Abstract
Objective
To determine the prevalence of HIV seropositivity among patients with squamous cell carcinoma of the conjunctiva.
Methods
All patients with clinical and histopathological confirmation of squamous cell carcinoma seen during a ten year period (July 1999 to June 2009) were tested for HIV (Human Immunodeficiency Virus). The number of patients with squamous cell carcinoma of the conjunctiva who are HIV positive were counted.
Results
A total of thirty-three(33) eyes in thirty-two(32) patients were confirmed histopathologically to have conjunctival squamous cell carcinoma. Their ages ranged from 22 years to 66 years with a mean age of (38.6±11.8) years (SD). The male to female ratio was 1:1.5. Twenty four (75%) of these patients were HIV positive.
Conclusions
Squamous cell carcinoma is associated with the human immunodeficiency virus and is thus a marker for the disease in Benin City, Nigeria.
Keywords: Squamous cell carcinoma, Conjunctiva, HIV
1. Introduction
Squamous cell carcinoma of the conjunctiva is the most frequently encountered conjunctival malignancy[1]. It is characterised by low grade aggressiveness that seldom leads to intraocular or intraorbital invasion[2]–[4]. It is slowly growing and occurs more commonly in the tropics than in temperate regions[1]. This has been attributed to the high ambient ultraviolet radiation found in the tropics[5].
The incidence of this neoplasm worldwide varies from 0.02 to 3.5 per 100 000[6]. There have been reports documenting a recent increase in its incidence especially in equatorial Africa[7],[8]. A combination of risk factors such as intense exposure to ultraviolet light, HIV-induced immunosuppression resulting in reduction in the effectiveness of the immune surveillance system and co-infection with the human papilloma virus is believed to hasten its development[9].
Various reports show that there is a higher prevalence of HIV seropositivity among patients presenting with squamous cell carcinoma of the conjunctiva[7]–[9]. In some cases, it may be the only manifestation in an otherwise healthy looking adult[10]. Thus, it is a marker for HIV in Africa.
Previous authors in Benin City, Nigeria have documented the association between herpes zoster ophthalmicus and HIV infection[11].
The aim of this study is to determine the association between squamous cell carcinoma of the conjunctiva and HIV in Benin City.
2. Materials and methods
This is a prospective study of patients diagnosed with squamous cell carcinoma of the conjunctiva from the pathology department of the University of Benin Teaching Hospital, Benin City from July 1999 to June 2 009. The age, sex, occupation, presenting complaints and duration of symptoms were noted. The presenting visual acuity, retroviral status using the Western blot technique, histological type of carcinoma, the treatment offered and follow up period were also noted. Analysis of the findings was done by computer using the Instat GraphPadtm version 2.05a software. The study was approved by the ethics committee of the hospital.
Treatment included excision biopsy with 2 mm free margin and mitomycin C application to the base of the tumour for localised tumours, enucleation of the affected eye for patients with visual loss following intraocular extension, incision biopsy/debulking and adjuvant radiotherapy for patients with intraorbital extension. Recurrent localised tumours also had cryotherapy applied to the margins of the resected tumour.
3. Results
A total of thirty three eyes in thirty two patients had histopathologic confirmation of squamous cell carcinoma of the conjunctiva. There were thirteen males and nineteen females giving a male to female ratio of about 1:1.5. Their ages ranged from 22 years to 66 years with a mean age of 38.6 years±11.8(SD), Median=36. Table 1 shows the biodata of the patients.
Table 1. Squamous cell carcinoma of the conjunctiva and HIV status.
| S/N | Occupation | Sex | Age | Visual acuity | Eye affected | HIV status | Treatment |
| 1 | Mechanic | M | 27 | NLP | RE | +VE | ENU |
| 2 | Trader | F | 30 | NLP | RE | +VE | ENU+RA |
| 3 | Tailor | F | 32 | 6/5 | LE | +VE | EXC |
| 4 | Technician | M | 45 | 6/6 | RE | +VE | EXC |
| 5 | Farmer | F | 57 | NLP | RE | -VE | INC+RA |
| 6 | Sec | M | 48 | 6/9 | LE | +VE | EXC |
| 7 | Tailor | F | 28 | 6/18 | LE | -VE | EXC |
| 8 | Civil Serv | F | 36 | 6/24 | LE | +VE | EXC |
| 9 | Driver | M | 58 | LP | LE | -VE | ENU |
| 10 | Driver | M | 58 | 6/18 | RE | -VE | EXC |
| 11 | Policeman | M | 42 | 6/6 | RE | +VE | EXC |
| 12 | Farmer | M | 48 | 6/12 | RE | -VE | EXC |
| 13 | Student | F | 28 | 6/36 | LE | +VE | EXC |
| 14 | Student | F | 28 | 6/6 | LE | -VE | EXC |
| 15 | Trader | F | 36 | 6/12 | RE | -VE | EXC |
| 16 | Trader | F | 32 | NLP | RE | +VE | ENU |
| 17 | Student | M | 26 | 6/6 | RE | -VE | EXC |
| 18 | Farmer | M | 55 | NLP | RE | +VE | ENU+RA |
| 19 | Student | M | 22 | 6/60 | LE | +VE | EXC |
| 20 | Civil Serv | M | 40 | 6/12 | LE | +VE | EXC |
| 21 | Civil Serv | F | 52 | 6/18 | RE | +VE | EXC |
| 22 | Student | F | 35 | 6/5 | RE | +VE | EXC |
| 23 | Trader | F | 43 | 6/24 | RE | +VE | EXC |
| 24 | Trader | F | 66 | 6/18 | LE | +VE | EXC |
| 25 | Civil Serv | F | 36 | 6/18 | RE | +VE | EXC |
| 26 | Civil Serv | F | 28 | 6/9 | LE | +VE | EXC |
| 27 | Civil Serv | M | 55 | 6/36 | LE | +VE | EXC |
| 28 | Trader | F | 39 | 6/12 | RE | +VE | EXC |
| 29 | Farmer | F | 50 | 6/6 | LE | -VE | EXC |
| 30 | Trader | F | 37 | 6/9 | RE | +VE | EXC |
| 31 | Farmer | M | 25 | 6/6 | RE | +VE | EXC |
| 32 | Student | M | 22 | 6/6 | LE | +VE | EXC |
| 33 | Trader | F | 30 | 6/36 | LE | +VE | EXC |
KEY: VA- visual acuity, RE-right eye, LE -left eye, +VE-positive, -VE-negative, EXC-excision biopsy with mitomycin-c, RA-radiotherapy, ENU-enucleation, INC-incision biopsy, Sec-security man, Civil Serv- Civil Servant.
The right eye was involved in 18 cases (54.5%) while the left was involved in 15 cases (45.5%). Twenty one cases (63.6%) had a presenting visual acuity in the affected eye of 6/18 and better. Six cases (18.2%) were blind in the affected eye. This is shown in Table 1.
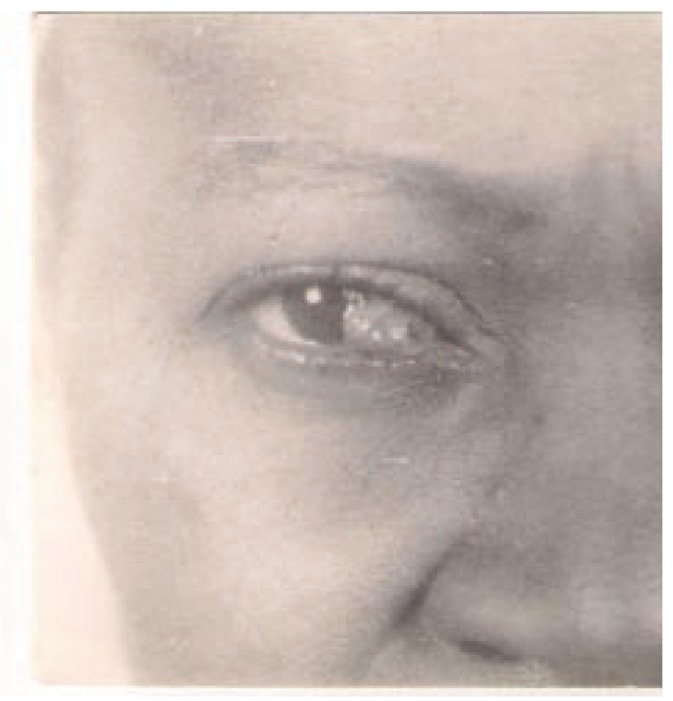
The main presenting symptom was a growth in the affected eye in 30 patients with a duration from 2 weeks to 2 years with a mean of 7.5 months (Figure 1). The other presenting complaints were ocular pain in 16 patients, redness of the eyes in 12 patients and decrease in vision in 10 patients. Six patients complained of tearing while 5 complained of itching in the affected eye.
Figure 1. The right eye of a patient with squamous cell carcinoma of the conjunctiva.
Twenty four patients (75%) were retroviral positive while eight patients (25%) were negative for the human immunodeficiency virus.
Twenty seven eyes (81.8%) with localised tumours had excision biopsy with mitomycin C application. One patient who was also HIV positive presenting with a recurrent tumour had cryotherapy applied to the margins of the tumour in addition to mitomycin C application. Four eyes (12.1%) had enucleation following intraocular extension with poor visual potential. One of the patients had regional metastasis to the ipsilateral preauricular and submandibular lymph nodes was also HIV positive. Two eyes (6.1%) had incision biopsy with radiotherapy due to intraorbital extension. One patient had repeat excision biopsy with mitomycin C for a recurrent tumour. This patient although not HIV positive earlier had enucleation for the same tumour in the contralateral eye following intraocular extension with visual loss.
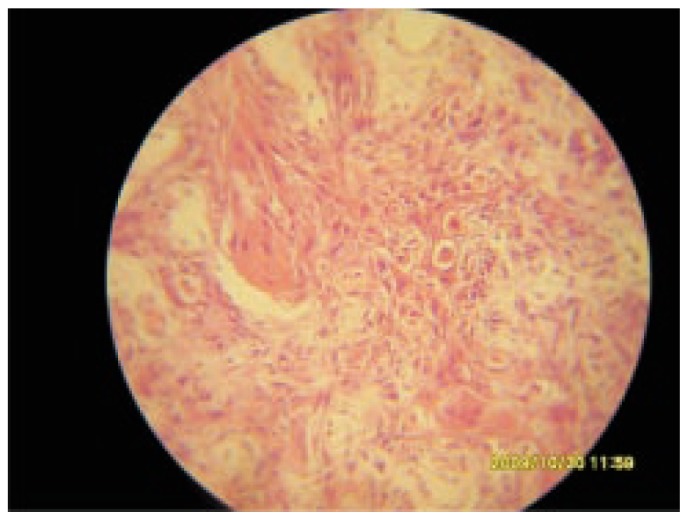
Eighteen eyes (54.5%) had well differentiated invasive squamous cell carcinoma (Figure 2), six eyes (18.2%) had moderately differentiated squamous cell carcinoma while four eyes (12.1%) had poorly differentiated squamous cell carcinoma. Five eyes (15.2%) had carcinoma- in situ.
Figure 2. Well differentiated squamous cell carcinoma of the conjunctiva.
The follow up period following surgical intervention ranged from those lost to follow up after excision to a maximum of one year. Five patients (15.6%) were lost to follow up after excision of the tumour. The maximum follow up period of one year was recorded in only one patient (3.1%).
4. Discussion
Squamous cell carcinoma although, the most frequently encountered conjunctival malignancy is still an uncommon tumour of the conjunctiva[1],[6]. The exact cause is not known. There are various theories of aetiology which include exposure to ultraviolet light, chronic local irritation, pre-existing trauma or local inflammation[5],[10]–[13].
In this study, the mean age of the patients presenting with this condition over the period was 38.6 years. This is lower than that of 45 years reported by Olurin14 and 42 years reported by Ukponmwan et al[15]. This may indicate a changing pattern in the presentation of the disease with a steady decrease in the age at presentation due to other modifying factors. However, it still falls within the period where it is found to be more common which is between the fourth and sixth decade[1],[4].
Outdoor workers constituted 53.1% of the patients. This is lower than 77.8% reported by Ukponmwan et al[15]. The disparity may be attributed to the fact that their study was conducted mostly prior to the wide prevalence of the HIV pandemic in the study area which may now be a modifying factor. Occupational exposure to sunlight has been identified as a risk factor of squamous cell carcinoma[5],[16],[17].
In this study, there was a female preponderance with a male to female ratio of 1:1.5. This is in contrast to other findings which show more males affected[4],[15],[17]. The male predominance in the presentation of the disease has been linked to their occupational exposure to sunlight which is lacking in this study.
Six eyes (18.2%) had a visual acuity of no light perception at presentation due to intraocular and intraorbital extension, one of which had ipsilateral nodal involvement of the preauricular and submandibular nodes. This may indicate delayed presentation as some patients had duration of symptoms of up to 2 years. Late presentation to the hospital among patients with squamous cell carcinoma in Nigeria has been previously documented[4],[15]. Delay in seeking medical attention has been found to be an important prognostic factor in squamous cell carcinoma of the conjunctiva[15],[16]. Squamous cell carcinoma of the conjunctiva appears to behave more aggressively in the tropics than in temperate regions[18]. The more aggressive nature of the tumour is reflected by intraocular and intraorbital extension with a higher incidence of metastasis and tumour related deaths[18].The major factor for regional or distant metastasis is the delay in seeking medical advice[18].
The prevalence of HIV seropositivity in this study was 75%. In Uganda, a study done found a prevalence of 71% while in Malawi, this was 86%[8],[9]. A case control study in Rwanda also demonstrated that HIV infection is a risk factor for the development of squamous cell dysplasia and neoplasia of the conjunctiva[7]. These findings are all similar and suggest a strong association between HIV and squamous cell carcinoma of the conjunctiva.
One patient had bilateral disease with the right eye presenting first before the left. He had enucleation for the right eye due to intraocular extension and excision with MMC in the left eye. Systemic evaluation ruled out an underlying malignant condition which indicates that it is a primary malignancy. This presentation has also been earlier documented[19]. This patient who was HIV negative is a driver and exposed to ultraviolet radiation, a prime culprit in the aetiology of squamous cell carcinoma[5].
There was poor follow up after resection of the tumour with failure of 5 patients to present after the surgery. The maximum follow up period recorded was one year. This may reflect the level of education of the patients and is a well documented problem in the management of patients in Nigeria[4],[15].
There is a rise in the incidence of squamous cell carcinoma of the conjunctiva which is closely linked to the HIV pandemic. Vigorous health education of the people on the prevention of HIV and the importance of early presentation for medical intervention will be of immense benefit. Health education of outdoor workers on the use of ultraviolet radiation blocking lenses by is also beneficial.
Squamous cell carcinoma of the conjunctiva has been shown to be a marker of HIV seropositivity or AIDS in patients in this study. It is recommended that all patients presenting with squamous cell carcinoma of the conjunctiva in Nigeria and Africa should be tested for HIV seropositivity.
Patients should be educated or encouraged to present early to the hospital to enable early and prompt treatment of the condition (tumour) and so improve prognosis.
Footnotes
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39(6):429–450. doi: 10.1016/s0039-6257(05)80054-2. [DOI] [PubMed] [Google Scholar]
- 2.Iliff WJ, Marback R, Green WR. Invasive squamous cell carcinoma of the conjunctiva. Arch Ophthalmol. 1975;93:119–122. doi: 10.1001/archopht.1975.01010020125005. [DOI] [PubMed] [Google Scholar]
- 3.Nicholson DH, Herschler J. Intraocular extension of squamous cell carcinoma of the conjunctiva. Arch Ophthalmol. 1977;95:843–846. doi: 10.1001/archopht.1977.04450050121015. [DOI] [PubMed] [Google Scholar]
- 4.Abiose A, Adido J. Invasive squamous cell carcinoma of the conjunctiva in Kaduna. Nig J Ophthalmol. 1986;2:34–39. [Google Scholar]
- 5.Newton R, Ferlay J, Reeves G, Beral V, Parkin DM. Effect of ambient solar ultraviolet radiation on incidence of squamous cell carcinoma of the eye. Lancet. 1996;347:1450–1451. doi: 10.1016/s0140-6736(96)91685-2. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Foster CS. Squamous cell carcinoma of the conjunctiva. Int Ophthalmol Clin. 1997;37:73–85. doi: 10.1097/00004397-199703740-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kestelyn P, Stevens AM, Ndayambaje A, Hanssens M, Van de Perre P. HIV and conjunctival malignancies. Lancet. 1990;336:51–52. doi: 10.1016/0140-6736(90)91562-o. [DOI] [PubMed] [Google Scholar]
- 8.Waddell K, Lewallen S, Lucas S, Ateenyi-Agaba C, Herrington CS, Liomba G. Carcinoma of the conjunctiva and HIV infection in Uganda and Malawi. Br J Ophthalmol. 1996;80:503–508. doi: 10.1136/bjo.80.6.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ateenyi-Agaba C. Conjunctival squamous cell carcinoma associated with HIV infection in Kampala, Uganda. Lancet. 1995;345:695–696. doi: 10.1016/s0140-6736(95)90870-6. [DOI] [PubMed] [Google Scholar]
- 10.Guramatunhu S. Squamous cell carcinoma in HIV/AIDS. Comm Eye Health. 2003;16:37. [PMC free article] [PubMed] [Google Scholar]
- 11.Osahon AI. HIV infection and Herpes zoster opthalmicus, University of Benin Teaching Hospital eye clinic experience (initial observation) Nig J Ophthalmol. 1999;7(1):1–4. [Google Scholar]
- 12.Dawodu OA, Osahon AI. Ophthalmic herpes zoster and HIV infection in Edo state, Nigeria. S Afr Med J. 2005;95(1):30–31. [PubMed] [Google Scholar]
- 13.Kushner FH, Mushen RL. Conjunctival squamous cell carcinoma combined with malignant lymphoma. Am J Ophthalmol. 1975;80:503–506. doi: 10.1016/0002-9394(75)90215-9. [DOI] [PubMed] [Google Scholar]
- 14.Olurin O, William AO. Orbito-ocular tumours in Nigeria. Cancer. 1972;30:580–587. doi: 10.1002/1097-0142(197208)30:2<580::aid-cncr2820300239>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 15.Ukponmwan CU, Igbokwe UO, Aligbe JU. Squamous cell carcinoma of the conjunctiva in Benin City, Nigeria. Nig J Clin Prac. 2002;5:143–147. [Google Scholar]
- 16.McKelvie PA, Daniell M, McNab A, Loughnan M, Santamaria JD. Squamous cell carcinoma of the conjunctiva: a series of 26 cases. Br J Ophthalmol. 2002;86:168–173. doi: 10.1136/bjo.86.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tunc M, Char DH, Crawford B, Miller T. Intraepithelial and invasive squamous cell carcinoma: analysis of 60 cases. Br J Ophthalmol. 1999;83:98–103. doi: 10.1136/bjo.83.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tabbara KF, Kersten R, Daouk N, Blodi FC. Metastatic squamous cell carcinoma of the conjunctiva. Ophthalmol. 1988;95:318–321. doi: 10.1016/s0161-6420(88)33180-5. [DOI] [PubMed] [Google Scholar]
- 19.Olurin O. Bilateral conjunctival epithelioma in an adolescent. Ann Ophthalmol. 1975:633–636. [PubMed] [Google Scholar]


