Abstract
Increased visceral adiposity is a risk factor for metabolic disorders such as dyslipidemia, hypertension, insulin resistance and type 2 diabetes, whereas peripheral (subcutaneous) obesity is not. Though the specific mechanisms which contribute to these adipose depot differences are unknown, visceral fat accumulation is proposed to result in metabolic dysregulation because of increased effluent, e.g., fatty acids and/or adipokines/cytokines, to the liver via the hepatic portal vein. Pathological significance of visceral fat accumulation is also attributed to adipose depot/adipocyte-specific characteristics, specifically differences in structural, physiologic and metabolic characteristics compared with subcutaneous fat. Fat manipulations, such as removal or transplantation, have been utilized to identify location dependent or independent factors that play a role in metabolic dysregulation. Obesity-induced alterations in adipose tissue function/intrinsic characteristics, but not mass, appear to be responsible for obesity-induced metabolic dysregulation, thus “quality” is more important than “quantity.” This review summarizes the implications of obesity-induced metabolic dysfunction as it relates to anatomic site and inherent adipocyte characteristics.
Keywords: lipectomy, transplantation, portal vein, visceral obesity, adipose tissue, liver
Introduction
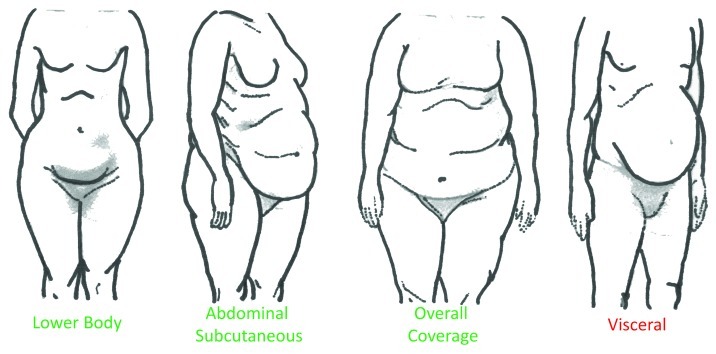
The distribution of accumulating adipose tissue varies among individuals but can generally be classified as lower body, abdominal subcutaneous (underneath the skin), overall coverage or visceral fat (located in the abdominal cavity among organs) (Fig. 1). Obesity-related adverse health consequences, however, are less related to total body fat deposition, and more strongly associated with a precise fat distribution. More specifically, lower body1 and abdominal subcutaneous2-4 fat accumulation are associated with reduced metabolic perturbations whereas upper body fat distribution and increased visceral fat,5-8 is associated with metabolic dysregulation. Metabolic disorders associated with upper body/visceral obesity include dyslipidemia,9 hypertension,10,11 insulin resistance and type 2 diabetes.12,13 Though the mechanisms for this connection remain to be elucidated the negative consequences of visceral fat are commonly attributed to fat mass, location and/or adipocyte specific physiology.
Figure 1. Description of body fat distribution in humans. Lower body: fat storage around the buttocks, hips and thighs. Abdominal subcutaneous: subcutaneous fat storage around the stomach and chest. Overall coverage: fat accumulation in the arms, breast, thighs, buttocks, lower back and breast. Visceral: intra-abdominal fat deposition among organs such as the intestines, stomach, liver and pancreas. Fat distributed within the visceral cavity is highly associated with obesity-related health consequences whereas other fat distribution is not.
Adipose Tissue Location
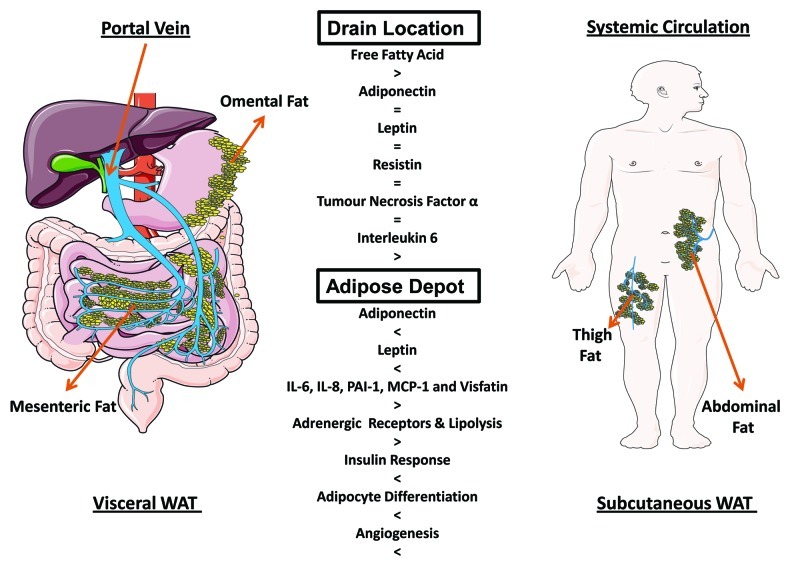
Approximately 85% of total adipose tissue mass, in lean or obese humans, is subcutaneous while the remaining 15% constitutes intra-abdominal fat, including both visceral and retroperitoneal adipose depots.14 Visceral fat, encompassing mesenteric and omental adipose depots (Fig. 1), only constitutes ~10% of total body fat,14 yet has the highest associated risk for metabolic dysregulation. Visceral obesity is presumed to predispose individuals to adverse health consequences based on its anatomical site and venous drainage to the liver; i.e., insulin-sensitive hepatocytes are directly exposed to the metabolites and secretory products released by visceral adipocytes into the portal vein.15-17 Because substrate delivery is a major determinant of both hepatic gluconeogenesis and very low-density lipoprotein (VLDL) synthesis,6 an increased volume of visceral fat, and subsequent release of fatty acids, glycerol and lactate in addition to numerous adipokines and pro-inflammatory cytokines directly into the portal vein would be expected to have a major influence on these hepatic processes.
Chronic exposure of the liver to elevated free fatty acids promotes liver gluconeogenesis,17,18 reduces enzymes involved in fatty acid oxidation and increases fat storage and synthesis in the liver19-21 and insulin resistance.21 Elevated fatty acid flux to the liver also decreases hepatic insulin binding and degradation.22 This results in systemic hyperinsulinemia23 and additional attenuation of insulin suppression of hepatic glucose production (i.e., hepatic insulin resistance).24 In addition, fatty acids facilitate hepatic glucose production by providing a continuous source of energy and substrate.24 Overall, an excess lipid load to the liver can result in ectopic lipid accumulation and development or exacerbation of insulin resistance.23,25 The insulin resistance associated with these processes in turn amplifies the metabolic effects of obesity by increasing dyslipidemia.26
Though visceral obesity is associated with an increase in post-prandial27 and post-absorptive28 systemic fatty acid concentration, and portal vein fatty acid concentration appears to increase proportionally with visceral fat accumulation29 (Fig. 2), some suggest visceral obesity is not the principal initiator of metabolic dysfunction. Alternative observations propose obesity-induced pathophysiology of the liver may be due to the limited ability of subcutaneous adipose tissue to store excess energy. In obese humans it is estimated that the subcutaneous adipose depot supplies the majority of free fatty acids in the portal29 and systemic circulation.29,30 Indeed, some estimate that only 5–20% of the portal vein fatty acid concentration originates from visceral adipose tissue.29 While factors other than visceral fat are likely involved in obesity-related metabolic disturbances, these data imply that the strong association of visceral fat and metabolic dysfunction involves multiple secreted factors.
Figure 2. Differences between visceral and subcutaneous adipose tissue depots. Drain location: the visceral depot (left) releases products into the portal vein, while the subcutaneous depot (right) releases products into the systemic circulation. In obesity, portal vein effluent to the liver contains higher concentrations of free fatty acids and interleukin-6 compared with the systemic circulation. Adipose depot: Visceral and subcutaneous fat are characterized by inherent differences. When compared with subcutaneous fat, visceral fat is characterized by reduced adiponectin and leptin, increased inflammatory adipo/cytokines, enhanced lipolysis, a reduced response to insulin and reduced differentiation and angiogenesis.
Adipokine/cytokine effluent to the hepatic portal vein is also proposed to play a role in the adverse health consequences resulting from visceral adipose tissue expansion. Common adipocytokines proposed to contribute to insulin resistance of the liver include adiponectin, leptin, resistin, tumor necrosis factor (TNF)-α and interleukin (IL)-6 (Fig. 2). Adiponectin is a modulator of numerous metabolic processes such as glucose regulation and fatty acid metabolism. It is considered an anti-diabetic, -atherogenic and -inflammatory peptide that is highly correlated with systemic insulin sensitivity.31-33 Unlike the majority of adipokines, adiponectin secretion and receptor expression within the liver are inversely associated with increasing adipose tissue mass and non-alcoholic steatohepatitis.34,35
However, obesity-induced alterations in portal vein adiponectin do not appear to be different than arterial adiponectin as a marker of hepatic metabolic dysregulation.36 Although both leptin and resistin can induce insulin resistance, these effects do not appear to be due to differences in portal vein and systemic concentration.37,38
Another consequence of expanding adipose tissue mass is increased production of proinflammatory molecules released from adipocytes and/or infiltrating macrophages.39 Obesity is characterized by elevations in several proinflammatory cytokines, including TNF-α and IL-6, and these cytokines have been linked to impairments in insulin action in liver, muscle and adipose tissue.37,40 Though systemic blood concentrations of TNF-α are increased in obesity, portal vein concentrations are not different than those measured in the peripheral artery.38 Some studies suggest, that TNF-α in blood of humans, unlike rodents,41 is not secreted at measurable levels.42,43 Instead of inducing alterations systemically, TNF-α modulates insulin sensitivity locally42 within adipocytes and stimulates expression of other adipo/cytokines like leptin and IL-6 and also increases the release of fatty acids.44 Though portal and systemic TNF-α concentration do not appear to be different, when detectable, TNF-α induced alterations in local adipose depot factors may contribute to portal vein increases in other adipo/cytokines. Alternatively, IL-6 in obese humans is ~50% higher in the portal vein than in the peripheral artery,38 thus is a potential mechanistic link between adipose depot anatomical site and obesity-induced adverse health consequences. Overall, further research is needed to clarify the direct effects of visceral fat pad expansion on hepatic and extra-hepatic metabolic regulation and the extent to which these effects are mediated by molecules secreted into the portal vein.
Inherent Characteristics of Adipose Tissue
Adipose tissue depots display distinct structural, physiologic and metabolic characteristics. Thus, it has been proposed that distinct biologic properties of native adipocytes contribute to the association between visceral fat and metabolic dysregulation. Since adipose tissue has been recognized as an endocrine organ that secretes numerous proteins that modify metabolism, much of the research has focused on depot-specific differences in adipo/cytokine release. Because the production of most adipo/cytokines is increased in the adipose tissue of obese individuals,45 it has been proposed that differential protein secretion accounts for the divergent metabolic consequences of visceral vs. subcutaneous fat. Obesity increases many adipo/cytokines, but only a few have been demonstrated to be consistently different between adipose depots (Fig. 2). For example, leptin and adiponectin gene expression46-48 and release49,50 appear to be higher in subcutaneous adipose tissue compared with visceral. Conversely, cytokine expression, specifically IL-6, IL-8, PAI-1, MCP-1 and Visfatin, appears to be greater in visceral fat compared with subcutaneous fat (for a review see ref. 51).
Metabolic characteristics also differ between visceral and subcutaneous adipose tissue depots (Fig. 2). For example, human studies have demonstrated a higher turnover of triglyceride in the upper body compartment compared with lower body fat.52 These differences are presumably due to higher triglyceride/fatty acid turnover in visceral adipocytes compared with subcutaneous fat due, at least in part, to a combination of increased lipolysis and decreased sensitivity to the antilipolytic effects of insulin.53 Consistent with this observation are studies that have examined the metabolic properties of isolated visceral adipocytes. In comparison with subcutaneous adipocytes, adipocytes isolated from visceral fat were characterized by higher rates of catecholamine-induced lipolysis,54,55 increased expression of β-1, -2 and -3 adrenergic receptors,56,57 and reduced responsiveness to the cAMP-lowering effects of α-adrenergic agonists.58 Consequently, although obesity appears to be associated with reduced expression of hormone-sensitive lipase and increased expression of lipoprotein lipase and fatty acid synthase, these proteins are all higher in visceral adipose tissue when compared with subcutaneous.59-61 In addition, in obese humans there is a direct inverse correlation between the antilipolytic effect of insulin and the amount of visceral adipose tissue, but not with subcutaneous adipose tissue or waist-hip-ratio (WHR),62 suggesting that antilipolytic signaling mechanisms are less active in visceral fat cells. In humans local infusion of insulin into the visceral region suppresses lipolysis, but only at a higher concentration than is effective in non-visceral adipose tissue.63 In vitro studies confirm that visceral adipocytes are less responsive to the antilipolytic effect of insulin than are subcutaneous adipocytes,64,65 visceral fat has a lower binding affinity for insulin66 and reduced insulin receptor substrate (IRS)-1 protein expression compared with subcutaneous adipocytes.65
Other intrinsic and extrinsic differences between adipose tissue depots may also modify gene expression and metabolism in adipocytes. Some proposed intrinsic influences include mean adipocyte size, adipocyte expansion capacity and cell heterogeneity. Increased visceral adipocyte size is linked to adipose tissue dysfunction, inflammation, adipocyte apoptosis, systemic lipotoxicity and subsequent decline in metabolic parameters67-69 whereas an increase in adipocyte size in subcutaneous adipose tissue is not.70 Visceral fat is also characterized by a reduced capacity for differentiation71 and increased susceptibility to apoptotic stimuli69 compared with subcutaneous fat. Other factors currently receiving attention include variations in connective tissue, macrophages, immune cells and stromovascular cells.72,73 Extrinsic factors which may play a role in the metabolic complications associated with increased visceral fat mass include angiogenic capacity and innervation.74,75 Overall, current research demonstrates that visceral adipose tissue is morphologically and functionally different than subcutaneous. The precise mechanisms responsible for adverse health consequences of expanding visceral fat, however, still remain unclear.
Identifying the Link between Visceral Fat and Deleterious Metabolic Outcomes through Fat Manipulation
Lipectomy (fat removal) studies
Selective reduction in intra-abdominal adipose tissue improves metabolic profile. More specifically, intra-abdominal lipectomy reverses insulin resistance and glucose intolerance in obese, aged and young rodents.76-81 Though controversial in humans,82,83 omental fat removal improves insulin action,84,85 whereas removal of non-visceral fat has no effect.86 Conflicting results among human omentectomy studies likely occur because outcome measurements are not consistent or sensitive enough to detect metabolic improvements. In addition, if omentectomy is combined with gastric bypass, the accelerated weight loss due to bypass could mask the beneficial effects of omental fat removal. While several studies have investigated lipectomy-induced alterations in insulin action, glucose tolerance and even adipokines, mechanisms by which these improvements occur remain unclear. Research suggests, however, that alterations in free fatty acids and adipo/cytokines may play prominent roles in fat removal-induced improvements in insulin signaling and glucose homeostasis.76-81
There is another, often forgotten or overlooked, consequence of lipectomy. In both humans and rodents there are fat removal-induced compensatory increases in non-excised adipose tissue depots. There is evidence that human liposuction increases body fat in non-excised areas87,88 and there is a preponderance of evidence that lipectomy induces compensatory increases in rodents.89-97 Several studies have found that compensatory increases in fat mass result from both larger mean fat cell size and increased adipocyte number.90,98,99 Hence, enhanced insulin sensitivity following fat removal may not be dictated by fat removal alone and may be based in part on compensatory increases of non-excised fat depots. Further, lipectomy results in decreased norepinephrine turnover in non-excised adipose tissue pads,100 implying that decreased sympathetic tone may contribute to lipectomy-induced compensatory increases of fat mass by means of promoting lipid accretion through decreased basal lipolysis. Independent studies indicate that a reduction of norepinephrine release to adipose tissues results in increased fat accumulation in adipocytes.98,101 Sensory innervation is hypothesized to initiate compensatory lipid increases via informing the brain of alterations in lipid reserves and consequently adjusting lipid storage (for a review see ref. 102).
Previous lipectomy studies in rodents are somewhat limited in that there is ambiguity as to whether excised fat was in fact attached to the portal drainage to the liver. As an example, epididymal white adipose tissue (EWAT) is in an intra-abdominal location in rats and mice that allows for fast and simple removal, thus many researchers have considered epididymal fat to be a visceral depot. However, because of its drainage into the systemic circulation, EWAT should not be considered a visceral depot.103 In addition, EWAT has no human equivalent, making it more appropriate to conduct lipectomy studies that manipulate actual visceral adipose tissue such as mesenteric and omental WAT (MWAT and OWAT).
Transplantation studies
Recent studies have begun to investigate metabolic alterations following transplantation of adipose tissue. Investigation of morphological and physiological changes in the transplanted adipocytes between lean and genetically obese mice revealed that abnormalities of obese-derived adipose tissue are due to extrinsic and not intrinsic factors.104 That report, however, was limited in that the actual effects of adipose tissue transplantation on overall physiology were negated due to small tissue-sample size. Additional studies later demonstrated that physiological changes can be revealed after transplantation using larger amounts of adipose tissue. The ability of larger amounts of adipose tissue to survive after removal and insertion to another site has been repeatedly demonstrated in humans by reconstructive and plastic surgeries termed autologous fat transplantation.105 Only recently have the effects of added body fat been scrutinized.106 Successful transplantation of physiologically meaningful amounts of subcutaneous adipose tissue in mice and Siberian hamsters is associated with revascularization and normal appearance both macro- and microscopically.107-110 Fat transplantation has not been observed to lead to compensatory decreases in total body fat suggesting that body fat regulation is a system biased toward rectifying decreases but not increases in lipid storage capacity.109,110
A seminal study utilizing adipose tissue transplantation to define the role adipose tissue physiology plays in insulin resistance and type 2 diabetes used a paradoxical approach via a lipoatrophic (low fat mass) recipient. This study demonstrated that the addition of normal subcutaneous adipose tissue to lipoatrophic mice reversed hyperphagia, insulin resistance, hepatic steatosis and hypoleptinemia,108 suggesting that lack of adipose tissue caused the metabolic abnormalities. The mechanisms leading to these improvements, however, are unknown but may involve enhanced free fatty acid uptake by adipocytes and muscle and increased circulating leptin.
The connection among increased visceral fat mass, insulin resistance and type 2 diabetes is well documented. However, the contribution of increased intra-abdominal fat mass vs. obesity-induced functional modifications in adipose tissue metabolism is currently being defined. Transplantation of adipose tissue from lean donor rodents to the intra-abdominal cavity of a lean recipient, thus mimicking visceral obesity, is a standard model used to characterize these differences. Although human data predicts that increased visceral fat mass is a fundamental problem in obesity-related metabolic disorders, data from rodent studies support an alternative view. Intra-abdominal transplantation of adipose tissue of non-visceral origin in most cases has beneficial effects on metabolism.111-113 In addition, implantation of specific fat depots produces cell-autonomous distinctive changes in glucose tolerance and insulin sensitivity.111-113 Mechanisms for these beneficial improvements are uncertain but do not appear to involve changes in inflammatory cytokines, adipokines (e.g., adiponectin, leptin or resistin) or free fatty acids.111,113 Only one of the previous studies placed the transplanted tissue in a manner that allowed for maximal revascularization proximal to the portal vein. The others sutured transplants to the visceral side of the peritoneum on the anterior abdominal wall, with a high probability that revascularization would occur through the abdominal wall and thus the systemic circulation.111-113 All previous studies drew blood from the systemic circulation. Therefore, future studies should utilize approaches that result in transplanted tissue that is vascularized by vessels that deliver blood directly into the hepatic portal drainage and blood sampling from both the portal vein and systemic circulation. In support of such an approach, recent studies have demonstrated that transplantation of non-visceral (e.g., subcutaneous) fat into the visceral cavity improves glucose tolerance and enhances hepatic insulin sensitivity, in part, via decreased portal vein lipid concentrations and consequently reduced liver fat storage.114-116 However, at least one study, using similar techniques, observed impaired glucose tolerance and hepatic insulin resistance, implicating IL-6 as the mechanism for dysregulation.117 Overall, these data suggest that visceral fat mass per se is not the mechanism linking visceral fat to obesity-related metabolic disorders. The link between visceral fat and insulin resistance likely involves inherent differences in the metabolic behavior of visceral fat. This suggests that the “quality” of fat plays a larger role than the “quantity” in the development of obesity-related metabolic diseases.
Conclusions
Increased visceral adiposity is an associated risk factor of metabolic disorders; research also suggests it is the origin. Metabolic improvement following decreases in visceral adipose tissue mass, but not peripheral (subcutaneous) demonstrates a direct relationship between central obesity and metabolic dysregulation. The connection, however, cannot exclusively be attributed to location providing visceral adipose depot adipocytes structure, physiologic and metabolic characteristics are different than subcutaneous adipose depot. Fat addition mimicking visceral obesity, via transplantation, does not impair metabolic function, but rather improves it, thus implies specific obesity-induced dysfunction of visceral adipocytes. Indeed, intrinsic properties of adipocytes, regardless of location, are responsible for metabolic dysregulation. In accord, obesity-induced alterations in adipose tissue function rather than mass are responsible for the adverse metabolic consequences of obesity. Hence, increased intra-abdominal fat mass is not necessary for the development of insulin resistance. In addition, to completely understand how adipocyte intrinsic characteristics regulate obesity-induced metabolic dysregulation the role of extrinsic factors (i.e., hormones, growth factors, vasculature, sympathetic/sensory innervation and cross-talk with associated organs) should be investigated as well. Alterations in the extrinsic environment following fat removal or transplantation have yet to be investigated, though fat manipulation causes great changes between adipocytes, vasculature and nerves. Overall, identification of regionally secreted or extrinsic factors may provide targets for treatments to prevent or reverse co-morbidities associated with obesity.
Acknowledgments
The work in this area was supported by NIH grant K01 DK087816. Certain components of Figure 2 were based on medical art templates provided by Servier (www.servier.com).
Footnotes
Previously published online: www.landesbioscience.com/journals/adipocyte/article/21756
References
- 1.Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Yudkin JS, et al. Hoorn study Trunk fat and leg fat have independent and opposite associations with fasting and postload glucose levels: the Hoorn study. Diabetes Care. 2004;27:372–7. doi: 10.2337/diacare.27.2.372. [DOI] [PubMed] [Google Scholar]
- 2.Cefalu WT, Wang ZQ, Werbel S, Bell-Farrow A, Crouse JR, 3rd, Hinson WH, et al. Contribution of visceral fat mass to the insulin resistance of aging. Metabolism. 1995;44:954–9. doi: 10.1016/0026-0495(95)90251-1. [DOI] [PubMed] [Google Scholar]
- 3.Seidell JC, Björntorp P, Sjöström L, Kvist H, Sannerstedt R. Visceral fat accumulation in men is positively associated with insulin, glucose, and C-peptide levels, but negatively with testosterone levels. Metabolism. 1990;39:897–901. doi: 10.1016/0026-0495(90)90297-P. [DOI] [PubMed] [Google Scholar]
- 4.Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006;14:336–41. doi: 10.1038/oby.2006.43. [DOI] [PubMed] [Google Scholar]
- 5.Björntorp P. Metabolic implications of body fat distribution. Diabetes Care. 1991;14:1132–43. doi: 10.2337/diacare.14.12.1132. [DOI] [PubMed] [Google Scholar]
- 6.Kissebah AH, Krakower GR. Regional adiposity and morbidity. Physiol Rev. 1994;74:761–811. doi: 10.1152/physrev.1994.74.4.761. [DOI] [PubMed] [Google Scholar]
- 7.Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. 1956;4:20–34. doi: 10.1093/ajcn/4.1.20. [DOI] [PubMed] [Google Scholar]
- 8.Björntorp P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis. 1990;10:493–6. doi: 10.1161/01.ATV.10.4.493. [DOI] [PubMed] [Google Scholar]
- 9.Kissebah AH, Alfarsi S, Adams PW, Wynn V. Role of insulin resistance in adipose tissue and liver in the pathogenesis of endogenous hypertriglyceridaemia in man. Diabetologia. 1976;12:563–71. doi: 10.1007/BF01220632. [DOI] [PubMed] [Google Scholar]
- 10.Cassano PA, Segal MR, Vokonas PS, Weiss ST. Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol. 1990;1:33–48. doi: 10.1016/1047-2797(90)90017-M. [DOI] [PubMed] [Google Scholar]
- 11.Seidell JC, Cigolini M, Deslypere JP, Charzewska J, Ellsinger BM, Cruz A. Body fat distribution in relation to serum lipids and blood pressure in 38-year-old European men: the European fat distribution study. Atherosclerosis. 1991;86:251–60. doi: 10.1016/0021-9150(91)90221-N. [DOI] [PubMed] [Google Scholar]
- 12.Carey VJ, Walters EE, Colditz GA, Solomon CG, Willett WC, Rosner BA, et al. Body fat distribution and risk of non-insulin-dependent diabetes mellitus in women. The Nurses’ Health Study. Am J Epidemiol. 1997;145:614–9. doi: 10.1093/oxfordjournals.aje.a009158. [DOI] [PubMed] [Google Scholar]
- 13.Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17:961–9. doi: 10.2337/diacare.17.9.961. [DOI] [PubMed] [Google Scholar]
- 14.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Association for Weight Management and Obesity Prevention. NAASO. Obesity Society. American Society for Nutrition. American Diabetes Association Waist circumference and cardiometabolic risk: a consensus statement from shaping America’s health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Diabetes Care. 2007;30:1647–52. doi: 10.2337/dc07-9921. [DOI] [PubMed] [Google Scholar]
- 15.Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science. 1996;271:665–8. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- 16.Bergman RN. Non-esterified fatty acids and the liver: why is insulin secreted into the portal vein? Diabetologia. 2000;43:946–52. doi: 10.1007/s001250051474. [DOI] [PubMed] [Google Scholar]
- 17.Williamson JR, Kreisberg RA, Felts PW. Mechanism for the stimulation of gluconeogenesis by fatty acids in perfused rat liver. Proc Natl Acad Sci U S A. 1966;56:247–54. doi: 10.1073/pnas.56.1.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson JR. Mechanism for the stimulation in vivo of hepatic gluconeogenesis by glucagon. Biochem J. 1966;101:11C–4C. doi: 10.1042/bj1010011c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clarke SD. Polyunsaturated fatty acid regulation of gene transcription: a mechanism to improve energy balance and insulin resistance. Br J Nutr. 2000;83(Suppl 1):S59–66. doi: 10.1017/S0007114500000969. [DOI] [PubMed] [Google Scholar]
- 20.Xu J, Nakamura MT, Cho HP, Clarke SD. Sterol regulatory element binding protein-1 expression is suppressed by dietary polyunsaturated fatty acids. A mechanism for the coordinate suppression of lipogenic genes by polyunsaturated fats. J Biol Chem. 1999;274:23577–83. doi: 10.1074/jbc.274.33.23577. [DOI] [PubMed] [Google Scholar]
- 21.Oakes ND, Cooney GJ, Camilleri S, Chisholm DJ, Kraegen EW. Mechanisms of liver and muscle insulin resistance induced by chronic high-fat feeding. Diabetes. 1997;46:1768–74. doi: 10.2337/diabetes.46.11.1768. [DOI] [PubMed] [Google Scholar]
- 22.Svedberg J, Björntorp P, Smith U, Lönnroth P. Free-fatty acid inhibition of insulin binding, degradation, and action in isolated rat hepatocytes. Diabetes. 1990;39:570–4. doi: 10.2337/diabetes.39.5.570. [DOI] [PubMed] [Google Scholar]
- 23.Dobbins RL, Szczepaniak LS, Bentley B, Esser V, Myhill J, McGarry JD. Prolonged inhibition of muscle carnitine palmitoyltransferase-1 promotes intramyocellular lipid accumulation and insulin resistance in rats. Diabetes. 2001;50:123–30. doi: 10.2337/diabetes.50.1.123. [DOI] [PubMed] [Google Scholar]
- 24.Boden G. Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes. 1997;46:3–10. doi: 10.2337/diabetes.46.1.3. [DOI] [PubMed] [Google Scholar]
- 25.Heilbronn L, Smith SR, Ravussin E. Failure of fat cell proliferation, mitochondrial function and fat oxidation results in ectopic fat storage, insulin resistance and type II diabetes mellitus. Int J Obes Relat Metab Disord. 2004;28(Suppl 4):S12–21. doi: 10.1038/sj.ijo.0802853. [DOI] [PubMed] [Google Scholar]
- 26.Voshol PJ, Rensen PC, van Dijk KW, Romijn JA, Havekes LM. Effect of plasma triglyceride metabolism on lipid storage in adipose tissue: studies using genetically engineered mouse models. Biochim Biophys Acta. 2009;1791:479–85. doi: 10.1016/j.bbalip.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Roust LR, Jensen MD. Postprandial free fatty acid kinetics are abnormal in upper body obesity. Diabetes. 1993;42:1567–73. doi: 10.2337/diabetes.42.11.1567. [DOI] [PubMed] [Google Scholar]
- 28.Jensen MD, Haymond MW, Rizza RA, Cryer PE, Miles JM. Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest. 1989;83:1168–73. doi: 10.1172/JCI113997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nielsen S, Guo Z, Johnson CM, Hensrud DD, Jensen MD. Splanchnic lipolysis in human obesity. J Clin Invest. 2004;113:1582–8. doi: 10.1172/JCI21047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo Z, Hensrud DD, Johnson CM, Jensen MD. Regional postprandial fatty acid metabolism in different obesity phenotypes. Diabetes. 1999;48:1586–92. doi: 10.2337/diabetes.48.8.1586. [DOI] [PubMed] [Google Scholar]
- 31.Laakso M. Cardiovascular disease in type 2 diabetes: challenge for treatment and prevention. J Intern Med. 2001;249:225–35. doi: 10.1046/j.1365-2796.2001.00789.x. [DOI] [PubMed] [Google Scholar]
- 32.Funahashi T, Nakamura T, Shimomura I, Maeda K, Kuriyama H, Takahashi M, et al. Role of adipocytokines on the pathogenesis of atherosclerosis in visceral obesity. Intern Med. 1999;38:202–6. doi: 10.2169/internalmedicine.38.202. [DOI] [PubMed] [Google Scholar]
- 33.Yokota T, Oritani K, Takahashi I, Ishikawa J, Matsuyama A, Ouchi N, et al. Adiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophages. Blood. 2000;96:1723–32. [PubMed] [Google Scholar]
- 34.Kaser S, Moschen A, Cayon A, Kaser A, Crespo J, Pons-Romero F, et al. Adiponectin and its receptors in non-alcoholic steatohepatitis. Gut. 2005;54:117–21. doi: 10.1136/gut.2003.037010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lihn AS, Bruun JM, He G, Pedersen SB, Jensen PF, Richelsen B. Lower expression of adiponectin mRNA in visceral adipose tissue in lean and obese subjects. Mol Cell Endocrinol. 2004;219:9–15. doi: 10.1016/j.mce.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Magkos F, Fabbrini E, Patterson BW, Eagon JC, Klein S. Portal vein and systemic adiponectin concentrations are closely linked with hepatic glucose and lipoprotein kinetics in extremely obese subjects. Metabolism. 2011;60:1641–8. doi: 10.1016/j.metabol.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferńndez-Veledo S, Nieto-Vazquez I, Vila-Bedmar R, Garcia-Guerra L, Alonso-Chamorro M, Lorenzo M. Molecular mechanisms involved in obesity-associated insulin resistance: therapeutical approach. Arch Physiol Biochem. 2009;115:227–39. doi: 10.1080/13813450903164330. [DOI] [PubMed] [Google Scholar]
- 38.Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S. Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes. 2007;56:1010–3. doi: 10.2337/db06-1656. [DOI] [PubMed] [Google Scholar]
- 39.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW., Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoene M, Weigert C. The role of interleukin-6 in insulin resistance, body fat distribution and energy balance. Obes Rev. 2008;9:20–9. doi: 10.1111/j.1467-789X.2007.00410.x. [DOI] [PubMed] [Google Scholar]
- 41.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 42.Sopasakis VR, Nagaev I, Smith U. Cytokine release from adipose tissue of nonobese individuals. Int J Obes (Lond) 2005;29:1144–7. doi: 10.1038/sj.ijo.0803002. [DOI] [PubMed] [Google Scholar]
- 43.Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab. 1997;82:4196–200. doi: 10.1210/jc.82.12.4196. [DOI] [PubMed] [Google Scholar]
- 44.Sethi JK, Hotamisligil GS. The role of TNF alpha in adipocyte metabolism. Semin Cell Dev Biol. 1999;10:19–29. doi: 10.1006/scdb.1998.0273. [DOI] [PubMed] [Google Scholar]
- 45.Mohamed-Ali V, Pinkney JH, Coppack SW. Adipose tissue as an endocrine and paracrine organ. Int J Obes Relat Metab Disord. 1998;22:1145–58. doi: 10.1038/sj.ijo.0800770. [DOI] [PubMed] [Google Scholar]
- 46.Montague CT, Prins JB, Sanders L, Digby JE, O’Rahilly S. Depot- and sex-specific differences in human leptin mRNA expression: implications for the control of regional fat distribution. Diabetes. 1997;46:342–7. doi: 10.2337/diabetes.46.3.342. [DOI] [PubMed] [Google Scholar]
- 47.Samaras K, Botelho NK, Chisholm DJ, Lord RV. Subcutaneous and visceral adipose tissue gene expression of serum adipokines that predict type 2 diabetes. Obesity (Silver Spring) 2010;18:884–9. doi: 10.1038/oby.2009.443. [DOI] [PubMed] [Google Scholar]
- 48.Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology. 2004;145:2273–82. doi: 10.1210/en.2003-1336. [DOI] [PubMed] [Google Scholar]
- 49.Van Harmelen V, Reynisdottir S, Eriksson P, Thörne A, Hoffstedt J, Lönnqvist F, et al. Leptin secretion from subcutaneous and visceral adipose tissue in women. Diabetes. 1998;47:913–7. doi: 10.2337/diabetes.47.6.913. [DOI] [PubMed] [Google Scholar]
- 50.Baglioni S, Cantini G, Poli G, Francalanci M, Squecco R, Di Franco A, et al. Functional differences in visceral and subcutaneous fat pads originate from differences in the adipose stem cell. PLoS One. 2012;7:e36569. doi: 10.1371/journal.pone.0036569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mirza MS. Obesity, Visceral Fat, and NAFLD: Querying the Role of Adipokines in the Progression of Nonalcoholic Fatty Liver Disease. ISRN Gastroenterol. 2011;2011:592404. doi: 10.5402/2011/592404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jensen MD. Health consequences of fat distribution. Horm Res. 1997;48(Suppl 5):88–92. doi: 10.1159/000191335. [DOI] [PubMed] [Google Scholar]
- 53.Ostman J, Arner P, Engfeldt P, Kager L. Regional differences in the control of lipolysis in human adipose tissue. Metabolism. 1979;28:1198–205. doi: 10.1016/0026-0495(79)90131-8. [DOI] [PubMed] [Google Scholar]
- 54.Rebuffé-Scrive M, Andersson B, Olbe L, Björntorp P. Metabolism of adipose tissue in intraabdominal depots of nonobese men and women. Metabolism. 1989;38:453–8. doi: 10.1016/0026-0495(89)90198-4. [DOI] [PubMed] [Google Scholar]
- 55.Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106:473–81. doi: 10.1172/JCI10842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hellmér J, Marcus C, Sonnenfeld T, Arner P. Mechanisms for differences in lipolysis between human subcutaneous and omental fat cells. J Clin Endocrinol Metab. 1992;75:15–20. doi: 10.1210/jc.75.1.15. [DOI] [PubMed] [Google Scholar]
- 57.Arner P, Hellström L, Wahrenberg H, Brönnegård M. Beta-adrenoceptor expression in human fat cells from different regions. J Clin Invest. 1990;86:1595–600. doi: 10.1172/JCI114880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vikman HL, Savola JM, Raasmaja A, Ohisalo JJ. Alpha 2A-adrenergic regulation of cyclic AMP accumulation and lipolysis in human omental and subcutaneous adipocytes. Int J Obes Relat Metab Disord. 1996;20:185–9. [PubMed] [Google Scholar]
- 59.Ramis JM, Bibiloni B, Moreiro J, García-Sanz JM, Salinas R, Proenza AM, et al. Tissue leptin and plasma insulin are associated with lipoprotein lipase activity in severely obese patients. J Nutr Biochem. 2005;16:279–85. doi: 10.1016/j.jnutbio.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 60.Berndt J, Kovacs P, Ruschke K, Klöting N, Fasshauer M, Schön MR, et al. Fatty acid synthase gene expression in human adipose tissue: association with obesity and type 2 diabetes. Diabetologia. 2007;50:1472–80. doi: 10.1007/s00125-007-0689-x. [DOI] [PubMed] [Google Scholar]
- 61.Berndt J, Kralisch S, Klöting N, Ruschke K, Kern M, Fasshauer M, et al. Adipose triglyceride lipase gene expression in human visceral obesity. Exp Clin Endocrinol Diabetes. 2008;116:203–10. doi: 10.1055/s-2007-993148. [DOI] [PubMed] [Google Scholar]
- 62.Albu JB, Curi M, Shur M, Murphy L, Matthews DE, Pi-Sunyer FX. Systemic resistance to the antilipolytic effect of insulin in black and white women with visceral obesity. Am J Physiol. 1999;277:E551–60. doi: 10.1152/ajpendo.1999.277.3.E551. [DOI] [PubMed] [Google Scholar]
- 63.Mittelman SD, Van Citters GW, Kirkman EL, Bergman RN. Extreme insulin resistance of the central adipose depot in vivo. Diabetes. 2002;51:755–61. doi: 10.2337/diabetes.51.3.755. [DOI] [PubMed] [Google Scholar]
- 64.Bolinder J, Kager L, Ostman J, Arner P. Differences at the receptor and postreceptor levels between human omental and subcutaneous adipose tissue in the action of insulin on lipolysis. Diabetes. 1983;32:117–23. doi: 10.2337/diabetes.32.2.117. [DOI] [PubMed] [Google Scholar]
- 65.Zierath JR, Livingston JN, Thörne A, Bolinder J, Reynisdottir S, Lönnqvist F, et al. Regional difference in insulin inhibition of non-esterified fatty acid release from human adipocytes: relation to insulin receptor phosphorylation and intracellular signalling through the insulin receptor substrate-1 pathway. Diabetologia. 1998;41:1343–54. doi: 10.1007/s001250051075. [DOI] [PubMed] [Google Scholar]
- 66.Lefebvre AM, Laville M, Vega N, Riou JP, van Gaal L, Auwerx J, et al. Depot-specific differences in adipose tissue gene expression in lean and obese subjects. Diabetes. 1998;47:98–103. doi: 10.2337/diabetes.47.1.98. [DOI] [PubMed] [Google Scholar]
- 67.Veilleux A, Caron-Jobin M, Noël S, Laberge PY, Tchernof A. Visceral adipocyte hypertrophy is associated with dyslipidemia independent of body composition and fat distribution in women. Diabetes. 2011;60:1504–11. doi: 10.2337/db10-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gauthier MS, O’Brien EL, Bigornia S, Mott M, Cacicedo JM, Xu XJ, et al. Decreased AMP-activated protein kinase activity is associated with increased inflammation in visceral adipose tissue and with whole-body insulin resistance in morbidly obese humans. Biochem Biophys Res Commun. 2011;404:382–7. doi: 10.1016/j.bbrc.2010.11.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Niesler CU, Siddle K, Prins JB. Human preadipocytes display a depot-specific susceptibility to apoptosis. Diabetes. 1998;47:1365–8. doi: 10.2337/diabetes.47.8.1365. [DOI] [PubMed] [Google Scholar]
- 70.Spiegelman BM. PPAR-gamma: adipogenic regulator and thiazolidinedione receptor. Diabetes. 1998;47:507–14. doi: 10.2337/diabetes.47.4.507. [DOI] [PubMed] [Google Scholar]
- 71.Hauner H, Wabitsch M, Pfeiffer EF. Differentiation of adipocyte precursor cells from obese and nonobese adult women and from different adipose tissue sites. Horm Metab Res Suppl. 1988;19:35–9. [PubMed] [Google Scholar]
- 72.Poussin C, Hall D, Minehira K, Galzin AM, Tarussio D, Thorens B. Different transcriptional control of metabolism and extracellular matrix in visceral and subcutaneous fat of obese and rimonabant treated mice. PLoS One. 2008;3:e3385. doi: 10.1371/journal.pone.0003385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hoffstedt J, Arner E, Wahrenberg H, Andersson DP, Qvisth V, Löfgren P, et al. Regional impact of adipose tissue morphology on the metabolic profile in morbid obesity. Diabetologia. 2010;53:2496–503. doi: 10.1007/s00125-010-1889-3. [DOI] [PubMed] [Google Scholar]
- 74.Gealekman O, Guseva N, Hartigan C, Apotheker S, Gorgoglione M, Gurav K, et al. Depot-specific differences and insufficient subcutaneous adipose tissue angiogenesis in human obesity. Circulation. 2011;123:186–94. doi: 10.1161/CIRCULATIONAHA.110.970145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alvarez GE, Beske SD, Ballard TP, Davy KP. Sympathetic neural activation in visceral obesity. Circulation. 2002;106:2533–6. doi: 10.1161/01.CIR.0000041244.79165.25. [DOI] [PubMed] [Google Scholar]
- 76.Barzilai N, She L, Liu BQ, Vuguin P, Cohen P, Wang J, et al. Surgical removal of visceral fat reverses hepatic insulin resistance. Diabetes. 1999;48:94–8. doi: 10.2337/diabetes.48.1.94. [DOI] [PubMed] [Google Scholar]
- 77.Gabriely I, Ma XH, Yang XM, Atzmon G, Rajala MW, Berg AH, et al. Removal of visceral fat prevents insulin resistance and glucose intolerance of aging: an adipokine-mediated process? Diabetes. 2002;51:2951–8. doi: 10.2337/diabetes.51.10.2951. [DOI] [PubMed] [Google Scholar]
- 78.Kim YW, Kim JY, Lee SK. Surgical removal of visceral fat decreases plasma free fatty acid and increases insulin sensitivity on liver and peripheral tissue in monosodium glutamate (MSG)-obese rats. J Korean Med Sci. 1999;14:539–45. doi: 10.3346/jkms.1999.14.5.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pitombo C, Araújo EP, De Souza CT, Pareja JC, Geloneze B, Velloso LA. Amelioration of diet-induced diabetes mellitus by removal of visceral fat. J Endocrinol. 2006;191:699–706. doi: 10.1677/joe.1.07069. [DOI] [PubMed] [Google Scholar]
- 80.Foster MT, Shi H, Seeley RJ, Woods SC. Transplantation or removal of intra-abdominal adipose tissue prevents age-induced glucose insensitivity. Physiol Behav. 2010;101:282–8. doi: 10.1016/j.physbeh.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shi H, Strader AD, Woods SC, Seeley RJ. The effect of fat removal on glucose tolerance is depot specific in male and female mice. Am J Physiol Endocrinol Metab. 2007;293:E1012–20. doi: 10.1152/ajpendo.00649.2006. [DOI] [PubMed] [Google Scholar]
- 82.Fabbrini E, Tamboli RA, Magkos F, Marks-Shulman PA, Eckhauser AW, Richards WO, et al. Surgical removal of omental fat does not improve insulin sensitivity and cardiovascular risk factors in obese adults. Gastroenterology. 2010;139:448–55. doi: 10.1053/j.gastro.2010.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Herrera MF, Pantoja JP, Velázquez-Ferńndez D, Cabiedes J, Aguilar-Salinas C, García-García E, et al. Potential additional effect of omentectomy on metabolic syndrome, acute-phase reactants, and inflammatory mediators in grade III obese patients undergoing laparoscopic Roux-en-Y gastric bypass: a randomized trial. Diabetes Care. 2010;33:1413–8. doi: 10.2337/dc09-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Thörne A, Lönnqvist F, Apelman J, Hellers G, Arner P. A pilot study of long-term effects of a novel obesity treatment: omentectomy in connection with adjustable gastric banding. Int J Obes Relat Metab Disord. 2002;26:193–9. doi: 10.1038/sj.ijo.0801871. [DOI] [PubMed] [Google Scholar]
- 85.Milleo FQ, Campos AC, Santoro S, Lacombe A, Santo MA, Vicari MR, et al. Metabolic effects of an entero-omentectomy in mildly obese type 2 diabetes mellitus patients after three years. Clinics (Sao Paulo) 2011;66:1227–33. doi: 10.1590/S1807-59322011000700018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Klein S, Fontana L, Young VL, Coggan AR, Kilo C, Patterson BW, et al. Absence of an effect of liposuction on insulin action and risk factors for coronary heart disease. N Engl J Med. 2004;350:2549–57. doi: 10.1056/NEJMoa033179. [DOI] [PubMed] [Google Scholar]
- 87.Yost TJ, Rodgers CM, Eckel RH. Suction lipectomy: outcome relates to region-specific lipoprotein lipase activity and interval weight change. Plast Reconstr Surg. 1993;92:1101–8, discussion 1109-11. doi: 10.1097/00006534-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 88.Lambert EV, Hudson DA, Bloch CE, Koeslag JH. Metabolic response to localized surgical fat removal in nonobese women. Aesthetic Plast Surg. 1991;15:105–10. doi: 10.1007/BF02273842. [DOI] [PubMed] [Google Scholar]
- 89.Mauer MM, Harris RB, Bartness TJ. The regulation of total body fat: lessons learned from lipectomy studies. Neurosci Biobehav Rev. 2001;25:15–28. doi: 10.1016/S0149-7634(00)00047-6. [DOI] [PubMed] [Google Scholar]
- 90.Mauer MM, Bartness TJ. Fat pad-specific compensatory mass increases after varying degrees of lipectomy in Siberian hamsters. Am J Physiol. 1997;273:R2117–23. doi: 10.1152/ajpregu.1997.273.6.R2117. [DOI] [PubMed] [Google Scholar]
- 91.Mauer MM, Bartness TJ. Temporal changes in fat pad mass and cellularity after lipectomy in Siberian hamsters. Physiol Behav. 1997;62:1029–36. doi: 10.1016/S0031-9384(97)00233-3. [DOI] [PubMed] [Google Scholar]
- 92.Mauer MM, Bartness TJ. Short-day-like body weight changes do not prevent fat pad compensation after lipectomy in Siberian hamsters. Am J Physiol. 1997;272:R68–77. doi: 10.1152/ajpregu.1997.272.1.R68. [DOI] [PubMed] [Google Scholar]
- 93.Mauer MM, Bartness TJ. Photoperiod-dependent fat pad mass and cellularity changes after partial lipectomy in Siberian hamsters. Am J Physiol. 1996;270:R383–92. doi: 10.1152/ajpregu.1996.270.2.R383. [DOI] [PubMed] [Google Scholar]
- 94.Mauer MM, Bartness TJ. A role for testosterone in the maintenance of seasonally appropriate body mass but not in lipectomy-induced body fat compensation in Siberian hamsters. Obes Res. 1995;3:31–41. doi: 10.1002/j.1550-8528.1995.tb00118.x. [DOI] [PubMed] [Google Scholar]
- 95.Mauer MM, Bartness TJ. Body fat regulation after partial lipectomy in Siberian hamsters is photoperiod dependent and fat pad specific. Am J Physiol. 1994;266:R870–8. doi: 10.1152/ajpregu.1994.266.3.R870. [DOI] [PubMed] [Google Scholar]
- 96.Hamilton JM, Wade GN. Lipectomy does not impair fattening induced by short photoperiods or high-fat diets in female Syrian hamsters. Physiol Behav. 1988;43:85–92. doi: 10.1016/0031-9384(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 97.Dark J, Forger NG, Stern JS, Zucker I. Recovery of lipid mass after removal of adipose tissue in ground squirrels. Am J Physiol. 1985;249:R73–8. doi: 10.1152/ajpregu.1985.249.1.R73. [DOI] [PubMed] [Google Scholar]
- 98.Shi H, Song CK, Giordano A, Cinti S, Bartness TJ. Sensory or sympathetic white adipose tissue denervation differentially affects depot growth and cellularity. Am J Physiol Regul Integr Comp Physiol. 2005;288:R1028–37. doi: 10.1152/ajpregu.00648.2004. [DOI] [PubMed] [Google Scholar]
- 99.Hausman DB, Lu J, Ryan DH, Flatt WP, Harris RB. Compensatory growth of adipose tissue after partial lipectomy: involvement of serum factors. Exp Biol Med (Maywood) 2004;229:512–20. doi: 10.1177/153537020422900609. [DOI] [PubMed] [Google Scholar]
- 100.Shi H, Bowers RR, Bartness TJ. Norepinephrine turnover in brown and white adipose tissue after partial lipectomy. Physiol Behav. 2004;81:535–42. doi: 10.1016/j.physbeh.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 101.Foster MT, Bartness TJ. Sympathetic but not sensory denervation stimulates white adipocyte proliferation. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1630–7. doi: 10.1152/ajpregu.00197.2006. [DOI] [PubMed] [Google Scholar]
- 102.Bartness TJ, Shrestha YB, Vaughan CH, Schwartz GJ, Song CK. Sensory and sympathetic nervous system control of white adipose tissue lipolysis. Mol Cell Endocrinol. 2010;318:34–43. doi: 10.1016/j.mce.2009.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Harris RB, Leibel RL. Location, location, location. Cell Metab. 2008;7:359–61. doi: 10.1016/j.cmet.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 104.Ashwell M. The use of the adipose tissue transplantation technique to demonstrate that abnormalities in the adipose tissue metabolism of genetically obese mice are due to extrinsic rather than intrinsic factors. Int J Obes. 1985;9(Suppl 1):77–82. [PubMed] [Google Scholar]
- 105.Sommer B, Sattler G. Current concepts of fat graft survival: histology of aspirated adipose tissue and review of the literature. Dermatol Surg. 2000;26:1159–66. doi: 10.1046/j.1524-4725.2000.00278.x. [DOI] [PubMed] [Google Scholar]
- 106.Liebelt RA, Vismara L, Liebelt AG. Autoregulation of adipose tissue mass in the mouse. Proc Soc Exp Biol Med. 1968;127:458–62. doi: 10.3181/00379727-127-32714. [DOI] [PubMed] [Google Scholar]
- 107.Colombo C, Cutson JJ, Yamauchi T, Vinson C, Kadowaki T, Gavrilova O, et al. Transplantation of adipose tissue lacking leptin is unable to reverse the metabolic abnormalities associated with lipoatrophy. Diabetes. 2002;51:2727–33. doi: 10.2337/diabetes.51.9.2727. [DOI] [PubMed] [Google Scholar]
- 108.Gavrilova O, Marcus-Samuels B, Graham D, Kim JK, Shulman GI, Castle AL, et al. Surgical implantation of adipose tissue reverses diabetes in lipoatrophic mice. J Clin Invest. 2000;105:271–8. doi: 10.1172/JCI7901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lacy EL, Bartness TJ. Effects of white adipose tissue grafts on total body fat and cellularity are dependent on graft type and location. Am J Physiol Regul Integr Comp Physiol. 2005;289:R380–8. doi: 10.1152/ajpregu.00116.2005. [DOI] [PubMed] [Google Scholar]
- 110.Lacy EL, Bartness TJ. Autologous fat transplants influence compensatory white adipose tissue mass increases after lipectomy. Am J Physiol Regul Integr Comp Physiol. 2004;286:R61–70. doi: 10.1152/ajpregu.00476.2003. [DOI] [PubMed] [Google Scholar]
- 111.Konrad D, Rudich A, Schoenle EJ. Improved glucose tolerance in mice receiving intraperitoneal transplantation of normal fat tissue. Diabetologia. 2007;50:833–9. doi: 10.1007/s00125-007-0596-1. [DOI] [PubMed] [Google Scholar]
- 112.Hocking SL, Chisholm DJ, James DE. Studies of regional adipose transplantation reveal a unique and beneficial interaction between subcutaneous adipose tissue and the intra-abdominal compartment. Diabetologia. 2008;51:900–2. doi: 10.1007/s00125-008-0969-0. [DOI] [PubMed] [Google Scholar]
- 113.Tran TT, Yamamoto Y, Gesta S, Kahn CR. Beneficial effects of subcutaneous fat transplantation on metabolism. Cell Metab. 2008;7:410–20. doi: 10.1016/j.cmet.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Foster MT, Shi H, Seeley RJ, Woods SC. Transplantation or removal of intra-abdominal adipose tissue prevents age-induced glucose insensitivity. Physiol Behav. 2010;101:282–8. doi: 10.1016/j.physbeh.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Foster MT, Shi H, Softic S, Kohli R, Seeley RJ, Woods SC. Transplantation of non-visceral fat to the visceral cavity improves glucose tolerance in mice: investigation of hepatic lipids and insulin sensitivity. Diabetologia. 2011;54:2890–9. doi: 10.1007/s00125-011-2259-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Foster MT, Shi H, Seeley RJ, Woods SC. Removal of intra-abdominal visceral adipose tissue improves glucose tolerance in rats: role of hepatic triglyceride storage. Physiol Behav. 2011;104:845–54. doi: 10.1016/j.physbeh.2011.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rytka JM, Wueest S, Schoenle EJ, Konrad D. The portal theory supported by venous drainage-selective fat transplantation. Diabetes. 2011;60:56–63. doi: 10.2337/db10-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]