The prevalence of overweight and obesity in adolescents has increased dramatically in the past several decades, with more than 18% of adolescents in the United States obese and 30% of adolescents overweight or obese. African American and Hispanic adolescents are disproportionately affected with higher rates of overweight and obesity compared to White adolescents (21% vs. 15%).1,2 Overweight adolescents are at risk for serious health consequences such as asthma, hyperlipidemia, hypertension, and type 2 diabetes. Overweight and obesity in adolescents have also been associated with psychological consequences such as low self-esteem, stigma, and depression.3 Adolescents, particularly minority youth, are an underserved population with respect to nutrition and health education.4,5 Thus, adolescence is a particularly critical developmental phase for obesity prevention programs.
Prevention is widely advocated as an important strategy to address the rising prevalence of obesity in adolescents6,7,8 as once youth become obese, treatment is difficult.9 School-based obesity prevention programs are one approach to reach adolescents at risk for overweight and obesity as well as engage adolescents in learning strategies to improve health behaviors. Schools also have an existing infrastructure to integrate obesity prevention education into the curriculum. Research on school-based obesity prevention programs has proliferated in the past two decades. The majority of programs have been multi-faceted and comprehensive and include health education (diet and physical activity), behavioral strategies (ie., goal setting), parental support, environmental modification, and/or policy change. Programs vary in curriculum, implementation, length, and supplemental components, such as parental support. Results of numerous meta-analyses and systematic reviews indicate that more than 75% of the programs resulted in significant improvements in knowledge, self-efficacy, and health behavior (physical activity, sedentary behavior, dietary intake).10,11 However, the impact on BMI has been mixed.12,13,14 Change in BMI is challenging to demonstrate in obesity prevention programs for youth who are predominately of normal weight at baseline, particularly if programs and follow-up were of short duration. Lack of improvement in BMI or health behavior may also be because programs were not implemented as intended and the full ‘dose’ of the program was not provided.
One promising solution to the challenge of implementing school-based obesity prevention programs with fidelity is to provide the program using interactive multimedia (ie., internet). With interactive multimedia, the program delivery is standardized and the burden to schools is dramatically reduced.7,15 Adolescents are very technologically savvy, with over 93% active users of the internet.16 Internet obesity prevention programs for youth have demonstrated significant improvements in dietary behaviors,4,17–19 physical activity,4,18–19 and BMI,4 thus demonstrating the potential of this approach in this population. However, few programs have specifically targeted adolescents or evaluated the effect on BMI. One study with adolescents that compared an internet obesity prevention program to traditional classroom education indicated better behavioral and psychosocial outcomes with the internet program. Adolescents also reported that they preferred the media based education over print materials and lectures.4
The complexity of obesity prevention will require multi-faceted and comprehensive community programs12: however, there needs to be a theoretically-based and developmentally appropriate health education and behavior change program at the center. Adolescents need to be knowledgeable about healthy foods and the risks of inactivity; they need to be cognizant of their own behaviors; and they need behavioral skills to promote behavior change.20 The HEALTH[e]TEEN© program was developed to provide interactive education and behavioral support on healthy eating and physical activity to reduce overweight and obesity in adolescents based on principles of interactive technology, social learning theory, and behavior change. Interactive technology contributes to experiential learning by including self-assessments, simulations, problem solving, repetition, and feedback.21 Social learning theory posits that personal factors of knowledge, self-efficacy, and skill development are critical to initiating and maintaining behavior change.22 Self-efficacy and skill development are enhanced through mastery of behavioral skills (goal setting and self-monitoring), observing others who are successful with the targeted behavior change (social modeling) and by verbal encouragement (social persuasion of peers or professional).
Because social learning theory also posits that the development of coping skills aimed at moderating psychological responses (i.e., stress reduction) can further assist individuals to carry out healthy lifestyle behaviors,22 additional lessons on coping skills training (CST) were added to the HEALTH[e]TEEN program and tested in this study. Previous research has demonstrated the efficacy of an in-person CST program in improving metabolic control and quality of life in adolescents with type 1 diabetes23 and improving health behaviors and insulin resistance in youth at-risk for type 2 diabetes.24 Key theoretical components and their operationalization in the HEALT[e]TEEN programs are identified in Table 1.
Table 1.
Theoretical Components of Program
| Principles of Program Development |
Theory Component | How operationalized in program | Programs |
|---|---|---|---|
|
Theory of Interactive Technology |
Interactive technology promotes experiential learning and tailored/individualized feedback. |
Lessons include self-assessment, simulations, problem-solving, repetition, and individualized feedback. |
Both |
| Health coaching and social networking provide individualized feedback. | |||
|
Social Learning Theory |
Knowledge provides necessary, but insufficient precondition to behavior change. |
Lessons provide content. |
Both |
| Confidence to perform a specific task (self-efficacy) is important to behavior change. Self-efficacy is enhanced by mastery of skills (goal setting & self-monitoring). |
Goal setting and self-monitoring included. | ||
| A reality television concept of the program includes diverse relatable characters who demonstrate typical situations (social modeling) in videos, text, and lesson commentary. | |||
| Self-efficacy is enhanced by social modeling and social persuasion. | |||
| Health coaching and social networking provide encouragement and social persuasion. | |||
| Social Learning Theory | Self-efficacy is enhanced by the moderation of psychological responses (ie., stress reduction). | Lessons provide content on stress reduction, assertive communication, conflict resolution, and social problem solving as it relates to healthy eating and physical activity. | HEALTH[e]TEEN + CST only |
Purpose
The purpose of this study was to compare the effectiveness of two school-based internet obesity prevention programs, HEALTH[e]TEEN and HEALTH[e]TEEN + CST, in diverse adolescents on body mass index (BMI), health behaviors (nutrition, physical activity, sedentary behavior), and self-efficacy at 3 and 6 months. It was hypothesized that the addition of CST would enhance the ability of adolescents to make positive health behavior change and thus improve health outcomes compared to the internet obesity prevention program alone. Program participation and satisfaction were also compared. A secondary aim was to explore moderators of intervention efficacy for the two programs.
Method
A randomized clinical trial with cluster randomization by class and repeated measures was conducted. A convenience sample was recruited from 3 high schools in two cities in the northeast between October, 2010 and January, 2011. Sample size was determined by a power analysis, based on data from a previous study of an in-person obesity prevention program.24 For 80% power to test the primary hypothesis, 392 pupils would be required at alpha=0.05.
Procedure
Approvals were obtained from the Yale Institutional Review Board and the Boards of Education prior to study implementation. Informed consent was obtained from a parent or guardian and assent was obtained from adolescents.
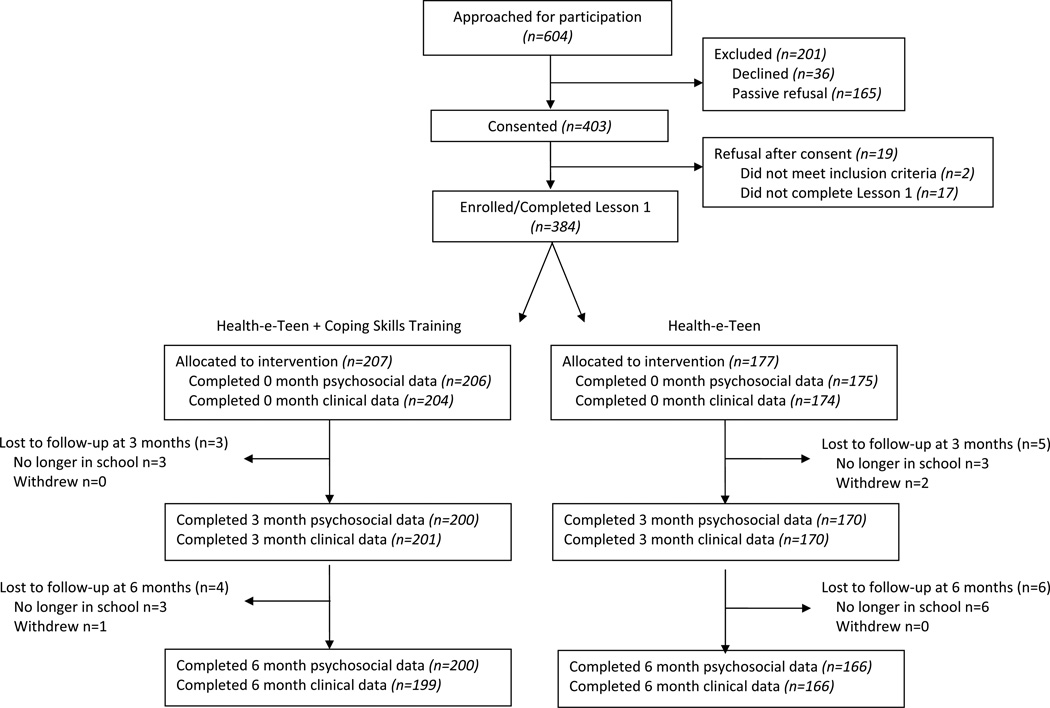
Students enrolled in Health or Biology classes were eligible to participate. Students were excluded if cognitive functioning prohibited them from completing study questionnaires and program materials, as identified by teachers. All students in the targeted classes participated in the program assigned to their class(n=604), though only students who returned consent forms participated in the research study (ie., data collection) (n=384). In total, students from 35 classes across all three schools participated in the study, with 66% of students who were approached consenting to participate in the study (Figure 1). Study participants received a gift card for completion of data collection ($25.00 at time 1; $30.00 at time 2 and 3). Two schools provided the program in class (n=26 classes) while one school provided the program as homework (n=9 classes). Attrition at 6 month follow-up was very low at 5%.
Figure 1.
Consort Table
Teachers and school administrators were involved in all decisions about study protocols to assure optimal implementation. Teachers were provided access to the websites and guidelines to promote student participation. The program was developed to be self-standing with teacher involvement required only to help students log onto the program and monitor student activity to assure that students were participating in the program (rather than exploring other websites). Teachers were also instructed to prompt students to complete lessons and self-monitoring as well as explore all components of the program. The research team was available for any questions or problems encountered during class time. Student participation was monitored bi-monthly by the research team and reported to classroom teachers. If class participation was low, the research team discussed strategies to enhance participation with teachers.
Programs
The major components of the HEALTH[e]TEEN program were lessons, goal setting, self-monitoring, health coaching, and social networking. There were 8 lessons on the topics of nutrition, physical activity, metabolism, and portion control. Lessons were highly interactive and students received individualized feedback via self-assessments and questions on content. Students were encouraged to record their food intake and physical activity each time they logged on, and the program provided a visual display of their progress. Students also set goals and monitored progress with completing goals. A blog by a “coach”, the opportunity to interact with a health coach (graduate nursing student) and other students, and a personal journal section were other components of the program. The HEALTH[e]TEEN + CST included all of the aforementioned components and the addition of 4 lessons on coping skills training (total of 12 lessons). CST lessons included social problem solving, stress reduction, assertive communication, and conflict resolution.25
Measures
Data Collection Procedures
Demographic information was collected from parents at the time of informed consent. Adolescent height, weight, and BMI data were collected in private locations at each school by trained research personnel. Adolescents also completed self-report questionnaires on health behaviors (nutrition, physical activity, sedentary behavior) and self-efficacy at baseline, 3 months, and 6 months. Satisfaction data were collected at 3 months. Self-report questionnaires were either completed online or by paper and pencil forms depending on the accessibility of the computer rooms at the time data collection was due. All paper forms were double-entered into password protected and secure electronic databases. Data comparisons were run to obtain 100% accuracy.
Primary Outcome
BMI
Height was obtained using one wall-mounted stadiometer (Health O Meter Metal Height Rod), calibrated in 1 centimeter intervals and was rounded up to the nearest centimeter. Weight in kilograms was measured to the nearest 0.1kilogram using a floor scale (Omron HBF-400 Body Fat Monitor and Scale). BMI was calculated according to the formula, BMI=kg/m2. Unadjusted BMI scores were used in all analyses based on recent recommendations for evaluating BMI longitudinally in youth.26
Secondary Outcomes
Sedentary behavior
Sedentary behavior was measured using an adapted version of a sedentary behavior questionnaire.27 Items include how many hours per day adolescents spend "watching television or movies", "playing video games", and “working on the computer” separately for a weekday and a weekend. Content validity has been established and survey questions are similar to those used and validated in epidemiologic studies.
Physical activity
Physical activity was measured using the Exercise survey items of the Youth Risk Behaviors Survey, a survey used since 1990 to assess health behaviors in youth.28 Six items evaluate days per week of moderate, vigorous, stretching and strengthening exercise. Adequate test-retest reliability with select items has been reported.29
Nutrition behavior
Nutrition behavior was measured with a 22-item survey adapted from the After School Student Questionnaire that elicits information on typical food and drink intake. Items are consistent with the Healthy People 2020 goals and select items (i.e., fruit and vegetable intake) have evidence of adequate test-retest reliability. In addition to key items evaluated, a total score was calculated by coding items such that a higher score was reflective of better nutrition behavior. The total score range is from 0 (unhealthy behavior) to 97 (healthy behavior). Validity has been demonstrated with significant correlations with select items and food record data.30
Self-efficacy
Self-efficacy for healthy eating and physical activity was measured with two subscales from the After School Student Questionnaire.31 The subscales consist of 12 items on how likely an individual is to eat healthily (8 items) and exercise (4 items). Higher scores are indicative of higher self-efficacy. Cronbach’s alpha was 0.70 for the dietary subscale and 0.82 for the exercise subscale in this study.
Satisfaction
A program satisfaction survey had 6 items on enjoyment, helpfulness, ability to navigate website, practice content, and overall satisfaction on a Likert scale. Mean scores are calculated with a range of 0 (not satisfied) to 5 (highly satisfied). The scale had adequate reliability with a Cronbach’s alpha of 0.80 in this study.
Usage
Usage data included lesson participation (i.e., percent of lessons completed relative to the program assigned) and self-monitoring (number of times students completed selfmonitoring). These data were generated from programming that linked student ID with user statistics.
Data Analysis
Analyses were conducted using SAS 9.2 (SAS Institute, Carry, NC). Descriptive statistics were calculated and groups were compared on baseline characteristics using t-tests for continuous variables and Fisher’s exact tests for categorical variables. To compare the effects of the two programs, mixed effect model analyses with autoregressive covariance structure for repeated data were used, with two groups, three time points, and intent to treat procedures. Differences in rates of change between the groups, based on an interaction of group-by-time in the regression model were used. For an overall effect of time, the group-by-time interaction was removed. Analyses were adjusted for age, gender, and race/ethnicity. Weight and BMI were not normally distributed; therefore these variables were transformed using log-transformation. To describe how strongly outcome changes of participants in the same school and class were correlated, the intraclass correlation coefficients (ICC) were obtained from a repeated mixed model with a random effect of school or class. The ICC’s were ignorable in the change of most outcomes, with the highest ICC observed on vigorous exercise (0.03) and moderate exercise (0.02) for school and on diet self-efficacy (0.02), stretching (0.03), muscle strengthening (0.02), and eating breakfast (0.02) for class. In order to account for the variability among the three schools and classes, a random effect of school or class was added to the model if it was significant. Program participation and satisfaction with programs were compared using t-tests. Because program implementation was different in some classes (homework vs. classroom), we also ran mixed model analyses exploring the effect of implementation by program.
Potential moderators of program efficacy included adolescent characteristics (gender, race/ethnicity, and weight status at baseline) and program usage (percent lessons completed). To examine if program efficacy was influenced by a potential moderator, an interaction moderatorby- time was tested for each outcome in the regression model. For the program usage moderation analysis, program usage was dichotomized into 2 groups consisting of students who completed 100% of lessons (n=233) vs. students who completed less than 100% of lessons (n=152).
Results
The mean age of students was 15.31 years (+0.69) with a mean BMI of 24.69 (+5.58). The majority of were girls (62%) and of diverse race/ethnicity (65% non-white). Thirty-eight percent of adolescents were overweight or obese, with 16% obese. Participants reported high sedentary behavior, moderate physical activity, and poor eating behaviors. There were no significant differences between groups at baseline (Tables 2 and 3). There were significant differences between schools with respect to gender and race/ethnicity; therefore these variables were controlled in all subsequent analyses.
Table 2.
Baseline Characteristics
| HEALTH[e]TEEN + CST N=207 |
HEALH[e]TEEN N=177 |
P-value | ||
|---|---|---|---|---|
| N (%) | N (%) | |||
| Gender | Male | 77 (37.2%) | 69 (39.0%) | .72(a) |
| Female | 130 (62.8%) | 108 (61.0%) | ||
| Age | 14–15 | 139 (67.2%) | 125 (70.6%) | .46(a) |
| 16–17 | 68 (32.8%) | 52 (29.4%) | ||
| Income | <$40,000 | 68 (42.2%) | 61 (45.2%) | .08(b) |
| $40,000–$79,999 | 54 (33.5%) | 58 (43.0%) | ||
| $80,000 + | 39 (24.2%) | 16 (11.8%) | ||
| Race | White, Non-Hispanic | 76 (37.3%) | 57 (33.9%) | .46(a) |
| White, Hispanic/Latino | 44 (21.6%) | 40 (23.8%) | ||
| African American | 59 (28.9%) | 42 (25.0%) | ||
| Other | 25 (12.3%) | 29 (17.3%) | ||
| Body Mass Index | BMI<25 | 125 (61.0%) | 111 (63.8%) | .57(a) |
| BMI≥25 | 80 (39.0%) | 63 (36.2%) | ||
| Adherences | Completed 100% | 109 (52.7%) | 123 (69.5%) | <.01(a) |
| Completed Less than 100% | 98 (47.3%) | 54 (30.5%) | ||
| N: Mean (SD) | N: Mean (SD) | |||
| Parent’s Education years | 146: 12.5 (3.0) | 133: 12.4 (3.3) | .87(c) | |
Note.
is p-values from chi-square test for cross table and
is p-values from Cochran-Armitage Trend test.
Parent’s education was tested based on Wilcoxon Rank Sum test (c).
BMI categories were classified based on the age-adjusted percentile of BMI for each gender (Resource: CDC).
Table 3.
Behavioral variables at baseline
| HEALTH[e]TEEN +CST N=207 |
HEALTH[e]TEEN N=177 |
P-value | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Self-Efficacy | ||||
| Healthy Diet (Range 0–24)) | 14.9 (3.3) | 15.0 (3.4) | .57(c) | |
| Healthy Exercise (Range 0–12) | 8.1 (2.4) | 8.3 (2.4) | .45(c) | |
| Sedentary Behavior | ||||
| Weekday (~hours/day) | 8.8 (2.9) | 9.1 (3.2) | .50(c) | |
| Weekend (~hours/day) | 9.0 (3.1) | 9.8 (3.5) | .04(c) | |
| Physical Activity | ||||
| Vigorous (days/week of 20 minutes) | 3.37 (2.43) | 3.29 (2.31) | .83(d) | |
| Moderate (days/week of 30 minutes) | 3.79 (2.42) | 3.73 (2.42) | .83(d) | |
| Stretching (days/week) | 2.49 (2.51) | 2.17 (2.49) | .21(d) | |
| Muscle Strengthening (days/week) | 2.57 (2.58) | 2.13 (2.41) | .11(d) | |
|
Eating Behavior (Children’s Health Behavior at Baseline) (Range 0–97) |
52.5 (12.3) | 53.8 (11.5) | .29(c) | |
| Fruits and Vegetables (servings/day) | 4.39 (2.25) | 4.53 (2.05) | .53(c) | |
| Breakfast (times/week) | 3.48 (2.64) | 3.69 (2.56) | .40(d) | |
| Sugar Drinks (servings/day) | 6.47 (3.25) | 6.06 (2.81) | .20(c) | |
| Fast Food (times/week) | 0.89 (1.11) | 0.78 (0.97) | .50(d) | |
| Junk Food (servings/day) | 3.10 (2.66) | 2.91 (2.14) | .97(d) | |
Note.
is p-values obtained from T-test comparing means between two groups and
is p-values obtained from Wilcoxon Rank Sum test (nonparametric test).
Weight intention was tested by chi-square test (e)
Satisfaction with the programs was high. The mean satisfaction score was 3.58 (+0.68). There was no significant difference between groups with respect to satisfaction (p=.26). Participation was also high with adolescents completing 83% of lessons (median 100%). In each group, more than half of participants completed all lessons (53% of participants in HEALTH[e]TEEN + CST and 70% in HEALTH[e]TEEN). Adolescents completed self-monitoring assessments 5.26 times (+2.75; median 5) over the 8–12 lessons. Adolescents of the HEALTH[e]TEEN + CST completed fewer lessons (p=.001), yet had higher participation in self-monitoring (p<.001).
In mixed model analyses, using intent to treat procedures and controlling for age, gender, and race/ethnicity, there were no significant differences between groups on any of the outcome variables (Table 4). However, there were significant improvements in the health behaviors of adolescents in both groups over 6 months. Adolescents demonstrated a significant increase in self efficacy (p<.001), healthy eating behavior (p<.001), fruit and vegetable intake (p<.001), moderate and vigorous exercise (p<.001), and stretching exercises (p<.01) along with a significant decrease in sugar-sweetened drinks (p<.001), junk food intake (p<.01), and sedentary behavior (p<.001). There was no time effect with respect to muscle strengthening, eating breakfast, and junk food intake. Since weight and BMI generally increase during adolescence, the time effect on weight and BMI change was tested against the projected increase due to change in age. There was a marginally significant decrease in weight (p=.05), but not BMI (p=.86).
Table 4.
Change of outcomes over 6 months
| Change of Outcomes over 6 months | Time Effect(a) |
||||
|---|---|---|---|---|---|
| Baseline Mean (SD) |
3 months Mean (SD) |
6 months Mean (SD) |
|||
| Weight & Body Mass Index | |||||
| Weight (lb) | All | 147.7 (39.2) | 148.5 (39.2) | 148.4 (38.0) | .05 |
| HEALTH[e]TEEN + CST | 149.4 (39.7) | 150.0 (38.0) | 150.0 (37.7) | .09 | |
| HEALTH[e]TEEN | 145.7 (38.6) | 146.8 (38.4) | 146.3 (38.3) | .06 | |
| Time×Group(b) | .6727 | ||||
| Body Mass Index | All | 24.6 (5.6) | 24.8 (5.6) | 24.9 (5.5) | .86 |
| HEALTH[e]TEEN + CST | 24.9 (5.8) | 25.0 (5.7) | 25.1 (5.6) | .87 | |
| HEALTH[e]TEEN | 24.3 (5.4) | 24.5 (5.4) | 24.6 (5.4) | .87 | |
| Time×Group(b) | .9945 | ||||
| Self-efficacy | |||||
| Healthy Diet (Range 0–24) | All | 14.9 (3.3) | 15.7 (3.4) | 16.0 (3.5) | <.01 |
| HEALTH[e]TEEN + CST | 14.9 (3.4) | 15.5 (3.3) | 15.9 (3.4) | <.01 | |
| HEALTH[e]TEEN | 15.0 (3.3) | 15.9 (3.5) | 16.2 (3.5) | <.01 | |
| Time×Group(b) | .7128 | ||||
| Exercise (Range 0–12) | All | 8.2 (2.4) | 8.8 (2.3) | 8.9 (2.3) | <.01 |
| HEALTH[e]TEEN + CST | 8.1 (2.4) | 8.7 (2.3) | 8.9 (2.4) | <.01 | |
| HEALTH[e]TEEN | 8.3 (2.4) | 8.9 (2.2) | 8.9 (2.3) | <.01 | |
| Time×Group(b) | .4556 | ||||
| Sedentary Behaviors | |||||
| Weekday (~hours/day) | All | 5.9 (2.3) | 5.5 (2.2) | 5.2 (2.3) | <.01 |
| HEALTH[e]TEEN + CST | 5.9 (2.2) | 5.4 (2.2) | 5.2 (2.3) | <.01 | |
| HEALTH[e]TEEN | 5.9 (2.5) | 5.6 (2.2) | 5.3 (2.3) | <.01 | |
| Time×Group(b) | .9557 | ||||
| Weekend (~hours/day) | All | 6.2 (2.7) | 5.7 (2.7) | 5.4 (2.7) | <.01 |
| HEALTH[e]TEEN + CST | 6.1 (2.6) | 5.6 (2.7) | 5.3 (2.6) | <.01 | |
| HEALTH[e]TEEN | 6.4 (2.8) | 5.8 (2.7) | 5.4 (2.9) | <.01 | |
| Time×Group(b) | .3967 | ||||
| Exercise | |||||
| Vigorous (days/week of 20 minutes) | All | 3.4 (2.4) | 3.9 (2.2) | 4.1 (2.1) | <.01 |
| HEALTH[e]TEEN + CST | 3.4 (2.4) | 4.1 (2.2) | 4.1 (2.1) | <.01 | |
| HEALTH[e]TEEN | 3.4 (2.3) | 3.7 (2.2) | 4.1 (2.1) | <.01 | |
| Time×Group(b) | .9829 | ||||
| Moderate (days/week of 30 minutes) | All | 3.8 (2.4) | 4.0 (2.2) | 4.3 (2.1) | <.01 |
| HEALTH[e]TEEN + CST | 3.8 (2.4) | 4.2 (2.2) | 4.4 (2.1) | <.01 | |
| HEALTH[e]TEEN | 3.9 (2.4) | 3.9 (2.1) | 4.3 (2.0) | .06 | |
| Time×Group(b) | .5958 | ||||
| Stretching (days/week) | All | 2.4 (2.5) | 2.8 (2.4) | 2.9 (2.5) | . <.01 |
| HEALTH[e]TEEN + CST | 2.5 (2.5) | 3.0 (2.5) | 3.0 (2.6) | .03 | |
| HEALTH[e]TEEN | 2.2 (2.5) | 2.5 (2.3) | 2.8 (2.5) | .03 | |
| Time×Group(b) | .8253 | ||||
| Muscle Strengthening (days/week) | All | 2.4 (2.5) | 2.8 (2.4) | 2.6 (2.5) | .12 |
| HEALTH[e]TEEN + CST | 2.6 (2.6) | 2.8 (2.4) | 2.8 (2.5) | .18 | |
| HEALTH[e]TEEN | 2.2 (2.4) | 2.7 (2.5) | 2.4 (2.5) | .40 | |
| Time×Group(b) | .7844 | ||||
| Eating Behaviors | |||||
| Fruits & Vegetables (servings/day) | All | 4.5 (2.2) | 4.9 (2.2) | 5.0 (2.0) | <.01 |
| HEALTH[e]TEEN + CST | 4.4 (2.3) | 5.0 (2.3) | 4.9 (2.1) | <.01 | |
| HEALTH[e]TEEN | 4.6 (2.0) | 4.9 (2.0) | 5.1 (1.9) | <.01 | |
| Time×Group(b) | .9162 | ||||
| Breakfast (days/week) | All | 3.6 (2.6) | 4.1 (2.5) | 3.8 (2.6) | .18 |
| HEALTH[e]TEEN + CST | 3.4 (2.6) | 4.1 (2.6) | 3.7 (2.7) | .29 | |
| HEALTH[e]TEEN | 3.7 (2.5) | 4.2 (2.4) | 3.9 (2.5) | .40 | |
| Time×Group(b) | .9211 | ||||
| Sugar Drinks (servings/day of soda and fruit juice) | All | 6.3 (3.1) | 5.8 (2.8) | 5.6 (2.8) | <.01 |
| HEALTH[e]TEEN + CST | 6.5 (3.3) | 5.9 (2.9) | 5.8 (2.9) | <.01 | |
| HEALTH[e]TEEN | 6.2 (2.8) | 5.6 (2.8) | 5.4 (2.6) | .01 | |
| Time×Group(b) | .8954 | ||||
| Fast Food (times/week) | All | 0.85 (1.05) | 0.78 (1.01) | 0.82 (1.02) | .78 |
| HEALTH[e]TEEN + CST | 0.90 (1.12) | 0.83 (1.09) | 0.80 (1.03) | .18 | |
| HEALTH[e]TEEN | 0.78 (0.96) | 0.72 (0.91) | 0.85 (1.00) | .28 | |
| Time×Group(b) | .0892 | ||||
| Junk Food (servings/day) | All | 3.0 (2.4) | 2.5 (2.1) | 2.6 (2.2) | <.01 |
| HEALTH[e]TEEN + CST | 3.1 (2.7) | 2.5 (2.2) | 2.7 (2.4) | .01 | |
| HEALTH[e]TEEN | 2.9 (2.2) | 2.4 (2.0) | 2.5 (1.9) | .06 | |
| Time×Group(b) | .7861 | ||||
| Total Eating Behavior (Range 0–97) | All | 52.9 (12.0) | 56.7 (11.5) | 56.8 (11.3) | <.01 |
| HEALTH[e]TEEN + CST | 52.4 (12.3) | 56.8 (11.9) | 56.4 (11.9) | <.01 | |
| HEALTH[e]TEEN | 53.5 (11.6) | 56.6 (11.1) | 57.2 (10.6) | <.01 | |
| Time×Group(b) | .6011 | ||||
Note.
Time effect(a) presents p-values for testing the improvement of outcome in each group after adjusting for age, gender, and race.
Time×Group(b) presents p-value for comparing the intervention effect between CST+HET and HET Only after adjusting for age, gender, and race.
With respect to program implementation, there was no difference between classroom and homework implementation by program on any outcome, with the exception of weight and BMI. For students in the HEALTH[e]TEEN + CST group, there was less increase in weight (p=.03) and BMI (p=.05) compared to the normal growth curve in the homework group compared to the in-class group. Across both programs, there were trends for students of the classroom implementation group to have greater improvements in self-efficacy, sedentary behavior, exercise, and eating behavior.
Adolescent age, gender, race/ethnicity, weight status (normal, overweight, or obese), and program usage (percent lessons completed) were tested for moderation of program efficacy on the outcomes of healthy eating, sedentary behavior, and moderate or vigorous exercise. There was significantly greater improvement in breakfast behavior of girls compared to boys (p=.02). Girls also significantly reduced junk food intake (p<.001), while males did not (p=.58). There were no other significant moderators of healthy eating, sedentary behavior, or exercise. Since program usage (lesson participation) was different between the 2 groups, the moderation of program usage was tested separately for each group (Table 5). Both groups improved moderate to vigorous exercise significantly for participants who completed all lessons (p=.005), but not for participants with lower lesson participation. However, the interaction of program usage-by-time was statistically significant only on moderate exercise in the HEALTH[e]TEEN program (p=.03). There were trends for participants with high program usage to have greater improvements in weekend sedentary behavior and junk food consumption compared to those with less program usage (Table 5).
Table 5.
Moderation Effect of Program Completion (100% completion vs. less than 100%)
| Outcomes | Estimated Coefficient of Time Effect | ||||
|---|---|---|---|---|---|
| HEALTH[e]TEEN + CST | HEALTH[e}TEEN | ||||
| Coeff (StdErr) |
P-value | Coeff (StdErr) |
P-value | ||
| Sedentary – Weekdays | |||||
| Completed all sessions | −0.09 (0.04) | .0215 | −0.12 (0.04) | .0023 | |
| Completed Less than 100% | −0.11 (0.04) | .0107 | −0.04 (0.06) | .5136 | |
| Time×Program Usage | .7785 | .2631 | |||
| Sedentary – Weekend | |||||
| Completed all sessions | −0.14 (0.05) | .0019 | −0.18 (0.04) | <.0001 | |
| Completed Less than 100% | −0.09 (0.05) | .0614 | −0.11 (0.07) | .1214 | |
| Time×Program Usage | .4368 | .3724 | |||
| Vigorous Exercise | |||||
| Completed all sessions | 0.16 (0.04) | .0001 | 0.16 (0.04) | <.0001 | |
| Completed Less than 100% | 0.08 (0.04) | .0840 | 0.03 (0.06) | .5574 | |
| Time×Program Usage | .1520 | .0846 | |||
| Moderate Exercise | |||||
| Completed all sessions | 0.13 (0.04) | .0044 | 0.12 (0.04) | .0048 | |
| Completed Less than 100% | 0.05 (0.05) | .2623 | −0.05 (0.06) | .4025 | |
| Time×Program Usage | .2329 | .0249 | |||
| Fruits & Vegetables | |||||
| Completed all sessions | 0.09 (0.04) | .0183 | 0.06 (0.03) | .0750 | |
| Completed Less than 100% | 0.08 (0.04) | .0638 | 0.12 (0.05) | .0278 | |
| Time×Program Usage | .7850 | .3807 | |||
| Breakfast | |||||
| Completed all sessions | 0.04 (0.04) | .3518 | 0.00 (0.04) | .9892 | |
| Completed Less than 100% | 0.03 (0.04) | .5673 | 0.10 (0.07) | .1380 | |
| Time×Program Usage | .8206 | .2156 | |||
| Sugar Drinks | |||||
| Completed all sessions | −0.10 (0.06) | .0645 | −0.12 (0.04) | .0100 | |
| Completed Less than 100% | −0.10 (0.06) | .0840 | −0.08 (0.07) | .2956 | |
| Time×Program Usage | .9907 | .5995 | |||
| Junk Foods | |||||
| Completed all sessions | −0.09 (0.04) | .0498 | −0.09 (0.04) | .0234 | |
| Completed Less than 100% | −0.07 (0.05) | .1438 | −0.00 (0.06) | .9475 | |
| Time×Program Usage | .7717 | .2351 | |||
Time × Program Usage represents the interaction effect between Time and program completion on outcome for each group.
Discussion
The purpose of this study was to compare the effectiveness of two school-based obesity prevention programs for adolescents provided over the internet. The primary hypothesis, that adolescents who participated in HEALTH[e]TEEN + CST would demonstrate better self-efficacy and health behaviors and less weight gain compared to an internet educational and behavioral program alone was not supported. The lack of differential effects of CST may have been due to the short-term follow-up or to implementation factors. CST may take longer to have effects, as coping skills take time and practice to develop and be able to use in social situations. Adolescents in the CST group also completed a lower percent of assigned lessons compared to the HEALTH[e]TEEN group, which may be related to the addition of 4 sessions. Standard procedures were used in implementing the programs across classes and groups. Variations in implementation occurred, however, with the program being provided as homework in some classes. In an exploratory analysis, there was some indication that program implementation may affect outcomes; however interpretation of this must be cautious due to the small sample size of the homework implementation group and the confound that all homework implementation occurred in one school. Variations across schools that could affect implementation and outcome included scheduling media rooms, level of teacher involvement, and unanticipated school closings. Studies conducted in highly unstable environments require different approaches, especially in community-based effectiveness trials such as this.32
Despite a lack of differential effects between programs, results of this study indicate that both programs improved adolescents’ self-efficacy and health behaviors in the short-term. Thus, internet education and behavioral support have the potential to improve health outcomes in adolescents. This is an important finding as programs that contribute to healthy dietary and physical activity behaviors in adolescents are greatly needed. The complexity of obesity prevention in adolescents will require multi-faceted and comprehensive programs in the future; however, central to such programs needs to be a theoretically-based and developmentally appropriate program that has been systematically developed and evaluated. More research with programs of longer duration and follow-up are needed to determine the effect on BMI as no change in BMI was demonstrated in this study of short duration.
Results of this study also indicate that school-based internet obesity prevention programs are appealing to adolescents as demonstrated by high participation and satisfaction. Benefits of multimedia obesity prevention programs include the ability to present content in an engaging and interactive format that is part of the world of today’s adolescents, to provide individualized feedback, and for students to learn at their own pace.15 Adolescents have reported that they preferred media based obesity prevention education over print materials and lectures. 4
Results of the moderation analysis indicated that girls improved select eating behaviors compared to boys, which is consistent with previous school-based obesity prevention studies, demonstrating that girls have higher participation18 and better outcomes.33,34 Girls may respond better to cognitive-behavioral programs based on social learning theory and may have heightened enthusiasm for programs due to concerns about their weight and body shape.35–37 There were not any other demographic or clinical characteristics that moderated program efficacy with respect to healthy eating, physical activity or sedentary behavior. Thus the program was equally effective across race/ethnicity, age, and adolescent weight status. There was some indication that program usage moderated improvement in select outcomes. Participation in internet programs is important, as several studies have shown a positive relationship between user logons or lesson completion and improved outcomes.19,38 A recent study indicated that adolescents were more likely to participate consistently in an internet program provided during school time compared to a program designed to completed on their own time.39 This suggests that school-based programs may be the best way to enhance participation in internet obesity prevention programs, particularly when considering the potential issue of access to the internet for minority and low-income populations.
Findings of this study must be interpreted in light of several limitations. The sample was from one geographical location and while inclusive of adolescents of diverse race/ethnicity, 34% of adolescents declined to participate in the study. Therefore, results of the study may not be generalizable to other adolescents. Teacher enthusiasm, technology expertise, or teaching style (ie., classroom control, monitoring of homework completion) was not systematically evaluated in this study, which may have influenced participation and outcomes. In addition, the outcomes of self-efficacy and health behaviors were self-report measures. However, these measures were brief, have been widely used with adolescents and have evidence of reliability and validity. As noted above, follow-up was limited to 6 months in this ARRA-funded study, which may have attenuated the impact of the program. Lastly, data on pubertal status was not collected, which impacts BMI change in adolescents. Given the age of the adolescents and BMI, it is highly likely that the majority of these youth were in advanced puberty.
Directions for Future Research
There are several important directions for future research. First, research is needed on school-based internet obesity prevention programs of longer duration that include a maintenance component. Follow-up of at least one year may be necessary to demonstrate a significant impact on BMI in adolescents. Second, future research on mediators and moderators to program efficacy are needed. Other intermediate outcomes, such as fitness level and body composition should be evaluated in future research. Intrinsic factors such as academic performance, student preferred learning style, and motivation may influence participation, satisfaction as well as outcomes of an internet obesity prevention program and should be considered in future research. Lastly, future research on internet obesity prevention programs for adolescents should include a systematic evaluation of implementation. While providing an obesity prevention program via the internet standardizes content, implementation factors such as teacher enthusiasm, teacher technology skills, classroom implementation, and classroom discussion may influence outcomes.
Acknowledgements
NIH/NINR: RC1NR011594
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to disclose
An abbreviated version of this manuscript was presented at the American Diabetes Association 72nd cientific Sessions in Philadelphia, PA, June 8–12, 2012.
Contributor Information
Robin Whittemore, Yale School of Nursing, New Haven, CT 06536, robin.whittemore@yale.edu, 203-737-2351.
Sangchoon Jeon, Yale School of Nursing.
Margaret Grey, Dean, Annie Goodrich Professor of Nursing, Yale School of Nursing.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. [Accessed 22 February 2012];J Am Med Assoc. 2010 303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. [Accessed 7 April 2012];J Am Med Assoc. 2010 303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 3.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. [Accessed 7 April 2012];Arch Dis Child. 2003 88(9):748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casazza K, Ciccazzo M. The method of delivery of nutrition and physical activity information may play a role in eliciting behavior changes in adolescents. [Accessed 22 February 2012];Eating Behav. 2007 8(1):73–82. doi: 10.1016/j.eatbeh.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Power TG, Bindler RC, Goetz S, Daratha KB. Obesity prevention in early adolescence: Student, parent, and teacher views. [Accessed 10 April 2012];J Sch Health. 2010 80(1):13–19. doi: 10.1111/j.1746-1561.2009.00461.x. [DOI] [PubMed] [Google Scholar]
- 6.Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: Health in the balance: Executive summary. [Accessed 22 February 2012];J Am Diet Assoc. 2005 105(1):131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 7.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. School-based obesity prevention: A blueprint for taming the epidemic. [Accessed 22 February 2012];Am J Health Behav. 2002 26(6):486–493. doi: 10.5993/ajhb.26.6.9. [DOI] [PubMed] [Google Scholar]
- 8.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. [Accessed 22 February 2012];Psychol Bull. 2006 132(5):667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caballero B. Obesity prevention in children: Opportunities and challenges. [Accessed 22 February 2012];Int J Obes. 2004 28(SUPPL. 3):S90–S95. doi: 10.1038/sj.ijo.0802797. [DOI] [PubMed] [Google Scholar]
- 10.Flodmark C, Marcus C, Britton M. Interventions to prevent obesity in children and adolescents: A systematic literature review. [Accessed 22 February 2012];Int J Obes. 2006 30(4):579–589. doi: 10.1038/sj.ijo.0803290. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity. A meta-analysis. [Accessed 22 February 2012];Am J Prev Med. 2009 37(5):418–427. doi: 10.1016/j.amepre.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Gittelsohn J, Kumar MB. Preventing childhood obesity and diabetes: Is it time to move out of the school? [Accessed 22 February 2012];Pediatr Diabetes. 2007 8(SUPPL. 9):55–69. doi: 10.1111/j.1399-5448.2007.00333.x. [DOI] [PubMed] [Google Scholar]
- 13.Kanekar A, Sharma M. Meta-analysis of school-based childhood obesity interventions in the U.K. and U.S. [Accessed 16 March 2012];Int Q Community Health Educ. 2009 29(3):241–256. doi: 10.2190/IQ.29.3.d. [DOI] [PubMed] [Google Scholar]
- 14.Katz DL. School-based interventions for health promotion and weight control: Not just waiting on the world to change. [Accessed 16 March 2012];Annu Rev Public Health. 2009 30:253–272. doi: 10.1146/annurev.publhealth.031308.100307. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. [Accessed 7 April 2012];Obes Rev. 2011 12(501):e298–e314. doi: 10.1111/j.1467-789X.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- 16.Lenhart A, Arafeh S, Smith A, Macgill A. The lives of teens and their technology. [Accessed February 22, 2012]; http://www.pewinternet.org/Reports/2008/Writing-Technology-and-Teens/04-The-Lives-of-Teens-and-Their-Technology/02-Nearly-all-teens-use-the-internet.aspx. Updated 2008. [Google Scholar]
- 17.Ezendam NP, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote EnergyBalance among adolescents: Results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166(3):248–255. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 18.Mauriello LM, Ciavatta MMH, Paiva AL, et al. Results of a multi-media multiple behavior obesity prevention program for adolescents. [Accessed 16 March 2012];Prev Med. 2010 51(6):451–456. doi: 10.1016/j.ypmed.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frenn M, Malin S, Brown RL, et al. Changing the tide: An internet/video exercise and low- fat diet intervention with middle-school students. [Accessed 16 March 2012];Appl Nurs Res. 2005 18(1):13–21. doi: 10.1016/j.apnr.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Hoelscher DM, Evans A, Parcel GS, Kelder SH. Designing effective nutrition interventions for adolescents. J Am Diet Assoc. 2002;102(3 Suppl):S52–S63. doi: 10.1016/s0002-8223(02)90422-0. [DOI] [PubMed] [Google Scholar]
- 21.Lieberman DA. Interactive video games for health promotion. In: Street R, Gold W, Manning T, editors. Health promotion and interactive technology: Theoretical applications and future directions. Mahwah, NJ: Lawrence Erlbaum; 1997. pp. 103–120. [Google Scholar]
- 22.Bandura A. The anatomy of stages of change. [Accessed 10 April 2012];Am J Health Promot. 1997 12(1):8–10. doi: 10.4278/0890-1171-12.1.8. [DOI] [PubMed] [Google Scholar]
- 23.Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. [Accessed 7 April 2012];J Pediatr. 2000 137(1):107–113. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- 24.Grey M, Jaser SS, Holl MG, Jefferson V, Dziura J, Northrup V. A multifaceted school-based intervention to reduce risk for type 2 diabetes in at-risk youth. [Accessed 22 February 2012];Prev Med. 2009 49(2–3):122–128. doi: 10.1016/j.ypmed.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grey M, Boland EA, Davidson M, Yu C, Tamborlane WV. Coping skills training for youths with diabetes on intensive therapy. [Accessed 15 April 2012]; [doi: 10.1016/S0897-1897(99)80123-2];Appl Nurs Res. 1999 12(1):3–12. doi: 10.1016/s0897-1897(99)80123-2. [DOI] [PubMed] [Google Scholar]
- 26.Berkey CS, Colditz GA. Adiposity in adolescents: Change in actual BMI works better than change in BMI z score for longitudinal studies. [Accessed 10 April 2012];Ann Epidemiol. 2007 17(1):44–50. doi: 10.1016/j.annepidem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 27.Robinson TN, Killen JD. Ethnic and gender differences in the relationships between television viewing and obesity, physical activity, and dietary fat intake. Journal of Health Education. 1995;26(2):S91–S98. [Google Scholar]
- 28.Centers for Disease Control and Prevention. Youth risk behavior survey. 2009 http://www.cdc.gov/yrbs.
- 29.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. [Accessed 7 April 2012];J Adolesc Health. 2002 31(4):336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 30.Prochaska JJ, Sallis JF. Reliability and validity of a fruit and vegetable screening measure for adolescents. [Accessed 7 April 2012];J Adolesc Health. 2004 34(3):163–165. doi: 10.1016/j.jadohealth.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 31.Kelder S, Hoelscher DM, Barroso CS, Walker JL, Cribb P, Hu S. The CATCH kids club: A pilot after-school study for improving elementary students' nutrition and physical activity. [Accessed 7 April 2012];Public Health Nutr. 2005 8(2):133–140. doi: 10.1079/phn2004678. [DOI] [PubMed] [Google Scholar]
- 32.Buckwalter KC, Grey M, Bowers B, et al. Intervention research in highly unstable environments. [Accessed 10 April 2012];Res Nurs Health. 2009 32(1):110–121. doi: 10.1002/nur.20309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maes L, Cook TL, Ottovaere C, et al. Pilot evaluation of the HELENA (healthy lifestyle in europe by nutrition in adolescence) food-O-meter, a computer-tailored nutrition advice for adolescents: A study in six european cities. [Accessed 22 February 2012];Public Health Nutr. 2011 14(7):1292–1302. doi: 10.1017/S1368980010003563. [DOI] [PubMed] [Google Scholar]
- 34.Haerens L, Deforche B, Maes L, Stevens V, Cardon G, De Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. [Accessed 22 February 2012];Obesity. 2006 14(5):847–854. doi: 10.1038/oby.2006.98. [DOI] [PubMed] [Google Scholar]
- 35.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: An evidence-based review. [Accessed 22 February 2012];Obesity. 2008 16(5):1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 36.O'Dea JA, Caputi P. Association between socioeconomic status, weight, age and gender, and the body image and weight control practices of 6- to 19-year-old children and adolescents. Health Educ Res. 2001;16(5):521–532. doi: 10.1093/her/16.5.521. [DOI] [PubMed] [Google Scholar]
- 37.Paxton SJ, Wertheim EH, Gibbons K, Szmukler GI, Hillier L, Petrovich JL. Body image satisfaction, dieting beliefs, and weight loss behaviors in adolescent girls and boys. [Accessed 22 February 2012];J Youth Adolescence. 1991 20(3):361–379. doi: 10.1007/BF01537402. [DOI] [PubMed] [Google Scholar]
- 38.Williamson DA, Davis Martin P, White MA, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent african-american girls. [Accessed 24 February 2012];Eating Weight Disord. 2005 10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 39.Neil AL, Batterham P, Christensen H, Bennett K, Griffiths KM. Predictors of adherence by adolescents to a cognitive behavior therapy website in school and community-based settings. [Accessed 24 February 2012];J Med Internet Res. 2009 11(1) doi: 10.2196/jmir.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]