Abstract
Purpose
This longitudinal study examines the association between homelessness and injection drug use initiation among a cohort of street-involved youth in a setting of high prevalence crystal methamphetamine use.
Methods
Data were derived from the At-Risk Youth Study, a prospective cohort of street-involved youth aged 14 to 26 recruited between September 2005 and November 2011. Cox proportional hazards regression was used to identify factors independently associated with time to injection initiation.
Results
Among 422 street-youth who had never injected at baseline, 77 injection initiation events were observed during follow-up. Homelessness was independently associated with injection initiation in multivariate Cox regression (Relative Hazard: 1.80 [95% CI: 1.13–2.87]) after adjusting for crystal methamphetamine use and other potential confounders.
Conclusions
These findings highlight that homelessness is a key risk factor for injection initiation among street-involved youth. Supportive housing interventions for street-youth may help prevent injection drug use initiation among this high-risk population.
Keywords: Youth, injection drug use, initiation, homelessness
Introduction
Street-involved youth experience numerous health and social challenges, and frequently report multiple barriers to obtaining housing [1]. Indeed, homelessness among street-involved youth is common and current data indicate the trend is increasing [2]. Injection drug use among this population is also prevalent and new injectors are often more likely to engage in risky injection practices that increase transmission of HIV and other infectious diseases [3]. Furthermore, in many urban settings, use of crystal methamphetamine is growing and may be contributing to increased initiation into injection drug use and related risk behaviors [4].
In the context of crystal methamphetamine epidemics characterized by alarmingly high rates of syringe sharing and HIV risk behavior [3, 4], the potential relationship between homelessness and injection initiation is of international interest given that risks related to homelessness may be highly amenable to intervention. The present study was conducted to examine if homelessness remains a key risk factor for injection initiation among a population of street-involved youth with a high prevalence of crystal methamphetamine use.
Methods
Data were derived from the At-Risk Youth Study (ARYS), which is a prospective cohort of street-involved youth in Vancouver, Canada. Street-involved youth are defined as youth age 14–26, who are absolutely, periodically or temporally at risk of being homeless, and spend a substantial amount of time on the street or heavily involved in the street economy [4]. The ARYS cohort has been described in detail previously [3,4]. In brief, eligibility criteria for the study included age 14–26 years and use of illicit drugs other than marijuana in the past 30 days. Interviews were conducted from September 2005 to November 2011. The study has been ethically approved.
The primary outcome was time to injection initiation and the primary independent variable of interest was homelessness in the last six months, defined as sleeping on the street or having no fixed address. To adjust for variables that might confound the relationship between injection initiation and homelessness, we examined the following covariates: gender (male vs. female), age (per year increase), ethnicity (Caucasian vs. other), daily consumption of alcohol, Marijuana use, non-injection cocaine use, crack cocaine smoking, non-injection crystal methamphetamine use, and non-injection heroin use (yes vs. no for all substance use variables). Substance use variables, as well as homelessness, refer to situations and behaviors over the previous six months and were treated as time-updated covariates on the basis of semi annual follow-up data. In addition, substance use variables were lagged to the previous available observation to protect against reverse causality.
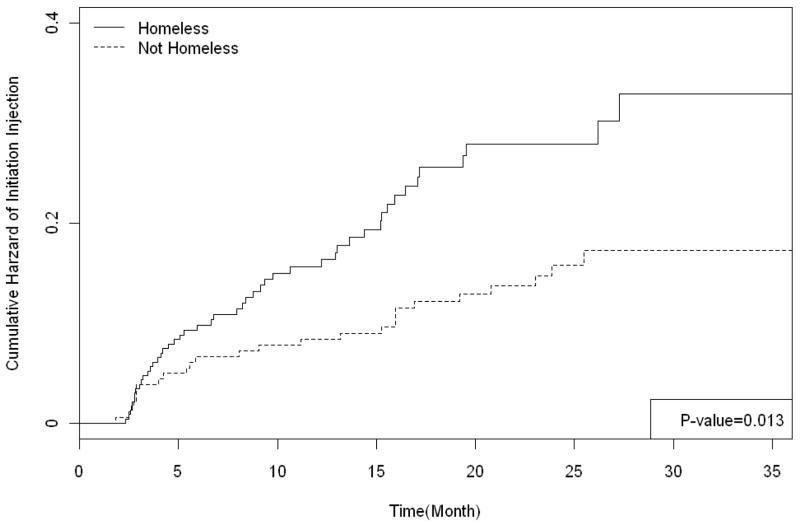
The cumulative hazard of injection initiation was calculated for youth who were and were not homeless during follow-up using Kaplan-Meier methods. Cox regression was then used to calculate unadjusted and adjusted relative hazards and 95% confidence intervals. To determine whether homelessness was independently associated with injection initiation while adjusting for the effect of crystal methamphetamine use, we fit a series of confounding models including homelessness and crystal methamphetamine use and all secondary variables. In a stepwise manner, we remove all secondary variables that did not change the coefficient for the effect of homelessness on injection initiation by at least 5%. Remaining variables were considered confounders and were included in the final multivariate analysis. All statistical analyses were performed using SAS software version 9.2.
Results
Of the 422 participants that met the inclusion criterion, 133 (32%) were female, and 148 (35%) reported non-injection methamphetamine use at baseline. Over study follow-up, 77 (18%) injection initiation events were observed. Baseline characteristic stratified by injection initiation are provided in Table 1. The Kaplan-Meier estimates of the cumulative hazard of injection initiation stratified by homelessness are shown in Figure 1. As shown, homeless participants demonstrate significantly higher risk of injection initiation (p = 0.013). The cumulative incidence of injection initiation among homeless participants reached 32.8% over study follow-up compared to 15.8% among those who were not homeless. Table 1 also shows the unadjusted and adjusted relative hazards of injection initiation. In multivariate Cox regression analyses, homelessness remains independently associated with time injection initiation (adjusted relative hazards =1.80, 95% Confidence Interval: 1.13–2.87), after adjusting for the effect of crystal methamphetamine use.
Table 1.
Baseline characteristics of street-involved youth who did and who did not initiate injection drug use and Univariate and Multivariate Cox regression analysis of factors associated with injection drug use initiation among street-involved youth in Vancouver (n = 422).
| Characteristic | Baseline characteristics | Univariate and Multivariate Cox regression analysis | ||||
|---|---|---|---|---|---|---|
| Injection initiation | Unadjusted HR† (95% CI) | p-value | Adjusted HR† (95% CI) | p-value | ||
| Yes (n=77) n (%) | No (n=345) n (%) | |||||
| Age | 21.3 (19.6, 22.5) | 21.6 (19.6, 23.3) | 0.96 (0.88 – 1.04) | 0.297 | ||
| Per year older | ||||||
| Caucasian | ||||||
| Yes | 54 (70.1) | 204 (59.1) | 1.50 (0.92 – 2.44) | 0.104 | ||
| No | 23 (29.9) | 141 (40.9) | ||||
| Male | ||||||
| Yes | 54 (70.1) | 235 (68.1) | 1.02 (0.63 – 1.67) | 0.920 | ||
| No | 23 (29.9) | 110 (31.9) | ||||
| Homeless | ||||||
| Yes | 57 (74.0) | 239 (69.3) | 1.80 (1.13 – 2.88) | 0.013 | 1.80 (1.13 – 2.87) | 0.014 |
| No | 20 (26.0) | 106 (30.7) | ||||
| Non-Injection Crystal Meth Use* | ||||||
| Yes | 41 (53.2) | 107 (31.0) | 1.83 (1.16 – 2.87) | 0.009 | 1.82 (1.16 – 2.85) | 0.010 |
| No | 36 (46.8) | 238 (69.0) | ||||
| Non-Injection Cocaine Use* | ||||||
| Yes | 31 (40.3) | 175 (50.7) | 0.99 (0.62 – 1.57) | 0.476 | ||
| No | 46 (59.7) | 170 (49.3) | ||||
| Crack Cocaine Smoking* | ||||||
| Yes | 52 (67.5) | 184 (53.3) | 1.38 (0.88 – 2.18) | 0.164 | ||
| No | 25 (32.5) | 161 (46.7) | ||||
| Non-Injection Heroin Use* | ||||||
| Yes | 18 (23.4%) | 48 (13.9) | 1.83 (1.06 – 3.14) | 0.029 | ||
| No | 59 (76.6%) | 297 (86.1) | ||||
| Marijuana Use* | ||||||
| Yes | 64 (83.1) | 316 (91.6) | 0.87 (0.47 – 1.61) | 0.653 | ||
| No | 13 (16.9) | 29 (8.4) | ||||
| Daily Alcohol Use* | ||||||
| Yes | 14 (18.2) | 59 (17.1) | 0.99 (0.55 – 1.80) | 0.982 | ||
| No | 63 (81.8) | 286 (82.9) | ||||
refers to the activities lagged to the pervious available follow-up
HR=Hazard Ratio
Figure 1.
Time to initiation of injection drug use among a cohort of street-involved youth in Vancouver stratified by homelessness (n=422).
Discussion
In our study, homelessness was independently associated with injection initiation after adjustment for various socio-demographic factors and substance use behaviors including crystal methamphetamine use. These findings suggest that homelessness may increase vulnerability to injection initiation.
In this study, age and gender were not significantly associated with injection initiation, whereas circumstances of injection initiation and factors associated with initiation have been found to vary by gender and age in earlier studies [5, 6]. Future studies should further examine these issues.
Overall our findings indicate that addressing the housing needs of street-involved youth may help prevent injection initiation. Given the documented difficulties that street-involved youth face obtaining housing [1], increasing the supply of youth focused housing is one step. However, it is critical that housing models be closely monitored and evaluated [7, 8]. Furthermore, identifying and addressing risk factors for homelessness among street-involved youth should be another priority. High intensity drug use, mental illness and inability to access mental health and addiction treatment have been linked to youth homelessness in past studies and intervention studies require further attention [9, 10]. It is also important to highlight that reducing youth homelessness in isolation will not address the complex determinants of injection initiation and evidence-based approaches are urgently required.
This study has several limitations. First, our sample is not a random sample and thus may not be generalizable. Second, our behavioral variables are based on self-report, and therefore may be subject to recall bias and socially desirable reporting. Third, as with any non-randomized study, the relationship between homelessness and injection initiation could be influenced by confounders not measured by the study instrument.
In summary, our findings highlight that homelessness is a key risk factor for injection initiation even after adjusting for other competing factors including crystal methamphetamine use. These findings suggest that supportive housing interventions in combination with other youth specific programs may help prevent injection initiation among this high-risk population.
Acknowledgments
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. We would specifically like to thank Deborah Graham, Peter Vann, Caitlin Johnston, Steve Kain, and Calvin Lai for their research and administrative assistance. The study was supported by the US National Institutes of Health (R01DA028532) and the Canadian Institutes of Health Research (MOP–102742). Kora DeBeck is supported by the Canadian Institutes of Health Research. Thomas Kerr is supported by the Michael Smith Foundation for Health Research. Julio Montaner has received an Avant-Garde award (DP1DA026182) from the National Institute of Drug Abuse, US National Institutes of Health. Funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr Evan Wood.
Footnotes
Competing Interests:
CF, KD, TK, SM, and EW have no conflicts of interest to declare. JM has received grants from, served as an ad hoc advisor to, or spoke at various events sponsored by; Abbott, Argos Therapeutics, Bioject Inc, Boehringer Ingelheim, BMS, Gilead Sciences, GlaxoSmithKline, Hoffmann-La Roche, Janssen-Ortho, Merck Frosst, Pfizer, Schering, Serono Inc, Thera Technologies, Tibotec, Trimeris.
Implications and Contribution:
This longitudinal study investigates the association between homelessness and time to first injection drug use among a cohort of street-involved youth. Findings indicate that homelessness is independently associated with injection initiation, which suggests that addressing the housing needs of street-involved youth may help prevent injection initiation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Krüsi A, Fast D, Small W, Wood E, Kerr T. Social and structural barriers to housing among street-involved youth who use illicit drugs. Health Soc Care Community. 2010;18(3):282–288. doi: 10.1111/j.1365-2524.2009.00901.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kulik DM, Gaetz S, Crowe C, Ford-Jones E. Homeless youth’s overwhelming health burden: Are view of the literature. Paediatr Child Health. 2011;16(6):43–47. doi: 10.1093/pch/16.6.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lloyd-Smith E, Kerr T, Zhang R, Montaner JSG, Wood E. High prevalence of syringe sharing among street involved youth. Addict Res Theory. 2008;16(4):353–358. [Google Scholar]
- 4.Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: The ARYS study. Harm Reduct J. 2006;3(18) doi: 10.1186/1477-7517-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roy é, Haley N, Leclerc P, Cédras L, Blais L, Boivin JF. Drug injection among street youths in Montréal: predictors of initiation. J Adolesc Health. 2003;80(1):92–105. doi: 10.1093/jurban/jtg092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doherty MC, Garfein RS, Monterroso E, Latkin C, Vlahov D. Gender differences in the initiation of injection drug use among young adults. J Adolesc Health. 2000;77(3):396–414. doi: 10.1007/BF02386749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briggs D, Rhodes T, Marks D, Kimber J, Holloway G, Jones S. Injecting drug use and unstable housing: Scope for structural interventions in harm reduction. Drugs (Abingdon Engl) 2009;16:436–450. [Google Scholar]
- 8.Wadd S, Hutchinson S, Taylor A, Ahmed S, Goldberg DJ. High-risk injecting behaviour in hostel accommodation for the homeless in Glasgow 2001–2002: A study combining quantitative and qualitative methodology. J Subst Use. 2006;11(5):333–341. [Google Scholar]
- 9.Rachlis B, Wood E, Zhang R, Montaner JS, Kerr T. High rates of homelessness among a cohort of street-involved youth. Health Place. 2009;15(1):10–17. doi: 10.1016/j.healthplace.2008.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hadland SE, Kerr T, Li K, Montaner JS, Wood E. Access to drug and alcohol treatment among a cohort of street-involved youth. Drug Alcohol Depend. 2009;101(1–2):1–7. doi: 10.1016/j.drugalcdep.2008.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]