .172 | .545 | [.389, .763] |
| Age Group | ||||
| 17–25 | 1.000 | |||
| 26–35 | .273 | .189 | 1.314 | [.908, 1.901] |
| 36–45 | .211 | .207 | 1.235 | [.823, 1.855] |
| 46+ | −.032 | .236 | .968 | [.609, 1.539] |
| Race/Ethnicity | ||||
| White | 1.000 | |||
| Black | −.417* | .176 | .659 | [.467, .930] |
| Hispanic | −.383* | .169 | .682 | [.489, .951] |
| Other | −1.198* | .595 | .302 | [.094, 968] |
| Education | −.178 | .114 | .837 | [.670, 1.05] |
| Behavioral Health Disorders | ||||
| Thought | 1.000 | |||
| Anxiety | .277 | .264 | 1.319 | [.785, 2.214] |
| Mood | .381 | .212 | 1.464 | [.966, 2.218] |
| PTSD | .568* | .249 | 1.765 | [1.084, 2.874] |
| Personality | .653 | .457 | 1.921 | [.784, 4.709] |
| Substance Abuse | .676 | .381 | 1.967 | [.932, 4.150] |
| Other | .291 | .367 | 1.338 | [.651, 2.748] |
| History of Substance Abuse | .580*** | .166 | 1.786 | [1.291, 2.471] |
| Criminal History | ||||
| Juvenile Record (yes) | −.067 | .138 | .935 | [.714, 1.225] |
| Previous Incarcerations | .041** | .016 | 1.042 | [1.010, 1.075] |
| Most severe charge on last sentence | ||||
| Person Offenses | 1.000 | |||
| Sexual Offenses | −.949** | .385 | .387 | [.182, .824] |
| Property Offenses | −.040 | .180 | .961 | [.675, 1.367] |
| Drug Offenses | .068 | .165 | 1.071 | [.775, 1.478] |
| Other | −.187 | .220 | .830 | [.539, 1.277] |
| Correctional Setting | ||||
| State Prison System | ||||
| County Houses of Correction | −.133 | .167 | .876 | [.632, 1.213] |
| Legal Supervision (Parole & Probation) | .276** | .129 | 1.318 | [1.023, 1.697] |
| Supervision -yes |
Note.
B = Log odds coefficient; SE = standard error; Exp(B) = odds ratio; CI = confidence interval.
Reference groups are indicated by Exp(B) = 1.000.
Because 183 individuals had missing data on key variables, only 1,200 individuals were included in this analysis.
p<.001;
p<.01;
p<.05
The odds of entering public substance abuse treatment within 24 months were estimated using a range of demographic, mental health, substance abuse history and criminal justice involvement factors described above and included in Table 1. The results of the logistic regression using these variables are shown in Table 5 using the groups designated with Exp(B)=1.000 as the reference group. As indicated, gender was a significant predictor of substance abuse treatment utilization post release. Males were roughly 0.55 times less likely to seek treatment than females when controlling all other independent variables in the model; odds ratio = .55; p<.001; 95% CI [.389, .763]. Although the level of significance for the race/ethnicity variable was at the 0.05 level (we set our threshold at .01), race/ethnicity is a socially significant variable given issues related to disproportionate minority confinement and in the context of inequality, crime, and treatment of dual disorders. Black (odds ratio .66) and Hispanic (odds ratio .68) individuals were less likely to engage in post release treatment than their white counterparts. Similarly, compared to persons with thought disorders, individuals with a diagnosis of posttraumatic stress disorder (odds ratio 1.765) were somewhat more likely to enter treatment within 24 months. No other diagnostic group had an effect approaching significance. Individuals with a pre-incarceration history of substance abuse noted in their correctional records had, not surprisingly, the highest probability of utilizing treatment. Comparing those offenders without a prior history of substance abuse, the odds ratio for ex-inmates with substance abuse histories was 1.786, indicating that the odds ratio for this group would increase by roughly .79 times compared to individuals who did not have a history of substance abuse.
In addition to the above, factors associated with criminal history, offense type, and placement under legal supervision at release were also significant. With respect to criminal history, the number of prior incarcerations was a significant and positive predictor of accessing treatment. although the number of prior incarcerations has a much wider range of values (0 – 70) than almost all other predictor variables. Specifically, the odds ratio for this variable is 1.042, indicating that a one unit (or 1 time) increase in the number of prior incarcerations can increase the odds of accessing treatment by .042. while holding all other variables constant in the model. Conversely, having a juvenile record was not a significant predictor of utilizing treatment, but individuals being released for sex offenses were only 39% as likely to access treatment as other individuals relased on other charges and this difference is significant at p<.01. Interestingly, individuals for whom drug charges were their most serious charge on their recent conviction were not significantly more likely than those without drug charges to enter treatment. As shown in Table 5, ex-inmates under legal/correctional supervision on parole or probation were roughly one-third more likely to engage in treatment than individuals who were not under any legal supervision. Finally, we attempted to include primary drug use and types of substance abuse services into our logistic regression model, but the variables were not significant so they were excluded from the final model.
DISCUSSION
The data suggest that substance abuse treatment for individuals with mental health issues and the added institutional transition of prisoner reentry should not be “specialty” or “boutique” treatment. Rather it should be a normative part and expectation of release and treatment plans across criminal justice and public health institutions and collaboratives for the first crucial months after release and ongoing thereafter. Substance abuse is a chronic relapsing disorder and being dually diagnosed is fairly normative among individuals with mental disorders involved with the criminal justice system. Study results point to the need for improved and specified treatment approaches, particularly for the majority of individuals accessing treatment who are mandated to treatment or requiring acute care/detoxification,. These individuals cycle across institutions. They are more likely to be female and have histories of substance abuse and previous incarcerations.
The service needs and contacts across substance abuse, mental health, and criminal justice systems among this population highlight individuals caught up in an institutional circuit that can result in life course persistent offending unless targeted interventions can effectively interrupt the circuit (Wiseman, 1970; Hopper, Jost, Welber & Haugland, 1997; Corporation for Supportive Housing, 2009). Stigma and burden may influence this circuit and perhaps explain why dual diagnosis services remain somewhat truncated. Similarly, stigma varies across race, gender, and ethnicity creating additional barriers for ex-inmates in general at time of parole or accessing services. The stigma of being dually diagnosed makes it increasingly difficult to access mental health services after release (Hartwell, 2004). Our results raise the question as to whether substance abuse treatment is equally accessible for all members of this population. For instance, our data suggests that Blacks and Hispanics are less likely to access treatment services.3
Consideration should be given to assure that services offered are culturally diverse and responsive. Conversely, females with a substance abuse history are more likely to access treatment over time than males. Women with children may be engaged with social services to a greater extent than men because of their greater involvement with their children or reliance on social services due to structural issues related to inequality. A worthy area to explore in future research, then, is identifying factors that serve as facilitators of, or barriers to, access to treatment for ex-inmates with dual diagnosis, including mandated treatment approaches and primary substance of abuse. This would entail looking at interaction effects between factors that may moderate associations between need for services and actual use of them. In the next iteration of this study we will examine these issues as affected by a range of mediators and moderators to treatment access.
It is also important to note that ex-inmates with previous incarcerations are more likely to access treatment within 24-months of release. These individuals are also more likely to be released under correctional supervision. Sex offenders, dually diagnosed or not, are typically released on lifetime parole, but for whatever reason are less likely to access substance abuse treatment. Perhaps lifetime parole mechanisms determine this outcome or restrictions on mobility in this group reduce their access to treatment services. This needs further investigation because untreated substance abuse in this population would seem to be a strong risk factor for re-offending. Rigorous post release conditions are not ideal for individuals with mental health issues; in fact, being dually diagnosed increased the 12-month risk of rearrest on a technical violation or new criminal offense for individuals on parole (Baillargeon et al., 2009). Thus, when dual diagnosis is a factor, questions regarding mandated treatment, first month release and transition plans, drug of choice, and responsible agency should be integrated into the process of planning prior to release and across the immediate post-release transition. Our analysis reveals that the probability of being female with a substance abuse and incarceration history significantly increased the odds of accessing services. Alcohol and opiates were the most commonly used drugs, and the services were accessed to meet supervision requirements or detoxification needs. Thus, dually diagnosed ex-inmates “of a type” – with the characteristics we have identified here -- are more likely to be shuffled across systems, traversing the institutional circuit, and ultimately ending up in the institution of the last resort, usually one operated by the criminal justice system, unless treatment services are better able to receive them and anticipate their needs.
Of concern is our finding that the majority of individuals who entered treatment utilized detoxification services which suggests that they did so in the context of an acute crisis. Similarly, the next most frequently accessed service type included mandated services. A closer examination of post detoxification service utilization and mandated treatment approaches is necessary in future research for individuals with dual diagnosis exiting corrections. While it seems the treatment system is responsive, with almost two-thirds of individuals accessing treatment post release, we cannot determine whether the services they received were effective for them, either clinically or within the social context in which these individuals live post-release. Clearly, more research needs to be done to both understand why individuals access treatment services and the exisiting post detoxification service linkages. This is worthy of closer examination in terms of portals to treatment, treatment specificity, and post treatment planning. As it stands, we cannot tell the more detailed story about what services maintain individuals in the community and what services and features of dual diagnosis volley individuals back and forth across the institutional circuit of the criminal justice and public health systems.
Limitations
Predicting substance abuse treatment utilization was limited by the overall quality of our administrative data. We spent a tremendous amount of time aligning and cleaning the dataset and completing missing data fields. Nevertheless, while we compiled the dataset we learned that each agency had different methods and purposes in their data collection and applications. For instance, substance abuse history was collected in a standardized manner for all Department of Correction inmates/facilities. However, one County House of Correction in the study collected this information manually from charts. It is possible that the manually entered data may not be complete. Nevertheless, we found that there was no significant difference in the rates between the two types of correctional institutions in terms of collecting the history of substance abuse variable. Still, we have no way of knowing if other correctional institutions missed people with substance abuse histories. This is a concern because nearly 30% of the individuals utilizing substance abuse treatment services by 24 months were not counted as having a substance abuse history.4 This nearly 30% would be an interesting group to examine more closely to consider if individuals are emerging from corrections and developing subsequent substance abuse problems or for the first time are motivated to access treatment. Similarly, mental health/primary disorder was coded by the research team from 52 pages of diagnostic materials and codes. Missing data in that variable could have occurred at any stage in the process from a clinician defining an inmate as having an open mental health case without coding a primary disorder into the chart to erroneously recoding the disorder into the research dataset. From the outset we had little ability to standardize how the information was collected across facilities given our reliance on the way institutions collect and store their data.
Other issues related to administrative data included our inability to specify certain variables. For instance, mood disorder is an overly general category and its use here is an example of an instance where manual data collection proved prohibitive in accessing more finely-tuned data. One facility coded all mood disorder data under the general code of “mood” and was later unable to go back and extract anxiety and trauma symptoms from that code. This loss to specificity is especially troublesome given the relation of trauma and post traumatic stress disorder to substance abuse. We also did not collect length of time served as the County House of Corrections quick turnover rate proved prohibitive. Our logistic regression did not explain a great deal of the variance in the model. Neither the Cox and Snell (pseudo R2 = .068) nor the Nagelkerke (pseudo R2 = .093) measures were large, suggesting that there are many factors beyond those captured here that explain the bulk of variance in this outcome.
Finally, our data raises questions about generalizability. Several factors may affect the generalizability of our findings including institutional data collection methodologies as well as our approach. We know close to 40% of our sample did not access substance abuse treatment services within 24-months of release. By 24 months post release the rate of treatment access was 61%, but this number does not reflect individuals who where reincarcerated, experienced lengthy hospitalizations for psychiatric or medical treatment or died during this period. We are well aware that individuals were taken out of the risk pool early and intermittently for a variety of reasons including hospitalizations. However, we were unable to obtain Medicaid data and subsequently unable to comment on general or psychiatric hospitalizations not related to the Department of Mental Health facilities. Lacking access to Medicaid data could also result in undercounting the number of people accessing substance abuse treatment services. Simply put, our analysis does not address the competing risks for treatment non-engagement. Although we have officially recorded utilization rates for substance abuse treatment, we can only theorize about “actual rates” due to limitations of administrative/secondary data.
Moreover, we are also cautious about cross population generalizability and are aware that our findings may be specific to Massachusetts and may not be generalized to released offenders in other states. Overall, we are cautious about the generalizability of our findings until future research of similar design is done in this area that validates our findings. Similarly, future research should more thoroughly investigate the issue of missing values as both systematic or random as related to the risk pool. In conclusion, more research with varied methodological approaches collecting more finely tuned data is more than justified given the public health and public safety issues associated with this population.
ACKNOWLEDGMENTS
This work was funded by the National Institute of Health NIMH1RC1MH088716-01. Thank you to Alison Moll our grant manager at UMass Boston. The investigators would also like to thank Dr. Martha Lyman, Michael Lupo and Julie White LICSW for their contributions and commitment to this project. Gratitude goes to our excellent research assistants from UMass Boston – Paul Anskat, Phoebe Lehman, Brianna Roach, Jenn Walker, Taylor Hall, and James Wall. Thanks to Debra Pinals, MD and Paul Benedict for their expertise and technical assistance from the Department of Mental Health; Lisa Sampson, Natalya Pushkina, William Saltzman and Ken Nelson for their support from the Department of Correction; and Andrew Hanchett, Hermik Babakhanlou-Chase, Adam Pojani, and Michael Botticcelli for their support from the Department of Public Health Bureau of Substance Abuse Services.
Dr. Hartwell has received compensation as a trainer and keynote speaker at Douglas Mental Health Institute, McGill University and from the National Institute of Mental Health as a grant reviewer in 2011 and 2012.
Footnotes
DISCLOSURES Drs. Deng, Fisher, and Fulwiler, Mr. Johnson, Ms. Siegfriedt, and Ms. Roy-Bujnowski have no financial relationships with commercial interests.
Massachusetts' DOC houses offenders who receive sentences more than 2.5 years who serve 4 years on average. County Houses of Corrections usually hold offenders whose sentences are 2.5 years or below averaging 9 months for time served. County Houses of Corrections usually supervise and control inmates who commit less serious crimes.
A paper describing this process was recently published (Hartwell et al., 2012).
Although race and ethnicity were significant at p<.05, which does not reach our statistical threshold, we believe this finding has sociological significance.
Essentially almost 30% of individuals accessing treatment are estimated to be new substance abuse treatment need cases without a prior substance abuse history (n=1,126).
REFERENCES
- Alverson H, Alverson M, Drake RE. Social patterns of substance use among people with dual diagnoses. Mental Health Services Research. 2001;3(1):3–14. doi: 10.1023/a:1010104317348. doi:10.1023/A:1010104317348. [DOI] [PubMed] [Google Scholar]
- Acevedo A, Garnick DW, Lee MT, Horgan CM, Ritter G, Panas L, Reynolds M. Racial and ethnic differences in substance abuse treatment initiation and engagement. Journal of Ethnicity in Substance Abuse. 2012;11(1):1–21. doi: 10.1080/15332640.2012.652516. doi: 10.1080/15332640.2012.652516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillargeon J, Williams BA, Mellow J, Harzke AJ, Hoge SK, Baillargeon G, Greifinger RB. Parole revocation among prison inmates with psychiatric and substance use disorders. Psychiatric Services. 2009;60(11):1516–1521. doi: 10.1176/appi.ps.60.11.1516. doi: 10.1176/appi.ps.60.11.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Justice Statistics Mental Health and Treatment of Prisoners and Probationers. Screening and eviction for drug abuse and other criminal activity. 2001;66:28776–28806. [Google Scholar]
- Clark R, Ricketts S, McHugo G. Legal system involvement and costs for persons in treatment for severe mental illness and substance use disorders. Psychiatry Services. 1999;50(5):641–647. doi: 10.1176/ps.50.5.641. [DOI] [PubMed] [Google Scholar]
- Corporation for Supportive Housing Frequent users of public services, ending the institutional circuit, changing systems to change lives. 2009 Retrieved from http://www.csh.org/wp-content/uploads/2011/12/Report_FUFBooklet.pdf.
- Draine J, Herman D. Critical time intervention for reentry from prison for persons with mental illness. Psychiatric Services. 2007;58(12):1577–1581. doi: 10.1176/ps.2007.58.12.1577. doi:10.1176/appi.ps.58.12.1577. [DOI] [PubMed] [Google Scholar]
- Drake RE, Wallach MA. Substance abuse among the chronically mentally ill. Hospital and Community Psychiatry. 1989;40(10):1041–1046. doi: 10.1176/ps.40.10.1041. [DOI] [PubMed] [Google Scholar]
- Drake RE, Bartels SJ, Teague GM, Noordsy D, Clark R. Treatment of substance abuse in severely mentally ill patients. Journal of Nervous and Mental Disease. 1993;181(10):606–611. doi: 10.1097/00005053-199310000-00006. [DOI] [PubMed] [Google Scholar]
- Drapalski A, Bennett M, Bellack A. Gender differences in substance use, consequences, motivation to change, and treatment seeking in people with serious mental illness. Substance Abuse & Misuse. 2011;46(6):808–818. doi: 10.3109/10826084.2010.538460. doi:10.3109/10826084.2010.538460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder L. A comparison of the community adjustment of mentally ill offenders with those from the general prison population. Law and Human Behavior. 1991;15(5):477–493. doi:10.1007/BF01650290. [Google Scholar]
- Fisher WH, Wolff N, Grudzinskas AJ, Roy-Bujnowski K, Banks S, Clayfield J. Drug arrests in a cohort of mental health service recipients. Psychiatric Services. 2007;58(11):1448–1453. doi: 10.1176/appi.ps.58.11.1448. doi:10.1176/appi.ps.58.11.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher WH, Roy-Bujnowski K, Grudzinskas AJ, Banks SM, Crockett E, Wolff N. Comparing risk of arrest among public mental health services recipients and the general public. Psychiatric Services. 2011;62(1):67–72. doi: 10.1176/ps.62.1.pss6201_0067. doi:10.1176/appi.ps.62.1.67. [DOI] [PubMed] [Google Scholar]
- Gagliardi GJ, Lovell D, Peterson PD, Jemelka R. Forecasting recidivism in mentally ill offenders released from prison. Law and Human Behavior. 2004;28(2):133–155. doi: 10.1023/b:lahu.0000022319.03637.45. doi:10.1023/B:LAHU.0000022319.03637.45. [DOI] [PubMed] [Google Scholar]
- Godley SH, Finch M, Dougan L, McDonnell M, McDermeit M, Carey A. Case management for dually diagnosed individuals involved in the criminal justice system. Journal of Substance Abuse Treatment. 2000;18(2):137–148. doi: 10.1016/s0740-5472(99)00027-6. doi:10.1016/S0740-5472(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Green CA. Gender and use of substance abuse treatment services. Alcohol Research & Health. 2006;29(1):55–62. [PMC free article] [PubMed] [Google Scholar]
- Green AI, Drake RE. Current epidemiology and emerging interventions for people with co-occurring mental illness and substance use disorders. Journal of Dual Diagnosis. 2011;7:1–3. doi: 10.1080/15504263.2011.571624. doi:10.1080/15504263.2011.571624. [DOI] [PubMed] [Google Scholar]
- Harris V, Koepsell TD. Rearrest among mentally ill offenders. Journal of the American Academy of Psychiatry & the Law. 1998;26(3):393–402. [PubMed] [Google Scholar]
- Hartwell S. Triple stigma: Persons with mental illness and substance abuse problems in the criminal justice system. Criminal Justice Policy Review. 2004;15(1):84–99. doi:10.1176/appi.ps.55.2.145. [Google Scholar]
- Hartwell SW, Deng X, Fisher WH, Fulwiler C, Sambamoorthi U, Johnson C, Siegfriedt J. Harmonizing databases? Using a quasi-experimental design to evaluate a public mental health re-entry program. Evaluation and Program Planning. 2012;35(1):461–472. doi: 10.1016/j.evalprogplan.2012.02.001. doi:10.1016/j.evalprogplan.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopper K, Jost J, Weber S, Haughland G. Homelessness, serious mental illness and the institutional circuit. Psychiatric Services. 1997;48(5):659–665. doi: 10.1176/ps.48.5.659. [DOI] [PubMed] [Google Scholar]
- Jacoby JB, Kozie-Peak B. The benefits of social support for mentally ill offenders: Prison-to-community transitions. Behavioral Sciences & the Law. 1997;15(4):483–501. doi: 10.1002/(sici)1099-0798(199723/09)15:4<483::aid-bsl280>3.0.co;2-f. doi:10.1002/(SICI)1099-0798(199723/09)15:4<483∷AID-BSL280>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- James DJ, Glaze LE. Mental health problems of prison and jail inmates. Bureau of Justice Statistics special report. 2006 Retrieved from http://bjs.ojp.usdoj.gov/content/pub/pdf/mhppji.pdf.
- Jennings J. Does assertive community treatment work with forensic populations? Review and recommendations. The Open Psychiatry Journal. 2009;3:13–19. [Google Scholar]
- Kleinpeter C, Deschenes EP, Blanks J, Lepage CR, Knox M. Providing recovery services for offenders with co-occurring disorders. Journal of Dual Diagnosis. 2006;3:59–85. doi:10.1300/J374v03n01_06. [Google Scholar]
- Lamberti JS, Weisman RL, Schwarzkopf SB, Price N, Ashton RM, Trompeter J. The mentally ill in jails and prisons: Towards an integrated model of prevention. Psychiatric Quarterly. 2001;72(1):63–77. doi: 10.1023/a:1004862104102. doi:10.1023/A:1004862104102. [DOI] [PubMed] [Google Scholar]
- Lovell D, Gagliardi G, Peterson P. Recidivism and use of services among persons with mental illness after release from prison. Psychiatric Services. 2002;53(10):1290–1297. doi: 10.1176/appi.ps.53.10.1290. doi:10.1176/appi.ps.53.10.1290. [DOI] [PubMed] [Google Scholar]
- Mallik-Kane K, Visher CA. Research report. Health and prisoner reentry: How physical, mental, and substance abuse conditions shape the process of reintegration. The Urban Institute; Washington, DC: 2008. Retrieved from http://www.urban.org/UploadedPDF/411617_health_prisoner_reentry.pdf. [Google Scholar]
- Morrissey J, Meyer P, Cuddeback G. Extending assertive community treatment to criminal justice settings: Origins, current evidence, and future directions. Community Mental Health Journal. 2007;43(5):527–544. doi: 10.1007/s10597-007-9092-9. doi:10.1007/s10597-007-9092-9. [DOI] [PubMed] [Google Scholar]
- McGillivray J, Moore M. Substance use by offenders with mild intellectual disability. Journal of Intellectual and Developmental Disability. 2001;26(4):297–310. doi:10.1080/13668250120087317. [Google Scholar]
- Osher FC. Integrated mental health/ substance abuse responses to justice involved persons with co-occurring disorders. Journal of Dual Diagnosis. 2008;4:3–33. doi:10.1300/J374v04n01_02. [Google Scholar]
- Sells DJ, Rowe M, Fisk D, Davidson L. Violent victimization of persons with co-occurring psychiatric and substance use disorders. Psychiatric Services. 2003;54:1253–1257. doi: 10.1176/appi.ps.54.9.1253. doi:10.1176/appi.ps.54.9.1253. [DOI] [PubMed] [Google Scholar]
- Smelson DA, Sawh L, Kane V, Kuhn J, Ziedonis D. The MISSION-VET treatment manual. 2011 Retrieved from http://www.va.gov/HOMELESS/docs/MISSION_Veteran_Treatment_Manual.pdf.
- Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatric Services. 2009;60(6):761–765. doi: 10.1176/ps.2009.60.6.761. [DOI] [PubMed] [Google Scholar]
- Swartz J, Lurigio A. Serious mental illness and arrest: The generalized mediating effect of substance use. Crime & Delinquency. 2007;53(4):581–604. doi:10.1177/0011128706288054. [Google Scholar]
- Theurer G, Lovell D. Recidivism of offenders with mental illness released from prison to an intensive community treatment program. Journal of Offender Rehabilitation. 2008;474(4):385–406. doi:10.1080/10509670801995023. [Google Scholar]
- Wexler HK. The promise of prison-based treatment for dually diagnosed inmates. Journal of Substance Abuse Treatment. 2003;25(3):223–231. doi: 10.1016/s0740-5472(03)00121-1. doi:10.1016/S0740-5472(03)00121-1. [DOI] [PubMed] [Google Scholar]
- Wiseman JP. Stations of the lost: The treatment of skid row alcoholics. The University of Chicago Press; Chicago, IL: 1970. [Google Scholar]